Abstract
Background
Yoga is a holistic therapy of expanding popularity, which has the potential to produce a range of physical, mental and social benefits. This trial evaluated the feasibility and effects of an adapted yoga programme on physical function and health-related quality of life in physically-inactive older adults.
Methods
In this randomised controlled pilot trial, 52 older adults (90% female; mean age 74.8 years, SD 7.2) were randomised 1:1 to a yoga programme or wait-list control. The yoga group (n = 25) received a physical activity education booklet and were invited to attend ten yoga sessions during a 12-week period. The control group (n = 27) received the education booklet only. Measures of physical function (e.g., Short Physical Performance Battery; SPPB), health status (EQ-5D) and mental well-being (Warwick-Edinburgh Mental Well-being Scale; WEMWBS) were assessed at baseline and 3 months. Feasibility was assessed using course attendance and adverse event data, and participant interviews.
Results
Forty-seven participants completed follow-up assessments. Median class attendance was 8 (range 3 to 10). At the 3-month follow-up, the yoga group had a higher SPPB total score compared with the control group (mean difference 0.9, 95% confidence interval [CI] -0.3 to 2.0), a faster time to rise from a chair five times (mean difference − 1.73 s, 95% CI −4.08 to 0.62), and better performance on the chair sit-and-reach lower-limb flexibility test (mean difference 5 cm, 95% CI 0 to 10). The yoga group also had superior health status and mental well-being (vs. control) at 3 months, with mean differences in EQ-5D and WEMWBS scores of 0.12 (95% CI, 0.03 to 0.21) and 6 (95% CI, 1 to 11), respectively. The interviews indicated that participants valued attending the yoga programme, and that they experienced a range of benefits.
Conclusions
The adapted yoga programme appeared to be feasible and potentially beneficial in terms of improving mental and social well-being and aspects of physical function in physically-inactive older adults. An appropriately-powered trial is required to confirm the findings of the present study and to determine longer-term effects.
Trial registration
Similar content being viewed by others
Background
Older adults (i.e., aged ≥60 years) who are physically inactive are at increased risk of falls, functional limitations, disability, and mental health problems [1,2,3,4]. Encouragingly, there is evidence that various physical activity interventions can elicit meaningful improvements in physical function and health-related quality of life in older people. Effective programmes have included aerobic exercise [5], progressive resistance training [6] and Tai Chi [7]. Yoga is an alternative approach to improving fitness and health outcomes in older adults.
In the West, the word ‘Yoga’ is the general term used for the practice of ‘Hatha Yoga’. Hatha Yoga is a centuries-old health and well-being system from India that involves a combination of physical postures or poses (asana), breathing exercises (pranayama), integrated breath-movement sequences, relaxation, and concentration/meditation. Many styles of Hatha Yoga have developed over the past few decades due to the global expansion of the teaching conducted by influential instructors such as Iyengar, Desikachar (Viniyoga), Pattabhi Jois (Astanga), Sivananda and Bikram (Hot Yoga). The differences are subtle, but the traditional physical poses (asana) of Hatha Yoga are the same. All Hatha Yoga classes require participants to hold and move between various stationary positions with the goal of developing strength, balance and flexibility. To ensure a total body workout, a mixture of standing, seated, kneeling, supine, and prone stationary positions are used, with transitions incorporating forward bends, back bends, side bends, twists, inversions and balances. All Hatha Yoga styles honour the importance of breathing exercises, mental concentration/meditation and relaxation.
The proposed benefits of regular Yoga practice are many and varied, including increases in muscular strength, flexibility and balance, reduced stress, anxiety and depression, and an enhancement of overall well-being and quality of life [8]. Interestingly, the findings of a systematic review of 16 studies (n = 649) [9] and a more recent trial of 118 participants [10] indicate that Yoga (of various types) may provide greater improvements in physical functioning and self-reported health status than conventional physical activity interventions in elderly people. However, the previous studies had limitations, including small sample sizes, a single Yoga teacher delivering the programme, and short-term follow-up. Furthermore, none of the included studies had been conducted in the United Kingdom.
