Abstract
Background
The pathological results obtained from endoscopic forceps biopsy (EFB) do not always align with the findings of postoperative endoscopic submucosal dissection (ESD). Furthermore, as ESD becomes more widespread, the number of noncurative endoscopic cases increases; thus, an accurate preoperative diagnosis and an appropriate treatment method are crucial. The purpose of this study was to explore the risk factors for postoperative pathological upgrading and noncurative resection and to gather experience in clinical and pathological diagnosis.
Methods
From March 2016 to November 2023, 292 ESD specimens were collected from 262 patients with gastric mucosal lesions. Clinicopathological information, the coincidence rate of pathological diagnosis between EFB and ESD specimens, and risk factors related to noncurative resection were analyzed retrospectively.
Results
The overall upgraded pathological diagnosis rate between EFB and ESD was 26.4%. The independent predictors for the upgraded group included proximal stomach lesions, lesion size > 2 cm, surface ulceration, and surface nodules. Twenty of the 235 early gastric cancer (EGC) patients underwent noncurative ESD resection. Multivariate analysis showed that undifferentiated carcinoma and tumor infiltration into the submucosa were significantly associated with noncurative resection.
Conclusion
Biopsy cannot fully represent the lesions of gastric intraepithelial neoplasia (GIN). When a suspected epithelial dysplasia is suspected, a careful endoscopic examination should be conducted to evaluate the lesion site, size, and surface characteristics to ensure an accurate diagnosis. Noncurative endoscopic resection is associated with undifferentiated carcinoma and submucosal infiltration. Clinicians must be familiar with these predictive factors for noncurative resection and select the appropriate treatment for their patients.
Similar content being viewed by others
Introduction
Gastric cancer (GC) is one of the most common types of cancer worldwide. Although mortality rates have been decreasing gradually, GC still ranks as the fifth most common cancer and the fourth leading cause of cancer-related deaths globally [1]. The treatment outcomes for advanced gastric cancer and early gastric cancer (EGC) differ significantly, with 5-year survival rates of less than 30% for the former and approximately 90% for the latter. Thus, early diagnosis of GC and proper treatment options are critical [2]. Previously, gastrectomy was the conventional treatment for EGC, but endoscopic submucosal dissection (ESD) is currently the preferred treatment because of its minimally invasive nature, rapid recovery, high curative ratio, and preservation of gastric function [3,4,5,6].
GC usually develops following atrophy, intestinal metaplasia, gastric intraepithelial neoplasia (GIN), intramucosal carcinoma, and invasive carcinoma (IC) [7]. GIN is a precancerous lesion, which is divided into low-grade dysplasia (LGD) and high-grade dysplasia (HGD). LGDs include mild-to-moderate dysplasia, whereas HGDs include significant dysplasia and cancer in situ [8]. An endoscopic forceps biopsy (EFB) is required to determine the preoperative diagnosis and the necessity of ESD. However, the pathological results of EFB do not always correspond to the findings of ESD, which may lead to an underestimation of a higher-grade dysplasia. These inconsistencies are classified as downgrades and upgrades. Moreover, there is a significant increase in the incidence of lymphovascular/perineural and submucosal invasion in the pathological upgrading group, leading to endoscopic noncurative resection and an unfavorable prognosis [9, 10]. Therefore, the aim of this study was to investigate the histopathological diagnostic coincidence rate between preoperative biopsy and postoperative ESD, explore risk factors for postoperative pathological upgrading and noncurative resection, and gather experience in clinical and pathological diagnosis.
Materials and methods
Data collection and grouping methods
This study was approved by the Ethics Committee of Zibo Municipal Hospital. From March 2016 to November 2023, 262 patients with 292 ESD specimens were retrospectively analyzed. The following information was collected: patient sex and age, lesion site, number of biopsy blocks, lesion size and macroscopic type, whether the surface was red, whether there were ulcers and nodules on the surface, and pathological findings on the EFB and ESD. The pathological data of all patients were re-evaluated by two pathologists with over five years of expertise. The inclusion criteria were as follows: (a) the patient must be at least 18 years old and have signed an informed consent before ESD; (b) EFB had to be performed before ESD; (c) computed tomography (CT) should not detect any indications of lymph node or systemic metastasis; and (d) the duration between biopsy and ESD should not exceed one month. The exclusion criteria were as follows: (a) incomplete clinical and pathological records; (b) lack of preliminary EFB results; (c) a neuroendocrine tumor, stromal tumor, or ectopic pancreatic diagnosis before ESD treatment. The existence of multiple lesions requires the consideration of each lesion as a unique case, with distinctions based on their respective pathological features.
