Abstract
Background
The purpose of this study was (1) to develop a virtual reality (VR) intervention program based on the psychological needs of patients residing in nursing facilities in South Korea to alleviate their behavioral and psychological symptoms and (2) to confirm the possibility of utilizing VR in patients with dementia.
Methods
In the first phase, patients with dementia residing in nursing homes and experiencing behavioral and psychological symptoms were recruited. Surveys and questionnaires were used to identify activities that alleviated the behavioral and psychological symptoms of dementia (BPSD) among the patients. These activities were classified into five types of psychological needs. In the second phase, a fully immersive, interactive, easy-to-use VR platform was developed that reflected these psychological needs. Patients with dementia experienced the VR content. The researchers assessed the level of the participants’ immersion, preference, and interaction with the VR using a 5-point Likert scale.
Results
In the feasibility test, 10 nursing home residents were recruited. The mean immersion score was 4.93 ± 0.16 points, the mean preference score was 4.35 ± 0.41 points, and the mean interaction score was 3.84 ± 0.43 points using a 5-point Likert scale. Higher mean scores indicated a more positive outcome. Six of the 10 participants required assistance while using the VR. The mean VR experience duration was 10.00 ± 3.46 min.
Conclusions
The VR-based intervention program that was developed to reduce BPSD was feasible for the participants and provided them with a high degree of satisfaction and immersion. Furthermore, this study also confirmed the convenience and safety of the program. These findings support the potential use of VR-based BPSD intervention programs to treat patients with dementia.
Similar content being viewed by others
Background
The number of people with dementia is rapidly increasing due to the aging of the global population. According to Alzheimer’s Disease International, in 2018, there were 50 million individuals with dementia globally, which represents a 6% increase from 2015 [1]. In South Korea, the prevalence of dementia in persons 65 years and older, as of 2018, was 10.1%, and the number has continued to increase [2].
Patients with dementia experience cognitive dysfunction and various behavioral and psychological symptoms, such as nervousness, depression, psychosis, yelling, and violence [3, 4]. Due to their loss of social and communication skills and limitations in their ability to undertake physical activity, patients with dementia experience issues in their relationships with others. This can exacerbate negative emotions and behavioral and psychological issues in older patients with dementia [5, 6]. The behavioral and psychological symptoms of dementia (BPSD) are one of the most significant reasons why those with dementia receive early admission into nursing facilities [7]. The early institutionalization into a nursing home leads to higher social costs and a lower quality of life for patients with dementia and their families [8].
Interventions that decrease BPSD include non-pharmacological interventions that focus primarily on reducing and removing the psychosocial or environmental risk factors associated with behavioral and psychological symptoms [9] and therapeutic approaches, such as recall therapy, horticultural therapy, music therapy, art therapy, animal-assisted therapy, and physical exercise [10,11,12]. However, it is difficult to apply existing non-pharmacological interventions to patients with dementia and decreased cognitive function. The application of these interventions is restricted due to a lack of trained professionals [13]. To overcome these restrictions, multisensory virtual reality (VR) platforms may be used to improve cognitive function and rehabilitation in patients with dementia, as VR platforms are advanced, adaptable, and easy-to-use [14,15,16,17,18]. VR refers to technologies that allow people to experience realistic situations or environments that are difficult to experience in reality [19, 20]. In particular, immersive VR can be used to focus on certain sensory stimuli and has been reported to facilitate positive emotions and improvements in their emotional state, interpersonal interactions, and communication [21,22,23].
The motivation to use VR may differ between individuals based on individual interests and preferences, aside from maladjustment to VR [13]. The psychological needs of people with dementia include comfort, identity, attachment, occupation, and inclusion [24]. While studies on patient-centered dementia care have considered these needs [25,26,27,28], very few studies have developed activities or interventions for dementia patients that consider their psychological needs.
This study involved three phases. The objective of the first phase was to confirm the activities that alleviate BPSD and classify these activities based on the patients’ psychological needs. The objective of the second phase was to develop VR platform environments based on the patients’ psychological needs and test whether it alleviates BPSD. The objective of the final phase was to evaluate the participants’ VR immersion, preferences and interactions with VR, and tolerance for VR.
