Abstract
Background
Management of patients with polypharmacy is challenging, and evidence for beneficial effects of deprescribing interventions is mixed. This study aimed to investigate whether a patient-centred deprescribing intervention of PCPs results in a reduction of polypharmacy, without increasing the number of adverse disease events and reducing the quality of life, among their older multimorbid patients.
Methods
This is a cluster-randomised clinical study among 46 primary care physicians (PCPs) with a 12 months follow-up. We randomised PCPs into an intervention and a control group. They recruited 128 and 206 patients if ≥60 years and taking ≥five drugs for ≥6 months. The intervention consisted of a 2-h training of PCPs, encouraging the use of a validated deprescribing-algorithm including shared-decision-making, in comparison to usual care. The primary outcome was the mean difference in the number of drugs per patient (dpp) between baseline and after 12 months. Additional outcomes focused on patient safety and quality of life (QoL) measures.
Results
Three hundred thirty-four patients, mean [SD] age of 76.2 [8.5] years participated. The mean difference in the number of dpp between baseline and after 12 months was 0.379 in the intervention group (8.02 and 7.64; p = 0.059) and 0.374 in the control group (8.05 and 7.68; p = 0.065). The between-group comparison showed no significant difference at all time points, except for immediately after the intervention (p = 0.002). There were no significant differences concerning patient safety nor QoL measures.
Conclusion
Our straight-forward and patient-centred deprescribing procedure is effective immediately after the intervention, but not after 6 and 12 months. Further research needs to determine the optimal interval of repeated deprescribing interventions for a sustainable effect on polypharmacy at mid- and long-term. Integrating SDM in the deprescribing process is a key factor for success.
Trial registration
Current Controlled Trials, prospectively registered ISRCTN16560559 Date assigned 31/10/2014.
The Prevention of Polypharmacy in Primary Care Patients Trial (4P-RCT).
Similar content being viewed by others
Background
Management of multimorbid patients, the majority of whom are treated by primary care physicians (PCP), is challenging [1,2,3,4]. A major issue in this predominantly old population is polypharmacy, commonly defined as the intake of five or more drugs per capita, which entails the risk of adverse drug reactions [5,6,7,8]. This subsequently leads to an increase in morbidity [9, 10], hospital admissions [11,12,13], health-related costs and ultimately, the number of deaths [14,15,16].
Several clinical deprescribing tools and strategies for different healthcare providers (pharmacists, physicians, nurses) [17,18,19,20,21,22,23,24,25], mostly for the inpatient setting and using computer-assisted decision aids, have been tested [26]. The communication about patients’ needs and preferences in the process of deprescribing is challenging and a patient-centred approach, taking into account these topics, is of utmost importance to enable safe and effective deprescribing [27,28,29,30,31]. One of the first landmark trials using this approach by Garfinkel and Mangin in 2010, introduced the Good Palliative-Geriatric Practice (GPGP) algorithm [32]. Studies with PCP-lead interventions in the primary care setting, including shared-decision-making (SDM) and long-term, follow up are still scarce.
According to previous studies of deprescribing efficiency, the impact of these interventions on clinically relevant endpoints, e.g. falls, use of health care facilities, morbidity or mortality, is often small or even nonexistent and varies [18, 19, 33, 34]. Furthermore, complex deprescribing interventions are challenging to implement in the primary care setting, e.g. due to time restrictions or structural shortcomings [17, 35, 36]. Thus, there is a need for effective and feasible approaches to reduce inappropriate polypharmacy in primary care, with an emphasis on acceptance and implementation into routine care [28, 37]. Therefore we designed a foreshorten, paper-based intervention to tackle two of the major barriers in the primary care setting especially common in Switzerland, time and lack of uniform digital solutions in practices [38, 39]. This study aimed to investigate whether a patient-centred deprescribing intervention of GPs results in a reduction of polypharmacy, without increasing the number of adverse disease events and reducing the quality of life, among their older multimorbid patients.
Methods
Design
We conducted a two-armed, cluster-randomised, clinical trial in Swiss primary care practices from January 1, 2015, to June 1, 2017.
Participants
We invited German-speaking, officially registered PCPs working in ambulatory primary care practices from northern Switzerland stepwise by canton (region) by letter to participate. We stratified enrolled PCPs as clusters by practice to avoid contamination. Approximately one-half of the clusters were randomised to the intervention (n = 22) and one-half to control group (n = 24). After randomisation PCPs received the allocated training session (see below), before identifying eligible patients by reviewing their daily patient list. We asked PCPs to recruit a maximum of 15 patients. They received an expense allowance of 100 CHF per recruited patient.
