Abstract
Background
Clinical studies indicate that strength-balance training for active fall prevention can prevent fractures in older people. The present modelling study evaluates the cost-effectiveness of fall prevention exercise (FPE) provided to independently living older people compared to no intervention in Germany.
Method
We designed a Markov model to evaluate the cost-effectiveness of a group-based FPE-program provided to independently living people ≥75 years from the perspective of the German statutory health insurance (SHI). Input data was obtained from public databases, clinical trials and official statistics. The incremental cost-effectiveness ratio (ICER) was presented as costs per avoided hip fracture. Additionally, we performed deterministic and probabilistic sensitivity analyses and, estimated monetary consequences for the SHI in a budget impact analysis (BIA).
Results
For women, the costs per hip fracture avoided amounted to €52,864 (men: €169,805). Results of deterministic and probabilistic sensitivity analyses confirmed the robustness of the results. According to the BIA, for the reimbursement of FPE additional costs of €3.0 million (women) and €7.8 million (men) are expected for the SHI.
Conclusions
Group-based FPE appears to be no cost-effective option to prevent fall-related hip fractures in independently living elderly. To allow a more comprehensive statement on the cost effectiveness of FPE fracture types other than hip should be increasingly evaluated in clinical trials.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
An increased risk of fall in higher age (i.e., > 75), is associated with both physical and mental restrictions for the affected individuals and, may result in premature death [1,2,3]. Falls can result in fractures at different sites, with proximal femur, pelvis, distal radius ankle and proximal humerus diagnosed most often in individuals aged between 70 and 89 years [4]. Fall-related fractures have significant socioeconomic consequences for both patients and the society. Particularly, hip fractures can lead to a substantial loss of healthy life-years in elderly people [5]. In the European Union, the costs of fall-related hip fractures, which are more than 90% of all hip fractures [6] amounted to €20 billion in 2010 [7, 8]. Particularly, elderly people with low bone density are at increased risk of hip fracture. Due to demographic changes, in the European Union, the number of osteoporosis-associated hip fractures is expected to increase from 615,000 in 2010 to 815,000 in 2050 (+ 32%) [8].
Among various measures to prevent falls and fall-related fractures, exercise is based on the knowledge that physical inactivity in older age increases the likelihood of suffering a fall-related fracture [9]. For the mode of action of exercise different mechanisms are discussed: exercise can prevent fractures from falls by improving balance and muscle strength, but also by strengthening muscles and/or increasing bone mineral density [10]. Therefore, for fall prevention exercises (FPE) it is recommended to include different modules of exercises such as improving balance with the addition of strength training and/or walking [11]. In addition, FPE should be carried out on a regular basis [11]. Structured, commonly used FPE programs are the Falls Management Exercise Program (FaME) and the Otago Exercise Program (OEP) [12].
Whereas high-level evidence for preventive measures is often difficult to achieve, FPE provided to elderly in community-based settings has been shown to be effective in reducing falls and fall-related fractures [11, 13, 14]. In addition, by providing group-based FPE many individuals can be targeted simultaneously.
Different cost-effectiveness analyses of exercise for fall prevention in different settings have been published, ranging from economic evaluations alongside clinical trials to modelling studies [15,16,17,18,19]. However, only few studies evaluated group-based FPE as a single intervention for community-dwelling elderly with regard to long-term consequences [15, 19, 20].
The objective of this analysis was to evaluate the cost-effectiveness (i.e., the costs per hip fracture avoided) of group-based FPE for elderly persons without care need compared to no intervention from the perspective of the German statutory health insurance (SHI). Furthermore, we estimated the monetary consequences of reimbursing such a program for the SHI.
Methods
We performed a cost-effectiveness analysis with a Markov-based simulation using TreeAge Pro© (TreeAge Software, Williamstown, Massachusetts). The model cohort, i.e. community-dwelling older people at average risk of hip fracture, entered the model at the age of 75 and was tracked for 25 years up to the age of 100 years. This age was chosen due to a lack of public data on German women and men older than 100 years. The chosen cycle length was 6 months because hip fractures are often followed by a re-fracture, nursing home admission or death within the first months post-fracture [21, 22].