Methods
Ethics approval and consent to participate
The project was approved by the Institutional Review Board of the Catholic University of Korea (MC18QNSI0055). Before participation, the researchers obtained written informed consent from each patient and the patient’s legal guardian or representative. The participants were recruited by recruitment notices posted in facilities after obtaining approval from the institution’s managers. Once identified, the mental health expert manager spoke with the patients to see whether they would agree to be contacted for participation in the study. Once agreed, we contacted the participants’ legal guardians or representatives to recruit the participants and obtain consent to participate. The participants were assured of the anonymity and confidentiality of all data collected and given an opportunity to ask questions. To overcome the short-term memory problems and variable capacity, the participants were informed of their right to withdraw at any stage from the study without giving a reason.
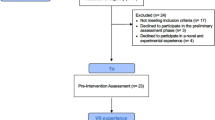
Phase 1: psychological needs to alleviate symptoms
This phase identified the psychological needs that alleviate the symptoms of the patients using polling surveys and questionnaires. The data source was a large-scale research project focused on BPSD to develop an intervention program for improving quality of life. In this study, the convenience sampling method was used, and details of the sampling process have been previously reported in Park et al. [29]. Patients with dementia were recruited from six nursing homes located in two cities. Participants’ preferred environment for intervention development was investigated. Their quality of life and symptoms of psychological impairment were measured to verify the effect of the intervention program. In this study, the data selection process was as follows. Among the recruited 325 participants, participants who reported behavioral and psychological symptoms were selected. Of these participants, only those who answered the questions addressing the activities that alleviated their BPSD were included. Based on this, 103 participants were included in the study, and 222 participants were excluded from the study.
A survey question addressed the activities that alleviated BPSD in patients: “When you feel agitation, aggression, psychosis, depression, and apathy, what activities make you feel better or alleviate your BPSD?” If the participant could not answer the question, the question was completed by asking the care staff who had been caring for the participant for at least 4 weeks (Additional file 1). The care staff responded with their observations on behalf of the patients. The answers were sorted and compiled into response categories and subcategories. Additionally, qualitative data from the participants’ narratives were analyzed thematically based on the psychological needs of patients with dementia [30,31,32].
Based on the five psychological needs of dementia patients [30], the activities were classified into the character-strengthening aspects of comfort (being free from distress and pain, experiencing reduced anxiety by receiving tenderness and friendliness, and feeling soothed), identity (having a sense of self, knowing details of their life history, knowing who one is in relation to significant others, and having a sense of continuity with the past), attachment (feeling security and safety, and trust), occupation (having a purpose in life and being empowered to have an impact), and inclusion (a feeling of belonging, being encouraged to interact with the social environment physically and emotionally). Two independent researchers (A and B) classified the alleviating activities based on the psychological needs of patients with dementia.
Phase 2: development of a VR intervention
The VR was designed using the analysis of psychological needs that alleviate BPSD, which was explored in Phase 1. The VR project was then implemented through collaboration with an external company that had the resources, experience, and time to meet the study requirements.
Design of VR and participants’ actions
The VR content was developed to fulfill the five psychological needs (comfort, identity, attachment, occupation, and inclusion) of the patients with dementia to strengthen the participants’ personality. The following sections detail the content and interactive factors of the VR experience (Table 1).
The VR was designed to meet the comfort needs of the participants, including physical touch (patting a friend on the shoulder), place of memory, forming a quiet environment, and walking. Identity needs were met by visiting family and viewing family pictures, while the inclusion needs were reflected in conversation, being with someone, positive expression, and words/expressions of acknowledgment. Attachment needs included hanging out with friends and family, and the occupation needs included selecting a destination that the patients wanted to visit, erasing graffiti, going grocery shopping, playing with dogs, and putting logs into a fireplace.
With the theme of “Train of memories,” this study implemented VR in 15 different places using four categories. The participant could choose the content via hand movements, and the content was categorized into “Streets of memory,” “Nostalgic youth,” “Homely hometown,” and “Where I want to go.” In the “Train of memories,” the participant could choose their destination by handing a train ticket to the train station attendant and could enjoy the scenery of the old train station. In the “Streets of memory,” the program depicted elementary schools of the past, neighborhood alleys, and old houses, and the participants experienced slap-match games in alleyways with friends, erasing graffiti on school blackboards, playing with puppies at home, and seeing family photos. “Nostalgic youth” included watching an old film at a theater, drinking tea in a traditional coffee house, and going home after shopping for groceries at a traditional market. “Homely hometown” allowed the participants to experience interactions such as playing in a river, stroking reed grass while walking in a breezy field, and placing kindling in a fireplace in a rural home. “Where I want to go” included visual and auditory stimuli, such as orchards, Namiseom Island, the sea at night, observing the rain, and the Jungnogwon Bamboo Garden. There were no intellectual or functional demands required during interactions with the virtual environment.
