Abstract
Aims
The aim of the research was to look into the connection between the occurrence of gallstones in adult US citizens and lipid accumulation products (LAP).
Methods
We conducted a cross-sectional study of 3,582 U.S. adults with relevant indicators collected from the 2017–2020 National Health and Nutrition Examination Survey (NHANES) database. Multifactorial logistic regression was used to investigate the linear relationship between LAP and gallstone incidence, while smoothed curve fitting was used to describe the nonlinear relationship, and subgroup and interaction analyses were used to evaluate the potential differences between groups.
Results
Among the 3582 participants aged ≥ 20 years included, there was a positive association between LAP and gallstones. Following adjustments for all covariates, the likelihood of getting gallstones rose by 29% for each unit rise in log2-LAP (OR = 1.29, 95% CI: 1.13‒1.49). Compared to those in the lowest tertile, those in the highest LAP tertile had a significantly higher risk of developing gallstones (OR = 1.97, 95% CI: 1.31‒2.95). Subgroup analyses indicated that the association between LAP and gallstones was not affected by the stratification of the variables examined.
Conclusion
Gallstones and LAP exhibited a positive association in our investigation, indicating that LAP may be utilized as a clinical indicator to determine the occurrence of gallstones.
Similar content being viewed by others
Background
Gallstone disease is one of the most common digestive disorders in the world, affecting about 10 to 15% of adults in the United States and Europe [1]. It is characterized by the production of hardened stones in the gallbladder or bile ducts. Most people with gallstones may have no evident symptoms [2], but when the stones clog the bile ducts or induce inflammation, a series of clinical symptoms such as abdominal pain, nausea, and vomiting, as well as complications such as perforation of the gallbladder, are often observed [3,4,5], which adversely impact the patient’s daily life and health state. Although the major risk factors for gallstones are known to include genetic predisposition, obesity, a high-fat diet, and certain gallbladder diseases [6, 7], reliable clinical indicators are still needed to predict the occurrence of gallstones.
In recent years, the number of people suffering from obesity has increased dramatically worldwide, posing a serious health threat [8]. Numerous metabolism-related diseases have a substantial correlation with obesity [9]. Currently, the body mass index (BMI) and waist circumference (WC) are the most widely used clinical markers for assessing obesity. However, when used, BMI is influenced by age and sex, fails to distinguish between variations in body composition, and may overestimate obesity in individuals with high levels of muscle mass. Several studies have highlighted the controversy surrounding BMI’s use in determining the risk of certain diseases and mortality [10, 11]. In addition, a limitation of WC is the inability to separate visceral and subcutaneous adipose tissue. As a new obesity assessment metric, lipid accumulation product (LAP) has been shown to be superior to traditional obesity metrics in predicting cardiovascular risk, and metabolic syndrome [12, 13]. Recent studies have also reported the association and unique predictive value of LAP with various diseases such as osteoarthritis, obstructive sleep apnea, psoriasis, and testosterone deficiency [14,15,16,17].
Therefore, this study used the National Health and Nutrition Examination Survey (NHANES) database, a survey database designed to assess the health and nutritional status of adults and children in the United States, to investigate the relationship between LAP and gallstones and examine the possible function of LAP in the prediction of gallstone risk by assessing the incidence of gallstones among individuals with varying levels of LAP.
Methods
Participants in the NHANES study
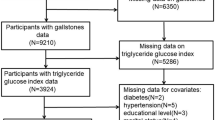
We selected 15,560 individuals from the 2017–2020 NHANES survey for the study. After screening, 3582 participants were ultimately included in this study (Fig. 1). We omitted those who lacked data on gallstones (6350), those who lacked data on calculated LAP (5460), and those who were missing other covariates (168). The data originates from the publicly accessible NHANES official website, The National Research Ethics Board of the United States reviewed and approved.
Measurement of the LAP
LAP is calculated using WC and triglycerides (TG) as described in previous literature: for men, LAP = (WC (cm) − 65) * TG (mmol/L); for women, LAP = (WC (cm) − 58) * TG (mmol/L).
Assessment of gallstones
The outcome variable was the occurrence of gallstones. To assess gallbladder stones, questionnaires were used, including: “Has a doctor or other health professional ever told you that you had gallstone?