For input data on clinical parameters and costs, different literature searches were performed in bibliographic databases (e.g., Medline) and public sources (e.g., Federal Statistical Office of Germany). Finally, most of the data for populating the model were based on German sources, supplemented by studies from other European countries. The appropriateness of the data applied for the model was checked by clinical experts. The primary outcome of this analysis was the incremental costs per avoided hip fracture. The cost-effectiveness-analysis was limited to hip fractures because these are expected to have the largest socioeconomic impact. In addition, fractures other than hip were often not reported in clinical trials [23].
Overview of the model structure
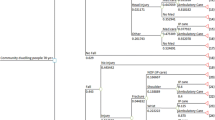
Our analysis was based on a previous Markov-model developed for a cost-utility-analysis of a home-safety intervention for older people in need of care [24]. The model included six health states: “well”, “hip fracture”, “post-fracture”, “nursing home”, “re-fracture in nursing home” and “death”. Women/men entered the model in the state “prior first hip fracture”, could remain in this state, suffer a hip fracture or die. (Note: deaths related to a hip fracture or occurring in the nursing home are considered separately in the further progress of the model.) If a first hip fracture occurs, subjects can return to home (state “post-fracture”), be admitted to nursing home (state “nursing home”), suffer a re-fracture or die. In case of a re-fracture, patients remain in the state “hip fracture”. Transitions to nursing home due to hip fracture were assumed only to occur in the first cycle after a hip fracture (compare Fig. 1). When admitted to nursing home, patients could stay in nursing home, suffer a re-fracture of the hip, or die.
Transition state Markov model for the base-case analysis [24]. Abbreviations. Non-inst.: non-institutionalized
Intervention
Among the several concepts for offering an FPE-program, two types are recommended: individualized home-based training and group-based exercises, both of them including strength- and balance-training [11]. Because of the group-based nature of most commercial FPEs in Germany, for our model a standardized group exercise was applied. We assumed FPE to be provided on a weekly basis, corresponding to the intervention frequency from an offer of a German hospital [25]. In accordance with similar studies, the program was assumed to include 24 one-hour sessions [12, 26]. In these sessions, the participants were assumed to receive different exercises and, specific guidance how to practice the exercises at home.
Clinical input data
Data on hip fracture rates were derived from a large claim data set from Southern Germany. In that analysis, incidences of femoral fractures (ICD-Code S72) in different care settings were analysed [27]. Hip fracture rates for the model population were calculated by limiting the number of femoral fractures to hip fractures, which were assumed to be 84% of all femoral fractures (i.e. ICD-Code S72.0-S72.2), and, by subtracting the proportion of fractures not resulting from a fall [28,29,30]. Risks of a re-fracture were taken from a large Danish population-based cohort study [22]. This study revealed a substantial increased relative risk of a re-fracture, which realigned within 20 years of follow-up. We applied these re-fracture risks also to individuals admitted to nursing home because of a lack of evidence for this subgroup.
Rates of nursing home admission after hip fracture were taken from insurance data reflecting community-dwelling people with a hospital admission or discharge diagnosis of a hip fracture (S72.0-S72.2) [21].
Data on mortality in the “prior first hip fracture”-state were taken from the Federal Statistical Office of Germany [31]. Both the increased short-term mortality in the first cycle after a hip fracture (state “hip fracture”) [21] and the increased long-term mortality after returning home (state “post-fracture”) was taken into account [32]. Data on short-term and long-term mortality after nursing home admission were taken from claims reflecting German nursing home residents [33] (Table 1).
A recent Cochrane review showed FPE to be effective in elderly people living without care in the community for the prevention of fractures [23]. The risk ratio (RR) of suffering at least one fracture was 0.73 [95% Confidence interval (CI): 0.56 to 0.95] compared to standard care or no intervention [23]. For our analysis, we adjusted this risk reduction for inadequate compliance (i.e., conforming to the recommendations) and non-persistence (i.e., conforming to a recommendation of continuing treatment for the prescribed length of time) [38]. Because some individuals may reject the offer of group exercise the intervention effect was reduced in accordance with the number of participants not taking part in the intervention [23, 28].
In order to take into account non-persistence, we calculated a proportional effect decrease of 28% annually [23, 39]. As a result, after 4 years the effect of the FPE was assumed to be zero.
Cost data
In accordance to the SHI-perspective, we included the costs of FPE, those of hip-fracture-related treatment and nursing. The costs assumed for the provision of FPE were in line with the requirements for fall prophylaxis training as defined by SHI, i.e., participants pay registration fees in advance and will receive up to 80% of the costs back by the SHI in case of regular participation [25, 40, 41]. Similar to the decreasing effect of the intervention, a yearly reduction of costs due to decreasing compliance and persistence was assumed (Table 2).
