Abstract
Background
High rates of food insecurity, obesity and obesity-related comorbidities in ageing South African (SA) women may amplify the risk of developing sarcopenic obesity. This study aimed to investigate the prevalence and correlates of sarcopenic obesity and its diagnostic components [grip strength, appendicular skeletal muscle mass (ASM) and body mass index (BMI)] in older SA women from a low-income setting.
Methods
This cross-sectional study recruited black SA women between the ages of 60–85 years (n = 122) from a low-income community. Testing included a fasting blood sample (markers of cardiometabolic risk, HIV), whole body and regional muscle and fat mass (dual-energy absorptiometry x-ray), anthropometry, blood pressure, functional movement tests, current medication use, demographic and health questionnaires, physical activity (PA; accelerometery), household food insecurity access scale, and a one-week quantified food frequency questionnaire. Foundation for the National Institutes of Health (FNIH) criteria (grip strength and ASM, adjusted for BMI) were used to classify sarcopenia. Participants with sarcopenia alongside a BMI of > 30.0 kg/m2 were classified as having sarcopenic obesity. Prevalence using other criteria (European Working Group on Sarcopenia in Older People, Asian Working Group for Sarcopenia and the International Working Group for Sarcopenia) were also explored.
Results
The prevalence of sarcopenia was 27.9%, which comprised of sarcopenia without obesity (3.3%) and sarcopenic obesity (24.6%). Other classification criteria showed that sarcopenia ranged from 0.8–14.7%, including 0.8–9.8% without obesity and 0–4.9% with sarcopenic obesity. Using multivariate-discriminant analysis (OPLS-DA) those with sarcopenic obesity presented with a descriptive profile of higher C-reactive protein, waist circumference, food security and sedentary time than women without sarcopenic obesity (p = 0.046). A similar profile described women with low BMI-adjusted grip strength (p < 0.001).
Conclusions
The majority of women with sarcopenia were also obese (88%). We show a large discrepancy in the diagnostic criteria and the potential for significantly underestimating the prevalence of sarcopenia if BMI is not adjusted for. The main variables common to women with sarcopenic obesity were higher food security, lower PA and chronic inflammation. Our data highlights the importance of addressing obesity within these low-income communities to ensure the prevention of sarcopenic obesity and that quality of life is maintained with ageing.
Similar content being viewed by others
Background
Economic and social transition in low-middle income countries (LMIC) has seen substantial increases in life expectancy alongside increasing rates of obesity and cardiometabolic disease [1]. Accordingly, age-related diseases such as sarcopenia are of increasing interest due to the impact on quality of life, frailty, falls and mortality [2,3,4]. Sarcopenia is operationally defined as low muscle mass and function, and has been shown to increase risk for developing functional limitations and physical disabilities, as defined by difficulty in performing daily activities [5]. Therefore, reversing, delaying, and/or preventing the onset of sarcopenia and maintaining functional mobility is paramount to ensuring quality of life with ageing [6]. However, data on the prevalence and understanding potential determinants of sarcopenia in LMIC's are scarce [7].
There are many different and population specific criteria for the classification of sarcopenia, including the European Working Group on Sarcopenia in Older People (EWGSOP [8, 9]), Asian Working Group for Sarcopenia (AWGS) [10], International Working Group for Sarcopenia (IWGS) [11] and The Foundation for the National Institutes of Health (FNIH) [7]. Development of the FNIH criteria included data in African Americans from a variety of income levels and has been previously used in studies of women from sub-Saharan Africa [7]. Importantly, the FNIH criteria incorporate cut-points for grip strength and appendicular skeletal muscle mass (ASM) adjusted for body mass index (BMI), which may be an optimal approach when classifying sarcopenia in individuals with obesity [12]. Notably, the criterion recommended for defining clinically meaningful low lean body mass is adjusted for BMI (ASMBMI) [12]. Moreover, individuals with obesity, regardless of age, have a greater absolute maximum muscle strength compared to individuals without obesity; however, when maximum muscular strength is normalised to body mass, individuals with obesity appear weaker [6]. Therefore, a similar approach by FNIH has identified clinically significant, gender-specific cut-points for BMI adjusted strength (Grip StrengthBMI) [12, 13].
This is particularly relevant when assessing sarcopenia in LMIC's that present with an increasing double burden of malnutrition, which refers to the co-existence of undernutrition and overweight/obesity [14]. In particular, SA women have the highest prevalence of overweight and obesity in sub-Saharan Africa (68%) [15, 16], which is occurring simultaneously with 64% of households experiencing food insecurity [17]. Furthermore, food insecurity is an upstream determinant of behaviours such as diet and physical activity (PA), which are in turn associated with an increased risk of overweight and obesity [17, 18]. The presence of obesity coupled with sarcopenia has recently been termed ‘sarcopenic obesity’ or ‘sarcobesity’, and has been shown to exacerbate cardiometabolic risk and functional limitations [6, 19]. The determinants of sarcopenia and sarcopenic obesity is complex and incorporates multiple factors, such as physical inactivity, low protein intake, chronic systemic inflammation, insulin resistance and fat infiltration into the muscle [20,21,22,23]. Previous studies examining these determinants have occurred in cohorts from high-income countries [7,8,9, 11, 23,24,25], with little data available from low-income settings [7, 26, 27]. It is anticipated that high rates of food insecurity, obesity and obesity-related comorbidities in ageing SA women may amplify the risk of developing sarcopenic obesity. However, socioeconomic status, PA, diet, and cardiometabolic risk separating those with and without sarcopenia or sarcopenic obesity have not been previously explored in African women. Using a cross-sectional design, this study aimed to compare the prevalence of sarcopenia using different criteria and investigate the correlates of sarcopenic obesity and its diagnostic components (grip strength, ASM and BMI) in older SA women from a low-income setting.
