Abstract
Purpose
To evaluate the impact of two different parameters (body position and distension medium) on the rectal sensory test in patients with functional constipation and provide data support for the development of standardized operating procedures in clinical practice.
Methods
Based on a single-center process of the rectal sensory test, 39 patients with functional constipation were recruited for rectal sensory test under different body positions and distension mediums.
Results
Among the items of the Constipation Scoring System, the score of frequency of bowel movements showed a negative correlation with the first constant sensation volume (r = -0.323, P = 0.045). Conversely, the score of painful evacuation effort showed a positive correlation with the desire to defecate volume (r = 0.343, P = 0.033). There was a statistically significant difference in the first constant sensation volume (when the distension medium was gas) measured in different body positions (left lateral position, sitting position, squatting position), and the data measured in the squatting position were significantly higher than those in left lateral position (P < 0.05). In terms of research on distension medium, it was found that the first constant sensation volume measured in the squatting position (when the distension medium was water) was significantly lower than that of gas (P < 0.05).
Conclusion
For patients with functional constipation, there are differences in the results of rectal sensory tests between body positions and distension mediums. When conducting multicenter studies, it is necessary to unify the standard operating procedure (SOP) for operational details to ensure consistency and reliability of the test results.
Similar content being viewed by others
Introduction
Functional constipation is a common clinical disease characterized by reduced bowel movements, dry stools, and difficulty in defecation [1]. With the increasing trend of population aging, its incidence rate is increasing year by year. The latest epidemiological data suggest that the global incidence of functional constipation is 11.6–32.3% [2,3,4,5]. However, due to issues such as poor clinical treatment efficacy, drug abuse, and susceptibility to recurrence, the prevention and clinical treatment of functional constipation have become common focuses of attention worldwide [6].
With in-depth research on its pathogenesis, the important role of rectal sensation in defecation has gradually been recognized, and rectal hyposensitivity (RH) is considered an important cause of functional constipation [7]. RH was first described in 1951 in patients who had undergone parasympathetic block prior to surgery [8]. RH is presented as a diminished perception of rectal distension and defined as an elevation of 1 or more of the 3 sensory thresholds (FCSV, DDV and MTV) in most studies [9]. Abnormal visceral sensitivity is widely considered important in the development of functional bowel disorders; however, the role of visceral insensitivity remains relatively unexplored compared with the study of visceral hypersensitivity in the past [10]. Normal rectal sensory function is crucial for the defecation process [11]. 48% of patients with constipation have impaired rectal sensation as the only abnormality during physiological examinations [10]. RH may participate in the occurrence and development of constipation through various mechanisms, leading to symptoms such as weakening of the desire to defecate, prolonged bowel movements, and incomplete rectal emptying [12, 13]: (1) stool retention: the lack of desire to defecate can lead to retention of feces, and the accumulation of more dry and hard feces will make it more difficult to discharge (and likely cause further dilation of the rectum); (2) reduced rectal contractility: when RH is accompanied by rectal dilation, it can reduce rectal contractility and affect bowel movements; (3) primary colonic peristalsis disorder: one-third of RH patients have been confirmed to have delayed colonic transmission, which may reflect a primary colonic peristalsis disorder.
An anorectal physiology analysis is conducted for patients with symptoms of anorectal dysfunction to identify potential pathophysiological mechanisms. Measurement of the rectal sensory threshold is one of the steps in the diagnosis of functional bowel dysfunction. The International Anorectal Physiology Working Group (IAPWG) published a standardized measurement protocol for anorectal function testing in 2020, but the details of sensory threshold measurement still need to be further clarified [14]. The inconsistency in specific measurement details has led to heterogeneity in various studies [15, 16]. There are many influencing factors for this method, which leads to heterogeneity among various studies. The influencing factors include [14, 17,18,19] (1)the type of distension: ramp distension and phasic distension; (2)distension medium: gas and water; (3)inflation rate: 10 ~ 100 mL/mins; (4)the distance of the balloon from the anal margin; (5)Examination position. The traditional measurement method is the left lateral position, which is not in line with human physiological defecation, and its data may affect the judgment of clinical physicians [20, 21]. Especially when required to perform defecation in lateral position, some patients may exhibit abnormal contraction or incomplete relaxation of anal pressure due to their inability to adapt to the lateral lying position bowel habits [22]. Different stool types can affect bowel movement [11, 23]. Therefore, it is necessary for pelvic floor surgeons to study and formulate a unified standard. Therefore, this single-center study was conducted to analyze the impact of different test parameters (body position and expanding medium) on rectal sensory tests in patients with functional constipation and to explore appropriate detection processes and technical parameters.