In order to take into account hip-fracture-related home care needs, the corresponding costs were estimated based on different care level rates [29, 42, 54]. For patients returning to home after a hip fracture, we assumed an increase of average care dependency of 9% in the age-group of 75–79 years and an increase of 22% in older age-groups [36]. Costs due to nursing home admission were calculated based on long-term care insurance statistics and the benefit claims per level of care (Table 2) [28, 54]. A nursing home admission was assumed to be irreversible (i.e., short-term stays were not considered).
Costs of hip fracture treatment include costs of inpatient treatment, outpatient treatment and rehabilitation. Data on surgical procedures for hip fracture treatment were taken from published evidence (S72.0-S72.2) [42]. The corresponding amounts of reimbursement to German hospitals were calculated with a freely available DRG-grouper [43]. Costs for inpatient rehabilitation were estimated on SHI statistics [46,47,48] while outpatient care costs were recalculated from a German cost-utility analysis [50]. Details on cost categories and calculation can be found in the appendix (Table A1 and A2).
Costs were reported in Euro (€). If costs occurred earlier than 2019, we adjusted for inflation (Table 2) [49].
Sensitivity analysis
We performed different sensitivity analyses with regard to input data and the model structure. For cost data, ranges of 40% as suggested by Briggs were used (except for the intervention costs, where we assumed a range of 50%) [55]. For transition probabilities without a 95%-CI, we used ranges of +/− 20%. For the effect measure, we used the 95%-CI.
Additionally, best- and worst-case analyses were applied. Best-case analysis included the lowest intervention costs and highest costs of treatment and nursing care post-fracture as well as the lower bound of the 95%-CI of the effect measure. In contrast, in the worst-case analysis we applied the highest intervention cost and, the lowest costs of treatment and nursing care costs post fracture as well as the upper bound of the 95%-CI of the effect measure.
Using appropriate distributions for each parameter, a Monte Carlo simulation with 10,000 iterations was performed to quantify the uncertainty of the input parameters. Distribution parameters were calculated from available 95%-CIs or from assumed standard deviations [55]. Treatment and nursing home costs were calculated independent on age, while costs of outpatient care and intervention costs were calculated for each age group. Results of the Monte Carlo simulation were presented as cost-effectiveness acceptability curves.
With regard to the chosen decision model, two structural sensitivity analyses were performed. In the structural analysis I, we added a transition for admissions to nursing home due to other reasons than hip fractures (i.e., from the “healthy” and the “post-fracture” state) [56]. In the structural analysis II, two health states for reflecting the economic impact of vertebral fractures were added (resulting in a ratio ‘costs per hip or vertebral fracture avoided’) [57, 58]. Illustrations of model structures and details on additional input parameters can be found in the appendix (figure A1 and A2, Table A7 and A8).
Budget impact analysis
Furthermore, we calculated the budget impact of a nationwide implementation of the training program for the German SHI. In order to calculate this budget impact analysis (BIA), the incremental costs were extrapolated with the number of independently living individuals based on their remaining life expectancy [29, 59]. Results are reported as annual costs for the SHI.
Results
For women aged 75, the provision of FPE resulted in an ICER of 52,864 € per hip fracture avoided. For men at this age, the ICER was €169,805 per hip fracture avoided (Table 3). FPE decreased the number of nursing home admissions due to hip fractures (0.02% for women and 0.01% for men) (Table 3).
Sensitivity analysis
For both women and men the efficacy of FPE had the highest impact on the result, followed by the intervention costs. When varying the efficacy of FPE, the costs of the intervention or, the fracture rates, for men the impact on the ICER was substantially higher than for women (see appendix, figure A3 and A4). Assuming a best-case scenario, for women FPE was dominating (i.e., less costly and more effective) compared to no FPE.
Assumed a willingness to pay (WTP) of zero, the probabilistic sensitivity analysis showed a probability of 47% for FPE being cost-effective in women. The probability increased to 57% at a WTP of 200,000€. For men, the probability of cost-effectiveness starts at 42% at a WTP of zero and amounts to 50% at a WTP of about €500,000 (Fig. 2).
Incorporation of additional transitions to nursing home unrelated to hip fractures (structural sensitivity analysis I) increased the ICER by €7000 (13%) for women. For the men there was an increase of about €2400 (1%) on the ICER. The inclusion of vertebral fractures in the model (structural sensitivity analysis II) decreased the ICER by 12% (€6200) for women and by 54% (€91,000) for men (see appendix, Table A9).