In 2009, the British Wheel of Yoga (BWY) Gentle Years Yoga© programme was developed in North Yorkshire, England to cater specifically for the needs of older people with age-related conditions such as osteoarthritis, hypertension, dementia, and sensory impairment. Adaptations to challenging Hatha Yoga poses were developed so that inactive older adults with comorbidities and physical limitations could safely participate whilst still reaping the health and well-being benefits of Hatha Yoga. This pragmatic randomised controlled pilot trial represents the first formal evaluation of this programme. Therefore, the aim of this study was to investigate the feasibility of the British Wheel of Yoga (BWY) Gentle Years Yoga© programme in physically-inactive older adults with various comorbidities, as well as its effects on physical function and health-related quality of life.
Methods
Trial design
In this randomised controlled trial, participants were assigned to one of two groups: Yoga programme or wait-list control. Recruitment occurred between February and March 2016, and data collection was performed at the Yorkshire Yoga & Therapy Centre between March and July 2016. The Northumbria University Faculty of Health and Life Sciences Research Ethics Committee approved the study (reference HLSGT180116). The trial was registered with the ClinicalTrials.gov (reference NCT02663726).
Setting and participants
The trial was conducted at a Yoga centre, two community-based facilities, and one care home in North Yorkshire, United Kingdom. Participant recruitment was undertaken via advertising in local newspapers, websites, and newsletters from local community organisations. Individuals were eligible if they were aged 60 years or older, and were willing and able to attend the assessment sessions and Yoga classes. Exclusion criteria included having a medical condition that precludes exercise [11] (e.g., unstable cardiac disease, uncontrolled hypertension, and uncontrolled metabolic diseases), having major surgery scheduled within 3 months of the baseline visit, current participation in >90 min per week of purposeful exercise (self-reported average over the past year), and participation in another clinical trial for which concurrent participation was deemed inappropriate. The presence or absence of these factors was determined by the research team during the first telephone contact with prospective participants. Written, informed consent was obtained for all participants prior to the baseline assessments.
As this was a pilot study, no formal sample size calculation was performed [12]. Instead, we aimed to recruit at least 40 participants within the 2-month recruitment period. We believed this to be a feasible target, and one that would provide useful information for the design of a future definitive randomised controlled trial.
Baseline questionnaire
At the baseline visit, all participants completed a questionnaire that included questions relating to their age, sex, ethnicity, lifestyle habits, employment status, and current medications. In addition, participants were asked to indicate which of 27 comorbidities they suffered from; the list being based on work by Bayliss et al. [13].
Randomisation and interventions
Following completion of baseline assessments, which were all conducted on the same day, participants were randomly allocated in a ratio of 1:1 to Yoga intervention or wait-list control. The randomisation sequence was computer-generated by an investigator who was not involved in the recruitment process and was stratified by site, with one block per site.
All participants received an education booklet about physical activity for older adults [14]. The intervention group was also offered a Yoga programme, free of charge. The wait-list control group were offered the same Yoga programme, free of charge, after the 3-month follow-up assessment.
BWY Gentle Years Yoga© programme
Eight experienced Yoga teachers were recruited and trained for the study. All eight attended free practical training over three consecutive days in BWY Gentle Years Yoga© methods which included Safeguarding Vulnerable Adults training and a Dementia Friends information session. One trainee teacher lived in London and another in York and therefore they did not become teachers in the study which took place in Harrogate District of North Yorkshire, England. All teachers in the study taught the same form of Yoga as outlined in the BWY Gentle Years Yoga© training material. One teacher was selected to deliver each of the four courses, leaving three teachers spare to serve as back-up. Treatment fidelity was assessed through observation of each teacher’s class teaching on two separate occasions by JH, with assessments quality assured by LB. In addition to the three practical days of training (24 guided learning hours), the six teachers did a minimum of 46 h of home study, including assessed written work and exams.
The four Yoga courses were all delivered at different sites: one Yoga centre, two community centres and one care home for residents diagnosed with dementia and other co-morbidities. One of the community centres was located in one of the 20% most-deprived neighbourhoods in England.
