Abstract
Background
The FRAX® algorithm quantifies a patient’s 10-year probability of a hip or major osteoporotic fracture without taking an individual’s balance into account. Balance measures assess the functional ability of an individual and the FRAX® algorithm is a model that integrates the individual patients clinical risk factors [not balance] and bone mineral density. Thus, clinical balance measures capture aspects that the FRAX® algorithm does not, and vice versa. It is therefore possible that combining FRAX® and clinical balance measures can improve the identification of patients at high fall risk and thereby high fracture risk.
Our study aim was to explore whether there is an association between clinical balance measures and fracture prediction obtained from FRAX®.
Method
A cross-sectional study design was used where post hoc was performed on a dataset of 82 participants (54 to 89 years of age, mean age 71.4, 77 female), with a fall-related wrist-fracture between 2008 and 2012. Balance was measured by tandem stance, standing one leg, walking in the figure of eight, walking heel to toe on a line, walking as fast as possible for 30 m and five times sit to stand balance measures [tandem stance and standing one leg measured first with open and then with closed eyes] and each one analyzed for bivariate relations with the 10-year probability values for hip and major osteoporotic fractures as calculated by FRAX® using Spearman’s rank correlation test.
Results
Individuals with high FRAX® values had poor outcome in balance measures; however the significance level of the correlation differed between tests. Standing one leg eyes closed had strongest correlation to FRAX® (0.610 p = < 0.01) and Five times sit to stand was the only test that did not correlate with FRAX® (0.013).
Conclusion
This study showed that there is an association between clinical balance measures and FRAX®. Hence, the use of clinical balance measures and FRAX® in combination, might improve the identification of individuals with high risk of falls and thereby following fractures. Results enable healthcare providers to optimize treatment and prevention of fall-related fractures.
Trial registration
The study has been registered in Clinical Trials.gov, registration number NCT00988572.
Similar content being viewed by others
Background
Fall-related fractures are a problem for society, and account for significant morbidity and healthcare expenses in elderly patients [1–3]. Approximately one third of persons over 65 years of age fall each year [4, 5]. In 5–15 % of cases, a fall in an elderly person results in a fracture [6, 7]. Fractures are the most costly fall-related injuries. In the United States, fractures account for 35 % of injuries from falls but 61 % of the healthcare costs [3]. In Sweden the annual number of hip fractures is expected to double between 2002 and 2050, predicting 30,000 hip fractures in 2050 [8].
Risk factors for falling
Several risk factors for fall-related hip fracture have been identified, such as increasing age and previous fracture [9], and older adults with multiple risk factors and low bone mineral density are at the highest risk of hip fracture [10]. Balance is also a risk factor for falls but the variety of methods of assessing balance makes it difficult to appreciate the impact of balance on fall risk [11]. However, balance deficits can predict falls [12]. Asymmetric vestibular function affects balance [13] and is overrepresented among elderly persons with hip fractures [14] and wrist fractures [15]. It is also a strong predictor of falls among the elderly [13]. The age-related changes seen in the incidence of wrist fractures differs significantly from the increase seen in hip fracture incidence [16]. A deterioration of multiple sensory receptor systems and neuro-muscular function occurs in ageing, which probably result in a decrease in ability to extend the arm to alleviate the consequences of a fall [17], a pattern that explains the age differences between wrist and hip fracture incidence.
Fracture risk prediction tools
Since fall-related fractures are a huge problem for the society, and not seldom lethal for the affected person [18], the use of tools for the prediction of fracture seems essential. As many as 13 different tools have been identified, including between 4 and 31 clinical risk factors [19]. The most frequent used tool in research is the FRAX® algorithm which was developed by the World Health Organization, in collaboration with The University of Sheffield. FRAX® includes an online calculation tool and uses femoral neck bone mineral density, prior fractures, parental hip fracture history, age, sex, body mass index, ethnicity [not in all countries], smoking, alcohol use, glucocorticoid use, rheumatoid arthritis and secondary osteoporosis data to quantify a patient’s 10-year probability value of a hip or major osteoporotic fracture [20]. The main use of the FRAX® algorithm in clinical practice is for to identify those individuals who need a pharmacological intervention [21]. An individual’s risk of falling is not included in FRAX®, since comparable data of falls were missing when the tool was developed [22]. Quantitative adjustment of the FRAX® by including falls history does not seem to be possible currently [23]. To accomplish further fracture reduction, reduction of fall risk is required FRAX® seems to partly apprehend risk of future fall even it fall risk is not included in the tool [24]. Attempts have been made to combine fall risk instruments and FRAX® [25]. However, correlations between the instruments were weak and probably caused by the inclusion of age and sex in FRAX® and more research is therefore needed.