Patients and methods
This study recruited patients with functional constipation from the Anorectal Clinic from June 2021 to February 2022 to perform rectal sensory tests with different positions and distension mediums. The patient met the Roman IV diagnostic criteria for functional constipation [24]. Exclusion criteria: (1) patients with acute perianal disease accompanied by infection or bleeding symptoms. (2) Patients with rectal prolapse, rectal protrusion, and other organ prolapse. (3) patients who have undergone surgery for benign perianal diseases. (4) patients with diabetes mellitus accompanied by poorly controlled blood sugar or diabetic neuropathy. (5) patients with severe mental illness who could not cooperate with the examination; (6) patients with drug-induced constipation and secondary constipation with clear etiology, such as Parkinson’s disease, hypothyroidism, and spinal cord injury.
Procedures
The rectal sensory test, including the first constant sensation volume (FCSV), desire to defecate volume (DDV), and maximum tolerated volume (MTV), was performed using a catheter and balloon equipped with an anorectal motility analyzer (Triton, Leibri, Canada). Two hours before the test, 20 ml of a glycerin enema was used to empty feces from the rectum, and the given patient was informed of the meaning of FCSV, DDV and MTV [14]. The specific procedures of anorectal pressure test were as follows: rest, squeeze, long (endurance) squeeze, cough, and push. The whole process should be explained in detail to the patient [14]. First, the pressure-measurement tube was put into the anus and tell the patient to relax and remain quiet to avoid movement artifact, which lasted for 60 s. Secondly, ask the patient to contract his anus for 5 s 3times separated by a 30-s between‐maneuver recovery interval. Thirdly, the patient was then asked to perform a sustained contraction for 30 s and the pressure was recordedrecords the anal pressure during sustained voluntary effort over 30 s. A single endurance squeeze is performed followed by a 60‐s between‐maneuver recovery interval. Fourthly, the patient was asked to perform the coughing maneuver twice, 30s apart, and the change in pressure was observed. Fifthly, the patient was asked to perform three simulated defecation movements, each 15s, with an interval of 30s. Body position and distension parameters were fixed in the study for evaluation purposes, with the specific parameters as follows: (1) distension method: continuous balloon distension method was used to inject gas or water at a rate of 1 mL/s; (2) distension medium: gas and water (at room temperature) for patients separately; (3) distension speed: injection with a handheld syringe at a speed of 1 mL/s; (4) distance between the bottom of the balloon and the anal margin: 5 cm; (5) position: left lateral position, squatting position, and sitting position separately, with an interval of 10 min between each measurement position. Considering the safety of detecting MTV (balloon bursting, balloon unable to pump water), an MTV warning line of 180 ml was set in this study (if it was over 180 ml, water injection was stopped); (6) fixation of the balloon position: a piece of transparent adhesive tape was used to fix the catheter to the left perianal skin 1–2 cm from the anus to keep the tube somewhat movable but not easily dislodged during the test. If the catheter became dislodged or displaced during the three-position test, the catheter had to be reattached and the test repeated. All patients were tested by the same therapist and placed in the left lateral position for balloon insertion using the same test sequence of left lateral position (gas), left lateral position (water), sitting position (gas), sitting position (water), squatting position (gas) and squatting position (water). The schematic diagram shows the method of fixing the catheter and the position of the patient for examination (Fig. 1).