Multimedia technological design and implementation
Through collaboration with the external company, we created an interactive VR program for relieving BPSD. This intervention provided a fully immersive audio-visual experience of the different virtual environments. Sound, music, photos, and movies were added, in addition to anecdotes and verbal cues. To meet the psychological needs of older people with dementia, the content consisted of different environments, music, and natural sounds suitable for fostering the positive emotions of South Koreans.
The VR program was implemented using 360-degree video viewing, a 360-degree camera recording of the natural environment, editing, and graphics production, which maximized the reality and immersion. The interactions were implemented by attaching a leap motion to the Head Mounted Display (HMD; Samsung HMD Odyssey Windows Mixed Reality Headset plus Wireless controller), allowing for easy recognition of the participants’ hand movements. The seasons and various animated objects could be manipulated through leap motion sensors (LM-010), allowing the participants to interact with the scene through hand and arm movements. Particular movements moved animated objects, such as train tickets, blackboard erasers, slap cards, puppies, teacups, radishes, valley water, reeds, and firewood. The participants did not need to use joysticks or keyboards (Fig. 1).
Some screenshots from virtual reality interactions in this study: a) in “Train of memories,” a participant handing a train ticket to the train station attendant, b) in “Streets of memory,” a participant playing with puppies while playing bowls at home, c) in “Nostalgic youth,” a participant shopping for groceries at a traditional market, d) in “Homely hometown,” a participant placing kindling in a fireplace in a rural home
The platform allowed for overall easy solo use at home or with some assistance, thereby ensuring the platform’s safety. The participants were seated next to their caregiver or a research assistant throughout the VR session; postural demands were reduced by the participants remaining in their chair during the VR exercises.
Phase 3: feasibility test
Procedures
In Phase 3, the participants were also recruited through recruitment notices in residential and daycare facilities for older people. The participants were selected based on the following criteria: (1) they were a resident or daycare visitor with dementia, (2) they were aged 65 years or above, (3) they had a Mini Mental Status Examination-Korean version (MMSE-K) score of 15 or higher, (4) they had a Clinical Dementia Rating of 0.5 or higher, and (5) they understood the research process and agreed to participate. The exclusion criteria consisted of motor dysfunction due to cerebral infarction, other mental disorders, neurological disorders, and metabolic disorders. A total of 10 participants were recruited.
The VR-based intervention programs were provided to the participants in the program rooms of the institutions in 1–2 sessions for 20–30 min each. The intervention times were customized for the participants; lunch hours, visiting hours, and napping hours were avoided.
The participants’ age, MMSE-K scores, and Activities of Daily Life (ADL) scores were obtained from their medical records. The MMSE-K scores ranged from 0 to 30, with higher scores indicating better cognition and a score below 24 indicating cognitive impairment [33].
The participants used the VR at their own pace after receiving guidance from the trained researchers. They were guided to specific places they wanted to visit and experienced two to three VR places. To assess the immersion, preference, and interaction during the VR experience, the researchers asked the participants to respond to three questions relating to immersion, preferences, and degree of interaction in their VR experiences on a 5-point Likert scale (1 = “Very poor,” 2 = “Poor,” 3 = “Fair,” 4 = “Good,” 5 = “Excellent”) in every place they chose. Higher mean scores indicated a more positive experience, and the answers to these questions were obtained through the structured questionnaire.
To identify the participants’ tolerance for VR, the researchers recorded the need for assistance, duration of the VR experience, positive or negative experiences, and VR sickness (Additional file 2). Positive or negative experiences were measured by their visual alertness and verbal engagement. The following negative behaviors were recorded: complaining, agitation, wandering, hitting, grabbing, pushing, throwing objects, biting, hurting self or others, tearing objects or destroying property, and making physical/verbal sexual advances. The following positive behaviors were recorded: remaining seated and still, being focused, being calm, smiling, and communicating verbally or non-verbally. Two researchers observed and recorded the participants’ responses, and disagreements between their ratings were resolved by discussion and reaching a consensus. For the statistical analyses of the data, SPSS Statistics 27.0 was used, and these included frequency and descriptive analyses, in which the means, standard deviations, medians, and interquartile ranges (IQR) were analyzed.