The budget impact analysis showed that the provision of FPE to independently living community-dwelling adults aged 75 ≤ would be associated with annual costs of €3 Million (Mio) for women and €7.8 Mio for men.
Discussion
Summary of the main results
According to the results of this cost-effectiveness analysis group-based FPE for independently living older people cannot be considered as cost-effective. The provision of a FPE program revealed a cost-effectiveness ratio of €52,864 (women) and €169,805 (men), respectively. FPE provided for independently living people ≥75 years would result in additional costs of about €11 Mio for the German SHI. In order to achieve a probability of cost-effectiveness of at least 50%, the WTP had to be €100.000 for women and €200.000 for men. However, a structural sensitivity analysis indicated that the cost-effectiveness ratios for FPE would be more favourable when vertebral fractures (or other type of fractures) would be considered.
The unfavourable cost-effectiveness ratios of group-based FPE can be explained by three reasons: first, the low hip fracture rates in the population of independently living people (seven per 1000 women and four per 1000 men) [27]. Second, a conservative assumption for the data on efficacy of FPE by assuming a continuous decrease due to non-compliance and non-persistence. Finally, the exclusion of non-hip fractures due to a lack of data on efficacy of FPE for these fractures.
Strengths of our analysis
Overall, the data applied for the model appropriately reflects the care of elderly patients with hip fractures. Particularly, data on hip fractures was obtained from high-quality evidence or from German sources (e.g. [27]), ensuring a sufficient level of representativeness. By focusing on hip fractures, the model highlights the most relevant consequence of a fall from a socioeconomic perspective. Clinical data revealed that hip fractures are the major cause of disability, nursing home admission and mortality [60]. Moreover, for relevant input parameters we could rely on country-specific claims data with large samples [27, 28, 35]. Where no data were available for Germany, we could take data from European countries with a similar standard of care [22, 32]. A further strength of this analysis is in the consideration of transitions to nursing home due to hip fractures (including the increased risk of re-fractures in a nursing home setting).
Limitations
By using a modelling approach, different structural and parameter-related constraints may limit the validity of the results. First, the exclusion of non-hip fractures due to a lack of high-quality data may result in an underestimation of the cost-effectiveness of FPE. Although we met this limitation by incorporating vertebral fractures in a structural sensitivity analysis – which improved the ICER by 12% (women) and 54% (men) - other clinical events such as pelvic and wrist fractures or even traumatic brain injuries were not reflected in the model. In addition to the prevention of non-hip-fractures and other injuries, further potential health gains of FPE are in benefits to mental health resulting from social contact in a group, reduced depressive symptoms or less fear of falling [61]. Including these aspects is likely to improve the cost-effectiveness of FPE in independently living elderly. Moreover, the occurrence of cardiovascular events such as stroke would be positively affected by active training-sessions such as FPE [62].
Second, in the model, a transition to nursing home is only possible immediately after a hip-fracture. Whereas the impact of nursing home transitions unrelated to hip fractures was evaluated in sensitivity analyses, the number of delayed nursing home transitions after hip fractures is unknown. Consideration of delayed nursing home transitions because of a hip fracture may further improve the cost-effectiveness of FPE.
Third, compared to all nursing residents, for patients with a hip fracture who are admitted to nursing home, an increased mortality was based on claims data for the first 6 months post-fracture [21]. A persistent increase of mortality (i.e. > 6 months post-fracture) was not modelled due to a lack of data. However, variation of mortality parameters as part of the sensitivity analysis in the states post hip fracture resulted only in minor changes of the cost-effectiveness ratio.
Fourth, the costs of FPE were based on payments of the German SHI, which may differ from the real resource consumption. For example, Deverall et al. showed significant cost differences between a home-based, a peer-led group-based and a commercial provided group-based FPE [20]. In addition, the transferability of our results to other health care systems might be limited.
Finally, there is inconclusive evidence of adherence of FPE for the time beyond the study period (> 1 year). We conservatively assumed a 28% reduction of adherence per year which might still underestimate the real proportion of dropouts [39]. However, the assumed efficacy of FPE was based on a wide range of clinical trials in different settings [21].