Statistical analysis
Quantitative variables are presented herein as the mean ± SD. Qualitative variables are presented as counts (percentages). For the comparison of measurement data between the two groups, the normality test was first conducted, the t test was used for the normal distribution and the homogeneity of variance, and the Mann‒Whitney U nonparametric test was used for the nonnormal distribution. One-way ANOVA was adopted if the measurement data between multiple groups conformed to a normal distribution. If it did not conform to a normal distribution, the Kruskal‒Wallis H test was adopted. The chi-squared test was used to compare the rates of multiple groups. Relationships between the constipation scale and rectal sensory function (FCSV, DDV and MTV) were assessed by Spearman’s correlation coefficient. The difference was statistically significant at P < 0.05.
Results
Population
A total of 39 patients with functional constipation were included in the study and analysis of the impact of different positions and distension mediums on rectal sensory test. Among them, the proportion of female patients is higher than that of males, with 69.23% being female and 30.77% being male; The average age was 53.85 ± 14.19 years old, and the overall research subjects were mainly middle-aged and elderly; The average BMI was 22.70 ± 3.00 kg/m [2], which is generally in line with the normal body mass index; The rectal resting pressure, anal resting pressure, functional anal canal length, and maximum anal squeeze pressure in the left lateral position were all within the normal range evaluated by our unit. The constipation scale for enrolled patients, including the Constipation Scoring System (CSS), the Patient Assessment of Constipation Symptoms (PAC-SYM), and the Patient assessment of constipation quality of life questionnaire (PAC-QoL) are shown in Table 1.
Relationships between constipation scale and rectal sensory function
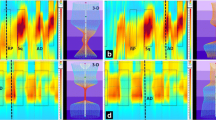
There was no correlation between BMI, age and rectal sensory function. Among the items of the CSS, the score of frequency of bowel movements showed a negative correlation with FCSV (r = -0.323, P = 0.045). In contrast, the score of painful evacuation effort showed a positive correlation with DDV (r = 0.343, P = 0.033) (see Fig. 2).
Relationships between the constipation scale and rectal sensory function. Abbreviations: * indicates p < 0.05, FCSV: first constant sensation volume, DDV: desire to defecate volume, MTV: maximum tolerated volume. FCSV, DDV and MTV were tested in the left lateral position using gas as the distension medium
Influence of distension medium on rectal sensory test
FCSV, DDV and MTV were evaluated by different distension media (water, gas) in the left lateral position and sitting position, and it was found that the differences were not statistically significant. The only significant difference was DDV between water or gas was in squatting (P = 0.017), indicating that in the squatting state, the sensitivity of the water evaluation is higher than that of the gas evaluation (see Table 2).
Influence of examination position on rectal sensory test
When gas was used as the distension medium, the difference in the FCSV between different body positions (left lateral, sitting, squatting) was statistically significant (P = 0.007). Further multiple comparisons were used, and significance values were adjusted using the Bonferroni correction method. There was a significant difference between the left lateral and squatting positions (P = 0.008). There was no statistically significant difference between the DDV and the MTV in different body positions in this condition. When water was used as the measuring medium for distension, there was no statistically significant difference in the FCS, DDV and MTV between different body positions (see Table 3).
Discussion
The exact cause of RH is not yet clear, but there is evidence to suggest that constipation, long-term inhibition of defecation, pelvic nerve injury, spinal trauma, perianal surgery, etc. may be related factors [25]. With the deepening of research on functional constipation, the importance of RH has been gradually recognized in functional constipation. In the research on the correlation between functional constipation and RH, a cross-sectional study (including 218 cases) found that 56% of functional constipation cases were accompanied by RH [9]. The rectal sensory function is performed in a left lateral position instead of a seated position, however the latter is the physiological position for defecation [21]. At the same time, the sensation of defecation is related to the size and weight of the feces [26, 27]. Therefore, this study designed to use different positions and distension mediums for rectal sensation measurement, to evaluate whether there are differences and whether the results can be mutually substituted in clinical practice.