Results
Activities that alleviate BPSD
Activities that alleviated BPSD among the patients were characterized and classified into five types of psychological needs. The need for “comfort” was rated highest in terms of providing relief from BPSD, with 36.9% out of a total of 103 patients making this assessment, followed by the need for “identity” (28.2%), “inclusion” (24.3%), “attachment” (10.7%), and “occupation” (6.8%). Activities related to the need for comfort included walking, eating snacks, physical contact (such as hugging and holding hands), and creating a quiet environment. Activities related to the need for identity included religious activities and visits from guardians and family members. Activities related to the need for inclusion involved receiving positive support from others. Activities related to the need for attachment included checking objects (checking their clothes and placing a name sticker on personal closets). Activities related to the need for occupation included reading, solving puzzles, and playing traditional South Korean card games (Table 2).
Immersion, preference, and interaction during VR experience
All participants were female. The mean age of the participants was 85.80 ± 3.26 years (Min 82 ~ Max 90, Median [IQR] 85.5 [84.25–88.75]). The participants had a mean MMSE-K score of 21.44 ± 4.59 points (Median [IQR] 22 [18.00–24.00]) and a mean ADL score of 4.33 ± 2.88 points out of 30 points (Median [IQR] 5 [1.75–6.00]).
As the participants engaged with the VR program, the researchers observed the level of the participants’ immersion, preference, and interaction with the VR on a 5-point Likert scale. The mean immersion score was 4.93 ± 0.16 points (Median [IQR] 5.00 [4.87–5.00]), the mean preference score was 4.35 ± 0.41 points (Median [IQR] 4.65 [3.84–4.90]), and the mean interaction score was 3.84 ± 0.43 points (Median [IQR] 3.85 [3.58–4.30]) in each of the virtual places.
Tolerance for VR experience
There were multiple indicators of VR tolerance. First, six out of the 10 participants required assistance, such as help with wearing the HMD, focusing their visual acuity on the HMD glasses, and capturing their hand movements via leap motion. The mean VR experience duration was 10.00 ± 3.46 min. The participants’ reactions throughout the VR were classified into positive or negative outcomes. Seven participants had positive responses to VR, while the remaining three had both positive and negative responses. The positive reactions included pleasure, such as focusing on the program for a set period, laughing, and communicating verbally and non-verbally in a stable state. Negative emotions were recorded as the occurrence of complaining (Table 3).
Discussion
The purpose of this study was (1) to develop a VR intervention program based on the psychological needs of patients residing in South Korean nursing facilities, (2) to test whether this VR intervention alleviates BPSD, and (3) to confirm the utilization of VR in patients with dementia. This program aims to improve the patients’ quality of life and provide effective care models for health professionals.
The VR program was designed to meet the participants’ psychological needs by securing their emotional immersion and engagement in accordance with the preferences and emotions of South Koreans. Comfort needs were most frequently suggested as a way to alleviate the patients’ behavioral and psychological symptoms. Patients with dementia maintain their identity through love and comfort, which provides them with a greater sense of well-being [34, 35]. Patients with dementia obtain happiness and enjoyment by engaging in meaningful activities, such as various leisure activities, social participation, and work-related activities, which improve the individual’s sense of autonomy and identity [36, 37]. When their psychological needs were satisfied, their anxiety and behavioral psychological symptoms decreased [38, 39], and such reductions have been effective in reducing the need for neuroleptics [16]. Additionally, this VR environment provides a multimedia platform that can facilitate the storage and retrieval of memories and simulate multisensory experiences. This could be used to create a therapeutic environment for alleviating BPSD.
The VR content developed in this study was applied to patients with dementia, and the evaluations were subsequently obtained from the participants’ immersion, preference, interaction, and tolerance for VR. The participants’ feedback was consistent with previous results demonstrating that patients with dementia participated more keenly in activities that reflected their individual preferences [35] and activities that they could recall and reminisce about [40,41,42,43]. A high degree of preference and immersion were confirmed among the participants, demonstrating the usability of the VR intervention program. This indicates that it is important for VR platforms to present a familiar environment, given the historical and cultural backgrounds of patients with dementia. Furthermore, intervention programs that reflect familiarity and various emotional stimuli can increase immersion and contribute to active interactions by helping the participants reminisce and recall the past [44].