Material and methods
Study participants
A convenience sample of community dwelling older women (n = 122) were recruited from a low-income, urban SA setting with a demographic profile composing of black South Africans [28]. Women were recruited from senior community groups/clubs and included those between the ages of 60–85 years, living independently (living in their own household or living with family) and who were ambulatory. One participant per household was recruited. Participants were excluded if they had any physical disability or condition that prevented them from completing the functional tests. In the context of the South African population, an older adult was classified as > 60 years based on the classification from the United Nations and due to the low life-expectancy of 65.1 years for South African adults (68.3 and 61.9 years for women and men, respectively) [29, 30].
Study design and ethical consideration
For this cross-sectional observational study, clinical research workers visited the community centres for consent and screening after which participants attended the university-based laboratory on two separate occasions with one week between testing sessions. The first testing session included fasting blood sample and HIV testing, body composition, blood pressure, functional movement tests, and sociodemographic and health questionnaires. Participants were fitted with accelerometers and asked to complete sleep diaries for the following week, which were collected at the second testing session. Participants also completed a nutritionist-administered one-week food frequency questionnaire. This study was approved by the Human Research Ethics Committee of the Faculty of Health Sciences at the University of Cape Town (HREC REF:095/2018), and the NHS, Invasive or Clinical Research Committee at the University of Stirling (NICR:17/18). All participants provided written and verbal consent prior to testing procedures, including consent for HIV testing with counsellor support.
Classification of sarcopenia and sarcopenic obesity
The FNIH Sarcopenia Project used an evidence-based approach to develop criteria for sarcopenia classification [12]. Recommendations for cut-points for low muscle strength and low lean muscle mass included Grip strengthBMI of < 0.56, and ASMBMI of < 0.512, respectively. Participants presenting with both low Grip strengthBMI and ASMBMI were classified as sarcopenic. Participants classified with sarcopenia alongside a BMI of > 30.0 kg/m2 were classified as having sarcopenic obesity [31]. The variability in the prevalence of sarcopenia and sarcopenic obesity based on the classification criteria of EWGSOP [8], EWGSOP-2 [9], AWGS [10], IWGS [11] and a criterion for ASMI in SA women [26] were also explored in this cohort (Table 1).
Components and correlates of sarcopenia and sarcopenic obesity
Body composition
Body mass (BW-150, NAGATA, Tainan, Taiwan) and stature (3PHTROD-WM, Detecto, Missouri, USA) were measured in lightweight clothing for the calculation of BMI and used to classify obesity (> 30.0 kg/m2) [32]. Waist circumference (WC) at the umbilicus, and hip circumference (HC) at the largest protrusion of the buttocks, were measured using a metal anthropometric tape measure (CESCORF, Brazil). Circumferences were measured over the naked skin and noted to the nearest 0.1 cm. Circumferences were used to calculate waist to hip ratio (WHR), with abdominal obesity classified as WC > 80 cm and WHR > 0.85 [32].
Whole body composition was measured using dual energy x-ray absorptiometry (DXA; Discovery- W®, version 12.7.3.7, Hologic, Bedford, MA, USA) according to standard procedures. Sub-total (excluding the head) fat mass (FM) and fat-free soft tissue mass (FFSTM) were used for all analyses. Appendicular skeletal muscle mass (ASM) was calculated using the sum of FFSTM (kg) of both legs and arms, which was further adjusted for stature (ASMI; kg/height (m2)) and BMI (ASMBMI). DXA-derived regional body fat distribution, including android and gynoid were determined as previously described [33] and expressed as a percentage of subtotal FM. Peripheral (appendicular) fat (kg) was calculated as the sum of FM of both legs and arms, which was further divided by ASM to calculate peripheral fat/ASM ratio. Subcutaneous (SAT) and visceral (VAT) adipose tissue areas were estimated as described previously [34] and used to calculate VAT/SAT ratio. Bone mineral density was quantified using DXA at the spine (lumbar vertebrae L1-L5), total hip and femoral neck and World Health Organisation classification (t-score < − 2.5) was used to determine those with osteoporosis (Low t-score at > 1 site) [35].
Sociodemographic and health questionnaires
Sociodemographic questionnaire included, estimated household monthly food costs, measures of household asset index (total of 11 assets that included the ownership of electrical appliances, computers, internet and/or motor vehicles), housing density (ratio of the number of people living in the house divided by the number of rooms) and the number of children (< 18 years) financially supported by the participants. Participants brought to the study site all medication/s currently prescribed to them for recording and was used to identify disease prevalence of hypertension, dyslipidemia, diabetes, arthritis, and HIV. Disease prevalence for cancer and tuberculosis was obtained using self-reported diagnosis and medication history of the disease and osteoporosis was identified from bone mineral density scans (DXA). Notably, through verbal communication with participants we identified a low reliability in the self-reported patient history of several chronic conditions (i.e. stroke, heart failure and coronary artery disease), which are not reported in the current study. Multi-morbidity was classified as having 2 or more of the aforementioned listed diseases. All participants underwent a rapid HIV test, due to previously identified associations between HIV and premature ageing, sarcopenia, obesity and visceral adiposity [36, 37]. Pre and post-test counselling were completed by a trained HIV counsellor and if the participant was HIV positive (known or unknown) they continued in the study and were referred to a local clinic for follow-up testing and counselling. All information on current and past smoking (duration of smoking and number of daily cigarettes) behaviours was obtained. Participants were also asked if they had fallen in the past year. A fall was defined as ‘any time you unexpectedly (or unintentionally) landed on the floor or ground’ [38]. Participants further completed a Household Food Insecurity Access Scale (HFIAS), which consists of nine questions about worry, availability and accessibility of foods for the household during the previous 30 days [39]. Total HFIAS ranges from 0 (food security) to 27 (maximum food insecurity).