PCPs continuously recruited patients independent of race or ethnicity whenever they fulfilled the following criteria: a) cared for by one of the participating PCPs b) ≥60 years of age c) ≥ 5 chronic drugs for ≥ 6 months d) capable of judgement. Enrolled patients were blinded to the study arm insofar as blinding was guaranteed by randomisation on PCP level. See the study flowchart to visualise the patient selection process (Fig. 1).
Intervention description
Intervention on PCP level (training session)
In the intervention group, PCPs received a lecture (length: 2 h) on polypharmacy and trained the use of our deprescribing-algorithm and to discuss its results with their patients (SDM). This intervention could take place immediately after obtaining informed consent or in a separate consultation. We adapted the Good Palliative-Geriatric Practice (GPGP) algorithm, which is a deprescribing tool developed for and tested in a geriatric setting [32]. Adaption meant simplifying from six to four key questions to answer. See Fig. 2 for details. We previously pilot-tested this adapted algorithm to assess its feasibility and practicability in the primary care setting [40].
In the control group, PCPs received a general lecture (length: 2 h) on multimorbidity and instructions for collecting usual care data. For blinding purposes, we informed PCPs that the study purpose was to investigate best practices for physician-patient communication.
Intervention on patient-level (during the first encounter)
After obtaining informed consent from the patient, a practice-nurse, or the PCP created a list of the patient’s current medication. Then, the PCP defined the four main diagnoses and a list of the four most important complaints in consensus with the patient, to facilitate prioritisation of treatment goals. PCPs in the intervention group then decided for every single drug listed if it was appropriate for the patient, according to the algorithm (Fig. 2).
Based on these questions, the PCP made a recommendation for each drug. In an SDM procedure that followed the PCPs recommendation, the PCP and patient then decided together what changes to implement, always with the option to restart if symptoms should increase or if the disease should deteriorate. PCPs used a checklist, including many individual steps to guide the first consultation (see Additional file 1 for details). The SDM procedure was guaranteed by the stepwise character of the algorithm, including the task of SDM itself.
Time points and outcomes
Time points are defined as follows:
Pre-Intervention T0 (before the first consultation, previously also named baseline), Post-Intervention T1 (at the end of the first consultation), after 6-Months T2, and after 12-Months T3.
Primary outcome
Mean difference in the number of drugs per person (DPP) between Pre-Intervention and after 12 months.
Secondary outcomes
Mean difference in the number of dpp between Pre-Intervention and Post-Intervention
-
2.1
Mean difference in the number of dpp between Pre-Intervention and after 6 months
-
2.2
Number of drugs with PCP’s recommendation to change and what kind of change (either stopping, dose change or alternative drug)
-
2.3
Frequency of discrepant decisions between PCP and patient about the change of a drug, and therapeutic groups of drugs patients were not willing to change
-
2.4
Number of dpp taken without the PCPs knowledge, at Pre-Intervention
-
2.5
Symptom scores, rates of hospitalisation, death and unexpected clinical events
-
2.6
Quality of life rating by the patients at Pre-Intervention, after 6 and 12 months
-
2.7
Time consumption due to the intervention, by the practice nurse and by PCP
For further details, including interim analysis and stopping guidelines, see study protocol [41].
Measures
PCPs and patients collected data on pre-coded paper documents (Additional file 1) at the four-time points. PCPs stored the codes identifying the individual patient in their practice. Data transfer to the electronic database was carried out and double-checked by two research associates.
We categorised diagnoses according to an adapted version of a classification system by van den Bussche et al. [42] For coding of complaints we used ICPC-2 coding [43] and for drugs the ATC code [44]. We compared diagnosis and complaints as perceived by PCPs and patients based on ratings. (For details and results see [45]). Patients reported QoL, as well as the symptom score of the worst complaint on paper format all three consultations. We used three different tools to document QoL:
-
a)
five-point Likert-scale ranging from − 2 to + 2, with − 2 the worst possible, + 2, the best possible,
-
b)
a visual analogue scale (VAS) ranging from 0 to 100 to document their current health status, with 0 the worst possible, 100 the best possible, and
-
c)
the “functional” EQ-5D-3L set of questions concerning topics of mobility/activity, self-catering, general activities, pain/physical complaints and fear/depression [46]. Patients reported symptoms on a scale ranging from 0 (no symptoms) to 10 (worst symptoms possible). We asked PCPs to report all hospitalisations and deaths as well as all other clinical events they considered essential for our study on a pre-coded paper form, on which more detailed information on the events` character, the context and the consequences were required, as well as the PCPs probability estimate of the causal relationship between the previous deprescribing procedure and the event. In case of drop- out, patients̀ data gathered so far were computed.