This study followed the pathological diagnostic criteria of the World Health Organization (WHO) [8]. Patients with different pathological results, including nonneoplastic lesions (including gastritis and polyps), LGD, HGD, EGC, and progressive cancer, were included. We categorized the lesions into three groups based on the histological discrepancies between the EFB and ESD specimens. The first group, called the consistent group, included patients with the same diagnosis based on both EFB and ESD specimens. The second group, known as the upgraded group, consisted of patients in which subsequent ESD specimens showed a greater likelihood of malignancy, such as progression from LGD to HGD/adenocarcinoma or from HGD to adenocarcinoma. The third group, referred to as the downgraded group, included patients in which subsequent ESD specimens revealed a lower likelihood of malignancy, such as from HGD to LGD/nonneoplastic lesions or from LGD to nonneoplastic lesions [11, 12].
EFB process and endoscopic features
In order to identify potential lesions, the color, shape, texture, and distribution of mucosal blood vessels within the digestive tract are examined under white light endoscopy (WLE). If suspected epithelial dysplasia was found, lesion-targeted EFB was performed. Biopsy forceps (MTN-BF-23/18-A-1; Nanjing Micro-Tech Co., Ltd., Nanjing, China) with an opening diameter of 6 mm were used to estimate the lesion size. Ulcers, hemorrhage, and local fibrosis may be induced by multiple biopsies, which may increase the risk of adverse events and the difficulty of endoscopic therapy. Consequently, Chinese expert consensus suggests that 1–2 biopsies should be conducted for lesions with a diameter of less than 2 cm, and an additional biopsy should be obtained for every 1 cm increase in diameter. Sampling in the central region of the ulcer should be avoided, as it is frequently necrotic tissue and can easily result in hemorrhage and perforation [13].
Data on the macroscopic characteristics, including lesion site, lesion size, macroscopic type, and surface features, were collected from endoscopic reports. The stomach is divided into three parts based on its anatomical structure: proximal (cardia and fundus), middle (body), and distal (angle, antrum, and pylorus). The Paris classification was used to categorize macroscopic tumor types as elevated (0-I, 0-IIa), flat (0-IIb), or depressed (0-IIc, 0-III) [14]. Surface redness was defined as the surface of the lesion mucosa being redder than the surrounding mucosa, and surface nodules were defined as nodular or irregularly raised mucosa [15, 16]. Figure 1 depicts the following endoscopic characteristics in order: surface redness, surface nodules, and surface ulceration.
Indications for ESD
In addition to pathological diagnosis, the ultimate selection of ESD treatment should rely on a comprehensive risk-benefit analysis. Before ESD, endoscopic ultrasonography was used to assess the depth of tumor invasion and contrast-enhanced CT of the abdomen was used to evaluate lymph nodes and distant metastases. The Japanese ESD treatment guidelines for EGC (version 2) [3] classify the indications for ESD into three categories: absolute, expanded, and relative. The absolute indications were as follows: (1) intramucosal differentiated carcinoma, without ulceration, regardless of tumor size; (2) intramucosal differentiated carcinoma ≤ 3 cm in size with ulceration; and (3) intramucosal undifferentiated carcinoma ≤ 2 cm in size without ulceration. After the initial ESD resection, the expanded indications included local recurrence of an intramucosal differentiated malignant tumor with an endoscopic cure rate (eCura) of C-1. Cases that did not meet the criteria for absolute or extended indications and were unable to receive surgical treatment due to the following conditions were included: (1) intramucosal undifferentiated carcinoma > 2 cm in size without ulceration. (2) intramucosal differentiated carcinoma > 3 cm in size with ulceration. (3) intramucosal undifferentiated carcinoma with ulceration; and (4) submucosal invasive carcinoma, regardless of lesion size, type, or presence of ulceration.