Components of metabolic syndrome, inflammation, iron and vitamin-D
Participants arrived at the laboratory at 09:00 following an overnight fast (10–12 h). A fasting venous blood sample was collected for the analysis of cardiometabolic risk markers. Specifically, components of metabolic syndrome, including glucose (enzymatic method with hexokinase, Cobas Analyzer, Roche Diagnostics, Basel, Switzerland), high-density lipoprotein (HDL) cholesterol, and triglyceride (enzymatic colorimetric test, Cobas Analyzer) concentrations were analysed. Metabolic syndrome was determined if participants had three or more components using the 2009 harmonized criteria [40]. These components included: elevated waist circumference (≥80 cm in women), elevated triglycerides (≥1.7 mmol/L and/or using cholesterol lowering medication), reduced HDL cholesterol (< 1.3 mmol/L in women), elevated blood pressure (≥130 mmHg for systolic and/or ≥ 85 mmHg for diastolic and/or using blood pressure medication), and elevated glucose (≥5.6 mmol/L and/or using diabetes medication). Vitamin- D 25 OH (electrochemiluminescence binding assay, Cobas Analyzer), C-Reactive protein (CRP) (high-sensitivity, particle enhanced immunoturbidimetric assay, Cobas Analyzer) and ferritin (immunoassay, Cobas) were analysed. An acute inflammatory response was suspected when a high ferritin level (> 150 ng/mL) coincided with high CRP (> 20 mg/dL) and these data (n = 11) were removed from analyses [41].
Blood pressure was measured 3 times at 1-min intervals using an appropriately sized cuff and an automated blood pressure monitor (Omron 711, Omron Healthcare, Hamburg, Germany), after participants had rested in a seated position for 30 min. The mean of the two measurements is presented.
Functional movement tests
All functional movement tests were conducted on the same day and by the same research assistant. All tests were conducted in the order reported below.
Strength
Grip strength (kg) was measured in a seated position on the non-dominant hand using a hand dynamometer (T.K.K. 5401, Grip-D, Takei, Tokyo, Japan). The measures were taken with the arm static and elbow by the side in a right-angle position. The test was repeated 3 times with a 1-min rest between tests. The maximum score was used in the analysis [42].
Gait speed
Participants were required to complete a 10-m walk test which involved walking ‘at a fast pace’ between two markers that were set up 14 m apart. Tape was placed on the ground at the 2-m and 12-m mark in order to exclude the acceleration and deceleration phase to ensure a measure of ‘steady state’ walking was obtained [43]. The time taken to walk between the 2- and 12-m markers was recorded, and the test was repeated twice with a 1-min rest between tests. The mean score was used in the analysis (m/s).
Agility/dynamic balance
The 3-m timed-up and go test was completed by measuring the time taken to get up from a seated position (without using arms for assistance), walk around a marker at 3 m, and return to the seated position. This test was repeated twice with a 1-min rest between tests. The fastest time was used in the analysis (seconds) [44].
Aerobic endurance
The 6-min walk test was conducted once to measure the number of metres covered by walking in a 6-min time period. The research assistant used a stopwatch and walked quietly behind the participant during the test to mark and monitor the distance covered. Participants walked in a 20 × 5 m rectangle [43].
Physical activity, sleep and sedentary behaviour
Physical activity, sleep and sedentary behaviour were measured simultaneously with an Actigraph (GTX3+, ActiGraph LLC, Pensacola, Florida) and ActivPAL (PAL Technologies Ltd., Glasgow, Scotland). Both accelerometers were worn for seven consecutive 24-h days. The Actigraph was attached to the waist with a lightweight belt and the ActivPAL was worn on the mid anterior right thigh. Participants completed a sleep diary to record wake and sleep times over the 7-day period. Actigraph data was analysed (ActiLife, version 6) with valid wear defined as 600 min of waking wear time per day for a minimum of four days. Troiano cut-points were used to define total PA (> 100 cpm), light PA (100–2019 cpm) and moderate to vigorous physical activity (MVPA; > 2020 cpm) [45]. ActivPAL data were analysed (CREA beta-algorithm, PAL analysis, Version 8.10.8.32) with all participants presenting with a minimum of seven consecutive 24-h days. Wear time included a 24-h protocol, allowing for 4 h of non-wear time, minimum of 10 s non-upright and upright periods. Daily step count and number of sit to stand transitions, time spent upright (total of standing and stepping time), standing, stepping sitting, napping (secondary lying time), sleeping (primary lying time), total time spent in sedentary bouts of more than 30 and 60 min are reported, and daily energy expenditure (calories) was calculated by multiplying daily metabolic equivalent of task (MET) by body weight (kg).
Dietary intake
A nutritionist administered a 7-day quantified food frequency questionnaire (QFFQ) for each participant. Food portion sizes were estimated using household utensils, food containers and packaging, three-dimensional sponge models and “dish-up and measure”. Amounts reported in household measures or volume were converted to grams using the SA Medical Research Council (SAMRC) Food Quantities Manual for SA [46]. Food intake was converted to energy and macronutrients (fats, carbohydrates, protein (animal and plant), fibre, and added sugar) using the SA food composition database [47]. Food consumed during the 7-day reference period for the QFFQ were categorized into 12 food groups and expressed as a % of energy intake (%EI), based on a recent SA study [48]. The food groups included, fruits, vegetables, cooked porridge, starchy grains, legumes, nuts and seeds, milk and dairy products, animal source foods, fats and oils, sugar and sugary foods, savoury snacks, dishes and sauces and alcohol. Dietary data was removed if the participant reported below 4000 kJ per day (n = 19 removed).
Sample size calculation and statistical analyses
Based on methodology in Kruger et al. [26] we used G*Power 3.1 to estimate sample size for a multiple regression model with a medium effect size (F tests – Linear multiple regression: Fixed model, R2 increase at 95% power, medium effect size = 0.15), which gave a sample size of n = 107.