Comparison with previous studies
Previous economic modelling studies, which evaluated the cost-effectiveness of FPE, differed in multiple methodological aspects. In addition, the reported results varied markedly:
Assessing balance and strength exercise provided to community living elderly, the analysis of Frick et al. resulted in an ICER of about €115,000 per QALY gained (compared to standard care) [19, 63]. Church et al. compared different strategies for fall prevention [15]. For the comparison of group-based exercise to no intervention in the general population, there was an ICER in the amount of €2964 per avoided fall [15, 63]. However, the probability of group-based exercise being cost-effective was about 10% at a WTP of 100,000. Deverall et al. compared three different types of exercise interventions [20]. As a result, a home-based exercise program was most cost-effective compared to no intervention with an ICER of €3594 per QALY gained, followed by a peer-led group-based variant (€7343) and a commercially provided group-based exercise (€26,665) [20, 63].
To some extent, the differences between the compared models result from the definition of outcome parameter (e.g. injuries, fractures or falls) and, the perspectives used for the analyses. In addition, the analyses targeted specific subgroups without using a well-established and standardized framework for determining a patient’s risk of fall [15, 20].
Future research
To obtain more reliable information about the cost-effectiveness of FPE, more data on clinical effectiveness are needed. Particularly, clinical trials addressing fractures other than hip would enable researchers to draw more robust conclusions. Furthermore, future trials should be sufficiently powered with fractures as primary outcome. Additionally, the inclusion of health gains beyond fracture prevention (e.g., benefits to mental health or less fear of falling) is desirable to provide more robust data on these outcomes [20, 64].
Because FPE is expected to result in a significant reduction of fractures over years but not months, future clinical studies also should reflect a sufficient period of observation. For all trials addressing fracture prevention, the attenuation of the treatment effect due to e.g. decreasing adherence should be taken into consideration.
Conclusions
Our analysis suggests that FPE delivered in a group-based setting may have only little impact for the prevention of fall-related hip fractures and the associated costs. Because of a higher fracture incidence in women compared to men, FPE in women has a more favourable cost-effectiveness ratio. For both women and men, our results show an improved cost-effectiveness-ratio when vertebral fractures were incorporated. To allow comprehensive statements on the cost-effectiveness of FPE more homogenous studies with statements on specific fracture types are needed.
Availability of data and materials
Datasets used and analysed during the current study are included in this published article and its supplementary files. The datasets used for the probabilistic sensitivity analysis are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- DRG:
-
Diagnosis-related groups
- e.g. :
-
For example
- FaME:
-
Falls Management Exercise Program
- FPE:
-
Fall prevention exercise
- ICD:
-
International classification of diseases
- ICER:
-
Incremental cost-effectiveness-ratio
- M:
-
Men
- Mio :
-
Million
- Non-inst.:
-
Non-institutionalized
- OEP:
-
Otago Exercise Program
- QALY:
-
Quality-adjusted life year
- SHI:
-
Statutory health insurance
- W:
-
Women
- WTP:
-
Willingness to pay
References
Schick S, Heinrich D, Graw M, Aranda R, Ferrari U, Peldschus S. Fatal falls in the elderly and the presence of proximal femur fractures. Int J Legal Med. 2018;132(6):1699–712. https://doi.org/10.1007/s00414-018-1876-7.
Peeters GM, Jones M, Byles J, Dobson AJ. Long-term consequences of noninjurious and injurious falls on well-being in older women. J Gerontol A Biol Sci Med Sci. 2015;70(12):1519–25. https://doi.org/10.1093/gerona/glv102.
Hartholt KA, Lee R, Burns ER, van Beeck EF. Mortality from falls among US adults aged 75 years or older, 2000-2016. Jama. 2019;321(21):2131–3. https://doi.org/10.1001/jama.2019.4185.
Court-Brown CM, Clement ND, Duckworth AD, Biant LC, McQueen MM. The changing epidemiology of fall-related fractures in adults. Injury. 2017;48(4):819–24. https://doi.org/10.1016/j.injury.2017.02.021.
Vestergaard P, Rejnmark L, Mosekilde L. Loss of life years after a hip fracture. Acta Orthop. 2009;80(5):525–30. https://doi.org/10.3109/17453670903316835.
Youm T, Koval KJ, Zuckerman JD. The economic impact of geriatric hip fractures. Am J Orthop (Belle Mead NJ). 1999;28(7):423–8.
Weyler EJ, Gandjour A. Socioeconomic burden of hip fractures in Germany. Gesundheitswesen. 2007;69(11):601–6. https://doi.org/10.1055/s-2007-992778.