Manera et al. [15, 45] reported that older individuals with mild cognitive disorders or Alzheimer’s disease had higher levels of satisfaction and reported less anxiety, discomfort, and fatigue with image-based VR exercises compared to paper and pencil exercises. The results of these studies indicate that well-developed VR content can be effectively applied to patients with dementia and mild cognitive impairment and can result in positive outcomes [46].
Despite these promising results, the usability problems of the VR system developed in this study need to be solved. In terms of the experience length, this varied from 5 to 15 min. This was because the participants chose different themes, and their interaction pace varied. The theme “street of memories” was selected the most, which included an elementary school, an alleyway, and a homely house. The theater and coffee house were selected the least. Considering that the participants’ mean age was 85.80 years, watching movies in the theater and drinking coffee in a café might not be preferred activities for these participants. Therefore, historical and cultural characteristics should be considered to develop immersive VR programs [47].
In this feasibility study, there were issues related to the assistance required to use the VR: the weight of the HMD (Samsung HMD Odyssey Windows Mixed Reality Headset and Wireless controllers 630 g), controlling the visual acuity, and capturing the participants’ hand movements via leap motion. The participants displayed difficulties operating the VR with hand movements mostly likely because of the decreased hand movement and cognitive functions of the older patients [48]. The patients complained of limited vision while wearing the HMD as they are cut off from the outside world; they also complained about the heavy weight of the displays [20]. The weight of the HMD is 590 g, which is relatively lighter than other HMDs; even lighter HMDs for older patients will be released in the future (e.g., HP Reverb G2). The VR environment requires active movement and the use of visual and auditory senses. This may be limited in older people with dementia since they typically experience reduced visual and auditory capacity, resulting in decreased accuracy and attention [5]. The results of this study indicate that the participants experienced some difficulties due to their diminished sensory capacity. This should inform the design, implementation, and evaluation of similar technologies or interventions. For instance, physical functions, such as visual acuity and hand power, and the weight of the HMD should be considered for the use of VR technology with dementia patients.
In the current study, VR sickness varied with two participants complaining about dizziness or nausea during the VR immersion. The VR intervention program test was implemented while the participants were seated, which decreased the effort required to maintain their posture. Clearer images and accurate motion tracking can reduce VR sickness [49, 50], and content requiring less movement [51] is less likely to lead to VR sickness. Although these symptoms are temporary [52], researchers and developers need to pay attention to this issue.
This feasibility study aimed to uncover the strengths and weaknesses of VR interventions. The findings demonstrate that it is feasible to use VR with patients with dementia but did not demonstrate the efficacy of VR to reduce BPSD. Further research should be conducted based on rigorous experimental design to build more evidence for VR intervention programs. High-quality methodological and experimental studies are required to demonstrate the effectiveness of randomized controlled trials and should be designed to include a control group of dementia patients as a long-term intervention program in a nursing home.
Typically, VR platforms have been underutilized in healthcare services for groups such as patients with chronic diseases or people with disabilities [53]. This is the first study to develop VR interventions for dementia patients by considering their psychological needs. Overall, this study has demonstrated that VR could increase immersion, preference, interaction, and tolerance, but such effects vary with the nature of the task. Moreover, unlike previous studies, this study demonstrated that a low demand VR environment that facilitates the storage and retrieval of preferred memories could permit the implementation of strategies to facilitate patients’ interactions. While VR-based programs have issues, such as high costs, difficulty in operating the system, space constraints, and low portability [54, 55], the VR program employed in this study increased the convenience and safety of use by using simple interactive motions, such as pointing one’s hand in the desired direction and avoiding the need for large and complex hardware.
Limitations and implications of the study
This study was a feasibility test with a limited sample. Future studies should recruit a large sample of participants and consider factors such as age, gender, personality type, and severity of dementia. Additionally, we used the trained researchers’ observations to screen the negative and positive responses during VR experience among the participants. The participants’ minor discomfort could not be reported because we did not use a standard measure. Researchers should continue to explore the potential discomfort of VR or sickness related to VR among the participants with cognitive decline using various measures such as self-reported questionnaires and standardized observations. In this study, there may have been some response bias since the researchers and assessors were the same. After completing the intervention, collecting immediate feedback from participants with moderate-to-severe dementia can be challenging since they struggle to respond to these types of questions. A mixed-methods approach involving semi-structured interviews and observational data should be used to assess their responses in future studies.