At present, the main method for measuring rectal sensory function is volume measurement using rectal dilation, which is widely used in clinical practice [10, 19]. Balloon distension is currently the most commonly used evaluation method for rectal sensory function, which uses a handheld syringe to slowly inject gas/water to expand the balloon and reflects the sensitivity of the rectum based on the volume of injection [18]. Simple balloon distension appears satisfactory for the initial assessment of rectal sensory function and will identify patients with elevated sensory threshold volumes [28].
On the basis of simple balloon distension, barostat distension was invented [19]. A barostat is an electromechanical device that uses a computer-controlled pressure regulator and a highly flexible polyethylene bag to provide equal pressure rectal dilation for more accurate measurement [28,29,30]. Barostat can provide information on the biomechanical properties of the intestinal wall, but it has not yet been widely used in clinical practice due to the long operation time (60–90 min) and high cost [31]. In addition to the volumetry-based methods, there are currently relevant studies using a bipolar ring electrode supplying a constant current to test the electrical sensitivity of rectal mucosa. Researchers believe that electrical testing avoides the variables inherent in balloon distension and is well tolerated, accurately quantifiable, and reproducible [32]. The heat stimulation method has also been explored as a method for evaluating rectal sensation. The median rectal heat threshold was found to be similar in males (median, 47 degrees C; range, 44–50 degrees C) compared with females (median, 45 degrees C; range, 43–50 degrees C; P > 0.05) and there was a high degree of repeatability with rectal heat and balloon distension thresholds (MTV, r = 0.8; P < 0.001, measured with balloon distension) [33]. Although the rectum is sensitive to electrical and thermal stimulation, mechanical distention is the most reliable and physiologic stimulus for the assessment of sensation [19]. Electrical stimulation and heat stimulation are considered to bypass the end organ receptor, which can bypass the mucosal receptor and directly depolarize the free nerve ending, directly stimulate the surrounding neuronal axons, and cannot reflect the situation of rectal mucosal receptor [12]. At the same time, electrical stimulation and heat stimulation cannot simulate normal bowel stimulation. There is currently no consensus on whether the nonmechanical distension method represented by electrical stimulation and heat stimulation can replace volumetry. Therefore, it is currently limited to research and has not been clinically applied [19].
There are currently studies measuring the differences between the left lateral position, the squatting position, sitting position, and lithotomy position, but the results are heterogeneous (see Table 4). The method of using gas as a distension medium is widely used in clinical practice [10]. However, although there are relevant studies on whether there are differences between the distension medium of gases and other media, the conclusions are inconsistent (see Table 4). During rectal sensitivity testing using gas and water as distension media in 12 normal males, it was found that there was no difference between gas and water [17]. For patients with prolapsed hemorrhoids, the FCSV of gas is significantly lower than that of water in the left lateral position and the MTV of gas is significantly higher than that of water in the sitting position [34].
Based on the above literature research results, it was found that there is heterogeneity in the research results of rectal sensory testing between different body positions and different distension medium, which may be due to the different research subjects and specific operating parameters used. Therefore, this study fixed the relevant operating parameters for rectal sensory testing for patients with functional constipation. In this study, it was found that there was a statistically significant difference in the FCSV (distension medium: gas) among different body positions (left lateral position, sitting position, squatting position), and the data measured in the squatting position were significantly higher than those in the left lateral position (P < 0.05). The difference may be due to relaxation of the puborectal and pelvic floor muscles during squatting, opening of the right angle of the anus, straightening of the angle of the rectum and anal canal, and anatomical changes affecting the patient’s perception of stimuli [11, 38, 39]. At the same time, the patient’s attention and sensory abilities may be distracted by maintaining the body balance and feeling uncomfortable in the legs when using a squatting position, causing an increase in the sensory threshold value. A thorough evaluation of the patient’s anorectal function is important, especially in terms of patient referrals to different treatment centers and pre- and post-treatment assessments. We found that the data measured in the sitting position were more stable when either gas or water was the medium, and were not significantly different from the other positions. Water was also more stable than gas. At the same time, considering that the current defecation habits of people are mainly in the sitting position and that feces have a certain weight, it is recommended to use the sitting position and water as the medium for the measurements, taking into account the data of this study.