ESD process
The steps in the procedure are as follows: lesion identification, lesion marking, submucosal injection, and submucosal dissection. ESD was performed using a one-channel endoscope (EPK-i7000; Pentax Medical Co., Tokyo, Japan). Before performing ESD, an endoscopic examination was carried out to identify the exact boundary of the lesion, and mucosal markings were primarily made by electrocoagulation 3 to 5 mm away from the lesion’s border. After placing numerous dots around the lesion, normal saline mixed with methylene blue and epinephrine was injected into the submucosal layer. A needle knife was used to make a small cut, which was then followed by a circular cut outside the marked area. Subsequently, the submucosal layer was dissected parallel to the muscular layer using an endoscopic scalpel (MK-T-2-195; Nanjing Micro-Tech Co., Ltd., Nanjing, China) until the lesion was entirely removed. To achieve preventive hemostasis, coagulation was applied to all visible, nonbleeding vessels. To avoid folding, the resected specimen was immediately stretched, attached to a flat foam board, and marked on both the oral and anal sides. The specimens were subsequently soaked in 10% formalin for 24–48 h and sent to pathologists.
Pathological section production
Prior to sampling, a full image of the specimen was captured to document its dimensions, color, texture, and shape, as well as its distance from the resection boundary. The horizontal and vertical margins were marked with different colors of dye. Sections were started along the line with the shortest distance from the edge of the lesion to the lateral margin of the specimen, and then were serially sectioned parallel to this line with an interval of 2.0 to 3.0 mm. After sampling, tissue strips were sequentially placed into the embedding box, with each box containing ≤ 3 strips, and the sequence was recorded. When the length of the mucosa exceeded the length of the embedding box, the specimen was cut vertically into two sections and placed in the same embedding box. It is vital to remember that before placing the tissue, a layer of sponge should be placed in the embedding box, followed by the mucosa. The tissue’s surface should then be covered with another layer of sponge, and a mark should be put on the same side to ensure consistent embedding orientation. After dehydrating and dipping the tissue in wax, the technician turned the strip over 90° on the same side, cut the side facing down, and embedded it consecutively, with the first and last piece embedded 90° in reverse to observe the horizontal margin around the entire mucosa. Finally, the obtained formalin-fixed paraffin-embedded (FFPE) tissues were serially sectioned at 2 mm intervals, stained with hematoxylin-eosin (HE), and viewed under a microscope.
Pathological examination of ESD specimens
The pathological data of all patients were re-evaluated by two pathologists with over five years of expertise. After excluding biopsy-caused ulcers, surface ulcers were ruled as positive [17]. Histological evaluation was performed in accordance with the diagnostic criteria for the digestive system established by the World Health Organization. The differentiated adenocarcinoma types included well- or moderately differentiated papillary adenocarcinoma and tubular adenocarcinoma, while poorly differentiated adenocarcinoma, signet-ring cell carcinoma, and mucinous adenocarcinoma were categorized as undifferentiated. The pathological results of the ESD specimens included tumor size, histological classification, invasion depth, presence of ulceration (UL), involvement of venous (V) and/or lymphatic (Ly) vessels, and resection margins [vertical margin (VM) and horizontal margin (HM)]. The muscularis mucosae served as a reference point to ascertain the degree of tumor invasion (Fig. 2). Therefore, the depth of tumor invasion was categorized as M (mucosal invasion), SM1 (submucosal invasion within 500 μm from the bottom margin of the muscularis mucosa), or SM2 (tumor invasion into the submucosa exceeding 500 μm from the muscularis mucosa). Endoscopic curability was evaluated using the aforementioned variables.
Infiltration characteristics of early gastric cancer after endoscopic submucosal dissection (hematoxylin-eosin staining, 100 x). (A) Tumor invasion into the lamina propria. (B) Tumor infiltrating the muscularis mucosa layer. (C) Submucosal invasion within 500 μm from the muscularis mucosa. (D) Submucosal infiltration exceeding 500 μm from the muscularis mucosa. (E) Tumor infiltration with lymphovascular embolus. (F) Tumor with a positive vertical margin (red arrow)
Criteria for curative and noncurative resection of ESD specimens
The ESD treatment guidelines for EGC [3] describe curative resection as a pathological evaluation that meets the criteria for endoscopic curability A (eCuraA) or B (eCuraB). eCuraA: If a lesion is removed en bloc and meets all of the following requirements: (1) pT1a, mainly differentiated type, UL0, V0, Ly0, HM0, VM0, regardless of size; (2) pT1a, tumor size ≤ 2 cm, mainly undifferentiated type, UL0, V0, Ly0, HM0, VM0; or (3) pT1a, tumor size ≤ 3 cm, mainly differentiated type, UL1, V0, Ly0, HM0, VM0. eCuraB: If a lesion is resected en bloc, the tumor size ≤ 3 cm in size, is mostly differentiated, and fits the following conditions: pT1b1 (SM1), V0, Ly0, HM0, and VM0. CuraC is a lesion that does not meet any of the eCuraA or eCuraB requirements specified above, indicating the possibility of a residual tumor. When eCuraC lesions are differentiated and meet other criteria for classification into eCuraA or eCuraB but were not resected en bloc or have positive HM, they are classified as eCuraC-1. All other eCuraC lesions are classified as eCuraC-2.