Additionally, to those characteristics above, we collected the following patient and PCP characteristics. For patients: Age [years], sex (PCP classified), number of drugs and living situation. For PCPs: Age [years], sex (investigator classified), working experience [years], type of practice [single or group] and affiliation to physician network [yes or no]. We used the web-based data management program SecuTrial® (version 5.0.1, 2016) [47]. We applied CONSORT guidelines for reporting of all data and visualisation of study flow [48].
Statistical analysis
We randomised in blocks, making sure PCP’s from the same practice were in the same group to prevent contamination. Freely available software named “randomization.com” was used [49].
We performed power calculations for the study’s primary outcome, with a power of 80%, a two-sided alpha-error of 2.5%, a cluster effect of 2% [50], a standard error of 2.8 and an assumed effect size of 0.8 dpp (based on our pilot) [40] and an assumed drop-out rate of 10%.
For the descriptive analysis of PCPs’ and patients’ characteristics, we used frequencies and percentages for categorical variables, and for continuous variables means and standard deviation (SD) or median and interquartile range (IQR). To compare groups with categorical variables, we used the Chi-square test or Fisher’s exact test. For comparison of groups and times with continuous variables, we used Welch’s t-test or Mann-Whitney-U test. We provided p-values and 95% confidence intervals (95%-CI). We used the statistical program R® Version 3.5 37.
As a sensitivity analysis, we calculated the deprescribing rate, defined as the proportion of the number of drugs stopped at a given time point in relation to the number of drugs at baseline, for each time point after Pre-Intervention. We compared the rates between groups using Chi-square test or Fisher’s exact test. The distribution of drugs which were recommended to change by the PCP and those with a patient’s agreement to the recommendation was calculated.
Results
Mean age of the 334 included patients (128 intervention group/ 206 control group) was 76.2 (SD 8.5) years, 136 (45.5%) females, taking 8.05 (SD 2.5) dpp, with no significant differences between groups. Drop-out rates were 9.3% (31 of all patients), 6.0% (20 of all patients) due to death and 3.3% (11 of all patients) due to the change of attending PCP. Mean age of 46 participating PCPs was 49.4 (SD 9.3), 30 (65%) males, working for 13.6 (SD 9.7) years in private practice. (For further details see Additional file 2 and (25)) The main therapeutic drug classes were cardiovascular (30% of all drugs), neurologic-analgetic (15.6%) and anticoagulant (8.7%) drugs at baseline. Rates of drugs stopped were 41.7% for cardiovascular, 14.8% for neurologic-analgetic and 8.3% for anticoagulant drugs. For further details on drugs, see Additional file 3.
The mean difference in the number of dpp between Pre-Intervention and after 12 months (primary outcome) was 0.379 in the intervention group (8.02 at Pre-Intervention and 7.64 after 12 months; p = 0.059) and 0.374 in the control group (8.05 at Pre-Intervention and 7.68 after 12 months; p = 0.065). For the time points Post-Intervention and after 6 months, there was a significant reduction in dpp in the intervention group (p = < 0.001 and 0.002). In the control group, there was no significant change in the number of dpp over all time points. In the between-group comparison, there was no significant difference at all time points, except for Post-Intervention (p = 0.002) (Fig. 3). For further details, see Table 1.
The deprescribing rates at T2 and T3 were between 23.9 and 29.0% in the intervention group and between 14.0 and 21.5% in the control group (p < 0.001 for difference) (Additional file 4).
Intervention group PCPs recommended changes of drugs in 209 (20.5%) of all 1019 drugs at baseline. In 170 (81.3%) of these 209 recommendations, patients implemented a change. One hundred five drugs were stopped, and 85 (81%) of them remained stopped after 12 months.
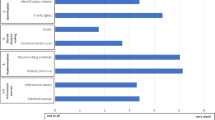
On PCP level, the agreement of patients to the recommended drug changes was 86% (weighted mean per centre 0.858, SD 0.231) (Fig. 4).