Covariates
Based on previous studies, confounding factors that may be associated with LAP and gallstones were included in the final analysis [18, 19], including gender (male/female), age (years), race(Mexican American/Other Hispanic/Non-Hispanic White/Non-Hispanic Black/Other Race), educational status(less than high school/high school/more than high school), marital status(cohabitation/solitude), and poverty-to-income ratio (PIR) in demographic data. Ultrasound transient elastography of the liver in examination data. Also included in the questionnaire data are smoking, alcohol consumption, hypertension, diabetes, cancer and asthma.A history of smoking was defined as having smoked at least 100 cigarettes in a lifetime, a history of alcohol consumption was defined as having ever had any kind of alcohol, and asthma, diabetes, hypertension, and cancer were identified by whether or not they had ever been told in the questionnaire that they had these diseases. The use of the controlled attenuation parameter (CAP) reflects hepatic steatosis, which was diagnosed when the CAP was ≥ 285 dB/m in reference to previous studies [20].
Statistical analysis
EmpowerStats 4.0 (http://www.empowerstats.com/) was used, and p < 0.05 was considered statistically significant. Categorical data were expressed as proportions and continuous variables were expressed as mean ± SD. To investigate the association between gallstones and LAP, multivariate logistic regression models were used. Three models were used for multivariate testing: model 2 included adjustments for sex, age, race, marital status, PIR, and education level; model 3 included adjustments for all covariates. Model 1 did not include any adjustments. The variables were changed to fit the smoothing curves. Subgroup analyses and interaction tests were used to examine the heterogeneity of associations between subgroups of different ages, sex, hypertension, diabetes, and other conditions. .
Results
Baseline characteristics of participants
A total of 3582 participants were included, with 49.25% being male and an average age of 50.75 years. The mean LAPs of all participants were 51.86 (54.37), of which 377 (10.52%) had gallstones. The clinical characteristics of the participants stratified according to the presence or absence of gallstones as a column variable are shown in Table 1. Age, gender, race, PIR, BMI, TG, WC, smoking, asthma, cancer, hypertension, and diabetes were significantly different between the two groups (p < 0.05). Compared to the non-gallstone group, the gallstone group had higher waist circumference, BMI, and age; they also had poorer income and more females than males. They were more likely to be concurrent smokers and to have asthma, cancer, hypertension, diabetes, and hepatic steatosis.
Association of LAP with gallstones
Table 2 shows the results of the multifactorial regression analysis of LAP and gallstones and we observe a positive correlation between LAP and gallstones, which remained stable (OR = 1.29, 95% CI: 1.13‒1.49) in the fully adjusted model (Model 3), meaning that the likelihood of getting gallstones rose by 29% for each unit rises in log2-LAP. The above associations remained statistically significant after dividing LAP into tertiles (P less than 0.01 for all trends). Participants in the highest tertile of LAP were significantly more likely to develop gallstones compared to those in the lowest tertile of LAP (OR = 1.97, 95% CI: 1.31‒2.95). Furthermore, the nonlinear positive connection between LAP and gallstones was further supported by the findings of smoothed curve fitting (Fig. 2).
Subgroup analysis
We conducted interaction tests and subgroup analyses by sex, age, smoking status, alcohol use, asthma, cancer, hypertension, diabetes, and hepatic steatosis to determine if the relationship between LAP and gallstones is constant across groups. As shown in Fig. 3, our results indicate that the positive association between LAP and gallstones is similar across populations.
Discussion
A positive link was found between gallstones and LAP in this cross-sectional study with 3582 participants. Following adjustments for all covariates, the likelihood of getting gallstones rose by 35% for each unit rise in log2-LAP [1.35 (1.21, 1.50)]. This suggests that LAP may have potential clinical value in predicting gallstone risk.