Data were expressed as mean ± standard deviation (SD) or median interquartile range (IQR - 25th–75th percentile) depending on the normality of continuous variables. Normality was tested using Shapiro-Wilks test and skewed data were log transformed before analysis. Data was analysed using IBM SPSS statistics (Version 26, Statistical Package for the Social sciences, Chicago, IL, USA). P values are uncorrected for multiple testing and are reported, with significance set at p < 0.05.
All outcomes were firstly compared univariately between groups (with and without sarcopenia) using an independent t-test or Mann-Whitney U test for normally distributed and skewed data, respectively. Secondly, to investigate the differences in lifestyle behaviors (diet and PA), components of metabolic syndrome, body composition, functional movement and socioeconomic status between those with and without sarcopenic obesity, we explored the data using a multivariate analysis. Firstly, a principle component analysis identified that there were no outliers. Secondly, orthogonal partial least squares discriminant analysis (OPLS-DA; SIMCA v.15.2 (Sartorius, Umetrics, Umea, Sweden) models were calculated to explore the differences between those with and without sarcopenic obesity. OPLS-DA is a supervised modelling approach that uses a predefined binary variable as the outcome (2 class model that describes those with and without sarcopenic obesity). Finally, two further OPLS models were conducted using grip strengthBMI and ASMBMI as continuous predictors. Both OPLS and OPLS-DA models summarise the largest systematic variation in the dataset into 1 latent variable (OPLS as one constant predictor variable and OPLS-DA as a 2-class model). These methods are highly suitable for a large number of highly correlated variables and provides information on the variables that have the largest discriminatory power [49]. To prevent overfitting of models, the models were validated based on ANOVA of the cross-validated OPLS-DA scores (CV-ANOVA) for significance testing [50]. A validated and significant model was considered with a CV-ANOVA of p < 0.05. Variables in each model were considered significant when fulfilling the statistical significance criteria using post-hoc linear regression on loadings calculated from the validated OPLS-models on a 95% confidence level [51]. All data in the OPLS models are reported as loading weight (w) with 95% confidence intervals, which describes the contribution of each listed variable (X variable) to the model. Variables with large w’s (positive or negative) are highly correlated with the Y variable that represents the continuous predictors (OPLS) or groupings (OPLS-DA).
Results
Sarcopenia criteria
The application of different sarcopenia criteria is presented in Table 1. The FNIH criteria for sarcopenia was used to classify participants with sarcopenia (27.9%), which comprised of sarcopenia without obesity (3.3%) and sarcopenic obesity (24.6%). Using other sarcopenia classification criteria, the prevalence of sarcopenia ranged from 0.8–14.7%, which included 0.8–9.8% without obesity and 0–4.9% with sarcopenic obesity.
We then compared functional and body composition characteristics of the women with and without sarcopenia based on the FNIH criteria (Table 2). The majority (n = 87, 71%) of the total sample were classified as obese, with 88% (n = 30) of participants with sarcopenia and 65% (n = 57) of participants without sarcopenia being obese (p = 0.005). Accordingly, variables relating to total adiposity and body fat distribution were higher in those with sarcopenia (p < 0.05). Functional movement tests showed lower grip strength, gait speed and endurance (6-min walk test) in those with sarcopenia (p < 0.05).
Univariate analysis shows that the majority of the cohort (73%) presented with metabolic syndrome and the prevalence tended to be higher in women with sarcopenia (Table 3). Furthermore, the sarcopenic group had higher CRP and lower iron levels (ferritin) compared to those without sarcopenia (p < 0.05). Participants with sarcopenia supported more children (p < 0.05) and few women in the cohort were previous (n = 5) or current smokers (n = 11).
Physical activity, sedentary behaviour and dietary intake data are shown in Table 3. Univariate analysis showed that women with sarcopenia presented with a lower daily step count, stepping time, and sit to stand transitions than women without sarcopenia (p < 0.05). The mean macronutrient consumption for the whole cohort comprised of 64.8 ± 7.2%EI carbohydrates, 12.3 ± 2.1%EI protein and 21.2 (17.5–25.1) %EI fat. Further, the dominant food groups consumed were starchy grains (31.1 ± 11.4%EI), and sugar and sugary foods (14.9 (10.1–20.8) %EI). There were no differences in dietary intake between the women with sarcopenia and those without.
The prevalence of falls and multimorbidity are presented in Table 4. Falls in the last year were reported by 38% (n = 46) of women and this did not differ between those with and without sarcopenia (p > 0.05). Ninety one percent (n = 111) of women had multimorbidity (> 2 diseases) and this did not statistically differ by group (p > 0.05). Women with sarcopenia had a higher prevalence of hypertension (97%, n = 33) compared to women without sarcopenia (82%, n = 72; p < 0.05).
Correlates of sarcopenic obesity and its components using OPLS modelling
As the majority of participants with sarcopenia (FNIH criteria) were also obese we explored correlates of sarcopenic obesity. OPLS-DA modelling was used to determine a profile of variables that discriminated between non-sarcopenic and sarcopenic obese individuals (CV-ANOVA p < 0.001; Fig. 1). Figure 1 (a) presents individual variability based on group classification (b) and the variables that significantly discriminated between groups. This model presents behavioural (dietary intake, PA and sedentary behaviour), sociodemographic and phenotypic characteristics (components of metabolic syndrome, VAT/SAT ratio and functional movement) to assist in developing a profile in SA women that may identify those with sarcopenic obesity. Interestingly, those with sarcopenic obesity supported more children and were more food secure. Unsurprisingly, several metabolic syndrome components (waist circumference and triglycerides), alongside chronic systemic inflammation (CRP) were higher in those with sarcopenic obesity. In terms of the functional movement tests, gait speed was not a significant contributor to the model, but rather those with sarcopenic obesity had lower cardiovascular fitness (6-min walk test), daily step count, stepping time, light PA, sit to stand transitions, and daily energy expenditure. Time spent sitting for more than 30 and 60-min bouts was significantly higher in those with sarcopenic obesity. Interestingly, there were no dietary intake characteristics that significantly contributed to the sarcopenic obesity profile.