Statistical analysis
IBM SPSS Statistics version 26 was used for the statistical analyses (IBM Corp., Armonk, NY, USA). Categorical and continuous variables were expressed as the n (%) and mean ± standard deviation, respectively. The chi-square or Fisher’s exact test for categorical variables and Student’s t-test for continuous variables were used in univariate analysis to determine risk factors for pathological upgrading and noncurative endoscopic resection. Variables with p < 0.05 were further analyzed using multiple logistic regression models. P < 0.05 was considered to indicate statistical significance.
Results
General clinical features
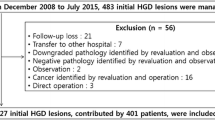
A total of 274 patients received gastric ESD, of whom 12 were excluded (10: incomplete data, 2: non-epithelial neoplastic lesions). Finally, 262 patients (292 ESD specimens) were included in the study for analysis (Fig. 3). Table 1 summarizes the baseline information of the selected patients, including their frequency distributions and relevant clinical features. The patients were primarily male (71.9%), with a male-to-female ratio of 2.56:1. The average age (± standard deviation) was 61.86 ± 10.30 years. Of 292 lesions, 44 (15.1%) were found in the proximal stomach, 83 (28.4%) in the middle stomach, and 165 (56.5%) in the distal stomach. Thirty patients had multiple lesions. There were 51 (17.5%) lesions with a diameter greater than 2 cm, while 241 (82.5%) had a diameter less than 2 cm. Surface nodules, redness, and ulceration were observed in 41 (14.0%), 143 (49.0%), and 35 (12.0%) lesions, respectively. There were 90 (30.8%) cases of the elevated type, 49 (16.8%) cases of the flat type, and 153 (52.4%) cases of the depressed type.
Pathological assessment after ESD
After reviewing the pathological slides, the final ESD diagnoses included 15 (5.1%) cases of nonneoplastic lesions, 42 (14.4%) cases of LGD, and 235 (80.5%) cases of EGC, with the latter comprising 158 (54.1%) cases of HGD and 77 (26.4%) cases of IC (Table 1). Ulceration was observed in 16 (5.5%) specimens, including 2 (0.7%) cases of nonneoplastic lesions, 2 (0.7%) cases of HGD, and 12 (4.1%) cases of IC. Three (1.0%) cases exhibited positive horizontal margins, including two (0.7%) with IC and one (0.3%) with HGD. Six (2.1%) cases demonstrated positive vertical margins, all of which were classified as IC. Lymphovascular tumor emboli were found in eight (2.7%) cases. Among the 235 cases with EGC, 205 (87.2%) had intramucosal carcinomas (pTl a, including 158 (67.2%) cases with HGD and 47 (20%) cases with intramucosal IC), whereas 30 (12.8%) cases had submucosal infiltration, with 18 (7.7%) cases with infiltration < 500 μm (pTlbl, SMl), and 12 (5.1%) cases with infiltration ≥ 500 μm (pTlb2, SM2).
Comparison of pathological diagnoses between the EFB and ESD specimens
Table 2 presents the results of both EFB and ESD. Of the 292 cases, 21 (7.2%) were classified as nonneoplastic, 18 (6.2%) as LGDs, 236 (80.8%) as HGDs, and 17 (5.8%) as IC with EFB. A total of 187 patients were pathologically identical between the EFB and ESD specimens, with a concordance rate of 64.0% (187/292). The overall upgraded pathological diagnostic rate was 26.4% (77/292), and the overall downgraded pathological diagnosis rate was 9.60% (28/292). Of the 21 patients initially diagnosed with gastritis by EFB, ten (47.6%) were upgraded to LGD. Of the 18 patients initially diagnosed with LGD by EFB, three (16.7%) were downgraded to gastritis, while seven (38.9%) were upgraded to HGD. Furthermore, of the 236 patients initially diagnosed with HGD, 60 (25.4%) were ultimately diagnosed with IC, 151 (64.0%) remained with HGD, and 24 (10.2%) and 1 (0.4%) were downgraded to LGD and gastritis following ESD, respectively. Representative images depicting the differences between EFB and ESD are shown in Fig. 4.