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the european union: medical management, epidemiology and economic burden. a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
Lagerros YT, Hantikainen E, Michaelsson K, Ye W, Adami HO, Bellocco R. Physical activity and the risk of hip fracture in the elderly: a prospective cohort study. Eur J Epidemiol. 2017;32(11):983–91. https://doi.org/10.1007/s10654-017-0312-5.
Department of Health. Falls and Fractures - Exercise Training to Prevent Falls (laterlifetraining.co.uk) 2009. https://www.laterlifetraining.co.uk/wp-content/uploads/2011/12/FF_Exercise-Training-to-Prevent-Falls.pdf. Accessed 25 May 2021.
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758.12. https://doi.org/10.1136/bjsports-2016-096547.
Iliffe S, Kendrick D, Morris R, Masud T, Gage H, Skelton D, et al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess. 2014;18(49):1–105 vii-xxvii,.
El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f6234.
Panel on Prevention of Falls in Older Persons AGS, British Geriatrics S. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57.
Church J, Goodall S, Norman R, Haas M. The cost-effectiveness of falls prevention interventions for older community-dwelling Australians. Aust N Z J Public Health. 2012;36(3):241–8. https://doi.org/10.1111/j.1753-6405.2011.00811.x.
Farag I, Howard K, Hayes AJ, Ferreira ML, Lord SR, Close JT, et al. Cost-effectiveness of a home-exercise program among older people after hospitalization. J Am Med Dir Assoc. 2015;16(6):490–6. https://doi.org/10.1016/j.jamda.2015.01.075.
Patil R, Kolu P, Raitanen J, Valvanne J, Kannus P, Karinkanta S, et al. Cost-effectiveness of vitamin D supplementation and exercise in preventing injurious falls among older home-dwelling women: findings from an RCT. Osteoporos Int. 2016;27(1):193–201. https://doi.org/10.1007/s00198-015-3240-9.
McLean K, Day L, Dalton A. Economic evaluation of a group-based exercise program for falls prevention among the older community-dwelling population. BMC Geriatr. 2015;15(1):33. https://doi.org/10.1186/s12877-015-0028-x.
Frick KD, Kung JY, Parrish JM, Narrett MJ. Evaluating the cost-effectiveness of fall prevention programs that reduce fall-related hip fractures in older adults. J Am Geriatr Soc. 2010;58(1):136–41. https://doi.org/10.1111/j.1532-5415.2009.02575.x.
Deverall E, Kvizhinadze G, Pega F, Blakely T, Wilson N. Exercise programmes to prevent falls among older adults: modelling health gain, cost-utility and equity impacts. Inj Prev. 2019;25(4):258–63. https://doi.org/10.1136/injuryprev-2016-042309.
Benzinger P, Riem S, Bauer J, Jaensch A, Becker C, Buchele G, et al. Risk of institutionalization following fragility fractures in older people. Osteoporos Int. 2019;30(7):1363–70.
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res. 2009;24(7):1299–307. https://doi.org/10.1359/jbmr.090207.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:CD012424.
Kunigkeit C, Stock S, Müller D. Cost-effectiveness of a home safety intervention to prevent falls in impaired elderly people living in the community. Arch Osteoporos. 2018;13(1):122.
Evangelisches Klinikum Köln-Weyertal. Kurs KE3607 (Sturzprophylaxe - für Menschen ohne Gehhilfe) 2019. https://www.evk-gesund.de/index.php?id=12&kathaupt=11&knr=KE3607&kursname=Sturzprophylaxe+-+fuer+Menschen+ohne+Gehhilfe. Accessed 8 Aug 2020.
Korpelainen R, Keinanen-Kiukaanniemi S, Nieminen P, Heikkinen J, Vaananen K, Korpelainen J. Long-term outcomes of exercise: follow-up of a randomized trial in older women with osteopenia. Arch Intern Med. 2010;170(17):1548–56. https://doi.org/10.1001/archinternmed.2010.311.
Rapp K, Becker C, Cameron ID, Klenk J, Kleiner A, Bleibler F, et al. Femoral fracture rates in people with and without disability. Age Ageing. 2012;41(5):653–8. https://doi.org/10.1093/ageing/afs044.
Federal Statistical Office. The Federal Health Monitoring Information System 2019. www.gbe-bund.de. Accessed 8 Aug 2020.