To explore the relationship between symptom scales and rectal sensory thresholds, we correlated all 8 items of CCS with sensory thresholds and found that FCSV were negatively correlated with the score of frequency of bowel movements (r = -0.323, P = 0.045) and incomplete evacuation (r = -0.170, P = 0.300). This suggests that there may be a relative increase in rectal sensitivity in this group of patients with fewer bowel movements. On further analysis of the relationship between CCS total score and rectal sensitivity, no significant correlation was found. We analysed that the each item in the CCS scale do not represent the overall change in constipation symptoms. However, due to our small sample size in this case, there may be a bias in the data. Therefore, further expansion of the sample size is needed in future studies.
Anorectal manometry has been widely utilized in clinical treatment and assessment. Several studies have indicated significant variations in anorectal manometry results based on different positions. This study aims to compare and analyze the impact of different examination positions and dilatation media on rectal sensory detection in patients with functional constipation, in order to recommend more suitable examination positions and testing media for clinical use. The goal is to fully capture anorectal changes under physiological conditions, provide more precise data for clinical practice, and offer data support for future studies with larger samples. The sample size of this study was small, so the data may be statistically biased. Patients were not given comprehensive constipation-related tests, including colonic transit time and whole colon manometry. Patients were also not stratified and analysed according to severity or subtype of constipation. Therefore, there is a need for subsequent studies to include larger sample sizes and more detailed and comprehensive assessments to conduct in-depth research.
Conclusion
Based on the results of this study, there are differences in the results of sensory testing between body positions and distension mediums. It is necessary to use the commonly used defecation posture of patients for rectal sensation testing rather than collecting data from the left lateral position alone. Taking into account the data from this study, it is recommended to use the sitting position and water as the medium for the measurements. However, due to the small sample size of this study, there may be bias in the data. When formulating standard values, each center needs to pay attention to the setting of details such as the body position and the distension medium. When conducting multicenter studies, it is necessary to unify the standard operating procedure (SOP) settings for operational details to ensure the consistency of the study.
Data availability
Data can be made available from the Corresponding Author on reasonable request.
Abbreviations
- SOP:
-
Standard operating procedure
- RH:
-
Rectal hyposensitivity
- BMI:
-
Body Mass Index
- CSS:
-
Constipation Scoring System
- DDV:
-
Desire to defecate volume
- FCSV:
-
First constant sensation volume
- IAPWG:
-
International Anorectal Physiology Working Group
- MTV:
-
Maximum tolerated volume
- PAC-QoL:
-
Patient assessment of constipation quality of life questionnaire
- PAC-SYM:
-
Patient Assessment of Constipation Symptoms
References
Bharucha AE, Wald A. Chronic constipation. Mayo Clin Proc. 2019;94(11):2340–57.
Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018;209(2):86–91.
Ghoshal UC, Sachdeva S, Pratap N, Verma A, K Ar Yampudi A, Misra A, Abraham P, Bhatia SJ, Bhat N, Chandra A. Indian consensus on chronic constipation in adults: a joint position statement of the Indian Motility and Functional Diseases Association and the Indian Society of Gastroenterology. Indian J Gastroenterol 2018.
Hanifah O. Fatima; Safira; Alatas; Badriul; Hegar; William; Cheng; Arnesya, Epidemiology of Paediatric constipation in Indonesia and its association with exposure to stressful life events. BMC Gastroenterol 2018.
Mill M, Koppen I, Benninga MA. Controversies in the management of functional constipation in children. Curr Gastroenterol Rep. 2020;21(6):23–.
Stern T, Davis AM. Evaluation and treatment of patients with constipation. JAMA. 2016;315(2):192–3.
Gladman MA, Scott SM, Chan CL, Williams NS, Lunniss PJ. Rectal hyposensitivity: prevalence and clinical impact in patients with intractable constipation and fecal incontinence. Dis Colon Rectum. 2003;46(2):238–46.
Goligher JC, Hughes E. Sensibility of the rectum and colon. Its rle in the mechanism of anal continence. Lancet. 1951;257(6654):543–8.
Ting Y. Dong; Qian; Yongping; Zheng; Ya; Jiang; Ping; Wu, Rectal Hyposensitivity Is Associated With a Defecatory Disorder But Not Delayed Colon Transit Time in a Functional Constipation Population. Medicine 2016.
Gladman MA, Scott SM, Williams NS, Lunniss PJ. Clinical and physiological findings, and possible aetiological factors of rectal hyposensitivity. Br J Surg. 2003;90(7):860–6.
Palit S, Lunniss PJ, Scott SM. The physiology of human defecation. Dig Dis Sci. 2012;57(6):1445–64.
Burgell RE, Scott SM. Rectal hyposensitivity. J Neurogastroenterology Motil. 2012;18(4):373–84.
Gladman M, Aziz Q, Scott S, Williams N, Lunniss P. Rectal hyposensitivity: pathophysiological mechanisms. Neurogastroenterology Motility: Official J Eur Gastrointest Motil Soc. 2009;21(5):508–16. e4-5.
Carrington EV, Heinrich H, Knowles CH, Fox M, Rao S, Altomare DF, Bharucha AE, Burgell R, Chey WD, Chiarioni G, Dinning P, Emmanuel A, Farouk R, Felt-Bersma RJF, Jung KW, Lembo A, Malcolm A, Mittal RK, Mion F, Myung SJ, O’Connell PR, Pehl C, Remes-Troche JM, Reveille RM, Vaizey CJ, Vitton V, Whitehead WE, Wong RK, Scott SM. The international anorectal physiology working group (IAPWG) recommendations: standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020, 32 (1), e13679.
Ahn JY, Myung SJ, Jung KW, Yang DH, Koo HS, Seo SY, Yoon IJ, Kim KJ, Ye BD, Byeon JS, Jung HY, Yang SK, Kim JH. Effect of biofeedback therapy in constipation according to rectal sensation. Gut Liver. 2013;7(2):157–62.
Felt-Bersma RJ, Gort G, Meuwissen SG. Normal values in anal manometry and rectal sensation: a problem of range. Hepatogastroenterology. 1991;38(5):444–9.
Sun WM, Read NW, Prior A, Daly JA, Cheah SK, Grundy D. Sensory and motor responses to rectal distention vary according to rate and pattern of balloon inflation. Gastroenterology. 1990;99(4):1008–15.
Barnett JL, Hasler WL, Camilleri M. American Gastroenterological Association medical position statement on anorectal testing techniques. American Gastroenterological Association. Gastroenterology. 1999;116(3):732–60.
Scott SM, Gladman MA. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterol Clin North Am 2008, 37 (3), 511 – 38, vii.
Su H, Peng L, Sun G, Yang Y, Wu J, Jiang G, Ge H. Effect of different body position on anorectal manometry for chronic constipation patients. Eur Rev Med Pharmacol Sci. 2019;23(19):8493–500.
Wu GJ, Xu F, Lin L, Pasricha PJ, Chen JDZ. Anorectal manometry: should it be performed in a seated position? Neurogastroenterol Motil 2017, 29 (5).
CX Z, HY J, XR Y, J W, JL L, Y Y, Y Z. Effect of semi-recumbent lithotomy and left lateral position on anorectal manometry. J Colorectal anal Surg. 2020;26(4):464–8.
de Loubens C, Dubreuil A, Lentle RG, Magnin A, Kissi NE, Faucheron JL. Rheology of human faeces and pathophysiology of defaecation. Tech Coloproctol. 2020;24(4):323–9.
Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R, Disorders B. Gastroenterology 2016.
Gladman M, Lunniss A, Peter J, Scott S. M.; Swash, Rectal Hyposensitivity. Am J Gastroenterol 2006.
Gregersen H. Novel Bionics Assessment of Anorectal Mechanosensory Physiology. Bioeng (Basel) 2020, 7 (4).
Bannister JJ, Davison P, Timms JM, Gibbons C, Read NW. Effect of stool size and consistency on defecation. Gut. 1987;28(10):1246–50.