Each course involved ten 75-min, group-based classes delivered across a 12-week period (approximately one class per week). The programme introduced participants to the foundational elements of Yoga adapted appropriately for older adults, including asana, pranayama, relaxation techniques, mental focus, and philosophy. Classes consisted of an introduction to the weekly theme, pain-relieving or settling-in relaxing poses, a programme of seated and standing practices, educative postural advice, breath work, concentration activities, and 5 to 15 min of relaxation. Examples of the seated poses used are shown in Fig. 1. Poses targeted stiff, weak, and untrained areas of the whole body, with the intention of improving mobility, strength, and posture and reducing pain. Later classes featured postures that built on previous weeks (in accordance with the training principle of progressive overload), with a key aim of increasing participants’ ability and confidence to perform activities of daily living (e.g. climbing stairs, getting out of a chair).
During the supervised classes, the teachers modified the practices so that each individual could adopt a safe variation of the poses and sequences that would not compromise their health. For example: when the class was performing a forward bend, individuals with osteoporosis were instructed to flex only at the hip and to avoid flexion of the spine; people with hypertension or cardiac conditions learned to modify the angle of the forward bend so that the head was never lower than the heart; people with replacement knees or hips were taught how to perform asana such as utkatasana (or sit-to-stand modification) and virabhadrasana II (seated warrior 2) without jeopardising the artificial joint, and; people with dementia or suspected cognitive impairment were given tools to help them to remember sequences, such as performing actions while singing well-known songs from childhood. The following bullet points summarise how the adapted Yoga classes differ from standard Hatha Yoga classes:
-
For the most part, participants are seated on chairs, and when standing, they use the chair or other aids for support;
-
The classes do not use supine, semi-supine or prone asana; instead, the key elements of traditional supine/prone asana are integrated into seated or standing postures;
-
The classes hold static asana (isometric postures) for a shorter length of time, especially those that could cause more pronounced acute increases in blood pressure;
-
The physical set up of the class has been adapted to suit people with sensory impairment; specifically, participants being relatively close to the instructor, lighting levels being higher, the colour of equipment being in contrast to that of the walls and floor, and no music played during instruction;
-
The pace and overall structure of the class allows greater time for recovery from the more intense activities (e.g. by having a simple breathing practice follow a more-challenging asana);
-
Instructions are in short, single-point sections with time allowed for information processing to facilitate understanding in individuals with cognitive impairment;
-
Longer warm-up and overall slower pace, making it safer for older adults and at a level where they can work without feeling ‘left behind’ or ‘too old for Yoga’, or having their self-confidence eroded;
-
Breathing practices avoid retention, as this is contraindicated for individuals with hypertension;
-
Mobilisation, asana, and concentration exercises (dharana) are incorporated that specifically focus on balance and co-ordination.
Once the teachers were satisfied that the participants knew how to adapt the exercises for their medical conditions, self-practice sheets were distributed and the participants were encouraged to practice selected Yoga activities at home for 10–20 min on most days. As the supervised work in class became progressively more challenging, students were given new information sheets that allowed them to develop their home Yoga routine. There were three information sheets in total, and these were typically distributed in weeks 1, 3 and 6.
Study measures
Outcomes were measured before randomisation and 3 months after randomisation. Assessors were blinded to group assignment. The primary outcome measures were the total score on the Short Physical Performance Battery (SPPB), and performance on the individual components of the SPPB: standing balance, chair sit-to-stand, and 4-m walking time. The SPPB is a functional performance measure that depends on leg strength and balance [15, 16], which were targets of the Yoga programme.
Short Physical Performance Battery (SPPB)
The SPPB combines data from standing balance, time to rise and stand from a seated position 5 times, and time to walk 4 m at a usual pace. Individuals receive a score of 0 for each task they are unable to complete. Scores of 1 to 4 are assigned for remaining tasks, according to established methods [15, 16]. Scores are then summed to obtain a total score ranging from 0 to 12 [15, 16].
For the standing balance component, participants are asked to hold 3 increasingly difficult standing positions for 10 s each: the side-by-side stand, semi-tandem stand (standing with feet parallel and the heel of one foot touching the base of the first toe of the opposite foot), and the full-tandem stand (standing with one foot directly in front of the other) [15, 16]. Scores range from 0 (unable to hold the side-by-side stand for 10 s) to 4 (able to hold the full-tandem stand for 10 s) [15, 16].