Recommended drug changes and agreement. Number of drug changes recommend per primary care physician during the first consultation (T0). This recommendation Red bar shows the number of drugs recommend for change by the primary care physician and the blue bar shows the number of drugs on which the patient and the primary care physician agreed to proceed with the recommended change
PCPs reported that no drugs were taken without their previous knowledge at Pre-Intervention. For more information on drug classes that were stopped, restarted and started due to a new indication, see Fig. 5 and Additional file 5.
During the follow-up period, 43 (33.6%) of patients were hospitalised in the intervention group compared to 54 (26.2%) in the control group (p = 0.32 for between-group difference), and seven (5.5%) patients died in the intervention group compared to 13 (6.3%) in the control group (p = .95 for between-group difference) See Table 2 for details.
Mean QoL values on 0–100 point scale at the three-time points were between 65.9 and 67.2 for the intervention group and between 65.0 and 69.0 for the control group, with no significant difference between groups (p from 0.270 to 0.383) and between time points. A significant increase in the QoL value in the control group between baseline and after 12 months (p = 0.025) was the only exception. Mean QoL on Likert-scale, and functional EQ-5D-3L showed no significant difference between time points or groups. For further details, see Table 3.
Overall time consumption of PCPs and nurses during the first consultation was 30.1 (SD 10.7) minutes in the intervention and 27.1 (SD 13.84) minutes in the control group (p = 0.066).
Discussion
In our study population of older community-dwelling patients with polypharmacy, the use of a straight-forward and patient-centred deprescribing procedure was effective immediately after the intervention, but not after 6 and 12 months) compared to the control group providing usual care. Clinical events, hospitalisations and death rates, as well as QoL measures, were not significantly different between groups at all time points.
Effectiveness over time
Our intervention resulted in a statistically significant immediate reduction in the number of drugs per patient, and 81% of all drugs stopped during the intervention consultation remained stopped after 12 months. However, the reduction in the total number of drugs was not preserved over time due to new prescriptions.
A probable reason might be our study population of old and multimorbid patients. As previously shown by Lam and others, this population is at high risk for new diseases, clinical events, hospitalisations and symptoms. Almost two-thirds of all patients faced either a clinical event or hospitalisation during the follow-up period, leading to new drugs and multiple drugs changes [51,52,53] (Table 2, Additional file 3). This natural course of diseases and consecutive drug treatment may dilute the overall impact of the intervention over time. As previously recommended by Dills et al., our results encourage repeated deprescribing interventions to reach a sustainable mid- and long-term effect, [54].
Safety and quality of life
Whenever deprescribing interventions are carried out, it is of utmost importance not to harm patients or deteriorate their QoL. As a non-inferiority safety measure, we found no negative impact of the intervention on clinical events, hospitalisations or deaths. Regarding QoL, resulting levels are in line with previously reported results in multimorbid patients in the Swiss primary care setting [55], but lower than those in the general population [32, 56,57,58]. Most importantly, the QoL results of the two groups in our study did not differ statistically significantly (Table 3)., thus reflecting that the deprescribing intervention was not inferior to usual care regarding QoL, i.e. did not lower the QoL of patients. Therefore we can conclude that the PCPs have deprescribed appropriately, without taking the risk of clinical or subjective deterioration of the patient.
However, the functional EQ-5D-3L QoL score decreased in both groups, likely due to the natural loss of function caused by ageing. (Table 3). As stated by Rickert et al. in their latest paper, the fact, the reduction of drugs did not increase harm to patients, can be seen as a positive result in itself [59].
Importance of SDM
The results of our study emphasise that an individualised approach and interaction with the patient is crucial for a successful and sustainable deprescribing. We ensured individualisation and interaction with the patient, by mean of addressing and prioritising patients’ subjective complaints in addition to medical diagnosis. Furthermore, we integrated SDM into the deprescribing algorithm. Our finding that patients agreed to a drug change in 86% of drugs recommended to change (on PCP level) indicates a high adherence towards the intervention, and we believe that this mainly due to focus on SDM during the deprescribing process. PCPs not only have frequent patient consultations and thus windows of opportunity to tackle polypharmacy together with their patient, but are also highly trusted by patients, as previously reported in a paper by our study group [60]. Mutual trust facilitates SDM procedures, resulting in more successful deprescribing [29, 60,61,62,63]. Von Buedingen et al., also using an SDM approach, reported a similar high adherence of patients towards their initial decision [52, 64, 65]. Page et al. came to a similar conclusion in their extensive systematic review on the feasibility and effect of deprescribing in older patients, highlighting the importance of patient-specific individualised approaches such as ours using SDM as the central mean of an intervention [18].