However, the VR-based intervention program developed in this study to reduce BPSD was feasible for the participants and provided them with a relatively high degree of satisfaction and immersion. Furthermore, this study also confirmed the convenience and safety of the program. These findings build evidence for the potential utility of VR programs to alleviate BPSD.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- BPSD:
-
Behavioral and psychological symptoms of dementia
- VR:
-
Virtual reality
- MMSE-K:
-
Mini mental status examination-korean version
- ADL:
-
Activities of daily life
- HMD:
-
Head mounted display
References
Patterson C. World Alzheimer report 2018: the state of the art of dementia research: new frontiers. London: Alzheimer’s Disease International (ADI); 2018.
National Institute of Dementia. Korean dementia observation. 2020. https://www.nid.or.kr/info/dataroom_view.aspx?bid=209. Accessed 20 Aug 2020.
Desai AK, Schwartz L, Grossberg GT. Behavioral disturbance in dementia. Curr Psychiatry Rep. 2012;14(4):298–309.
Bessey LJ, Walaszek A. Management of behavioral and psychological symptoms of dementia. Curr Psychiatry Rep. 2019;21(8):66.
Yuill N, Hollis V. A systematic review of cognitive stimulation therapy for older adults with mild to moderate dementia: an occupational therapy perspective. Occup Ther Int. 2011;18(4):163–86.
Tible OP, Riese F, Savaskan E, von Gunten A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther Adv Neurol Disord. 2017;10(8):297–309.
Song JA, Park JW, Kim HJ. Impact of behavioral and psychological symptoms of dementia on caregiver burden in nursing homes. J Korean Gerontol Nurs. 2013;15(1):62–74.
Wang HX, MacDonald SW, Dekhtyar S, Fratiglioni L. Association of lifelong exposure to cognitive reserve-enhancing factors with dementia risk: a community-based cohort study. Plos Med. 2017;14(3):e1002251.
Gitlin LN, Kales HC, Lyketsos CG. Nonpharmacologic management of behavioral symptoms in dementia. JAMA. 2012;308(19):2020–9.
Hsieh CJ, Chang C, Su SF, Hsiao YL, Shih YW, Han WH, Lin CC. Reminiscence group therapy on depression and apathy in nursing home residents with mild-to-moderate dementia. J Exp Clin Med. 2010;2(2):72–8.
Majić T, Gutzmann H, Heinz A, Lang UE, Rapp MA. Animal-assisted therapy and agitation and depression in nursing home residents with dementia: a matched case–control trial. Am J Geriatr Psychiatry. 2013;21(11):1052–9.
Hsu MH, Flowerdew R, Parker M, Fachner J, Odell-Miller H. Individual music therapy for managing neuropsychiatric symptoms for people with dementia and their carers: a cluster randomised controlled feasibility study. BMC Geriatr. 2015;15(1):84.
Scales K, Zimmerman S, Miller SJ. Evidence-based nonpharmacological practices to address behavioral and psychological symptoms of dementia. Gerontologist. 2018;58(suppl_1):S88–S102.
Anderson AP, Mayer MD, Fellows AM, Cowan DR, Hegel MT, Buckey JC. Relaxation with immersive natural scenes presented using virtual reality. Aerosp Med Hum Perform. 2017;88(6):520–6.
Manera V, Chapoulie E, Bourgeois J, Guerchouche R, David R, Ondrej J, Drettakis G, Robert P. A feasibility study with image-based rendered virtual reality in patients with mild cognitive impairment and dementia. Plos One. 2016;11(3):e0151487.
McEwen D, Taillon-Hobson A, Bilodeau M, Sveistrup H, Finestone H. Two-week virtual reality training for dementia: single-case feasibility study. J Rehabil Res Dev. 2014;51(7):1069.
Moyle W, Jones C, Dwan T, Petrovich T. Effectiveness of a virtual reality forest on people with dementia: a mixed methods pilot study. Gerontologist. 2018;58(3):478–87.
Zygouris S, Ntovas K, Giakoumis D, Votis K, Doumpoulakis S, Segkouli S, Karagiannidis C, Tzovaras D, Tsolaki M. A preliminary study on the feasibility of using a virtual reality cognitive training application for remote detection of mild cognitive impairment. J Alzheimers Dis. 2017;56(2):619–27.
