Abstract
Background
Despite transarterial chemoembolization (TACE) was recommended as first line therapy for intermediate hepatocellular carcinoma (HCC), the efficacy of transarterial embolization (TAE) has not been widely recognized. This work was to determine whether TAE was as effective and safe as TACE for unresectable HCC.
Methods
We performed a systematic search of electronic databases and other sources for randomized controlled studies (RCTs) comparing TAE with TACE for unresectable HCC. