Abstract
Background
People with dementia have unique palliative and end-of-life needs. However, access to quality palliative and end-of-life care for people with dementia living in nursing homes is often suboptimal. There is a recognised need for nursing home staff training in dementia-specific palliative care to equip them with knowledge and skills to deliver high quality care.
Objective
The primary aim was to evaluate the effectiveness of a simulation training intervention (IMPETUS-D) aimed at nursing home staff on reducing unplanned transfers to hospital and/or deaths in hospital among residents living with dementia.
Design
Cluster randomised controlled trial of nursing homes with process evaluation conducted alongside.
Subjects & setting
One thousand three hundred four people with dementia living in 24 nursing homes (12 intervention/12 control) in three Australian cities, their families and direct care staff.
Methods
Randomisation was conducted at the level of the nursing home (cluster). The allocation sequence was generated by an independent statistician using a computer-generated allocation sequence.
Staff from intervention nursing homes had access to the IMPETUS-D training intervention, and staff from control nursing homes had access to usual training opportunities. The predicted primary outcome measure was a 20% reduction in the proportion of people with dementia who had an unplanned transfer to hospital and/or death in hospital at 6-months follow-up in the intervention nursing homes compared to the control nursing homes.
Results
At 6-months follow-up, 128 (21.1%) people with dementia from the intervention group had an unplanned transfer or death in hospital compared to 132 (19.0%) residents from the control group; odds ratio 1.14 (95% CI, 0.82-1.59). There were suboptimal levels of staff participation in the training intervention and several barriers to participation identified.
Conclusion
This study of a dementia-specific palliative care staff training intervention found no difference in the proportion of residents with dementia who had an unplanned hospital transfer. Implementation of the intervention was challenging and likely did not achieve adequate staff coverage to improve staff practice or resident outcomes.
Trial registration
Australian New Zealand Clinical Trials Registry (ANZCTR): ACTRN12618002012257. Registered 14 December 2018.
Similar content being viewed by others
Background
People with advanced dementia and their families have specific palliative and end-of-life care needs due to the unpredictable disease trajectory, the severe cognitive impairment that affects the person’s decision-making capacity, verbal communication and behavioural and psychological symptoms of dementia, and the impact it can have on family carer burden [1,2,3,4,5]. For many people with advanced dementia, the last months or years of life are spent in nursing homes [6]. However, there are reports of suboptimal palliative and end-of-life dementia care, including unnecessary transfers to hospital, burdensome interventions, and poor pain management [3, 7, 8]. It has been identified that a major contributory factor to this includes low levels of staff education and skills in provision of palliative and end-of-life care [9, 10].
Training nursing home staff in dementia-specific palliative care is a recognised strategy to improve the quality of care provided, and has been recommended by the European Association for Palliative Care, the Worldwide Hospice Palliative Care Alliance, and more recently in Australia by the Royal Commission into Aged Care Quality and Safety [5, 9,10,11]. Despite this recommendation, there is a paucity of robust research and evidence to support the use of dementia palliative care training interventions. Previous studies were small, involved one or two sites only, or used a non-randomised study design [12,13,14,15,16,17]. Our study set out to help fill this gap in evidence and was innovative in its use of simulation training. Simulation is an immersive training technique that attempts to evoke real-life scenarios to promote deeper learning and better transfer of skills to work. There is a growing evidence base to support the benefits of simulation in healthcare education. Meta-analyses have shown simulation using virtual patients and technology enhanced simulation can improve healthcare professionals’ knowledge and skills and have small to moderate patient benefits compared to no training or traditional education methods [18,19,20]. However, to date very few simulation studies have been conducted in nursing homes and there are no controlled trials on dementia-specific palliative care [21]. Among the few studies that have assessed dementia-specific palliative care training in nursing homes, two used simulation techniques but were single-site, non- randomised studies and of low methodological quality [15, 16].
This study evaluated a training program IMproving Palliative care Education and Training Using Simulation in Dementia (IMPETUS-D) for nurses and personal care workers (PCWs), aimed at improving the quality of palliative care provision and outcomes for people with dementia living in nursing homes. The study used a cluster randomised controlled trial (RCT) design in parallel with a process evaluation. The primary aim was to evaluate the effectiveness of IMPETUS-D training on reducing unplanned transfers to hospital and/or deaths in hospital among residents living with dementia. The study tested the hypothesis that nursing homes that participated in the IMPETUS-D training intervention would reduce the rate of unplanned transfers to hospital and or deaths in hospital among residents with dementia by 20% compared to the control nursing homes.
Methods
The trial was registered (ANZCTR: ACTRN12618002012257) and conducted according to a pre-defined published protocol to minimise potential biases, and subsequent deviations are reported [22]. Research methods and reporting were in accordance with the CONSORT 2010 statement: extension to cluster randomised trials [23]. Ethics approval was received by the Melbourne Health Human Research and Ethics Committee (HREC/17/MH/336).
Trial design
A multi-centre, cluster RCT design with an associated process evaluation was undertaken in Australia. Study sites were nursing homes (the clusters). A single private aged care provider managed all facilities. The study ran from December 2018 to October 2020. All nursing homes entered the study in December 2018 and baseline data collection commenced, staff from all the intervention nursing homes received access to the training intervention in early April 2019, the follow-up period commenced 1 October 2019 to 30 September 2020.
Participants and recruitment
The study involved 24 private nursing homes in Sydney, Melbourne and Adelaide, Australia. To be eligible for inclusion in the study, nursing homes had to have a minimum of 20 people with dementia living permanently in the care home and requiring high level care. All permanent care home residents with a recorded diagnosis of dementia were included.
People with dementia were defined as having a diagnosis of dementia if this was documented in residents’ nursing home files by a medical practitioner or nurse. Nurses and PCWs who worked at the nursing homes were recruited to participate, with additional promotion and information about the study provided face-to-face at staff meetings, and via flyers in staff rooms. Plain language statements were provided in hard copy and electronically to all potential staff participants, and consent was obtained from staff who participated in surveys and interviews. Participation in research activities and the training was voluntary.
Bereaved family members of residents with dementia who died during the follow-up period were invited to participate in a survey. The invitation was posted 6-8 weeks after the death of a resident. If no response was received, one follow-up phone call was made to check the survey had been received, to further explain the project and remind families to participate if they wished.
Intervention
The IMPETUS-D training program (intervention) was developed for the study by experts in simulation and healthcare worker education. The topics covered were informed by the best practice dementia and palliative care literature, the IMPETUS-D Project Working and Advisory Group, and input from key stakeholders including the end-users (personal care workers and nurses) and family carers. The program comprised 11 modules covering key aspects of best practice palliative and end-of-life care for people with dementia living in nursing homes (Table 1). Modules included case studies with short video scenarios filmed in authentic care home settings. These videos were used as the basis for questions to stimulate learning and practicing ‘what to say’ in different situations, for example, when family are worried about a resident not eating towards the end of life. The length of modules ranged from 15 to 45 mins.
The training could be accessed online via desktop computer, laptop, tablet, or smartphone. PCWs were expected to complete five core modules – Modules 1-3 and 10, and one symptom management module (Modules 6-9). The remaining modules were recommended. Nurses were expected to complete the two goals of care (GOC) modules and the communication module, and the remaining modules were recommended. As an incentive staff were paid the equivalent of three hours of their salary if they participated in the training outside their work hours, and other evidence-based strategies were used to promote staff participation (Table 2).
Control
Staff from nursing homes in the control group did not receive the IMPETUS-D training but had access to usual training opportunities.
Outcomes
Outcome measures pertain to the cluster or nursing home level. The primary outcome measure was the proportion of residents with dementia who had an unplanned hospital transfer and/or death in hospital during the 6-months follow up. Secondary outcomes measures were: hospital transfers or deaths in hospital over 12-months among residents with dementia, uptake of GOC plans over 6 and 12-months for residents with dementia, change in staff knowledge and attitudes about palliative care for people with dementia at 6 months follow up, and bereaved family satisfaction with care.
Randomisation and blinding
Randomisation was conducted at the level of the nursing home (cluster). The allocation sequence was generated by an independent statistician using a computer-generated allocation sequence. To ensure equal numbers of nursing homes per study arm, the randomisation used blocks of 4, stratified by city and facility size (small or large, based on the total number of residents). To preserve blinding, the randomisation list was stored and maintained in a secure location by the statistician who was independent from trial recruitment or training.
Data collection
Details of the data collection for outcome measures can be found in the protocol paper [22]. A dedicated study database was developed using the Research Electronic Data Capture (REDCap) tools hosted at the University of Melbourne [24]. Baseline resident demographic and clinical information, and follow-up resident-level outcomes (hospital transfers and deaths) were collected by project nurse consultants (not blinded to allocation) from the residents’ care home records or extracted from the provider’s database.
At baseline and 6-months follow-up, care home staff were invited to complete a survey which included demographic information and the Questionnaire on Palliative Care for Advanced Dementia (qPAD) [25]. The qPAD is a 2-part instrument consisting of a 23-item knowledge test and 12-item attitude scale. It was used to measure the secondary outcomes of staff knowledge and attitudes towards providing palliative dementia care. A total qPAD score (range 12-83) was derived by adding knowledge test (range 0-23) and attitude scale (range 12-60) scores; higher scores indicating better knowledge and more positive attitudes.
During the follow-up period, bereaved families’ perception of care was assessed using the Satisfaction With Care at the End-of-Life Dementia (SWC-EOLD) scale [26]. The SWC-EOLD assessed satisfaction with care during the last 90 days of life, and consisted of 10 items, each measured on a 4-point Likert scale defined as 1=strongly disagree, to 4=strongly agree. The total SWC-EOLD score was calculated by adding all 10 items (range 10-40); higher scores indicated greater satisfaction.
Sample size and power calculations
An a-priori sample size calculation was undertaken as per protocol [22]. The power analyses were based on the following assumptions: proportion of composite events (hospital transfer and/or death in hospital) of 0.65 and 0.85 over 6 months of follow-up in the intervention and control groups respectively, two-sided significance level of 0.05 (alpha). We estimated that 12 clusters (nursing homes) in each study arm, with 20 – 25 residents with dementia in each cluster, was needed with an Intra-Cluster Correlation (ICC) of 0.05. With these assumptions, the minimum power to observe a difference of proportion by 0.20 between the intervention and control group is 94%.
Statistical analysis
Descriptive statistics were used to summarise baseline care home and resident-level characteristics. Analyses of primary and secondary outcomes were on an intention to treat (ITT) basis, with the fundamental principles of analysing data from cluster RCTs followed. To compare the proportion of composite events for the primary outcome, logistic regression models were used with standard errors weighted by the cluster effects, clusters being the nursing homes. Estimated odds ratio (OR) and associated 95% confidence interval are presented, along with the p value for testing the hypothesis that the OR is 1. Total scores from the qPAD and SWC-EOLD were considered as a continuous variable. Mean scores were compared between the groups using mixed models which adjust for cluster effect. Statistical analyses were conducted in Stata MP version 15 [27]. All statistical tests were two-sided and the significance level was set at 0.05.
Process evaluation
Process evaluation was used to assess the implementation of the training intervention, to explore barriers and facilitators that influence implementation of the intervention, as well as the intervention mechanisms and outcomes, and was informed by the Medical Research Council (MRC) Process Evaluation of Complex Interventions [28] to guide the process evaluation and Consolidated Framework for Implementation Research (CFIR) [29, 30]. The CFIR provides a menu of constructs across five domains that have been associated with effective implementation. The CFIR domains of Inner setting, Intervention characteristics, and Characteristics of individuals, were used to explore participants’ experience, and barriers to participation, in addition to measures of staff participation and module completion (reach and dose) as described below.
The a-priori aim was for 80% of staff to complete the core modules for their discipline. This was amended during the training period to 50% of nurses in response to feedback from the provider and from staff that staff had other mandated training occurring at the same time. Data on the number of staff who participated in the training, the number of modules, and the number of core modules commenced and completed was collected from the learning management system (LMS) and from attendance records at each face-to-face training session.
Data on participants’ experience and satisfaction with the intervention was collected from feedback items at the end of each module, and at 6-month follow-up staff interviews and follow-up staff surveys. Data from the research team notes and log of activities, informal feedback from staff, follow-up staff surveys, and staff interviews was used to identify factors that may have influenced reach, dose, participant satisfaction and barriers to participation.
Qualitative data from the surveys and interviews were imported from Microsoft Excel and Microsoft Word files into NVivo 12 for coding [31]. Data was analysed by the research team and key themes identified based on anticipated and emergent themes [32]. An iterative process was used, with coding trees and summarised data presented to members of the IMPETUS-D Project Working and Advisory Group for review and input.
Results
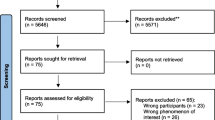
Of the 44 nursing homes, 27 were eligible for inclusion. To obtain balance across locations and size, 24 nursing homes were randomised into the intervention or control group (Fig. 1). All 24 agreed to participate in the study, and all remained involved in the study throughout the project timeline.
Residents with dementia
At baseline, among all residents living in the 24 nursing homes 1304 (59.8%) had a diagnosis of dementia recorded; 608 in the intervention nursing homes and 696 in the control nursing homes. Demographic and clinical data of residents with dementia were similar for those living in the intervention and control homes, except more residents from the intervention group had an advance care directive (ACD) in place (Table 3).
Unplanned hospital transfers and deaths in hospital are shown in Table 4. During 6-months follow-up, a total of 260 (19.9%) residents with dementia from all care homes had at least one unplanned hospital transfer; 128 (21.1%) in the intervention and 132 (19.0%) in the control group. Analysis of the primary outcome (proportion of hospital transfers or deaths in hospital among residents with dementia over 6 months) yielded an odds ratio of 1.14 (95% CI, 0.82-1.59), p = 0.44. Overall, 154 residents died during 6-months, 75 (12.3%) from the intervention and 79 (11.4%) from the control group.
During 12-months follow-up, 407 (31.2%) residents with dementia had at least one unplanned transfer to hospital, 201 (33.1%) from the intervention and 206 (29.6%) from the control group (odds ratio 1.17; 95% CI, 0.84-1.63); and 310 (23.8%) residents died, 154 (25.3%) from the intervention and 156 (22.4%) from the control group.
Two of the core nursing modules focused on GOC discussions and documenting GOC medical treatment plans [33]. A new GOC form was introduced in the module and all senior nurses and general managers were sent a copy of the form. However, there was no uptake of the form which relied on a doctor for completion. This was despite general practitioners being sent information about the forms.
Staff knowledge and attitudes
A total of 330 staff completed the follow-up qPAD, 122 from the intervention and 208 from the control nursing homes. Staff from both groups were similar in terms of sex, age, position, years’ of aged care experience, hours worked per week, and highest level of education. (Appendix 1). Among them, 218 staff completed both baseline and follow-up qPAD, 96 from the intervention and 122 from control nursing homes.
There was no significant between-group difference in total qPAD scores; intervention group mean score=60.1 (95% CI 57.4-62.8) compared to the control group mean score=59.5 (95% CI 57.2-61.8), p = 0.77. Most of the variability was contributed by individuals (93%) not nursing homes (7%) indicating clustering did not have a big effect on scores. Similarly, when baseline scores were accounted for, there was no significant between-group difference in total qPAD scores; adjusted intervention group mean score=61.1 and control group mean score=60.0 (p = 0.53).
Bereaved carer survey
A total of 72 of 258 bereaved carer surveys were received over 12-months. At the request of the provider, surveys were not sent if nursing homes had experienced COVID outbreaks or if coroner’s investigation was underway. There were no significant between group differences in mean SWC-EOLD scores, with mean scores of 26.6 in the intervention and 27.0 in the control group, p = 0.80. Most of the variability was contributed by individuals (87%) not nursing homes (13%) demonstrating that clustering did not have had a big effect on SWC-EOLD score.
Process evaluation findings
Fidelity
The IMPETUS-D program was largely implemented as intended, with all planned implementation strategies completed in full or in part. Due to low uptake of the online modules and feedback from staff, the training period was extended from 2 months as originally planned to 6 months, and face-to-face training sessions were held by members of the research team and the project consultant nurses at each of the intervention sites to boost training participation. The IMPETUS-D Project Working and Advisory Group decided the priority was to maximise staff participation. Although the mode of delivery of the IMPETUS-D intervention was modified, the module content was not altered and the online modules were projected on a screen or on multiple laptops for group learning.
Reach and dose
During the 6-month training period 42 (4.3%) staff completed their core modules, 27 (3.7%) PCWs and 15 (6.0%) nurses. None of the nursing homes achieved the aim of 50% of nurses completing core modules. The three nursing homes with the highest proportion of nurses completing core modules were 24% (care home 9), 21% (care home 4) and 15% (care home 3) (Fig. 2).
Overall, 251 (26%) staff completed at least one module during the training period, 79 nurses and 172 PCWs. One hundred sixty staff attended the face-to-face sessions, and 102 participated in the training online, with some staff completing modules both online and at face-to-face sessions. The proportion of staff from each care home who participated in the training ranged from 15 to 53%.
Staff satisfaction with the training
Among the 103 follow-up survey respondents who had done the training, 61 (59%) agreed that completing the modules increased their confidence in looking after residents with dementia, 12 (12%) did not agree or were unsure and 30 (29%) did not respond. The reasons staff gave for not participating in the training included: 25% were unable to attend the session, 17% were not aware of the training, 16% had technical issues accessing the training online, and 15% did not have time.
Barriers to participation
The CFIR was used to guide the thematic analysis of the qualitative interview and survey data [30]. Barriers were categorized according to the following three CFIR domains and their associated constructs – (i) Inner setting (the organisation of the care home), (ii) Intervention characteristics, and (iii) Characteristics of individuals. Examples of quotes from the interviews and survey data on main barriers (according to CFIR constructs) to staff participation have been presented in Table 5.
One of the main barriers to staff participation was having competing priorities that occurred at the same time as the IMPETUS-D program was implemented, specifically the introduction of the National Aged Care Standards and the Royal Commission into Aged Care Quality and Safety. Staff were expected to attend training in preparation for the new standards, and many had additional administrative work in relation to the new standards and the Royal Commission, and these activities took time and the focus away from IMPETUS-D. These barriers relate to the CFIR constructs of relative priority (standards took priority over IMPETUS-D training) and available resources (staff not having adequate or dedicated time and resources to do the training). In addition, there were organisational and nursing home level barriers, that affected implementation including variable leadership engagement, intra-organisational communication, turnover of care home management and senior nurse roles at 50% of intervention homes (stability of the team), and time constraints and disruption to schedule. Some characteristics of the training intervention itself were also reported as potential barriers to implementation including the online and individual learning approach, the use of a separate LMS rather than the organisation’s LMS that staff were familiar with, complexity of the intervention with multiple modules, targeting multiple disciplines, and that the training was not mandatory.
Discussion
The IMPETUS-D simulation-based staff training program on quality palliative and end-of-life care in dementia had no effect on hospital transfers and deaths in hospital of nursing home residents with dementia, staff knowledge and attitudes, or bereaved family satisfaction with care. Implementation of the intervention was suboptimal with only 26% of staff participating in the program.
Comparison with other studies
Our systematic review of five controlled studies found there is a lack of evidence to support simulation training in non-cancer palliative care for healthcare workers [21]. Improvements in staff communication skills, knowledge acquisition and attitudes towards death and comfort were reported in three studies, but these studies had several methodological limitations. Further, one good quality RCT was unable to show any change in clinician practice or patient outcomes. The variability of these findings highlighted the need for more rigorous research to evaluate the effect of simulation training in this clinical field, including studies to establish optimal duration and types of simulation applications, and the impact of training interventions on practice change and patient outcomes.
Two recent cluster RCTs have evaluated palliative care training programs in nursing homes [34, 35]. However, these studies did not focus on dementia-specific palliative care. The European multi-country PACE study assessed an intervention that used a train-the-trainer approach to integrate non-specialist palliative care in 37 nursing homes compared to 36 controls [35]. They were unable to show improvements in residents’ comfort at end-of-life, and despite improvements in intervention staff knowledge compared to the controls, the difference was not clinically relevant. The process evaluation found high variability in the implementation of the intervention, and reported the main reasons related to the program itself and its delivery, the PACE trainer, and organisational issues [36]. This study, like the IMPETUS-D study did not have effective implementation of the intervention.
The study by Lamppu et al. (2021) assessed the effectiveness of staff training in palliative and end-of-life care in 20 Helsinki nursing homes [34]. The intervention training was based on a palliative care training-needs survey and this likely contributed to the high participation rates (74%). However, they were unable to show any between-group differences in residents’ health-related quality-of-life, hospital admissions or emergency presentations. They attributed the null findings to potential poor selection of quality-of-life instrument, lower than expected deaths, and different learning needs of professions; and concluded that training interventions alone might be insufficient to produce improvements in practice or outcomes.
Both these studies were unable to show the training led to improvements in resident outcomes. Further studies may need to incorporate interventions beyond education alone to impact on staff practice change and improve resident and family carer outcomes. There is some evidence to suggest use of staff training in combination with follow-up expert consultation [37] or supervision sessions to help staff incorporate strategies into practice [38], but this has not been well established for staff training in aged care or dementia-specific palliative care.
Strengths and limitations
Strengths of the IMPETUS-D study include its large sample size. multi-site design and use of an innovative simulation-enhanced program about the specific palliative care needs of people with dementia. All 24 nursing homes recruited to the study, participated in the research and all intervention nursing homes participated in the training. However, there were several study limitations.
Despite use of evidence-based implementation strategies, the degree of staff participation was lower than expected and a key limitation to this study. One of the biggest issues was the timing of the implementation of the intervention. It was unfortunate that the training was implemented at the same time as major changes in the national aged care standards were introduced and these took priority. Despite nursing homes being aware of the new standards, they were not prepared for the amount of additional training and administrative work it entailed. Several other barriers to IMPETUS-D uptake were identified and related to staff (turnover and high workload), organisational or inner setting factors (lack of time, communication, scheduling disruptions), and the characteristics of the training intervention (technical issues, its voluntary nature, complexity and design quality). Strategies such as having the IMPETUS-D training integrated into the organisation’s training schedule and available on the organisation’s learning management system, or implementing a more simplified version such as targeting only nurses or implementing it in a stepped approach may have helped overcome some of these barriers and increased uptake. However, many of these challenges have been reported in other nursing home-based studies [39, 40], and highlight the need for future research to evaluate the effect of strategies to address common barriers.