Gladman MA, Dvorkin LS, Lunniss PJ, Williams NS, Scott SM. Rectal hyposensitivity: a disorder of the rectal wall or the afferent pathway? An assessment using the barostat. Am J Gastroenterol. 2005;100(1):106–14.
Whitehead WE, Delvaux M. Standardization of barostat procedures for testing smooth muscle tone and sensory thresholds in the gastrointestinal tract. The Working Team of Glaxo-Wellcome Research, UK. Dig Dis Sci. 1997;42(2):223–41.
Rey E, Alvarez Sánchez A, Díaz-Rubio M. Which is the best distension protocol to study rectal sensitivity in the irritable bowel syndrome? Rev Esp Enferm Dig. 2002;94(4):211–20.
L Z, Y D, Lin L. The importance of rectal sensitivity in functional bowel dysfunction (in Chinese). Chin J Gastroenterol. 2019;24(7):440–3.
Kamm MA, Lennard-Jones JE. Rectal mucosal electrosensory testing–evidence for a rectal sensory neuropathy in idiopathic constipation. Dis Colon Rectum. 1990;33(5):419–23.
Chan CL, Scott SM, Birch MJ, Knowles CH, Williams NS, Lunniss PJ. Rectal heat thresholds: a novel test of the sensory afferent pathway. Dis Colon Rectum. 2003;46(5):590–5.
C W, Q Z. The effect of body position and rectal contents on anorectal pressure in patients with prolapsed hemorrhoids. J Fudan Univ (Natural Science). 2013;52(05):669–73.
Kadam-Halani PK, Pahwa AK, Koelper NC, Arya LA, Sammel MD, Andy UU. Comparison of Anorectal Manometry Testing in Left lateral and lithotomy positions. Female Pelvic Med Reconstr Surg. 2020;26(10):630–4.
YH L. Observation of different examination positions for anorectal manometry in patients with functional constipation (in Chinese). China Health Care Nutr. 2017;27(3):67.
LH W, MJ L, FP C, YY Z, JY W. Effect of different postures on high Resolution Anorectal Manometry in patients with functional constipation (in Chinese). J Nurs (China). 2015;22(17):51–3.
Sakakibara R, Tsunoyama K, Hosoi H, Takahashi O, Sugiyama M, Kishi M, Ogawa E, Terada H, Uchiyama T, Yamanishi T. Influence of body position on defecation in humans. Low Urin Tract Symptoms. 2010;2(1):16–21.
Takano S, Sands DR. Influence of body posture on defecation: a prospective study of the thinker position. Tech Coloproctol. 2016;20(2):117–21.
Acknowledgements
None.
Funding
The Yangfan Project of Shanghai Science and Technology Commission (23YF1448000); National Natural Science Foundation of China (Nos. 82305235 and 82174373); Shenkang Promotion of Clinical Specialty Ability Improvement Project (SHDC22021316-A); Program for Xinglin Scholar at Shanghai University of Traditional Chinese Medicine (RC-2017-02-08); Shanghai Hospital Development Center Foundation (SHDC12024135); Shanghai key Clinical Specialty (shslczdzk04301); Development highland construction of TCM- the inheritance and extension plan of traditional Chinese Medicine School in Shanghai [ZY(2021-2023-0209)]; Shanghai Sinus Fistula Disease Research Center (2023ZZ02003); National Administration of Traditional Chinese Medicine High level Key Discipline of Traditional Chinese Medicine - Traditional Chinese Medicine Anorectal Diseases.
Author information
Authors and Affiliations
Contributions
Y.Y., C.W. and Y.C. conceived the experiments. Y.Y., C.X. and Y.L. wrote the manuscript. C.X., Y.S., L.M., J.W. and M.W. performed the experiment. C.X. and Y.L. performed data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of Longhua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine approved the study. Informed consent was obtained from the participants before the study and participation was voluntary.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xiao, CF., Li, YF., Sun, YY. et al. Influence of the examination position and distension medium on the rectal sensory test in patients with functional constipation. BMC Gastroenterol 24, 238 (2024). https://doi.org/10.1186/s12876-024-03309-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03309-5