Balance
Losing one’s balance, and thus falling, is often a result of incorrect weight shifting. In the prevention of falls and thereby prevention of potential fractures, a multitask approach is beneficial [26]. Such multitask approaches comprise balance measures that assess balance and functional ability. In the elderly, these performance-oriented functional tests are widely adopted [27, 28] to identify risk groups for falling.
Balance measures assess the functional ability of an individual and the FRAX® algorithm has an individual’s rate of osteopenia as the key feature. Thus, clinical balance measures capture aspects that the FRAX® algorithm does not, and vice versa. It is therefore possible that combining FRAX® and clinical balance measures can improve the identification of patients at very high fall risk. However, if there is an association between clinical balance measures and FRAX® is unclear.
Our study aim was to explore whether there is an association between clinical balance measures and fracture prediction obtained from FRAX®.
Methods
Participants
Post hoc data analysis was performed on a dataset of 82 participants aged over 50 with fall-related fractures. Data were collected in Malmö, Sweden, between Dec 2008 and Nov 2012, when 85 patients were allocated to a randomized controlled trial. Sixty eight patients completed the study and 17 interrupted [15]. In the present study, baseline measures for the total study sample is used, expect for three patients, where FRAX® data were not available. Thus, the study comprised of 82 patients (77 female, 93.9 %) 54 to 89 years of age (mean 71.4, SD = 9.1), who all had a fall-related wrist fracture. All patients lived at home, 31 with a partner and 51 by themselves. Mean value for self-rated health, measured by the EQ5D visual analogue scale [29] was 73 (standard deviation 16.6). In this study, balance measures and FRAX® data were used. The study was approved by the regional ethical review board in Lund [number 585/2008].
Balance measures
The balance measures used have been shown in previous studies to be relevant for assessing elderly patients in risk of falling [12, 30, 31].
The balance measures were:
-
Tandem stance (standing in a heel-to-toe position) with eyes open (TSEO) and Tandem stance with eyes closed (TSEC) [32–34]. The time that the participant was able to maintain this position, up to 30 s, was measured. Three attempts were allowed and the best attempt was used.
-
Standing on one leg with eyes open (SOLEO) and Standing on one leg with eyes closed (SOLEC) [33]. Time up to 30 s was measured and three attempts were allowed.
-
Walking in a modified figure of eight [35], where steps outside the figure were counted.
-
Walking heel-to-toe in a straight line [34], where steps outside the line were counted.
-
Walking as fast as possible for 30 m with one turn after 15 m [36]. Time in seconds was measured.
-
Five times sit-to-stand test (FTSST) [37] where the participant sat on a stool and stood up and sat down five times while the time was measured.
FRAX®
FRAX® algorithms calculate the 10-year probability of fracture. The output is a 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture (value 0.00–1.00). FRAX® values were calculated using the web-based calculation tool for Sweden [20]. FRAX® value of <5 is considered as low fracture risk, value between ≥5 and <7.5 is considered as intermediate risk and value of ≥7.5 is considered as high risk [38]. The information from the questionnaire was transferred to the calculation tool.
Statistical analysis
All data were examined visually for skewness and kurtosis and checked for normality using the Shapiro-Wilks test. For normally-distributed variables, mean and standard deviation were presented (age), and for non-normal variables, median and interquartile range (all others).
Correlation coefficients were calculated for the bivariate relationship between each of the balance tests and the FRAX score for 10-year probability for hip and major osteoporotic fractures. Spearman’s rank correlation test was used due to the non-normality of the data.
Analyses were performed using SPSS Inc., version 22.
Results
Participants
Characteristics of the participants and balance measures are shown in Table 1. One participant was not able to perform neither Walking heel-to-toe in a straight line nor Walking in the modified figure of eight, although could perform the remaining balance tests thus including the results in the correlation analysis.
Median value for TSEO was 30 s and 91.5 % of the participants could maintain the position for 30 s.
Median value for Walking heel-to-toe was 1 step and 37 % of the participants could perform the test without stepping outside the line at all.
Median value for Walking in the figure of eight was 2 steps and 38 % could perform the test without stepping outside the figure at all.