For the chair sit-to-stand component, participants sit in a straight-backed chair with arms folded across their chest and stand 5 times consecutively as quickly as possible. Time to complete 5 chair rises is measured [15, 16]. Scores range from 0 (unable to complete 5 chair rises within 60 s) to 4 (able to complete 5 chair rises in ≤11.1 s) [15, 16].
For the walking component, participants are asked to complete a timed 4-m walk at a usual pace. The lowest time (quickest walk) from two valid attempts was recorded at baseline and follow-up. Scores range from 0 (unable to complete) to 4 (able to complete in <4.82 s) [17].
The following variables from the SPPB were analysed: total SPPB score; standing balance time, calculated as the sum of time able to stand in the three positions, up to a maximum of 30 s; chair sit-to-stand time, measured as the time (in seconds) to complete 5 chair rises, and; the time (in seconds) to walk 4 m at a usual pace.
Secondary outcome measures
Secondary outcome measures included body mass and stature (for the calculation of body mass index), waist circumference, resting systolic and diastolic blood pressure (A&D TM-2655P, PMS Instruments Ltd., Berkshire, UK), the EuroQol EQ-5D-5L health index [18], the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) [19], upper- and lower-body flexibility using the back-scratch and chair sit-and-reach components of the Senior Fitness Test [20], respectively, and adverse events.
The EQ-5D-5L is a simple, self-administered measure of health status that comprises two parts. The first part comprises five health dimensions – mobility, self-care, usual activities, pain/discomfort and anxiety/depression – with five levels of severity for each dimension [18]. Together, the five responses represent a ‘health state’, which can be converted using a standard algorithm to produce a single health state utility score [21]. The second part asks the respondent to assess their health ‘today’ on a visual analogue scale (VAS) of 0 to 100.
The WEMWBS is a 14-item questionnaire that uses a 5-point Likert scale to give a score of one to five for item and a total score ranging 14 to 70 – a higher WEMWBS score indicates a higher level of mental well-being [19].
Intervention acceptability
The acceptability of the study design and Yoga programme was assessed using class attendance rates and participant feedback via telephone interviews conducted within a 2-week period following the 3-month assessment. The participant interviews lasted up to 20 min and covered perceived benefits and negative consequences from participating in the study, feedback regarding specific design features of the study (including the Yoga programme and assessment procedures), and perceptions of barriers and facilitators to intervention participation. Audio recordings of the interviews were subsequently transcribed, before two of the authors (GT and LB) used a thematic analysis approach to summarise the data. This involved listening to the audio files and reading the transcripts several times to become familiar with the data, pooling quotes from different participants that related to the same part of the interview topic guide, and producing a summary of the findings for each part of the interview topic guide.
Statistical analysis
The effect of the intervention was evaluated using an analysis of covariance model. The 3-month outcome was the dependent variable and trial arm (intervention and control) was the independent variable. The baseline value of the outcome was included as a covariate [22], with study site as a random effect [23]. The analyses were done on an intention-to-treat basis, including only those participants with both baseline and follow-up data available (i.e., complete case analysis). The treatment effect (intervention minus control) is presented with its 95% confidence interval (CI). Analyses were conducted using IBM SPSS Statistics Version 22 (IBM United Kingdom Limited, Hampshire, UK).
Results
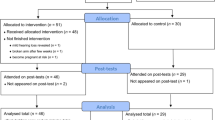
A total of 82 people were screened, and 52 (63.4%) were randomised among the four centres: 25 to Yoga and 27 to wait-list control (Fig. 2). Forty-seven (90%) of the participants were female and the mean age was 74.8 years (SD 7.2). The participants were all white, and the majority were retired (92%) and living in a community dwelling (88%). Participants often had multiple comorbidities (range 0 to 6), which included osteoarthritis (n = 20), hypertension (n = 12), depression/anxiety (n = 11), hypercholesterolemia (n = 7), rheumatoid arthritis (n = 6), asthma (n = 6), dementia (n = 4), osteoporosis (n = 4), cancer (n = 4), and cerebrovascular disease (n = 4). The participants in the two groups had similar baseline characteristics (Table 1), although there was a higher proportion of previous smokers in the control group (60% versus 33%).