As far as we know, this is the first research to assess the connection between LAP and gallstones.LAP values are a comprehensive assessment of obesity in combination with WC and TG levels, and current evidence has shown that obesity poses a significant risk for the development of gallstones [21]. BMI and WC are commonly used to assess obesity, and previous studies have shown that overweight and obese people have a significantly higher risk of having symptomatic gallstones [22, 23]. Additional studies have also found an 81% increase in gallstone prevalence for each standard deviation increase in WC [24]. However, since BMI cannot assess localized obesity and WC does not distinguish between visceral and subcutaneous fat, both have limitations in the prediction of disease. A previous prospective study showed that abdominal obesity was significantly associated with gallstones and independent of BMI [25]. Additionally, the research by Radmard et al. demonstrated that there was no meaningful correlation between the development of gallstones and subcutaneous fat [26]. These results suggest that BMI and WC are somewhat controversial in independently predicting gallstone risk.LAP is a simple and non-invasive method for assessing visceral fat accumulation and metabolic abnormalities. It has been linked to a variety of disorders and has been shown to be a more accurate predictor of cardiovascular disease [27, 28]. therefore, the present study used the composite index, LAP, to investigate the relationship with gallstones.
According to this study, there is a positive correlation between LAP and gallstones, and there may be more than one mechanism underlying this association. First. High LAP is usually accompanied by high levels of TG and low levels of HDL cholesterol. Elevated TG leads to supersaturation of cholesterol in the bile, which increases the formation of cholesterol crystals and the occurrence of gallstones. At the same time, lower HDL cholesterol impairs its ability to remove cholesterol from the tissues, allowing more cholesterol to accumulate in the bile [29,30,31]. Second. Enlarged WC is usually accompanied by visceral fat accumulation, which is closely related to insulin resistance. Insulin resistance leads to elevated levels of insulin, which in turn promotes the synthesis of more cholesterol by the liver, as well as inhibiting the secretion of bile acids, leading to an increase in the concentration of cholesterol in the bile, which promotes the formation of gallstones [30, 32,33,34]. Third. High LAP is usually associated with chronic inflammation and oxidative stress states. High concentrations of inflammatory mediators, such as interleukin-6 and C-reactive protein, impair the gallbladder’s ability to contract normally, leading to incomplete emptying of the gallbladder and thus increasing the risk of gallstone formation [35, 36]. Fourth. Accumulation of visceral fat and insulin resistance also affects the kinetic function of the gallbladder. It has been found that patients with obesity and metabolic syndrome have significantly reduced gallbladder emptying capacity, leading to cholestasis, which promotes gallstone formation [37]. Furthermore, leptin, a hormone that plays an important role in the development of obesity, has been related to gallstone formation by controlling bile acid metabolism [38, 39].
The results of this study showed consistency across gender and age groups, indicating the broad applicability of LAP as a predictor of gallstone risk. Secondly, the sample of this study was obtained from a representative official database, and it is the first time that this composite index has been utilized to investigate the association between it and gallstones. However, this study has several limitations. First, due to the availability of data on gallstones, this study only included data from 2017 to March 2020, and due to the reason that it was a cross-sectional study lacking time-series data, we were only able to reveal associations without being able to determine causality. Second, this study used self-reported outcome variables, lacked a more precise imaging diagnosis, and because most gallstones are clinically asymptomatic, the results of the study were influenced by whether participants received regular medical checkups or whether they received appropriate medical care from their family physicians, and there is a possibility that a person could be incorrectly diagnosed with or without gallstones, and thus the report may have potential research bias. In addition, the information on gallstones in this study was based on the question “Have you had gallstones? ”, which did not provide any information about the type of gallstones, so we were unable to perform subgroup analyses stratified by gallstone composition. Finally, even though we included many covariates in performing the multivariate regression analyses, there may still be some residual confounding. In view of these limitations, later multicenter investigations as well as observation of the occurrence of gallstones over time in patients with higher LAP are needed to further evaluate and confirm our findings.
Conclusion
This study demonstrates that excessive LAP levels are linked to a greater risk of gallstones and that active weight management and lifestyle treatments may enhance or minimize the incidence of gallstones.
Availability of data and materials
The NHANES data that support the findings of this study are openly available at https://www.cdc.gov/nchs/nhanes/index.htm.
Data availability
The survey data are publicly available on the internet for data users and researchers throughout the world (www.cdc.gov/nchs/nhanes/).
Abbreviations
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- LAP:
-
Lipid accumulation products
- NHANES:
-
National Health and Nutrition Examination Survey
- PIR:
-
Poverty-to-income ratio
- TG:
-
Triglyceride
References
Di Ciaula A, Wang DQ, Portincasa P. An update on the pathogenesis of cholesterol gallstone disease. Curr Opin Gastroenterol. 2018;34(2):71–80.