Multivariate characteristic profile for non-sarcopenic and sarcopenic obese participants (n = 118; OPLS-DA CV-ANOVA P < 0.001). (a) OPLS-DA cross-validated scores (tcv [1]) that describes participant variability in the characteristic profile. (b) The characteristic profile that discriminates between non-sarcopenic and sarcopenic obese participants. The asterisk (*) represent variables that significantly (P < 0.05) discriminate between those with and without sarcopenic obesity. Error bars represent 95% confidence intervals. All data in the OPLS-DA models are reported as loading weight (w [1]), which describes the contribution of each listed variable (X variable) to the model
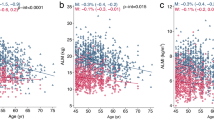
The two main components for the FNIH classification of sarcopenia used in the current study include, ASMBMI and grip strengthBMI. To understand the contribution of each correlate to the latent variable we generated two OPLS models with ASMBMI and grip strengthBMI as continuous predicted variables. Notably, there was no significant OPLS model profile that correlated with ASMBMI (CV-ANOVA p = 1.00). In contrast, Fig. 2 (a) shows individual variability in the model and identifies participants with low grip strengthBMI based on the FNIH criteria. The significant cross-validated model (CV-ANOVA p < 0.001; Fig. 2 b) identifies that a higher asset index was the only significant sociodemographic component that was associated with lower grip strengthBMI. In terms of the components of metabolic syndrome, a lower grip strengthBMI was associated with a higher waist circumference, blood pressure, triglycerides and systemic inflammation (CRP). Those with a lower grip strengthBMI had lower gait speed, agility and balance (TUG) and cardiovascular fitness (6-min walk test). This model shows a similar PA profile that identified those with sarcopenic obesity, with lower daily MVPA and time spent upright as additional variables that were associated with a lower grip strengthBMI. In terms of dietary intake, consumption of cooked porridge (%EI) correlated with a higher grip strengthBMI, while consumption of animal protein foods (%EI), cholesterol and fibre correlated with a lower grip strengthBMI.
Multivariate associations between changes in BMI-adjusted grip strength (FNIH criteria) and characteristics that relate to the pathophysiology of sarcopenia (n = 121; OPLS CV-ANOVA P < 0.001). (a) OPLS cross-validated scores (tcv [1]) that describes participant variability and (b) multivariate associations in the characteristic profile at the variable level. The asterisk (*) represent variables that are significantly (P < 0.05) associated grip strength. Error bars represent 95% confidence intervals. All data in the OPLS models are reported as loading weight (w [1]), which describes the contribution of each listed variable (X variable) to the latent variable that is produced by the model. Variables with large weights (w [1]) (positive or negative) are highly correlated with grip strength
Discussion
In this sample of older African women from a low-income setting, we show a 27.9% prevalence of sarcopenia, which comprises of 3.3% with sarcopenia and 24.6% with sarcopenic obesity. This highlights that both sarcopenia and obesity co-exist in this cohort, with the FNIH criterion reporting a significantly higher prevalence than when using other age and population specific cut-points. These findings indicate a large discrepancy in diagnostic criteria and the potential for significantly underestimating the prevalence of sarcopenia if an appropriate population-specific criterion is not applied and if BMI is not adjusted for. Furthermore, we show that the main correlates that describe a profile of sarcopenic obesity were lower food insecurity, low PA and fitness, and a chronic inflammatory state; highlighting the importance of addressing obesity within these communities to prevent sarcopenic obesity and maintaining quality of life with ageing.
The majority of women classified as sarcopenic (27.9%) were also obese (88%). However, the current study also shows that other criteria (EWGSOP, IWGS and AWGS) present a prevalence of total sarcopenia which ranged from 0.8–14.7%, which indicates the need for a population-specific criterion that has not been previously addressed in Africa. Importantly, the FNIH criteria include data in African American cohorts and were generated from data providing normative values for grip strength and ASM when adjusting for BMI [12]. Previous findings have shown that sarcopenia defined using methods considering both stature and fat mass are better at predicting weakness, reduced physical function and overall sarcopenia related disability than using ASMI and grip strength methods alone [3, 6, 12, 13]. Given the high prevalence of obesity in the current cohort (71%) and SA women (overweight and obesity of ~ 68%) [15, 16], this factor should not be ignored when assessing sarcopenia in this setting. Indeed, these data clearly indicate that FNIH BMI adjusted criteria may be an optimal set of criteria [15, 16, 31]. Previous data using the EWGSOP in SA women has shown a prevalence of 8.9% sarcopenia, however, this study included younger (45+ years old) women with a BMI range of underweight to overweight [27]. Using the same criteria (Table 1) our cohort reports a prevalence of 14.7%. Furthermore, a Gambian cohort of women between 40 and 75+ years, with normal BMI (~ 22 kg/m2) reported a prevalence of 45% and 10% sarcopenia when applying FNIH and EWGSOP criteria, respectively [7]. Notably, the FNIH criteria have only been validated in adults over 65 years, which is problematic when the mean life-expectancy of South Africans is 65.1 years [29]. To reduce discrepancies when reporting sarcopenia prevalence, African population-specific criterion needs to be used, and obesity adjusted for.