Federal Statistical Office. Pflegestatistik. Pflege im Rahmen der Pflegeversicherung. Deutschlandergebnisse 2018. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Publikationen/Downloads-Pflege/pflege-deutschlandergebnisse-5224001179004.pdf?__blob=publicationFile&v=5. Accessed 30 Mar 2021.
Youm T, Koval KJ, Kummer FJ, Zuckerman JD. Do all hip fractures result from a fall? Am J Orthop (Belle Mead NJ). 1999;28(3):190–4 PubMed PMID: 10195844.
Federal Statistical Office. Results of the causes of death statistics for Germany - Detailed four-digit ICD10 classification - 2016. Available from: https://www.destatis.de/GPStatistik/receive/DEHeft_heft_00096650. Accessed 30 Mar 2020.
Jürisson M, Raag M, Kallikorm R, Lember M, Uusküla A. The impact of hip fracture on mortality in Estonia: a retrospective population-based cohort study. BMC Musculoskelet Disord. 2017;18(1):243.
Allers K, Hoffmann F. Mortality and hospitalization at the end of life in newly admitted nursing home residents with and without dementia. Soc Psychiatry Psychiatr Epidemiol. 2018;53(8):833–9. https://doi.org/10.1007/s00127-018-1523-0.
Federal Statistical Office. Detailed diagnostic data 2017. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhaeuser/Publikationen/Downloads-Krankenhaeuser/tiefgegliederte-diagnosedaten-5231301177015.html. Accessed 30 Mar 2021.
Jacobs H, Zeeb H, Hoffmann F. Incidence rates of and mortality after hip fracture among German nursing home residents. Int J Environ Res Public Health. 2018;7:15(2).
Becher K. Klinischer Verlauf von Patienten mit Hüftfraktur. Bochum: Ruhr-Universität Bochum; 2006.
Schulz C, Buchele G, Rehm M, Rothenbacher D, Roigk P, Rapp K, et al. Patient characteristics as Indicator for care dependence after hip fracture: a retrospective cohort study using health insurance claims data from Germany. J Am Med Dir Assoc. 2019;20(4):451–5. https://doi.org/10.1016/j.jamda.2018.09.029.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7. https://doi.org/10.1111/j.1524-4733.2007.00213.x.
van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22(2):120–33. https://doi.org/10.1016/s0749-3797(01)00413-5.
Techniker Krankenkasse. Satzung der Techniker Krankenkasse 2019. https://www.tk.de/resource/blob/2024414/dc9e58d58b7bf17f071c588f6151abf8/tk-satzung-data.pdf. Accessed 30 Mar 2021.
National Association of Statutory Health Insurance Companies. Prevention Guide 2018. https://www.gkv-spitzenverband.de/krankenversicherung/praevention_selbsthilfe_beratung/praevention_und_bgf/leitfaden_praevention/leitfaden_praevention.jsp Accessed 30 Mar 2021.
Muller-Mai CM, Schulze Raestrup US, Kostuj T, Dahlhoff G, Gunster C, Smektala R. One-year outcomes for proximal femoral fractures: Posthospital analysis of mortality and care levels based on health insurance data. Unfallchirurg. 2015;118(9):780–94. https://doi.org/10.1007/s00113-013-2534-7.
DRG-Research Group. Webgrouper 2019. https://www.drg-research-group.de/index.php?option=com_webgrouper&view=webgrouper&Itemid=112. Accessed 30 Mar 2021.
National Association of Statutory Health Insurance Companies. Statutory co-payments 2019. https://www.gkv-spitzenverband.de/service/versicherten_service/zuzahlungen_und_befreiungen/gesetzliche_zuzahlungen/gesetzliche_zuzahlungen.jsp. Accessed 30 Mar 2021.
Muller F, Galler M, Zellner M, Bauml C, Grechenig S, Kottmann T, et al. Total hip arthroplasty for hip fractures: time to surgery with respect to surgical revision, failure, and mortality. Geriatr Orthop Surg Rehabil. 2019;10:2151459318818162.
Federal Ministry of Health. Statutory health insurance. Final accounting results 2017. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Statistiken/GKV/Finanzergebnisse/KJ1_2017_Internet.pdf. Accessed 30 Mar 2021.
Grund S, Roos M, Duchene W, Schuler M. Treatment in a center for geriatric traumatology. Dtsch Arztebl Int. 2015;112(7):113–9. https://doi.org/10.3238/arztebl.2015.0113.