Barriers towards deprescribing
However, several psychological barriers are hindering a minority of patients from implementing drug changes [27, 66, 67]. We reported several reasons for a disagreement of or our study patients with the recommendations of PCP elsewhere [60]. The open discussion of deprescribing barriers is essential, to find solutions and to increase the efficacy of the deprescribing interventions [27]. This discussion and finding consent again is an integral part of the SDM process.
Time constraint is another major deprescribing barrier [17, 27, 35]. Our consultation duration was twice as long as an average encounter in the Swiss healthcare system, probably reflecting the task of dealing with multimorbid and complex patients, requiring more consultation time compared to the average ambulatory care population [68,69,70]. However, the duration did not differ significantly between groups. We conclude that our straight-forward study intervention itself did not require additional time which is supporting the feasibility of the intervention.
Another barrier is the fact that some PCPs may be reluctant to use a paper-based or digital “stand-alone” deprescribing algorithm. The integration of our procedure in existing electronic medical records and decision aids remains a promising option for further implementation while keeping in mind that this step is challenging and might induce potential new barriers [39, 59].
Strengths
First, to our knowledge, the 12 months follow-up of this study is among the longest in deprescribing research and this setting. Second, we hardly selected our study population, resulting in a population of patients mainly living independently at home. Thus, thinking in terms of dissemination and public health impact, our findings may help to deal with older outpatient PCP population with polypharmacy.
Limitations
First, we cannot rule out a selection bias of PCPs with a commitment for deprescribing and patient-centred communication style above-average volunteering more frequently for study participation. Otherwise, we believe the trial findings are generalisable for older patients in an industrialised outpatient primary care setting. Thus one must always bear in mind that the primary care setting is quite different between countries. Second, although the cluster-randomisation performed on PCP level resulted in an equal number of PCPs in both groups, the number of patients in the two groups varied noticeably, with fewer patients in the intervention group. Besides the fact that the protocol defined a maximum number of patients per PCP but not a minimal one, there is no apparent reason for this. However, we cannot rule out a potential association between the intervention procedure and the smaller number of patients in the intervention group. If we assume causality, this would be a limitation regarding the feasibility of the intervention. Third, we did not control for continuous patient recruitment by PCPs, thus cannot rule out a selection bias on patient level. Fourth, we cannot exclude an underreporting bias of clinical events, as long-term impacts of discontinuing drugs may sometimes require a longer time than our follow-up of 12 months.
Conclusion
Our straight-forward and patient-centred deprescribing procedure is effective immediately after the intervention, but not after 6 and 12 months. Finding the ideal interval for repetition of deprescribing interventions will allow archiving sustainable mid and long term effects. Integrating SDM in the deprescribing process is a crucial factor for success.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files. We will additionally share a minimal anonymised data set necessary to replicate our study findings. See Additional file 6, which includes an additional data description.
Abbreviations
- DPP:
-
drugs per patient
- GPGP:
-
Good Palliative-Geriatric Practice
- IQR:
-
interquartile range
- PCPs:
-
primary care physicians
- QoL:
-
quality of life
- SDM:
-
Shared decision making
- SD:
-
standard deviation
- VAS:
-
visual analogue scale
References
Rizza A, et al. Age- and gender-related prevalence of multimorbidity in primary care: the Swiss FIRE project. BMC Fam Pract. 2012;13:113.
Wallace E, et al. Managing patients with multimorbidity in primary care. BMJ. 2015;350:h176.
Smith SM, et al. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. 2012;345:e5205.
Mc Namara KP, et al. Health professional perspectives on the management of multimorbidity and polypharmacy for older patients in Australia. Age Ageing. 2017;46(2):291–9.
Gallagher P, et al. Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol. 2011;67(11):1175–88.
Wise J. Polypharmacy: a necessary evil. BMJ. 2013;347:f7033.
Sonnichsen A, et al. Polypharmacy in chronic diseases-Reduction of Inappropriate Medication and Adverse drug events in older populations by electronic Decision Support (PRIMA-eDS): study protocol for a randomised controlled trial. Trials. 2016;17:57.