Sarcopenic obesity has been shown to exacerbate functional limitations and cardiometabolic risk [6, 19]. The current study showed that 38% of women reported that they had fallen in the past year, compared to 26.4% previously reported [52]. While a recent meta-analysis identified a higher rate of falls and fractures in older adults with sarcopenia [53], we show that those with sarcopenia had lower cardiovascular fitness and gait speed, but a similar prevalence of falls to those without sarcopenia. We suggest that collecting information on the number of falls may be more sensitive in detecting frailty and risk of sarcopenia. Further, environmental context is also important when understanding the mechanisms of falls in low-income settings (poor infrastructure, overcrowding and hazards in small dwellings) [52]. We also showed that 91% of women had multimorbidity (> 2 chronic diseases), with the three most prevalent diseases being hypertension (86%), dyslipidemia (73%) and type 2 diabetes (36%), which are all components of the metabolic syndrome. Although hypertension was the only disease that was more prevalent in those with sarcopenia, only waist circumference and triglycerides were the metabolic syndrome components that discriminated between those with and without sarcopenic obesity. Our results show that the high rate of chronic disease and multi-morbidity is of concern in this cohort and is probably reflective of the high prevalence of obesity. This demonstrates the need for targeting obesity and non-communicable diseases in LMIC settings.
Low-grade chronic inflammatory status is associated with obesity and sarcopenia and may represent increased risk for developing cardiometabolic diseases [20, 22, 54]. The current study showed that higher levels of systemic inflammation (as indexed by CRP) were associated with sarcopenic obesity, which is supported by a recent meta-analysis that showed that sarcopenia is associated with higher CRP, but not with higher IL-6 or TNFα [22]. Notably, CRP was associated with lower grip strength, but not muscle mass, which suggests that the inflammatory contribution to sarcopenic obesity may reflect muscle quality rather than quantity. Indeed, studies in older men and women (> 60 years) reported that higher baseline levels of IL-6 and CRP increased the risk for loss of strength over 3 years [55]. Accordingly, higher systemic concentrations of CRP may reflect higher adiposity in those with sarcopenia or sarcopenic obesity [19]. Women have higher relative adipose tissue compared to men and this may also explain previous data showing an independent association between low grade systemic inflammation (as indexed by CRP) and muscle strength in older women, but not men [56]. Consequently, sarcopenia may originate from processes such as age-related changes in body fat and body fat distribution, with the consequent low-grade chronic inflammatory state suggested to exacerbate progression of the disease [22].
Our results showed that a more food secure environment and financially supporting more children were part of the characteristic profile that described the sarcopenic obese cohort. National data from SA reports that 26% of the population regularly experience hunger and a further 28% are at risk of hunger, with access to food, household income and social protection (i.e. social grants for child support) all determining factors of food security [17]. Furthermore, socioeconomic status affects behavioural (i.e. PA and diet) characteristics [17, 18]. The present study shows an association between sarcopenic obesity and increased food security, suggesting a higher socioeconomic status, but lower PA and higher sedentary behaviour profile. Although dietary variables did not discriminate between those with and without sarcopenic obesity, we paradoxically showed that those who had a lower grip strength consumed more animal protein foods and less cooked porridge. Although these findings are difficult to explain, we hypothesise that either 1) the animal protein foods were of poor quality (i.e. processed meats, meat cuts with high fat content) and/or 2) those sufficiently affluent to buy meat and animal based products did less daily PA, which may impact on strength. However, longitudinal data is required to assess these hypotheses. Specifically, additional sources of high-quality protein that are sustainable, affordable and culturally appropriate for low-income communities (i.e., red meat, poultry, fish, dairy, soy, nuts seeds and legumes) in combination with a physically active lifestyle may preserve muscle mass and function in older adults [57, 58]. In a low-income setting, plant-based protein is the most affordable source and further research is required to determine the effects it has on the overall prevention of sarcopenia and sarcopenic obesity in these high-risk communities.
Socioeconomic status within low-income communities may influence PA patterns and overall cardiovascular fitness [17, 18, 59]. Previous research in older adults in highly developed countries have shown increased risk for all-cause mortality with higher sedentary time [60], and accumulating a higher percentage of sedentary time in bouts of > 60 min [61]. The current study showed that increased sitting time in bouts of 60 min rather than total daily sitting time were characteristics of the sarcopenic obese participants and were related to a lower grip strengthBMI. The odds of being abdominally obese increases by 6.8% up to 48% for each 60 min sedentary bout increment [62]. Therefore, sedentary behaviour may also reflect higher levels of adiposity rather than sarcopenia per se. Regardless, higher adiposity in the current study was clearly associated with characteristics of sarcopenia. When considering the impact of sedentary behaviour on health-related outcomes, time spent being physically active, regardless of intensity also needs to be considered [60]. Importantly, a maximal risk reduction for all-cause mortality in older adults is observed at 7500 steps/day, 375 min/day of light PA, or 24 min/day of MVPA [60, 63]. In the present study, the mean daily step count of those without sarcopenia (7574 steps/day) was above the daily recommended step count for older adults, while those with sarcopenia were below, with a mean daily step count of 6037 steps/day. Although both groups were below the recommended light PA and MVPA recommendations, the sarcopenic group spent ~ 30 min/day less time in total MVPA and light PA compared to those without sarcopenia. Accordingly, our results suggest that increasing PA, while interrupting sedentary time can be collectively targeted for intervention-based research for the overall prevention of sarcopenic obesity.
Limitations
The current study presents several limitations that need to be considered when interpreting the results. The cross-sectional nature of the study does not allow an assessment of causation. Thus, longitudinal and interventional studies are required in this population to extend the current descriptive findings. Although the HFIAS has been validated for use in South Africa, limitations with the access component of the questionnaire have been identified and expectations of possible financial or food aid influence results towards a more affirmative response [64]. The convenience sampling included few sarcopenic participants without obesity; however, the obesity prevalence reflects national data of older SA women, but these data may not be reflective of women in SA without obesity. Further, this study attempted to recruit an equal number of men and women, however there were major challenges with the recruitment, retention and compliance of the men, resulting in the capturing of incomplete data on only n = 25 men. This is common in epidemiological studies in SA and represent a significant limitation to the present study and current literature [65, 66]. Accordingly, these data can only be extrapolated to older black SA women. Larger cohort studies are required across Africa to understand the burden that sarcopenia and sarcopenic obesity may pose on the ageing population in LMIC.