Data on “Parent fractured hip”, “Secondary osteoporosis” and “Femoral neck BMD” were missing for all cases and equated to the non-presence of each feature for study purposes [20]. Also, the “Smoking” value for one participant was missing and set to “no” and “Rheumatoid Arthritis” value for one participant was missing and set to “no”.
Bivariate correlation analysis
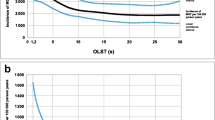
The bivariate correlation analysis showed that individuals with high values on FRAX® (both FRAX®hip and FRAX®osteo) also had poor outcome on: TSEO, TSEC, SOLEO, SOLEC, Walking heel to toe, Walking in the modified figure of eight and Fast walking test (Spearmans rho −0.319–0.610). Correlations are displayed in Table 2. SOLEC had the strongest correlation with FRAX® (Fig. 1) and FTSST had no correlation to FRAX® (Fig. 2).
Discussion
Main findings
This study indicated significant correlations between FRAX® values and seven out of eight balance measures. SOLEC had the strongest correlation to both FRAX®osteo and FRAX®hip. These findings imply a relation between FRAX® and all clinical balance measures except FTSST in a population with high risk fallers who already had a fall-related fracture.
Discussion of the results
Maintaining balance involves a complex system of skills in motor function, integrated with somatosensory input and processed in the brainstem. Furthermore, balance performance differs between age-groups and between different groups of patients. It has not been possible to detect any single balance measure that can predict future fracture [39]. Thus, balance measures, adequate for the age- and patient group, used together with FRAX®, is likely to increase the chance to identify persons at very high risk of sustaining a fall-related fracture. The importance of choosing the adequate balance measure is supported by a previous study showing that poor ability to stand in tandem stance with eyes open doubles the risk of falling [12]. The population median age in that study was 82 years, thus older than the population in our study and the median value for tandem stance with eyes open was 16 s (SD12), compared to 30 s in our study. This suggests that SOLEC may be a more appropriate balance test for the age group included in our study.
The need to use arm support when rising from a chair has previously been used to predict hip fractures in elderly women [40]. The mean age of the population in that study was 7 years higher than in our study. Furthermore, in that study only the need to use arms was registered rather than the time it took to rise five times without support from the arms. Thus, FTSST seems to be an appropriate measure for patients that are older than the participants in our study.
Tandem stance and standing one leg is performed up to 30 s, which means that there is a ceiling effect in those measures. In TSEO, 91.5 % of the participants accomplished 30 s, indicating that this balance measure probably is too easy to detect balance disturbances in this group of patients. Our participants had a median value of 21 s for Walking as fast as possible for 30 m, which respond well to values from other research on similar group of patients [34].
The participants in this study were living at home and had a good self-rated health (mean value 73) which was expected. Hence, other balance measures that have been found appropriate for detecting fall risk among frail elderly, such as the Timed Up and Go test, was not considered suitable [41].
Also, the median FRAX® values among the participants in our study was 0.27 and 0.11 implying low fracture risk, even if all of them had sustained a fall-related fracture and thereby have high risk of fall [11]. This might imply the use of other measures along with FRAX® to improve fracture prediction.
Other fracture risk prediction tools include fall risk in the tool, such as GARVAN and Qfracture. GARVAN has shown to have equal discriminative ability as FRAX® [42] and Qfracture has shown to have better discriminative ability for hip fracture than FRAX® [43]. Both GARVAN and Qfracture include fall risk in the fracture prediction by including history of falls but not balance measures. Hence, by including balance measures in a fracture prediction tool instead of history of falls, it might be possible to identify individuals at high risk of falling even before the first fall.
There are only five men in this study and therefore not possible to adjust for sex. However, when analyzing the results with men excluded, the results were the same. Other authors have adjusted for age when analyzing the correlation between FRAX® and balance measures and found that age explained the correlation [25]. We did not adjust for age in our analysis, since age is included in the FRAX® algorithm and therefore inevitable seems to explain any correlation.
Strengths and limitations
Limitations of the present study include the missing data entries when calculating the FRAX® values with the online calculation tool. We suspect that the missing data have diluted our results and that correlations would be even stronger without missing data. Another limitation is the absence of bone density in the calculation of FRAX®. However, research in the effect of inclusion of bone mineral density in the FRAX® calculation is inconclusive: inclusion has been shown to both underestimate [40] and overestimated [44] risk. Also, all participants had in fact sustained a fall-related wrist-fracture. Previous fracture indicates a substantial risk of future fracture [45]. Hence, we hope that this means that we have identified persons at a very high risk of fall but it can also mean that the sample is biased, which will have to be considered when reflecting on the results.