Logters T, Hakimi M, Linhart W, Kaiser T, Briem D, Rueger J, et al. Early interdisciplinary geriatric rehabilitation after hip fracture : effective concept or just transfer of costs? Unfallchirurg. 2008;111(9):719–26. https://doi.org/10.1007/s00113-008-1469-x.
Federal Statistical Office. Consumer price index 2019. https://www.destatis.de/DE/Themen/Wirtschaft/Preise/Verbraucherpreisindex/_inhalt.html#sprg238918. Accessed 30 Mar 2021.
Kreck S, Klaus J, Leidl R, von Tirpitz C, Konnopka A, Matschinger H, et al. Cost effectiveness of ibandronate for the prevention of fractures in inflammatory bowel disease-related osteoporosis: cost-utility analysis using a Markov model. Pharmacoeconomics. 2008;26(4):311–28. https://doi.org/10.2165/00019053-200826040-00004.
Rote Liste GmbH. Rote Liste 2019. https://www.rote-liste.de/. Accessed 30 Aug 2021.
National Association of Statutory Health Insurance Physicians. Uniform value scale 2019. https://www.kbv.de/html/ebm.php. Accessed 30 Aug 2021.
Association of Statutory Health Insurance Physicians Berlin. Physical Therapy Remuneration List (May 2019). https://www.kvberlin.de/20praxis/50verordnung/20heilmittel/hm_verguetung/verguetung_physio.pdf. Accessed 30 Mar 2021.
Federal Ministry of Health. The benefits of long-term care insurance at a glance 2019. https://www.bundesgesundheitsministerium.de/leistungen-der-pflege.html. Accessed 30 Mar 2021.
Briggs A. Handling uncertainty in economic evaluation and presenting the results. In: Drummond M, A. M, editors. Economic evaluation in health care New York: Oxford University Press; 2004.
Rothgang H, Kulik D, Müller R, Unger R. GEK-Pflegereport 2009. Schwäbisch Gmünd: GEK – Gmünder ErsatzKasse; 2009.
Bleibler F, Konnopka A, Benzinger P, Rapp K, Konig HH. The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany--a demographic simulation model. Osteoporos Int. 2013;24(3):835–47. https://doi.org/10.1007/s00198-012-2020-z.
Lange A, Zeidler J, Braun S. One-year disease-related health care costs of incident vertebral fractures in osteoporotic patients. Osteoporos Int. 2014;25(10):2435–43. https://doi.org/10.1007/s00198-014-2776-4.
Mauskopf JA, Sullivan SD, Annemans L, Caro J, Mullins CD, Nuijten M, et al. Principles of good practice for budget impact analysis: report of the ISPOR task force on good research practices--budget impact analysis. Value Health. 2007;10(5):336–47. https://doi.org/10.1111/j.1524-4733.2007.00187.x.
Uriz-Otano F, Pla-Vidal J, Tiberio-Lopez G, Malafarina V. Factors associated to institutionalization and mortality over three years, in elderly people with a hip fracture-an observational study. Maturitas. 2016;89:9–15. https://doi.org/10.1016/j.maturitas.2016.04.005.
Mortazavi SS, Shati M, Ardebili HE, Mohammad K, Beni RD, Keshteli AH. Comparing the effects of group and home-based physical Acivity on mental health in the elderly. Int J Prev Med. 2013;4(11):1282–9.
Prior PL, Suskin N. Exercise for stroke prevention. Stroke Vasc Neurol. 2018;3(2):59–68 56.
Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evidence Policy. 2010;6(1):51–9. https://doi.org/10.1332/174426410X482999.
Karnon J, Afzali HHA, Putro G, Thant PW, Dompok A, Cox I, et al. A cost-effectiveness model for frail older persons: development and application to a physiotherapy-based intervention. Appl Health Econ Health Policy. 2017;15(5):635–45. https://doi.org/10.1007/s40258-017-0324-z.
Acknowledgements
We thank Mr. Arim Shukri for statistical advice.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
BS and DM developed the model. BS performed the analysis, interpreted the data and wrote the manuscript. DM was a major contributor in writing the manuscript. StS revised the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Scheckel, B., Stock, S. & Müller, D. Cost-effectiveness of group-based exercise to prevent falls in elderly community-dwelling people. BMC Geriatr 21, 440 (2021). https://doi.org/10.1186/s12877-021-02329-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02329-0