The 52 participants heard about the study in the following ways: 22 (42.3%) via newspaper articles/advertisements; 11 (21.2%) via taster sessions at an Arthritis Care meeting, community centres, and a residential care home; 10 (19.2%) via a Yorkshire Yoga E-newsletter and friends/relatives of people at Yorkshire Yoga; 8 (15.4%) via leaflets delivered door-to-door in areas with a high concentration of older people, and; 1 (1.9%) via information displayed in a GP surgery.
Participant retention and intervention attendance
Four Yoga participants did not complete the follow-up assessments: three withdrew because of health problems that were unrelated to the study (eye surgery [n = 1], liver and kidney problems [n = 1], and “unwell”/bed-bound [n = 1]) and one withdrew due to a family bereavement. These participants had completed 0, 3, 5, and 6 Yoga sessions, respectively, before withdrawing. One control participant died before the follow-up assessment. The death was unrelated to the study.
Of the 21 Yoga participants who completed the study, median class attendance was 8 (range 3 to 10). Eighteen (86%) attended at least 5 of the 10 classes, and 14 (67%) attended at least 8 of the 10 classes. All of the treatment fidelity checks indicated that the Yoga sessions were delivered to the standards set in the initial teacher training.
Effect of intervention on outcome measures
The Yoga group had better self-reported health status and mental well-being at 3 months than the control group (Table 2). The adjusted mean EQ-5D utility, EQ-Visual Analogue Scale, and WEMWBS scores were 0.12 (95% CI, 0.03 to 0.21), 17 (8 to 26), and 6 (1 to 11) points higher in the Yoga group at 3 months, respectively. Lower body flexibility (chair sit-and-reach test) was also better in the Yoga group at 3 months (mean difference 5 cm, 0 to 10 cm). All aspects of physical function also appeared to be superior in the Yoga group at 3 months. Table 2 reveals that most of the 95% confidence intervals lie on the positive side, suggestive of beneficial effects. However, the confidence intervals also reveal that the true population effects could range from trivial negative (harmful) effects of 0.07 to 0.18 SD to moderate beneficial effects of 0.44 to 0.78 SD. There were unclear effects on body mass index, waist circumference and blood pressure; however, resting heart rate was lower in the Yoga group at 3 months (mean difference 6 beats/min, 1 to 11). There was one non-serious adverse event, which was probably related to the Yoga programme. Here, the participant reported that specific exercises aggravated her existing lower back pain during the first couple of sessions, but that this problem soon subsided and did not occur again for the remainder of the course.
Interview feedback
Twenty (95%) of the 21 Yoga participants who completed the study also completed an exit interview. The one person who did not complete an interview was uncontactable despite numerous attempts. Eighteen people (90%) reported enjoying the Yoga programme and all 20 people stated the study procedures were acceptable and that they would recommend a study like this to other people they know. One person thought that the Short Physical Performance Battery was too easy, such that it was hard to see improvement on those tests, and one other person suggested that it may have been useful to include some type of walking endurance test. Fourteen people (70%) had paid to attend the next BWY Gentle Years Yoga© course, and three other people (15%) said that they were going to continue doing the home-based Yoga exercises. Reasons for people (n = 3) not continuing with Yoga included preference for other forms of exercise (n = 2) and that the classes were too easy (n = 1).
The interviewees reported a range of physical, mental and social benefits from participating in the Yoga programme (Table 3). The most commonly cited physical benefits included improved physical function (e.g., improved chair rising and walking ability) (n = 10), improved flexibility (n = 10) and reduced pain (n = 4). Cited mental health benefits included stress-relieving/calming effects (n = 7), improved mood (n = 2) and a reduced frequency of panic attacks (n = 1). Thirteen people (72%) indicated that they liked the social interaction that the group exercise classes provided. Furthermore, many of the participants explicitly stated that having other peoples’ company was one of the main benefits of attending the class, and that they had developed new friendships with other class attendees.
Discussion
This trial found that the BWY Gentle Years Yoga© programme, when delivered once a week for 10 weeks, is safe, feasible, and acceptable for physically-inactive older adults with a broad range of comorbidities. The programme also led to improvements in health status, mental well-being and physical function at 3 months.