Future research and clinical implications
The results indicate a relationship between FRAX® and clinical balance measures, with the strongest correlation between FRAX® and SOLEC. These findings may be used in future hypothesis testing, where this group is followed for observation of actual fracture incidence thus potentially confirming a high risk group of acquiring fracture. However, the choice of balance measure, adequate for the age- and patient-group, seems crucial, both in research and in clinical practice.
Conclusion
This study showed that there is an association between clinical balance measures and FRAX®. Hence, the use of clinical balance measures and FRAX® in combination, might improve the identification of individuals with high risk of falls and thereby following fractures. Results enable healthcare providers to optimize treatment and prevention of fall-related fractures.
Ethics approval and consent to participate
The study was approved by the regional ethical review board in Lund [number 585/2008]. All patients gave their informed consent before entering the study.
Consent for publication
Not applicable.
Availability of data and materials
Data supporting findings in the study can be requested from corresponding author.
Abbreviations
- FRAX:
-
Fracture Risk Assessment Tool
- FTSST:
-
Five times sit-to-stand test FTSST.
- SOLEC:
-
Standing one leg eyes closed
- SOLEO:
-
Standing one leg eyes open
- TSEC:
-
Tandem standing eyes closed
- TSEO:
-
Tandem standing eyes open
References
Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH. Cost of falls in old age: a systematic review. Osteoporos Int. 2010;21(6):891–902.
Siracuse JJ, Odell DD, Gondek SP, Odom SR, Kasper EM, Hauser CJ, et al. Health care and socioeconomic impact of falls in the elderly. Am J Surg. 2012;203(3):335–8. discussion 8.
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–5.
Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82(8):1050–6.
Moreland J, Richardson J, Chan DH, O’Neill J, Bellissimo A, Grum RM, et al. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49(2):93–116.
Berry SD, Miller RR. Falls: epidemiology, pathophysiology, and relationship to fracture. Curr Osteoporos Rep. 2008;6(4):149–54.
Tiedemann AC, Murray SM, Munro B, Lord SR. Hospital and non-hospital costs for fall-related injury in community-dwelling older people. NSW Public Health Bull. 2008;19(9–10):161–5.
Rosengren BE, Karlsson MK. The annual number of hip fractures in Sweden will double from year 2002 to 2050: projections based on local and nationwide data. Acta Orthop. 2014;85(3):234–7.
Ensrud KE. Epidemiology of fracture risk with advancing age. J Gerontol A Biol Sci Med Sci. 2013;68(10):1236–42.
Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, et al. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc. 2004;52(9):1479–86.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68.
Hansson EE, Mansson NO, Ringsberg KA, Hakansson A. Falls among dizzy patients in primary healthcare: an intervention study with control group. Int J Rehabil Res 2008;31(1):51–7.
Ekvall Hansson E, Magnusson M. Vestibular asymmetry predicts falls among elderly patients with multi- sensory dizziness. BMC Geriatr. 2013;13(1):77.
Kristinsdottir EK, Jarnlo G-B, Magnusson M. Asymmetric vestibular function in the elderly might be a significant contribution to hip fractures. Scand J Rehab Med. 2000;32:56–60.
Ekvall Hansson E, Dahlberg LE, Magnusson M. Vestibular Rehabilitation Affects Vestibular Asymmetry among Patients with Fall-Related Wrist Fractures - A Randomized Controlled Trial. Gerontology. 2015;61(4):310–8.
Cooper C, Melton 3rd LJ. Epidemiology of osteoporosis. Trends Endocrinol Metab. 1992;3(6):224–9.
Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–7.
MSB. Swedish Civil Contigencis Agency. 2015 [cited 2015]. Available from: https://www.msb.se/en/. Accessed November 2015.
Marques A, Ferreira RJ, Santos E, Loza E, Carmona L, da Silva JA. The accuracy of osteoporotic fracture risk prediction tools: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(11):1958–67. doi:10.1136/annrheumdis-2015-207907.
Kanis JA. FRAX® WHO Fracture Risk Assessment Tool. 2015. Available from: http://www.shef.ac.uk/FRAX/.
Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E. FRAX and its applications to clinical practice. Bone. 2009;44(5):734–43.
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385–97.