Representative images of preoperative endoscopic biopsy and postoperative ESD examination in GIN patients (hematoxylin-eosin staining, 200 x). (A-B) Endoscopic biopsy specimen showing LGD, whereas ESD specimen showing HGD. (C-D) Endoscopic biopsy specimen showing HGD, whereas ESD specimen showing moderately differentiated adenocarcinoma
Univariate analysis of pathological upgrading after ESD
The lesions were separated into two groups based on pathological results (diagnose upgrading, diagnosis consistent/downgrading), and the causes for the differences between the two groups were investigated. Table 3 shows that pathological upgrading was significantly impacted by proximal stomach lesions, greater tumor size (> 2 cm), surface ulceration, surface nodules, and only one biopsy when compared to the two groups (all with p < 0.01).
Multivariate logistic regression analysis of pathological upgrading after ESD
Factors with p < 0.05 were selected by univariate analysis, including lesion site, lesion size, surface ulceration, surface nodules, and biopsy block as independent variables, and pathological escalation after ESD as dependent variables for logistic regression analysis. Proximal stomach lesions (odds ratio [OR]: 2.244; 95% confidence interval [CI]: 1.079–4.664; p = 0.030), lesion size > 2 cm (OR: 1.748; 95% CI: 1.312–2.330; p < 0.001), surface ulceration (OR: 0.155; 95% CI: 0.071–0.340; p < 0.001), and surface nodules (OR: 0.231; 95% CI: 0.120–0.446; p < 0.001) were found to be independent predictors for the upgraded group (Table 4).
Evaluating the curability and independent risk factors for noncurative resection
Table 5 shows the clinicopathological characteristics of patients with EGC in relation to their post-ESD curability outcomes. The patients were classified into two groups based on whether they underwent curative or noncurative resection. Of the 235 EGC cases, 215 (91.5%) underwent curative ESD, and 20 (8.5%) underwent noncurative resection. There were no differences in age, gender, or macroscopic type between the two groups; however, certain features of EGC, such as undifferentiated carcinoma (40%), proximal stomach lesions (40%), lesions larger than 2 cm (60%), and submucosal invasion (90%), were more common in the noncurative resection group.
Multivariate logistic regression analysis indicated that undifferentiated carcinoma (OR: 10.638; 95% CI: 1.303–86.850; p = 0.027) and submucosal invasion (OR: 102.241; 95% CI: 17.904-583.844; p < 0.001) were independent risk factors for noncurative resection of ESD (Table 6).
Discussion
GIN is a precancerous lesion with the potential to be malignant and requires therapy based on its histological grade. EFB and ESD are the most commonly used methods for diagnosing and treating GIN. However, the outcomes of biopsy specimens do not always match those of ESD samples. Thus, GIN diagnosed by EFB does not guarantee that there are no higher-grade tumor foci throughout the lesion.
Approximately 60–85% of patients with HGD will develop gastric cancer [18], so it is more rational to actively implement ESD for patients whose endoscopic biopsy results indicate HGD. Although LGD often manifests as a gradual development, 23% of patients progress to malignancy [18]. Jiu Won Hwang et al. [19] have shown that utilizing magnifying endoscopy (ME) in conjunction with narrow-band imaging (NBI), LGD lesions with well-defined boundaries and aberrant glandular duct opening morphology and/or microvascular morphology in the surface microstructure may suggest possible pathological upgrading. As a result, we advocate doing a standardized endoscopic evaluation of all lesions diagnosed as LGD by biopsy, with a special emphasis on the lesions’ boundary and surface microstructure using ME + NBI. A biopsy alone is insufficient for LGD lesions larger than 2 cm in size and/or with apparent boundaries and abnormal surface microstructure; diagnostic ESD resection is required instead [20].