Hamilton HJ, Gallagher PF, O'Mahony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatr. 2009;9:5.
Payne RA, et al. Is polypharmacy always hazardous? A retrospective cohort analysis using linked electronic health records from primary and secondary care. Br J Clin Pharmacol. 2014;77(6):1073–82.
Hakkarainen KM, et al. Modelling drug-related morbidity in Sweden using an expert panel of physicians. Eur J Clin Pharmacol. 2012;68(9):1309–19.
Budnitz DS, et al. Emergency hospitalisations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–12.
Reich O, et al. Potentially inappropriate medication use in older patients in Swiss managed care plans: prevalence, determinants and association with hospitalisation. PLoS One. 2014;9(8):e105425.
The RO, et al. Patterns of multimorbidity and prediction of hospitalisation and all-cause mortality in advanced age. Age Ageing. 2018;47(2):261–8.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalised patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200–5.
Hakkarainen KM, et al. Methods for assessing the preventability of adverse drug events: a systematic review. Drug Saf. 2012;35(2):105–26.
Wauters M, et al. Too many, too few, or too unsafe? Impact of inappropriate prescribing on mortality, and hospitalisation in a cohort of community-dwelling oldest old. Br J Clin Pharmacol. 2016;82(5):1382–92.
Rieckert A, et al. Reduction of inappropriate medication in older populations by electronic decision support (the PRIMA-eDS study): a qualitative study of practical implementation in primary care. BMC Fam Pract. 2018;19(1):110.
Page AT, et al. The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82(3):583–623.
Johansson T, et al. Impact of strategies to reduce polypharmacy on clinically relevant endpoints: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82(2):532–48.
Cooper JA, et al. Interventions to improve the appropriate use of polypharmacy in older people: a Cochrane systematic review. BMJ Open. 2015;5(12):e009235.
Barry PJ, et al. START (screening tool to alert doctors to the right treatment)--an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing. 2007;36(6):632–8.
Lavan AH, et al. STOPPFrail (screening tool of older persons prescriptions in frail adults with limited life expectancy): consensus validation. Age Ageing. 2017;46(4):600–7.
Lenaghan E, Holland R, Brooks A. Home-based medication review in a high risk elderly population in primary care--the POLYMER randomised controlled trial. Age Ageing. 2007;36(3):292–7.
Martinez YV, et al. A set of systematic reviews to help reduce inappropriate prescribing to older people: study protocol. BMC Geriatr. 2017;17(Suppl 1):231.
Willeboordse F, et al. Opti-med: the effectiveness of optimised clinical medication reviews in older people with 'geriatric giants' in general practice; study protocol of a cluster randomised controlled trial. BMC Geriatr. 2014;14:116.
Moxey A, et al. Computerised clinical decision support for prescribing: provision does not guarantee uptake. J Am Med Inform Assoc. 2010;17(1):25–33.
Reeve E, et al. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30(10):793–807.
Mangin D, et al. International Group for Reducing Inappropriate Medication use & Polypharmacy (IGRIMUP): position statement and 10 recommendations for action. Drugs Aging. 2018;35(7):575–87.
Willeboordse F, et al. Patient participation in medication reviews is desirable but not evidence-based: a systematic literature review. Br J Clin Pharmacol. 2014;78(6):1201–16.
Matthys J, et al. Patients' ideas, concerns, and expectations (ICE) in general practice: impact on prescribing. Br J Gen Pract. 2009;59(558):29–36.
Reeve E, et al. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmacol. 2014;78(4):738–47.
Garfinkel D, Mangin D. Feasibility study of a systematic approach for discontinuation of multiple medications in older adults: addressing polypharmacy. Arch Intern Med. 2010;170(18):1648–54.
Beuscart JB, et al. A systematic review of the outcomes reported in trials of medication review in older patients: the need for a core outcome set. Br J Clin Pharmacol. 2017;83(5):942–52.
Ziere G, et al. Polypharmacy and falls in the middle age and elderly population. Br J Clin Pharmacol. 2006;61(2):218–23.
Lugtenberg M, et al. Implementation of multiple-domain covering computerised decision support systems in primary care: a focus group study on perceived barriers. BMC Med Inform Decis Mak. 2015;15:82.
Beeler PE, Bates DW, Hug BL. Clinical decision support systems. Swiss Med Wkly. 2014;144:w14073.