In this study, the 5-level EQ-5D and WEMWBS were used to assess health status and mental well-being, respectively. Although there is no consensus, changes in the EQ-5D utility index and WEMWBS of 0.10 [24] and between 3 and 8 points [25], respectively, have been recommended as clinically important. In this trial, we observed that scores on these questionnaires were, on average, 0.12 and 6 points higher, respectively, in the Yoga group at 3 months. These potentially-important changes are consistent with the findings of a meta-analysis of 422 older adults published in 2012 [9], which showed moderate beneficial effects of Yoga (versus other exercise interventions) on the physical and mental component scores of the SF-36 health survey (standard mean differences of 0.65 [0.02 to 1.28] and 0.66 [0.10 to 1.22], respectively). The small-to-moderate improvements we observed in physical function outcomes (e.g., lower-body flexibility, standing balance, sit-to-stand), are also in accordance with the results of a recent systematic review [26], which reported standardised mean differences for the effect of Yoga (versus control) on balance of 0.40 (0.15 to 0.65; 6 trials, n = 307), and on mobility of 0.50 (0.06 to 0.95; 3 trials, n = 225). That we did not see larger between-group differences for some aspects of physical function might be due to some of the tests suffering from ceiling effects and low responsiveness. For example, 17 out of 26 (65%) control participants and 17 out of 21 (81%) Yoga participants attained the highest possible standing balance score at follow-up, indicating that this measure suffers from ceiling effects in this population. Additionally, it was unlikely that the Yoga programme would alter usual walking pace over 4 m. Alternative physical function tests, such as the 30-s chair rise, single leg stance, and 8-ft timed up-and-go, could be considered for use in future studies. Nevertheless, the results of this study provide encouraging evidence that the BWY Gentle Years Yoga© programme has several beneficial effects in older adults with various health problems.
High attrition rates have been reported among older exercisers in general [27]. This 10-week adapted Yoga programme showed a relatively low attrition rate of 16%, with the reasons for withdrawal being unrelated to the intervention. The feasibility of the Yoga programme was also demonstrated by the ease of recruitment in a short period of time from a small geographical area, and excellent attendance with two thirds of the participants attending at least 8 of the 10 classes. The interview responses indicated that participants found the programme to be suitable for their abilities and enjoyable. Other factors that likely promoted attendance included the opportunity for social interaction, and friendly and supportive instructors who modified the intervention content to suit individual needs. Although the attendance data may have been biased by the Yoga classes being free of charge, 70% of the Yoga participants had paid to attend the next 10-week course following completion of the 3-month assessment. Finally, the Yoga programme appeared to be safe, as there was only one transient, non-serious adverse event.
Strengths of this study include blinded outcome assessment, low rates of attrition and missing data, and the involvement of multiple teachers (n = 7) and intervention fidelity checks. Limitations include the small sample size, short-term follow-up, that the participants were predominantly female (which limits generalisability of the results), and a lack of quantitative data on adherence to the home-based Yoga practice. However, this was designed to be a pilot trial to assess the feasibility of the Yoga programme for older people and to assess the effect on physical function and quality of life in preparation for a larger trial over a wider geographical area. The study has achieved these aims.
Conclusions
A weekly group-based adapted Yoga programme with home practice appears to be a safe, feasible and acceptable activity for older adults with a broad range of comorbidities, which can lead to improvements in physical function and mental and social well-being. Further research is needed to confirm and expand on these findings.
Abbreviations
- BWY:
-
British Wheel of Yoga
- CI:
-
Confidence interval
- EQ-5D:
-
EuroQol five dimensions questionnaire
- EQ-VAS:
-
EuroQol Visual Analogue Scale
- SD:
-
Standard deviation
- SPPB:
-
Short Physical Performance Battery
- WEMWBS:
-
Warwick-Edinburgh Mental Well-being Scale
References
O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137(3):342–54.
Germain CM, Vasquez E, Batsis JA. Physical activity, central adiposity, and functional limitations in community-dwelling older adults. J Geriatr Phys Ther. 2016;39(2):71–6.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146.
Griffiths A, Kouvonen A, Pentti J, Oksanen T, Virtanen M, Salo P, et al. Association of physical activity with future mental health in older, mid-life and younger women. Eur J Pub Health. 2014;24(5):813–8.