Studies have indicated that the coincidence rate of pathological diagnosis between preoperative biopsy and postoperative ESD was 41.9–66.1%, whereas the upgrade rate of post-ESD diagnosis was 16.3 ~ 44.9% [11, 12, 21,22,23]. Consistent with the above reported statistics, our study revealed that the diagnostic coincidence rate before and after ESD was 64.0%, and the postoperative diagnostic upgrade rate was 26.4%. The postoperative pathological upgrading rates of nonneoplastic and LGD lesions were 47.6 (10/21) and 38.9% (7/18), respectively, which were greater than the rates reported in prior research [7, 12, 24]. The following factors may contribute to this disparity: First, there are insufficient biopsies. Second, the biopsy process is confined to clamping mucosal and submucosal tissues, leaving deeper abnormalities undetected. Third, lesions frequently have numerous components, such as nonneoplastic lesions, LGD, HGD, and IC, and the most severe lesions were not found during the endoscopic biopsy. Fourth, the nonneoplastic lesions that received ESD treatment were those assessed to have malignant potential by endoscopists and were chosen a second time, which could not represent the pathological upgrading of all nonneoplastic lesions. It is suggested that EFB diagnosis of nonneoplastic lesions (including gastritis and polyps) cannot entirely rule out the possibility of precancerous lesions. Special attention should be given to cases exhibiting the following endoscopic features, and if necessary, ESD is a feasible option: flat or depressed morphology, surface ulceration, and diameter exceeding 2 cm.
Postoperative pathological upgrading can occur for a variety of reasons, including macroscopic type, lesion location, lesion size, surface appearance (ulceration, nodule, and redness), and number of biopsies [7, 11, 12, 17, 25]. Multivariate regression analysis revealed that proximal stomach lesions (OR: 2.244; 95% CI: 1.079–4.664; p = 0.030), lesion size > 2 cm (OR: 1.748; 95% CI: 1.312–2.330; p < 0.001), surface ulceration (OR: 0.155; 95% CI: 0.071–0.340; p < 0.001), and surface nodules (OR: 0.231; 95% CI:0.120–0.446; p < 0.001) were risk factors for pathological upgradation. The upper 2/3 of the stomach is susceptible to pathological development because of the following factors: (1) Lesions in the middle or upper section of the stomach are more difficult to identify than those in the lower part due to the vast number of mucosal folds and limited observation area during gastroscopy. (2) Compared to the lower region, the cardia region has a greater density of lymphatic vessels, which increases the risk of tumor spread.
Curative resection is the aim of endoscopic resection for EGC; however, unintentional noncurative resection can occur under a variety of circumstances. The incidence of noncurative resection in our study was 8.5%, which was lower than that reported in previous studies [12, 26,27,28]. The small sample size of our analysis may have contributed to this discrepancy. Several previous studies have examined the risk variables linked to noncurative resection. In a study of 89 patients who underwent ESD, those with undifferentiated tumors, submucosal infiltration, vascular invasion, a positive vertical margin, and positive human epidermal growth factor receptor-2 (HER-2) had the highest chance of not being able to undergo curative resection [29]. A retrospective analysis of 3094 patients with EGC who underwent ESD therapy was performed to identify the risk factors related to noncurative resection. In that study, noncurative resection was associated with the following five factors: old age, undifferentiated tumor, tumor size > 2 cm, ulcer, and upper body tumor [26]. Furthermore, a study indicated that a tumor size greater than 2 cm, intraoperative bleeding, and Helicobacter pylori infection were risk factors for noncurative resection [30]. Another study revealed that undifferentiated carcinoma and tumors of the elevated or depressed type were risk factors [31]. In addition to lesion features, the effects of the surgical technique used by the endoscopist were also analyzed [32]. In the present study, undifferentiated tumors and submucosal infiltration were associated with noncurative resection. Taken together, the primary factors that rendered resection less likely to be successful were tumor location in the upper stomach, larger tumor size, ulceration, undifferentiated tumor, submucosal infiltration, vascular invasion, and positive margin.
There were some limitations in this study. First, owing to the retrospective nature of this study, there is a potential for bias in patient selection. Second, this study was conducted at a single center with a limited number of participants. Therefore, it is necessary to conduct larger clinical trials to thoroughly assess the risk variables associated with pathological upgrading and noncurative resection in patients with EGC. Third, the biopsies exhibited variations in both size and depth between patients. Biopsies that are either insufficient in size or quantity tend to underestimate the severity of GIN. Fourth, there were no magnifying endoscopy results within the collected data; therefore, the conclusions reached are limited. In the future, the author plans to enlarge the research facility, increase the number of patients, and add the findings of magnifying endoscopy to the study to improve data representativeness.