Johansson T, et al. Interventions to reduce inappropriate polypharmacy: implications for research and practice. Maturitas. 2017;97:66–8.
De Pietro C, et al. Switzerland: Health System Review. Health Syst Transit. 2015;17(4):1–288 xix.
Djalali S, et al. Undirected health IT implementation in ambulatory care favors paper-based workarounds and limits health data exchange. Int J Med Inform. 2015;84(11):920–32.
Neuner-Jehle S, Krones T, Senn O. Systematic elimination of prescribed medicines is acceptable and feasible among polymorbid family medicine patients. Praxis (Bern 1994). 2014;103(6):317–22.
The Prevention of Polypharmacy in Primary Care Patients Trial (4P-RCT). ISRCTN Registry, ISRCTN16560559, 2014.
van den Bussche H, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health. 2011;11:101.
Verbeke M, et al. The international classification of primary care (ICPC-2): an essential tool in the EPR of the GP. Stud Health Technol Inform. 2006;124:809–14.
International language for drug utilization research ATC/DDD. WHO Collaborating Centre for Drug Statistics Methodology. https://www.whocc.no/atc_ddd_index/. Accessed 4 Nov 2020.
Neuner-Jehle S, et al. Patient-provider concordance in the perception of illness and disease: a cross-sectional study among multimorbid patients and their general practitioners in Switzerland. Patient Prefer Adherence. 2017;11:1451–8.
EuroQol G. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
secuTrial(R). Available: http://www.secutrial.com/. Accessed 13 May 2019.
Campbell MK, et al. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661.
Available at: http://www.randomization.com/. Accessed 20 June 2019.
Jager C, et al. A tailored implementation intervention to implement recommendations addressing polypharmacy in multimorbid patients: study protocol of a cluster randomised controlled trial. Trials. 2013;14:420.
Lam KD, Miao Y, Steinman MA. Cumulative changes in the use of long-term medications: a measure of prescribing complexity. JAMA Intern Med. 2013;173(16):1546–7.
von Buedingen F, et al. Changes in prescribed medicines in older patients with multimorbidity and polypharmacy in general practice. BMC Fam Pract. 2018;19(1):131.
Potter K, et al. Deprescribing in frail older people: a randomised controlled trial. PLoS One. 2016;11(3):e0149984.
Dills H, et al. Deprescribing Medications for Chronic Diseases Management in Primary Care Settings: A Systematic Review of Randomized Controlled Trials. J Am Med Dir Assoc. 2018;19(11):923–35 e2.
N'Goran AA, et al. Comparing the self-perceived quality of life of multimorbid patients and the general population using the EQ-5D-3L. PLoS One. 2017;12(12):e0188499.
Hinz A, et al. The quality of life questionnaire EQ-5D-5L: psychometric properties and normative values for the general German population. Qual Life Res. 2014;23(2):443–7.
McCaffrey N, et al. Health-related quality of life measured using the EQ-5D-5L: south Australian population norms. Health Qual Life Outcomes. 2016;14(1):133.
Hanlon JT, et al. A randomised, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med. 1996;100(4):428–37.
Rieckert A, et al. Use of an electronic decision support tool to reduce polypharmacy in elderly people with chronic diseases: cluster randomised controlled trial. BMJ. 2020;369:m1822.
Zechmann S, Trueb C, Valeri F, Streit S, Senn O, Neuner-Jehle S. Barriers and enablers for deprescribing among older, multimorbid patients with polypharmacy: an explorative study from Switzerland. BMC Fam Pract. 2019;20(1):64. https://doi.org/10.1186/s12875-019-0953-4.
Palagyi A, et al. Barricades and brickwalls--a qualitative study exploring perceptions of medication use and deprescribing in long-term care. BMC Geriatr. 2016;16:15.
Dhillon AK, et al. General practitioners' perceptions on home medicines reviews: a qualitative analysis. BMC Fam Pract. 2015;16:16.
Schenk A, Eckardt-Felmberg R, Steinhagen-Thiessen E, Stegemann S. Patient behaviour in medication management: findings from a patient usability study that may impact clinical outcomes. Br J Clin Pharmacol. 2020;86(10):1958–68. https://doi.org/10.1111/bcp.13946.
Dalleur O, et al. Reduction of potentially inappropriate medications using the STOPP criteria in frail older inpatients: a randomised controlled study. Drugs Aging. 2014;31(4):291–8.