Jeong BY. Current status and implications of virtual reality ecosystem. Korea Information Soc Dev Ins. 2016;28(7):1–23.
de Vries AW, Willaert J, Jonkers I, van Dieën JH, Verschueren M. Virtual reality balance games provide little muscular challenge to prevent muscle weakness in healthy older adults. Games Health J. 2020;9(3):227-36.
Baker R, Bell S, Baker E, Holloway J, Pearce R, Dowling Z, Thomas P, Assey J, Wareing LA. A randomized controlled trial of the effects of multi-sensory stimulation (MSS) for people with dementia. Br J Clin Psychol. 2001;40(1):81–96.
Verkaik R, van Weert JC, Francke AL. The effects of psychosocial methods on depressed, aggressive and apathetic behaviors of people with dementia: a systematic review. Int J Geriatr Psychiatry. 2005;20(4):301–14.
Sánchez A, Millán-Calenti JC, Lorenzo-López L, Maseda A. Multisensory stimulation for people with dementia: a review of the literature. Am J Alzheimers Dis Other Dement. 2013;28(1):7–14.
Kitwood T. Dementia reconsidered: the person comes first. Open University Press Buckingham 1997;20.
McIntosh C, Westbrook J, Sheldrick R, Surr C, Hare DJ. The feasibility of dementia care mapping (DCM) on a neurorehabilitation ward. Neuropsychol Rehabil. 2012;22(6):920–41.
Yoshihara M. Person centered care research in Japan: have we traced kitwood or not? Osaka Prefecture Univ. 2015;66:39–52. https://doi.org/10.24729/00003047.
Doi T, Kuwahara N, Morimoto K. Assessing the use of communication robots for recreational activities at nursing homes based on dementia care mapping (DCM). International Conference on Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management; 2016. p. 203–11.
Schaap FD, Dijkstra GJ, Finnema EJ, Reijneveld SA. The first use of dementia care mapping in the care for older people with intellectual disability: a process analysis according to the RE-AIM framework. Aging Ment Health. 2018;22(7):912–9.
Park E-Y, Park S-M, Kim J-H. Psychometric properties of the geriatric quality of life-dementia in older adults with dementia or mild cognitive impairment living in nursing homes. BMC Geriatr. 2019;19(1):281.
Kitwood T. Positive long-term changes in dementia: some preliminary observations. J Ment Health. 1995;4(2):133–44.
Song JA, Park M, Park J, Cheon HJ, Lee M. Patient and caregiver interplay in behavioral and psychological symptoms of dementia: family caregiver’s experience. Clin Nurs Res. 2018;27(1):12–34.
Polenick CA, Struble LM, Stanislawski B, Turnwald M, Broderick B, Gitlin LN, Kales HC. “I’ve learned to just go with the flow”: family caregivers’ strategies for managing behavioral and psychological symptoms of dementia. Dementia. 2020;19(3):590–605.
Lee KS, Cheong HK, Oh BH, Hong CH. Comparison of the validity of screening tests for dementia and mild cognitive impairment of the elderly in a community: K-MMSE, MMSE-K, MMSE-KC, and K-HDS. J Korean Neuropsychiatr Assoc. 2009;48(2):61–9.
Vernooij-Dassen M, Leatherman S, Olde Rikkert M. Quality of care in frail older people: the balance between receiving and giving. BMJ. 2011;342(7806):1062–3.
Vernooij-Dassen M, Moniz-Cook E. Person-centred dementia care: moving beyond caregiving. Aging Ment Health. 2016;20(7):667–8.
Phinney A, Chaudhury H, O’connor DL. Doing as much as I can do: the meaning of activity for people with dementia. Aging Ment Health. 2007;11(4):384–93.
Han A, Radel J, McDowd JM, Sabata D. Perspectives of people with dementia about meaningful activities: a synthesis. Am J Alzheimers Dis Other Dement. 2016;31(2):115–23.
Sloane PD, Hoeffer B, Mitchell CM, McKenzie DA, Barrick AL, Rader J, Stewart BJ, Talerico KA, Rasin JH, Zink RC. Effect of person-centered showering and the towel bath on bathing-associated aggression, agitation, and discomfort in nursing home residents with dementia: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(11):1795–804.
Cohen-Mansfield J, Libin A, Marx MS. Nonpharmacological treatment of agitation: a controlled trial of systematic individualized intervention. J Gerontol A Biol Sci Med Sci. 2007;62(8):908–16.