Innes K, Hudson J, Banister K, Croal B, Ramsay C, Ahmed I, et al. Core outcome set for symptomatic uncomplicated gallstone disease. Br J Surg. 2022;109(6):539–44.
Migda B, Gabryelczak MA, Migda A, Prostacka K. A rare complication of cholecystolithiasis: perforation of the gallbladder. J Ultrason. 2021;21(84):63–6.
Alemi F, Seiser N, Ayloo S. Gallstone disease: cholecystitis, mirizzi syndrome, bouveret syndrome, gallstone ileus. Surg Clin North Am. 2019;99(2):231–44.
Tanaka H, Imasato M, Yamazaki Y, Matsumoto K, Kunimoto K, Delpierre J, et al. Claudin-3 regulates bile canalicular paracellular barrier and cholesterol gallstone core formation in mice. J Hepatol. 2018;69(6):1308–16.
Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172–87.
Chen L, Yang H, Li H, He C, Yang L, Lv G. Insights into modifiable risk factors of cholelithiasis: a mendelian randomization study. Hepatology. 2022;75(4):785–96.
Gaskin CJ, Cooper K, Stephens LD, Peeters A, Salmon J, Porter J. Clinical practice guidelines for the management of overweight and obesity published internationally: a scoping review. Obes Rev. 2024;25(5): e13700.
Rhee EJ. The influence of obesity and metabolic health on vascular health. Endocrinol Metab (Seoul). 2022;37(1):1–8.
Jackson AS, Stanforth PR, Gagnon J, Rankinen T, Leon AS, Rao DC, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: the heritage family study. Int J Obes Relat Metab Disord. 2002;26(6):789–96.
Vecchié A, Dallegri F, Carbone F, Bonaventura A, Liberale L, Portincasa P, et al. Obesity phenotypes and their paradoxical association with cardiovascular diseases. Eur J Intern Med. 2018;48:6–17.
Kahn HS. The lipid accumulation product performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5:26.
Li Y, Zheng R, Li S, Cai R, Ni F, Zheng H, et al. Association between four anthropometric indexes and metabolic syndrome in US adults. Front Endocrinol (Lausanne). 2022;13:889785.
Huang J, Han J, Rozi R, Fu B, Lu Z, Liu J, et al. Association between lipid accumulation products and osteoarthritis among adults in the United States: a cross-sectional study, NHANES 2017–2020. Prev Med. 2024;180:107861.
Zhang C, Dong X, Chen J, Liu F. Association between lipid accumulation product and psoriasis among adults: a nationally representative cross-sectional study. Lipids Health Dis. 2024;23(1):143.
Zhou T, Chen S, Mao J, Zhu P, Yu X, Lin R. Association between obstructive sleep apnea and visceral adiposity index and lipid accumulation product: NHANES 2015–2018. Lipids Health Dis. 2024;23(1):100.
Zhang M, Zhang J, Cui Y, Xing Z. Predictive power of lipid-related indicators for testosterone deficiency: a comparative analysis, NHANES 2011–2016. Int Urol Nephrol. 2024;56(6):1825–33.
Liu X, Yan G, Xu B, Sun M. Association between monocyte-to-high-density lipoprotein-cholesterol ratio and gallstones in U.S. adults: findings from the national health and nutrition examination survey 2017–2020. Lipids Health Dis. 2024;23(1):173.
Slouha E, Biput SJ, Kuteyi A, Kalloo AE, Gorantla VR. Non-alcoholic fatty liver disease and gallstones: a systematic review. Cureus. 2023;15(9):e45027.
Siddiqui MS, Vuppalanchi R, Van Natta ML, Hallinan E, Kowdley KV, Abdelmalek M, et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17(1):156-63.e2.
Man S, Gao Y, Lv J, Tong M, Yin J, Wang B, et al. Metabolically healthy obesity was significantly associated with increased risk of gallstones. Eur J Endocrinol. 2022;186(2):275–83.
Katsika D, Tuvblad C, Einarsson C, Lichtenstein P, Marschall HU. Body mass index, alcohol, tobacco and symptomatic gallstone disease: a Swedish twin study. J Intern Med. 2007;262(5):581–7.
Banim PJ, Luben RN, Bulluck H, Sharp SJ, Wareham NJ, Khaw KT, et al. The aetiology of symptomatic gallstones quantification of the effects of obesity, alcohol and serum lipids on risk. Epidemiological and biomarker data from a UK prospective cohort study (EPIC-Norfolk). Eur J Gastroenterol Hepatol. 2011;23(8):733–40.