Garfinkel D, Zur-Gil S, Ben-Israel J. The war against polypharmacy: a new cost-effective geriatric-palliative approach for improving drug therapy in disabled elderly people. Isr Med Assoc J. 2007;9(6):430–4.
Reeve E, Wiese MD. Difficulties reducing inappropriate prescribing of proton pump inhibitors in the elderly. Drugs Aging. 2012;29(11):925–6 author reply 927-8.
Sinnott C, et al. GPs' perspectives on the management of patients with multimorbidity: systematic review and synthesis of qualitative research. BMJ Open. 2013;3(9):e003610.
Litschgi L, Fehr F, Zeller A. Characteristics of consultations by general practitioners in Switzerland - time, topics and verbal behaviour. Praxis (Bern 1994). 2011;100(18):1085–95.
Heiligers PJ, et al. Diagnoses and visit length in complementary and mainstream medicine. BMC Complement Altern Med. 2010;10:3.
Wilson A, Childs S. The relationship between consultation length, process and outcomes in general practice: a systematic review. Br J Gen Pract. 2002;52(485):1012–20.
Hasler S, et al. Effect of a patient-centered drug review on polypharmacy in primary care patients: study protocol for a cluster-randomised controlled trial. Trials. 2015;16:380.
Acknowledgements
We would like to thank Susan Hasler MD, Daniela Grundmann MD, Catrina Waldegg MD and Susan Groth for their contribution towards our study. Similarly, we thank Christine Bewick and Ursula Pinder for their language editing.
Authors` contributions
Acquisition, analysis, and interpretation of data: SZ, OS, FV, SE, CM, TR, SNJ. Drafting of the manuscript: SZ, SNJ, OS. Critical revision of the manuscript for important intellectual content: SZ, OS, FV, SE, CM, TR, SNJ. Statistical analysis: FV. Administrative, technical, or material support: FV. SZ, OS, FV, SE, CM, TR, SNJ have read and approved the submitted version of the manuscript and are personally accountable for the author’s own contributions and ensured that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Funding
“Gottfried and Julia Bangerter-Rhyner Foundation” 8472/ HEG-DSV supported this study. The funding organisations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the Canton of Zurich (reference KEK-ZH-number 2014–0595) reviewed and approved the study protocol [71]. All participating patients gave written consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that no competing interests, including financial and non-financial interests, activities, relationships and affiliations, exist.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PCP consultation checklist. Checklist PCPs of the intervention group used as a guideline and protocol for the first consultation. They documented all pre-interventional medication as well as PCPs recommendation, the PCPs reason for the recommendation and the shared-decision taken by the PCP and the patient.
Additional file 2.
Baseline characteristics. Patient and PCP characteristics at baseline, thereby comparing patients who dropped out to those who finished the study. a) Likert scale ranging from − 2 to + 2, (− 2 the worst possible, + 2, the best possible). b) Visual analogue scale (VAS) ranging from 0 to 100, (0 the worst possible, 100 the best possible) c) EQ-5D-3L scale from 1 to 5 (1 for no problems to 5 extreme or being unable to perform a task).
Additional file 3.
Drug charges in the intervention group. All drugs of invention group patients at baseline and changes due to the invention and during the follow-up.
Additional file 4.
Deprescribing rates over time. Deprescribing rates over time between the two groups at different time points. The deprescribing rate was defined as the proportion of the number of drugs stopped at a given time point in relation to the number of drugs at baseline. N.a. = Not available.
Additional file 5.
Overall drug changes during the study. All options a drug could take during the follow-up time of 12 months. Rows 5 to 8: pathways where drugs were stopped due to the actual intervention, + = drugs listed at this time point, − = drugs not listed at this time point, n.a. = not applicable. Example how to read the table: Option 5 (+/−/+/+) shows the pathway and the number of drugs stopped due to the intervention but restarted after 6 months, and still in place after 12 months.
Additional file 6.
Anonymised data set. A minimal anonymised data set, necessary to replicate our study findings. An additional data description is included.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zechmann, S., Senn, O., Valeri, F. et al. Effect of a patient-centred deprescribing procedure in older multimorbid patients in Swiss primary care - A cluster-randomised clinical trial. BMC Geriatr 20, 471 (2020). https://doi.org/10.1186/s12877-020-01870-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-020-01870-8