A pilot intervention phase was not undertaken due to time and resource constraints. This may have aided identification of modifiable barriers to participation and strategies to overcome these barriers could have been put in place. However, a pilot phase may not have mitigated unexpected system changes which were beyond researcher control. Further, the investigators considered that the bespoke design of the training package and high-level stakeholder buy-in and engagement with the training package with all homes being managed by the same private aged care provider would support staff access to and uptake of training. Unfortunately, in this study, this was not sufficient in and of itself to ensure staff participation and further research is needed to better understand nursing home context specific barriers and strategies to overcome these.
This study set out to evaluate the effectiveness of the IMPETUS-D intervention, but without sufficient staff participation (implementation failure), we were unable to establish the true effect of the training on staff knowledge, practice, and resident outcomes. Future work in this area might benefit from a more detailed assessment of individual care homes’ readiness to implement the training with input from general managers, nurses, PCWs, residents, and their families. This information could then be used to target care homes that are ready to implement the training, and to inform the research or implementation team on how best to support implementation, based on the local needs.
Conclusion
Our study of a staff training program on palliative dementia care was unable to show any differences in hospital transfers or staff knowledge and attitudes. Staff participation was lower than expected and highlighted the need to ensure nursing homes are ready to implement the intervention. Training programs for nursing home staff are important and necessary as the population ages and the prevalence of dementia increases. Further research is warranted to assess the impact of a more simplified and sustainable version of the IMPETUS-D training intervention, for example by assessing a smaller number of modules and targeting fewer staff groups; and to establish facilitation strategies that work to increase staff participation and successfully influence implementation.
Availability of data and materials
Data will be available after analyses is finalised and report / publication has been submitted and approved. Unidentifiable individual participant data and related data dictionaries will be available. Access is subject to approval by the Principal Investigator Professor Wen Kwang Lim.
Abbreviations
- ACD:
-
Advance care directive
- ACFI:
-
Aged Care Funding Instrument
- ANZCTR:
-
Australia and New Zealand Clinical Trial Register
- CFIR:
-
Consolidated Framework for Implementation Research
- GOC:
-
Goals of Care
- HREC:
-
Human Research and Ethics Committee
- ICC:
-
Intra-Cluster Correlation
- IMPETUS-D:
-
IMproving Palliative care Education and Training Using Simulation in Dementia
- ITT:
-
Intention to treat
- LMS:
-
Learning management system
- OR:
-
Odds ratio
- PCWs:
-
Personal care workers
- RCT:
-
Randomised controlled trial
References
Bernstein Sideman A, Harrison KL, Garrett SB, Naasan G, Ritchie CS. Practices, challenges, and opportunities when addressing the palliative care needs of people living with dementia: Specialty memory care provider perspectives. Alzheimers Dement. 2021;7(1):e12144. https://doi.org/10.1002/trc2.12144.
Dementia Australia. Palliative care and dementia. Dementia Australia paper number 43. 2018. [Accessed 20 Oct 2021]. Available from: https://www.dementia.org.au/sites/default/files/documents/Dementia-Australia-Numbered-Publication-43.pdf.
Palliative Care Australia and Alzheimer's Australia. End of life care for people with dementia. Survey report 2014. 2014.
Sampson EL. Palliative care for people with dementia. Br Med Bull. 2010;96:159–74. https://doi.org/10.1093/bmb/ldq024.
van der Steen JT, Radbruch L, Hertogh CM, et al. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. 2014;28(3):197–209. https://doi.org/10.1177/0269216313493685.
Australian Institute of Health and Welfare. Interfaces between aged care and health systems in Australia—where do older Australians die? 2021 [29 July 2021]. Available from: https://www.aihw.gov.au/reports/aged-care/where-do-older-australians-die/summary.
Martinsson L, Lundstrom S, Sundelof J. Quality of end-of-life care in patients with dementia compared to patients with cancer: a population-based register study. PLoS One. 2018;13(7):e0201051. https://doi.org/10.1371/journal.pone.0201051.
Mitchell SL, Kiely DK, Hamel MB. Dying with advanced dementia in the nursing home. Arch Intern Med. 2004;164(3):321–6. https://doi.org/10.1001/archinte.164.3.321.
Commonwealth of Australia. Royal commission into aged care quality and safety. Final report: care, dignity and respect. Volume 1. Summary and recommendations. 2021.
Worldwide Hospice Palliative Care Alliance (WHPCA). Palliative care and dementia statement - worldwide hospice palliative care alliance. 2015 [9 Aug 2019]. Available from: https://www.who.int/mental_health/neurology/dementia/NSA_WHPCA.pdf.