Conclusions
Collectively, we propose that the criterion presented by the FNIH is a feasible option for classifying sarcopenia in older, obese African women. The high prevalence of sarcopenia, obesity and multimorbidity demonstrate the need for sustainable interventions in these communities to reduce the burden on the health care system and to ensure that quality of life is maintained with ageing. Accordingly, targeting PA and dietary behaviours at a younger age should be a focus in LMIC to not only prevent obesity related multi-morbidities, but also sarcopenia.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
The GBD. 2015 obesity collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
Cesari M, Landi F, Vellas B, Bernabei R, Marzetti E. Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci. 2014;6:192–5.
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB, et al. Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc. 2007;55(5):769–74.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol Ser A Biol Med Sci. 2006;61(10):1059–64.
Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50(5):889–96.
Tomlinson DJ, Erskine RM, Morse CI, Winwood K, Onambélé-Pearson G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology. 2016;17(3):467–83.
Zengin A, Jarjou LM, Prentice A, Cooper C, Ebeling PR, Ward KA. The prevalence of sarcopenia and relationships between muscle and bone in ageing West-African Gambian men and women. J Cachexia Sarcopenia Muscle. 2018;9(5):920–8.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosisReport of the European working group on sarcopenia in older PeopleA. J Cruz-Gentoft et al Age Ageing. 2010;39(4):412–23.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–7 e2.
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–56.
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol Series A: Biomedical Sciences and Medical Sciences. 2014;69(5):547–58.
Alley DE, Shardell MD, Peters KW, McLean RR, Dam TTL, Kenny AM, et al. Grip strength cutpoints for the identification of clinically relevant weakness. J Gerontol Series A: Biomedical Sciences and Medical Sciences. 2014;69(5):559–66.
Ameye H, Swinnen J. Obesity, income and gender: the changing global relationship. Global Food Security. 2019;23:267–81.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
National Department of Health SSA, South African Medical Research Council, ICF. South Africa Demographic and Health Survey 2016: key indicators. NDoH, Stats SA, SAMRC and ICF Pretoria, South Africa and Rockville, Maryland; 2017.
Haysom G, Crush J, Caesar M. The urban food system of Cape Town, South Africa. Waterloo, ON: Hungry Cities Partnership; 2017.
Shisana O, Labadarios D, Rehle T, Simbayi L, Zuma K, Dhansay A, et al. The South African National Health and Nutrition Examination Survey (SANHANES-1). Cape Town; 2014. Report No.: 0796924767.
Auyeung TW, Lee JSW, Leung J, Kwok T, Woo J. Adiposity to muscle ratio predicts incident physical limitation in a cohort of 3,153 older adults—an alternative measurement of sarcopenia and sarcopenic obesity. Age. 2013;35(4):1377–85.
Morley JE, Abbatecola AM, Argiles JM, Baracos V, Bauer J, Bhasin S, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc. 2011;12(6):403–9.
Shad BJ, Wallis G, Van Loon LJC, Thompson JL. Exercise prescription for the older population: the interactions between physical activity, sedentary time, and adequate nutrition in maintaining musculoskeletal health. Maturitas. 2016;93:78–82.
Bano G, Trevisan C, Carraro S, Solmi M, Luchini C, Stubbs B, et al. Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas. 2017;96:10–5.
Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol. 2018;14(9):513–37.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101.
Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci. 2000;904(1):437–48.
Kruger HS, Micklesfield LK, Wright HH, Havemann-Nel L, Goedecke JH. Ethnic-specific cut-points for sarcopenia: evidence from black south African women. Eur J Clin Nutr. 2015;69:1–7.
Kruger HS, Havemann-Nel L, Ravyse C, Moss SJ, Tieland M. Physical activity energy expenditure and sarcopenia in black south African urban women. J Phys Act Health. 2016;13(3):296–302.
Smit W, de Lannoy A, Dover RVH, Lambert EV, Levitt N, Watson V. Making unhealthy places: the built environment and non-communicable diseases in Khayelitsha. Cape Town Health & Place. 2016;39:196–203.
Wang H, GBD demographics collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1160–203.
Raut MK. Global age-specific denominator estimation for monitoring of health and nutrition SDGs and indicators based on population projections of the UN world population prospects, 2017 revision, for the year 2018. Int J Community Med Public Health. 2019;6(1):177.
Prado CMM, Wells JCK, Smith SR, Stephan BCM, Siervo M. Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr. 2012;31(5):583–601.
World Health Organization. Waist circumference and waist–hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008. Geneva: World Health Organization; 2011. http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf.
Goedecke JH, Micklesfield LK, Levitt NS, Lambert EV, West S, Maartens G, et al. Effect of different antiretroviral drug regimens on body fat distribution of HIV-infected south African women. AIDS Res Hum Retrovir. 2013;29(3):557–63.
Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity. 2012;20(5):1109–14.
World Health Organisation (WHO). WHO scientific group on the assessment of osteoporosis at primary health care level. Paper presented at: Summary meeting report; 2004.
Lake JE. The fat of the matter: obesity and visceral adiposity in treated HIV infection. Current HIV/AIDS Reports. 2017;14(6):211–9.
Hawkins KL, Brown TT, Margolick JB, Erlandson KM. Geriatric syndromes: new frontiers in HIV and sarcopenia. AIDS. 2017;31(Suppl 2):S137.
Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. The Gerontologist. 2006;46(3):367–76.
Coates J, Swindale A, Bilinsky P. Household food insecurity access scale (HFIAS) for measurement of food access: indicator guide. Washington, DC: food and nutrition technical assistance project, academy for educational Development; 2007. p. 34.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–5.
World Health Organization (WHO). Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System (WHO/NMH/NHD/MNM/1122011. Accessed 18 Aug 2020.