Conclusions
In conclusion, if the lesion is located in the proximal portion of the stomach, is larger than 2 cm, and has ulcers or nodules on the surface, there is a substantial risk of pathological upgradation following ESD. Noncurative endoscopic resection is associated with depth of invasion, and histological type. To reduce unnecessary endoscopic ESD therapy, doctors should understand the predictors of noncurative endoscopy, thoroughly analyze endoscopic performance, and select the optimal treatment option for EGC patients.
Data availability
The data information used during this study are available from the corresponding author on reasonable request.
Abbreviations
- ESD:
-
Endoscopic submucosal dissection
- EGC:
-
Early gastric cancer
- EFB:
-
Endoscopic forceps biopsy
- GC:
-
Gastric cancer
- GIN:
-
Gastric intraepithelial neoplasia
- IC:
-
Invasive carcinoma
- LGD:
-
Low-grade dysplasia
- HGD:
-
High-grade dysplasia
- LNM:
-
Lymph node metastasis
- CT:
-
Computed tomography
- WHO:
-
World Health Organization
- UL:
-
Ulceration
- V:
-
Venous vessels
- Ly:
-
Lymphatic vessels
- VM:
-
Vertical margin
- HM:
-
Horizontal margin
- M:
-
Mucosal invasion
- SM1:
-
Submucosal invasion within 500 μm from the bottom margin of the muscularis mucosa
- SM2:
-
Tumor invasion into the submucosa exceeding 500 μm from the muscularis mucosa
- HER-2:
-
Human epidermal growth factor receptor-2
- NBI:
-
Narrow-band imaging
- eCura:
-
endoscopic cure rate
- WLE:
-
White light endoscopy
- FFPE:
-
Formalin-fixed paraffin-embedded
- HE:
-
Hematoxylin-eosin
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ME:
-
Magnifying endoscopy
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Embaye KS, Zhang C, Ghebrehiwet MA, et al. Clinico-pathologic determinants of non-e-curative outcome following en-bloc endoscopic submucosal dissection in patients with early gastric neoplasia. BMC Cancer. 2021;21:92.
Ono H, Yao K, Fujishiro M, et al. Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition). Dig Endosc. 2021;33:4–20.
Lee SH, Kim MC, Jeon SW, et al. Risk factors and clinical outcomes of non-curative resection in patients with early gastric Cancer treated with endoscopic submucosal dissection: a retrospective Multicenter Study in Korea. Clin Endosc. 2020;53:196–205.
Shichijo S, Uedo N, Kanesaka T, et al. Long-term outcomes after endoscopic submucosal dissection for differentiated-type early gastric cancer that fulfilled expanded indication criteria: a prospective cohort study. J Gastroenterol Hepatol. 2021;36:664–70.
Tanaka S, Kashida H, Saito Y, et al. Japan gastroenterological endoscopy society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020;32:219–39.
Li L, Zhou S, He C. Clinical characteristics and risk factors for upgraded pathology in patients with gastric intraepithelial neoplasia after endoscopic submucosal dissection. Rev Esp Enferm Dig. 2022;114:725–30.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182–8.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021; 24:1–21.
Yun HR, Huh CW, Jung DH, et al. Machine learning improves the prediction rate of non-curative resection of endoscopic submucosal dissection in patients with early gastric Cancer. Cancers (Basel). 2022;14:3742.
Noh CK, Jung MW, Shin SJ, et al. Analysis of endoscopic features for histologic discrepancies between biopsy and endoscopic submucosal dissection in gastric neoplasms: 10-year results. Dig Liver Dis. 2019;51:79–85.
Zhao YH, Zheng Y, Sha J, et al. A prediction model based on the risk factors Associated with pathological upgrading in patients with early-stage gastric neoplasms diagnosed by endoscopic forceps Biopsy. Gut Liver. 2023;17:78–91.
Ping Wang P, Li Y, Chen, et al. Chinese integrated guideline on the management of gastric precancerous conditions and lesions. Chin Med. 2022;17:138.
Endoscopic Classification Review Group. Update on the Paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;37:570–8.
Maekawa A, Kato M, Nakamura T, et al. Incidence of gastric adenocarcinoma among lesions diagnosed as low-grade adenoma/dysplasia on endoscopic biopsy: a multicenter, prospective, observational study. Dig Endosc. 2018;30:228–35.