Blumenthal JA, Emery CF, Madden DJ, Coleman RE, Riddle MW, Schniebolk S, et al. Effects of exercise training on cardiorespiratory function in men and women older than 60 years of age. Am J Cardiol. 1991;67(7):633–9.
Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009;3:CD002759.
Li F, Harmer P, McAuley E, Duncan TE, Duncan SC, Chaumeton N, et al. An evaluation of the effects of tai chi exercise on physical function among older persons: a randomized contolled trial. Ann Behav Med. 2001;23(2):139–46.
Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49–54.
Patel NK, Newstead AH, Ferrer RL. The effects of yoga on physical functioning and health related quality of life in older adults: a systematic review and meta-analysis. J Altern Complement Med. 2012;18(10):902–17.
Gothe NP, McAuley E. Yoga is as good as stretching-strengthening exercises in improving functional fitness outcomes: results from a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2016;71(3):406–11.
American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. Eighth ed. Philadelphia: Lippincott Williams & Wilkins; 2009.
Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol. 2010;10:67.
Bayliss EA, Ellis JL, Steiner JF. Subjective assessments of comorbidity correlate with quality of life health outcomes: initial validation of a comorbidity assessment instrument. Health Qual Life Outcomes. 2005;3:51.
British Heart Foundation. Be Active for Life. Available from: file:///C:/Users/JHCL9/Downloads/g364_be_active_for_life_0513.pdf.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94.
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–31.
Puthoff ML. Outcome measures in cardiopulmonary physical therapy: short physical performance battery. Cardiopulm Phys Ther J. 2008;19(1):17–22.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5:63.
Rikli R, Jones J: Senior Fitness Test Manual, Second edn:. Illinois: Champaign; 2001.; 2013.
van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–15.
Vickers AJ, Altman DG. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323(7321):1123–4.
Chu R, Thabane L, Ma J, Holbrook A, Pullenayegum E, Devereaux PJ. Comparing methods to estimate treatment effects on a continuous outcome in multicentre randomized controlled trials: a simulation study. BMC Med Res Methodol. 2011;11:21.
Chen P, Lin KC, Liing RJ, Wu CY, Chen CL, Chang KC. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual Life Res. 2016;25(6):1585–96.
Maheswaran H, Weich S, Powell J, Stewart-Brown S. Evaluating the responsiveness of the Warwick Edinburgh mental well-being scale (WEMWBS): group and individual level analysis. Health Qual Life Outcomes. 2012;10:156.
Youkhana S, Dean CM, Wolff M, Sherrington C, Tiedemann A. Yoga-based exercise improves balance and mobility in people aged 60 and over: a systematic review and meta-analysis. Age Ageing. 2016;45(1):21–9.
Findorff MJ, Wyman JF, Gross CR. Predictors of long-term exercise adherence in a community-based sample of older women. J Women's Health (Larchmt). 2009;18(11):1769–76.
Acknowledgements
The sponsor was Northumbria University. The authors would like to acknowledge the study participants for supporting this research. The yoga instructors were Jenny Howsam, Stephanie Braysmith, Elaine Archer and Yvonne Lovvatt, with Laura Bissell, Rachel Greer, Celia Grieve and Sheila Spurr providing supply cover when required.
Funding
This study was funded by The British Wheel of Yoga and The Big Lottery Fund – Awards for All. The funders played no role in study design or conduct.
Availability of data and materials
The dataset is available from the corresponding author on reasonable request.
Authors’ contributions
GT designed the study, participated in data collection, performed the statistical analysis, and drafted the manuscript. JH conceived of the study, participated in its coordination, and provided critical revision of the manuscript. MH participated in data collection and provided critical revision of the manuscript. LB conceived of the study, participated in its coordination, and provided critical revision of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The Northumbria University Faculty of Health and Life Sciences Research Ethics Committee approved the study (reference HLSGT180116). Written, informed consent was obtained for all participants prior to the baseline assessments.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tew, G.A., Howsam, J., Hardy, M. et al. Adapted yoga to improve physical function and health-related quality of life in physically-inactive older adults: a randomised controlled pilot trial. BMC Geriatr 17, 131 (2017). https://doi.org/10.1186/s12877-017-0520-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-017-0520-6