Yuan S, Gill D, Giovannucci EL, Larsson SC. Obesity, Type 2 diabetes, lifestyle factors, and risk of Gallstone Disease: a mendelian randomization investigation. Clin Gastroenterol Hepatol. 2022;20(3):e529-37.
Tsai CJ, Leitzmann MF, Willett WC, Giovannucci EL. Prospective study of abdominal adiposity and gallstone disease in US men. Am J Clin Nutr. 2004;80(1):38–44.
Radmard AR, Merat S, Kooraki S, Ashraf M, Keshtkar A, Sharafkhah M, et al. Gallstone disease and obesity: a population-based study on abdominal fat distribution and gender differences. Ann Hepatol. 2015;14(5):702–9.
Gui J, Li Y, Liu H, Guo LL, Li J, Lei Y, et al. Obesity- and lipid-related indices as a predictor of obesity metabolic syndrome in a national cohort study. Front Public Health. 2023;11: 1073824.
Lin M, Xie Y, Hong L, Wu S, Deng X, Chen Y, et al. Abnormal adiposity indices are associated with an increased risk of diabetes in a non-obese Asian population. Public Health. 2024;226:144–51.
Andreotti G, Chen J, Gao YT, Rashid A, Chang SC, Shen MC, et al. Serum lipid levels and the risk of biliary tract cancers and biliary stones: a population-based study in China. Int J Cancer. 2008;122(10):2322–9.
Hung MC, Chen CF, Tsou MT, Lin HH, Hwang LC, Hsu CP. Relationship between gallstone disease and cardiometabolic risk factors in Elderly people with non-alcoholic fatty liver disease. Diabetes Metab Syndr Obes. 2020;13:3579–85.
Chen L, Qiu W, Sun X, Gao M, Zhao Y, Li M, et al. Novel insights into causal effects of serum lipids and lipid-modifying targets on cholelithiasis. Gut. 2024;73(3):521–32.
Wang J, Yang J, Chen Y, Rui J, Xu M, Chen M. Association of METS-IR index with prevalence of gallbladder stones and the age at the first gallbladder stone surgery in US adults: a cross-sectional study. Front Endocrinol (Lausanne). 2022;13:1025854.
Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, et al. Gallstones. Nat Rev Dis Primers. 2016;2:16024.
Kim JM, Lee HL, Moon W, Koh DH, Lee OY, Yoon BC, et al. Association between insulin, insulin resistance, and gallstone disease in Korean general population. Korean J Gastroenterol. 2007;50(3):183–7.
Liu Z, Kemp TJ, Gao YT, Corbel A, McGee EE, Wang B, et al. Association of circulating inflammation proteins and gallstone disease. J Gastroenterol Hepatol. 2018;33(11):1920–4.
Liu T, Siyin ST, Yao N, Duan N, Xu G, Li W, et al. Relationship between high-sensitivity C reactive protein and the risk of gallstone disease: results from the Kailuan cohort study. BMJ Open. 2020;10(9): e035880.
Petroni ML. Review article: gall-bladder motor function in obesity. Aliment Pharmacol Ther. 2000;14(Suppl 2):48–50.
Wen J, Jiang Y, Lei Z, He J, Ye M, Fu W. Leptin influence cholelithiasis formation by regulating bile acid metabolism. Turk J Gastroenterol. 2021;32(1):97–105.
Hyogo H, Roy S, Paigen B, Cohen DE. Leptin promotes biliary cholesterol elimination during weight loss in ob/ob mice by regulating the enterohepatic circulation of bile salts. J Biol Chem. 2002;277(37):34117–24.
Acknowledgements
We would like to thank all participants in this study.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
HW and QH designed the research. HW, XF, and XZ collected, analyzed the data, and drafted the manuscript. XZ revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NHANES protocol was approved by the NCHS Ethics Review Board, and informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, H., Feng, X., Huang, Q. et al. Association between lipid accumulation products and gallstones: an analysis of the National Health and Nutrition Examination Survey 2017–2020. BMC Gastroenterol 24, 311 (2024). https://doi.org/10.1186/s12876-024-03410-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03410-9