Nam HS, Choi CW, Kim SJ, et al. Endoscopic predictive factors associated with local recurrence after gastric endoscopic submucosal dissection. Scand J Gastroenterol. 2018;53:1000–7.
Yabuuchi Y, Takizawa K, Kakushima N, et al. Discrepancy between endoscopic and pathological ulcerative findings in clinical intramucosal early gastric cancer. Gastric Cancer. 2021;24:691–700.
Sung JK. Diagnosis and management of gastric dysplasia. Korean J Intern Med. 2016;31:201–9.
Hwang JW, Bae YS. Mi Seon Kang. Predicting pre- and post-resectional histologic discrepancies in gastric low-grade dysplasia: a comparison of white-light and magnifying endoscopy. Gastroenterol Hepatol. 2016;31(2):394–402.
National Clinical Research Center for Digestive Disease (Shanghai), National Early Gastrointestinal-Center Prevention & Treatment Center Alliance, Helicobacter Pylori Group, et al. Chinese consensus on management of gastric epithelial precancerous conditions and lesions (2020). Chin J Dig et al. 2020; 40: 731–741.
RYU DG, Choi CW, Kang DH, et al. Pathologic outcomes of endoscopic submucosal dissection for gastric epithelial neoplasia. Medicine. 2018;97:e11802.
Zhou J, Li Y, Xiao J, et al. Discussion on pathological differences between preoperative biopsy and postoperative pathology of endoscopic submucosal dissection for gastric intraepithelial neoplasia. Clin J Gastrointest Endoscopy. 2019;6:97–101.
Yang L, Jin P, Wang X, et al. Risk factors associated with histological upgrade of gastric low-grade dysplasia on pretreatment biopsy. J Dig Dis. 2018;19(10):596–604.
Baek IH, Kim KO, Choi MH, et al. What is most important to the Endoscopist for Therapeutic Plan? Morphology versus Pathology: a Nationwide Multicenter Retrospective Study in Korea. Am Surg. 2018;84:644–51.
Yin Y, Wang T, Zhang P, et al. A novel model predicts postoperative pathology of colorectal high-grade intraepithelial neoplasia. J Surg Res. 2019;240:104–8.
Lee SH, Kim MC, Jeon SW, et al. Risk factors and clinical outcomes of non-curative resection in patients with early gastric cancer treated with endoscopic submucosal dissection: a retrospective multicenter study in Korea. Clin Endosc. 2019;53(2):196–205.
Hatta W, Gotoda T, Oyama T, et al. Is radical surgery necessary in all patients who do not meet the curative criteria for endoscopic submucosal dissection in early gastric cancer? A multi-center retrospective study in Japan. J Gastroenterol. 2017;52(2):175–84.
Nam HS, Choi CW, Kim SJ, et al. Preprocedural prediction of non-curative endoscopic submucosal dissection for early gastric cancer. PLoS ONE. 2018;13:e0206179.
Duan K, Li D, Shi D et al. Risk Factors and Timing of Additional Surgery after Noncurative ESD for Early Gastric Cancer. Can J Gastroenterol Hepatol. 2022; 21:2022:3421078.
De Marco MO, Tustumi F, Brunaldi VO, et al. Prognostic factors for ESD of early gastric cancers: a systematic review and meta-analysis. Endosc Int Open. 2020;8:E1144–55.
Ohara Y, Toshikuni N, Matsueda K, et al. The superficial elevated and depressed lesion type is an independent factor associated with non-curative endoscopic submucosal dissection for early gastric cancer. Surg Endosc. 2016;30:4880–8.
Toyokawa T, Inaba T, Omote S, et al. Risk factors for non-curative resection of early gastric neoplasms with endoscopic submucosal dissection: analysis of 1,123 lesions. Exp Ther Med. 2015;9:1209–14.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HPY and PJW conceived、designed the study, collected the data, performed the statistical analyses, and drafted the manuscript. XZ, DX and RCW provided useful input for the analyses and helped to edit the manuscript. All authors have read, reviewed, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Zibo Municipal Hospital (No. 20240219). Written informed consent was not required due to the retrospective nature of the study, and the need for consent to participate was also waived by the ethics committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, P., Zhao, X., Wang, R. et al. Risk factors for pathological upgrading and noncurative resection in patients with gastric mucosal lesions after endoscopic submucosal dissection. BMC Gastroenterol 24, 253 (2024). https://doi.org/10.1186/s12876-024-03342-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03342-4