Sousa-Santos AR, Amaral TF. Differences in handgrip strength protocols to identify sarcopenia and frailty-a systematic review. BMC Geriatr. 2017;17(1):238–59.
Duncan RP, Combs-Miller SA, McNeely ME, Leddy AL, Cavanaugh JT, Dibble LE, et al. Are the average gait speeds during the 10 meter and 6 minute walk tests redundant in Parkinson disease? Gait Posture. 2017;52:178–82.
Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.
SAFOODS. SAMRC Food Quantities Manual for South Africa. Cape Town: South African Medical Research Council; 3rd Edition. 2018.
SAFOODS. SAMRC Food Composition Tables for South Africa. Cape Town: South African Medical Research Council; 5th Edition. 2017.
Wentzel-Viljoen E, Laubscher R, Vorster HH. Changes in food intake from 2005 to 2010 by a cohort of black rural and urban African men and women in the north West Province of South Africa: the PURE-NWP-SA study. Public Health Nutr. 2018;21(16):2941–58.
Bylesjö M, Rantalainen M, Cloarec O, Nicholson JK, Holmes E, Trygg J. OPLS discriminant analysis: combining the strengths of PLS-DA and SIMCA classification. J Chemometrics: A Journal of the Chemometrics Society. 2006;20(8–10):341–51.
Eriksson L, Trygg J, Wold S. CV-ANOVA for significance testing of PLS and OPLS® models. J Chemometrics: A Journal of the Chemometrics Society. 2008;22(11–12):594–600.
Jonsson P, Björkblom B, Chorell E, Olsson T, Antti H. Statistical loadings and latent significance simplify and improve interpretation of multivariate projection models. bioRxiv. 2018;350975. https://doi.org/10.1101/350975.
Kalula SZ, Ferreira M, Swingler GH, Badri M. Risk factors for falls in older adults in a south African Urban Community. BMC Geriatr. 2016;16(1):51–62.
Yeung SSY, Reijnierse EM, Pham VK, Trappenburg MC, Lim WK, Meskers CGM, et al. Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2019;10(3):485–500.
Pradhan AD, Manson JAE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. J Am Med Assoc. 2001;286(3):327–34.
Schaap LA, Pluijm SMF, Deeg DJH, Visser M. Inflammatory markers and loss of muscle mass (sarcopenia) and strength. Am J Med. 2006;119(6):526 e17-e17.
Hamer M, Molloy GJ. Association of C-reactive protein and muscle strength in the English longitudinal study of ageing. Age. 2009;31(3):171–7.
Adesogan AT, Havelaar AH, McKune SL, Eilittä M, Dahl GE. Animal source foods: sustainability problem or malnutrition and sustainability solution? Perspective matters. Global Food Security. 2020;25:100325.
van Vliet S, Burd NA, van Loon LJC. The skeletal muscle anabolic response to plant-versus animal-based protein consumption. J Nutr. 2015;145(9):1981–91.
Tomaz SA, Davies JI, Micklesfield LK, Wade AN, Kahn K, Tollman SM, et al. Self-reported physical activity in middle-aged and older adults in rural South Africa: levels and correlates. Int J Environ Res Public Health. 2020;17(17):6325–37.
Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. Br Med J. 2019;366:l4570.
Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Safford MM, et al. Patterns of sedentary behavior and mortality in US middle-aged and older adults: a national cohort study. Ann Intern Med. 2017;167(7):465–75.
Judice PB, Silva AM, Sardinha LB. Sedentary bout durations are associated with abdominal obesity in older adults. J Nutr Health Aging. 2015;19(8):798–804.
Lee IM, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of step volume and intensity with all-cause mortality in older women. JAMA Intern Med. 2019;179(8):1105–12.
Deitchler M, Ballard T, Swindale A, Coates J. Validation of a measure of household hunger for cross-cultural use. Washington, DC: Food and Nurtrition Technical Assistance II Project (FANTA-2), Acedemy for Educational Development; 2010.
Peer N, Steyn K, Lombard C, Lambert EV, Vythilingum B, Levitt NS. Rising diabetes prevalence among urban-dwelling black south Africans. PLoS One. 2012;7(9):e43336.
Motala AA, Esterhuizen T, Gouws E, Pirie FJ, Omar MAK. Diabetes and other disorders of glycemia in a rural south African community: prevalence and associated risk factors. Diabetes Care. 2008;31(9):1783–8.
Acknowledgements
The authors would like to thank all participants who volunteered for this project. We would also like to thank our research workers Rasematla Sina Motadi and Nandi Magwaca.
Funding
Running costs for this study was funded by the Medical Research Council Confidence in Global Nutrition and Health Research (No.MR/R020221/1).
Author information
Authors and Affiliations
Contributions
Conception and design of research: All authors. Performed Experiments: AEM, JHG, FAOW. Analysed data: AEM, JHG, LKM. Interpreted results of experiments: All authors. Prepared figures: AEM. Drafted and revised manuscript: All authors. Approved final version of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics clearance was approved by the University of Cape Town’s Human Research Ethics Committee (HREC ref. no: 095/2018) and the NHS, Invasive or Clinical Research Committee at the University of Stirling (NICR:17/18). The study was performed in accordance with the principles of the Declaration of Helsinki (1964, amended last in Fortaleza Brazil, 2013), ICH Good Clinical Practice (GCP), and the laws of South Africa. Verbal and written informed consent were obtained from all participants prior to participant screening and all testing procedures.
Consent for publication
Not applicable.
Competing interests
The author(s) declare that they have no completing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mendham, A.E., Goedecke, J.H., Micklesfield, L.K. et al. Understanding factors associated with sarcopenic obesity in older African women from a low-income setting: a cross-sectional analysis. BMC Geriatr 21, 247 (2021). https://doi.org/10.1186/s12877-021-02132-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02132-x