Masud T, Binkley N, Boonen S, Hannan MT, Members FPDC. Official Positions for FRAX(R) clinical regarding falls and frailty: can falls and frailty be used in FRAX(R)? From Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(R). J Clin Densitom. 2011;14(3):194–204.
Harvey NC, Johansson H, Oden A, Karlsson MK, Rosengren BE, Ljunggren O, et al. FRAX predicts incident falls in elderly men: findings from MrOs Sweden. Osteoporos Int. 2016;27(1):267–74.
Holloway KL, Kotowicz MA, Lane SE, Brennan SL, Pasco JA. FRAX (Aus) and falls risk: Association in men and women. Bone. 2015;76:1–4.
Robinovitch SN, Feldman F, Yang Y, Schonnop R, Leung PM, Sarraf T, et al. Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet. 2013;381(9860):47–54.
Chiu AY, Au-Yeung SS, Lo SK. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil Rehabil. 2003;25(1):45–50.
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45(6):735–8.
EQ5D. [Web-page]. 2010 [cited 2010 2010-03-18]. EQ5D web page]. Available from: http://www.euroqol.org/. Accessed November 2015.
Hansson EE, Månsson NO, Håkansson A. Effects of specific rehabilitation for dizziness among patients in primary health care. A randomized controlled trial. Clin Rehabil. 2004;18(5):558–65.
Hansson EE, Månsson NO, Håkansson A. Balance performance and self-perceived handicap among dizzy patients in primary health care. Scand J Prim Health Care. 2005;23(4):215–20.
Briggs R, Gossman M, Birch R, Drews J, Shaddeau S. Balance performance among noninstitutionalized elderly women. Phys Ther. 1989;69(9):748–56.
Franchignoni F, Tesio L, Martino MT, Ricupero C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging (Milano). 1998;10(1):26–31.
Ledin T, Kronhed AC, Möller C, Möller M, Ödkvist LM, Olsson B. Effects of balance training in elderly evaluated by clinical tests and dynamic posturography. J Vestib Res. 1990–1991;1:129–38.
Jarnlo G-B, Nordell E. Reliability of the modified figure of eight-balance performance test for elderly women. Physiotherapy Theory and Practice. 2003;19:35–43.
Kronhed AC, Möller C, Olsson B, Möller M. The effect of short-term balance training on community-dwelling older adults. J Aging Phys Act. 2001;9:19–31.
Meretta BM, Whitney SL, Marchetti GF, Sparto PJ, Muirhead RJ. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. J Vestib Res. 2006;16(4–5):233–43.
Azagra R, Zwart M, Aguye A, Martin-Sanchez JC, Casado E, Diaz-Herrera MA, et al. Fracture experience among participants from the FROCAT study: what thresholding is appropriate using the FRAX tool? Maturitas. 2016;83:65–71.
Beckman A, Hansson EE. Fractures in people with dizziness: 5-year follow-up. J Am Geriatr Soc. 2011;59(9):1767–9.
Kim JW, Koh JM, Park JH, Chang JS. Validation of FRAX without BMD: an age-related analysis of the Fifth Korean National Health and Nutrition Examination Survey (KNHANES V-1, 2010). Bone. 2015;75:27–31.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Bolland MJ, Siu AT, Mason BH, Horne AM, Ames RW, Grey AB, et al. Evaluation of the FRAX and Garvan fracture risk calculators in older women. J Bone Miner Res. 2011;26(2):420–7.
Hippisley-Cox J, Coupland C. Predicting risk of osteoporotic fracture in men and women in England and Wales: prospective derivation and validation of QFractureScores. BMJ. 2009;339:b4229.
Egsmose EL, Birkvig M, Buhl T, Madsen OR. FRAX fracture risk in women with a recent fracture of the distal forearm: agreement between assessments with and without bone mineral density and impact of measurement side in the individual patient. Clin Rheumatol. 2015;34(7):1265–72.
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35(2):375–82.
Acknowledgements
Not applicable.
Funding
There was no external funding for this project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Hansson: has contributed to study design, data collection, and has contributed in writing the manuscript. Najafi: contributed in the statistical analysis of data and has contributed in writing the manuscript. Dahlberg: has contributed to study design, and drafting of the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Najafi, D.A., Dahlberg, L.E. & Hansson, E.E. A combination of clinical balance measures and FRAX® to improve identification of high-risk fallers. BMC Geriatr 16, 94 (2016). https://doi.org/10.1186/s12877-016-0266-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-016-0266-6