Chang E, Daly J, Johnson A, et al. Challenges for professional care of advanced dementia. Int J Nurs Pract. 2009;15(1):41–7. https://doi.org/10.1111/j.1440-172X.2008.01723.x.
Arcand M, Monette J, Monette M, et al. Educating nursing home staff about the progression of dementia and the comfort care option: impact on family satisfaction with end-of-life care. J Am Med Dir Assoc. 2009;10(1):50–5. https://doi.org/10.1016/j.jamda.2008.07.008.
Caplan GA, Meller A, Squires B, Chan S, Willet W. Advance care planning and hospital in the nursing home. Age Ageing. 2006;35:581–5.
Di Giulio P, Finetti S, Giunco F, et al. The impact of Nursing Homes staff education on end-of-life care in residents with advanced dementia: a quality improvement study. J Pain Symptom Manag. 2018. https://doi.org/10.1016/j.jpainsymman.2018.10.268.
Kortes-Miller K, Jones-Bonofiglio K, Hendrickson S, Kelley ML. Dying with Carolyn: using simulation to improve communication skills of unregulated care providers working in long-term care. J Appl Gerontol. 2016;35(12):1259–78. https://doi.org/10.1177/0733464815577139.
Livingston G, Lewis-Holmes E, Pitfield C, et al. Improving the end-of-life for people with dementia living in a care home: an intervention study. Int Psychogeriatr. 2013;25(11):1849–58. https://doi.org/10.1017/S1041610213001221.
Verreault R, Arcand M, Misson L, et al. Quasi-experimental evaluation of a multifaceted intervention to improve quality of end-of-life care and quality of dying for patients with advanced dementia in long-term care institutions. Palliat Med. 2018;32(3):613–21. https://doi.org/10.1177/0269216317719588.
Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–88. https://doi.org/10.1001/jama.2011.1234.
Kyaw BM, Saxena N, Posadzki P, et al. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res. 2019;21(1):e12959. https://doi.org/10.2196/12959.
Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28(8):1078–89. https://doi.org/10.1007/s11606-012-2264-5.
Tropea J, Bicknell R, Nestel D, et al. Simulation training in non-cancer palliative care for healthcare workers: a systematic review of controlled studies. BMJ Simul Technol Enhanced Learn. 2021;7(4):262–9. https://doi.org/10.1136/bmjstel-2019-000570.
Tropea J, Johnson CE, Nestel D, et al. A screen-based simulation training program to improve palliative care of people with advanced dementia living in residential aged care facilities and reduce hospital transfers: study protocol for the IMproving Palliative care Education and Training Using Simulation in Dementia (IMPETUS-D) cluster randomised controlled trial. BMC Palliat Care. 2019;18(1):86. https://doi.org/10.1186/s12904-019-0474-x.
Campbell MK, Piaggio G, Elbourne DR, Altman DG, Group C. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661. https://doi.org/10.1136/bmj.e5661.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Long CO, Sowell EJ, Hess RK, Alonzo TR. Development of the questionnaire on palliative care for advanced dementia (qPAD). Am J Alzheimers Dis Other Dement. 2012;27(7):537–43. https://doi.org/10.1177/1533317512459793.
Kiely DK, Volicer L, Teno J, Jones RN, Prigerson HG, Mitchell SL. The validity and reliability of scales for the evaluation of end-of-life care in advanced dementia. Alzheimer Dis Assoc Disord. 2006;20(3):176–81. https://doi.org/10.1097/00002093-200607000-00009.
StataCorp. Stata statistical software: release 15. College Station: StataCorp LLC; 2017.
Moore G, Audrey S, Barker M, et al. Process evaluation of complex interventions. UK Medical Research Council (MRC) guidance. 2015. [Accessed 20 Aug 2021]. Available from: https://mrc.ukri.org/documents/pdf/mrc-phsrn-process-evaluation-guidance-final/.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50.
CFIR Research Team-Center for Clinical Management Research. Consolidated framework for implementation research. 2021 [08 Oct 2021]. Available from: https://cfirguide.org/.
NVivo qualitative data analysis Software; QSR International Pty Ltd. Version 12 2018.
Liamputtong P. Research methods in health: foundations for evidence based practice; 2013.
Martin RS, Hayes BJ, Hutchinson A, Tacey M, Yates P, Lim WK. Introducing goals of patient care in residential aged care facilities to decrease hospitalization: a cluster randomized controlled trial. J Am Med Dir Assoc. 2019;20(10):1318–1324.e2. https://doi.org/10.1016/j.jamda.2019.06.017.