Kovach CR, Henschel H. Planning activities for patients with dementia: a descriptive study of therapeutic activities on special care units. J Gerontol Nurs. 1996;22(9):33–8.
Buettner LL, Fitzsimmons S. Activity calendars for older adults with dementia: what you see is not what you get. Am J Alzheimers Dis Other Dement. 2003;18(4):215–26.
Cohen-Mansfield J, Marx MS, Thein K, Dakheel-Ali M. The impact of past and present preferences on stimulus engagement in nursing home residents with dementia. Aging Ment Health. 2010;14(1):67–73.
Lopes TS, Afonso RMLBM, Ribeiro OM. A quasi-experimental study of a reminiscence program focused on autobiographical memory in institutionalized older adults with cognitive impairment. Arch Gerontol Geriatr. 2016;66:183–92.
Moon S, Park K. The effect of digital reminiscence therapy on people with dementia: a pilot randomized controlled trial. BMC Geriatr. 2020;20:1–11.
Manera V, Petit P-D, Derreumaux A, Orvieto I, Romagnoli M, Lyttle G, David R, Robert PH. ‘Kitchen and cooking,‘a serious game for mild cognitive impairment and Alzheimer’s disease: a pilot study. Front Aging Neurosci. 2015;7:24.
Corriveau Lecavalier N, Ouellet É, Boller B, Belleville S. Use of immersive virtual reality to assess episodic memory: a validation study in older adults. Neuropsychol Rehabil. 2020;30(3):462–80.
Jung GJ, Park JM, Lee GG, Chong MK, Sim HB, Lee J, Han H. Reminiscence reflecting cultural background in Korean older adults with dementia: a concept analysis. J East-West Nurs Res. 2018;24(2):110–8.
Grenier S, Forget H, Bouchard S, Isere S, Belleville S, Potvin O, Rioux M-E, Talbot M. Using virtual reality to improve the efficacy of cognitive-behavioral therapy (CBT) in the treatment of late-life anxiety: preliminary recommendations for future research. Int Psychogeriatr. 2015;27(7):1217.
Shin J, An G, Park JS, Baek SJ, Lee K. Application of precise indoor position tracking to immersive virtual reality with translational movement support. Multimed Tools Appl. 2016;75(20):12331–50.
Ray B, Jung J, Larabi M-C. On the possibility to achieve 6-DoF for 360 video using divergent multi-view content. 2018 26th European Signal Processing Conference (EUSIPCO); 2018. p. 211–5.
Guna J, Geršak G, Humar I, Song J, Drnovšek J, Pogačnik M. Influence of video content type on users’ virtual reality sickness perception and physiological response. Future Gener Comput Syst. 2019;91:263–76.
Weech S, Kenny S, Barnett-Cowan M. Presence and cybersickness in virtual reality are negatively related: a review. Front Psychol. 2019;10:158.
Coyle H, Traynor V, Solowij N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: systematic review of the literature. Am J Geriatr Psychiatry. 2015;23(4):335–59.
Cherniack EP. Polyphenols: planting the seeds of treatment for the metabolic syndrome. Nutrition. 2011;27(6):617–23.
Lee JH. A study on the revitalization of virtual reality-based education. KSDC. 2019;25(1):357–66.
Acknowledgments
Not applicable.
Funding
This work was supported by a Korea Research Foundation grant funded by the South Korean Government (MOEHRD, Basic Research Promotion Fund; NRF-2017R1E1A1A01075188). The funder had no role in the study design, data collection, data analysis, interpretation of data, presentation of results, or decision to submit for publication.
Author information
Authors and Affiliations
Contributions
JH contributed to the study’s conception, conducted the statistical analysis and interpretation of the data, and drafted the manuscript. SM and HJ interpreted the data and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of Catholic University (MC18QNSI0055) reviewed and approved the study protocol. The data were collected after participants provided written informed consent. The participants were assured anonymity and confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Open-ended questions for primary caregivers; Observation and records for patients with MCI or Dementia.
Additional file 2.
Observation and records for patients with MCI or Dementia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, JH., Park, S. & Lim, H. Developing a virtual reality for people with dementia in nursing homes based on their psychological needs: a feasibility study. BMC Geriatr 21, 167 (2021). https://doi.org/10.1186/s12877-021-02125-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-021-02125-w