Lamppu PJ, Finne-Soveri H, Kautiainen H, Laakkonen ML, Laurila JV, Pitkala KH. Effects of staff training on nursing home residents’ end-of-life care: a randomized controlled trial. J Am Med Dir Assoc. 2021. https://doi.org/10.1016/j.jamda.2021.05.019.
Van den Block L, Honinx E, Pivodic L, et al. Evaluation of a palliative care program for nursing homes in 7 countries: The PACE cluster-randomized clinical trial. JAMA Intern Med. 2020;180(2):233–42. https://doi.org/10.1001/jamainternmed.2019.5349.
Oosterveld-Vlug M, Onwuteaka-Philipsen B, Ten Koppel M, et al. Evaluating the implementation of the PACE steps to success programme in long-term care facilities in seven countries according to the RE-AIM framework. Implement Sci. 2019;14(1):107. https://doi.org/10.1186/s13012-019-0953-8.
Lamppu PJ, Pitkala KH. Staff training interventions to improve end-of-life care of nursing home residents: a systematic review. J Am Med Dir Assoc. 2021;22(2):268–78. https://doi.org/10.1016/j.jamda.2020.09.011.
Spector A, Orrell M, Goyder J. A systematic review of staff training interventions to reduce the behavioural and psychological symptoms of dementia. Ageing Res Rev. 2013;12(1):354–64. https://doi.org/10.1016/j.arr.2012.06.005.
Lam HR, Chow S, Taylor K, et al. Challenges of conducting research in long-term care facilities: a systematic review. BMC Geriatr. 2018;18(1):242. https://doi.org/10.1186/s12877-018-0934-9.
Low LF, Fletcher J, Goodenough B, et al. A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLoS One. 2015;10(11):e0140711. https://doi.org/10.1371/journal.pone.0140711.
Acknowledgements
The authors acknowledge the IMPETUS-D Working Group and Steering Committee, including Lee-Anne Henley, Liz Reymond, Stephen Wiblin, Margaret Winbolt, David Currow, Robyn Smith, Anita Goh, and Lyn Franco. Special thanks to Marg Ryan, Arlene Nunez, Gurleen Kaur, Amanda Smith, Kristine Min and all the staff and family participants.
Funding
This work was supported by funding from the Australian Government Department of Health under the Dementia and Aged Care Services Grant Opportunity 1. The funders did not have any input in the study design, analysis, or manuscript development. Joanne Tropea received a Melbourne Ageing Research Collaboration (MARC) PhD scholarship.
Author information
Authors and Affiliations
Contributions
JT wrote the main manuscript, JT and GH conducted the statistical analysis, and JT, CAB and BJH contributed to the analysis of the qualitative data. CEJ, DN, BJH, WKL, RB and JT developed the training intervention. All authors contributed design of the evaluation and the interpretation of findings and reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was received by the Melbourne Health Human Research and Ethics Committee (HREC/17/MH/336). All methods were performed in accordance with the National Statement of Ethical Conduct in Research Involving Humans, and the research arrangements of the organisations involved. Consent for participation in IMPETUS-D and the associated evaluation was conducted at the facility or group level. Consent from individuals living in the residential aged care facilities has been waived, as it was deemed unnecessary by the Melbourne Health Human Research and Ethics Committee. Individual consent from residential aged care staff who participated in the research was sought. Invitations to participate in the bereaved family carer survey and information about the project was provided to family members, and completion and return of the survey implied consent.
Patient safety
The number of deaths and hospital transfers was monitored in the control and intervention groups. The plain language statements included contact details of the principal investigator, project coordinator and the ethics committee that participants can contact in the event of a complaint or concern about the project. Any reported issues, adverse events and other unintended effects of the trial intervention were reported to the IMPETUS-D Project Working and Advisory Group and the IMPETUS-D Steering Committee.
Study management and oversight
This study was managed by the IMPETUS-D Project Working and Advisory Group, consisting of the principal investigator, co-investigators and representation from the aged care home provider. The IMPETUS-D Steering Committee with members from stakeholder groups provided additional governance oversight for the study monitoring.
Written 6-monthly progress reports were submitted to the funding body and annual progress reports submitted to the Melbourne Health ethics committee throughout the project timeline.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Characteristics and qPAD scores of staff who completed the follow-up survey (N=330)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tropea, J., Nestel, D., Johnson, C. et al. Evaluation of IMproving Palliative care Education and Training Using Simulation in Dementia (IMPETUS-D) a staff simulation training intervention to improve palliative care of people with advanced dementia living in nursing homes: a cluster randomised controlled trial. BMC Geriatr 22, 127 (2022). https://doi.org/10.1186/s12877-022-02809-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-02809-x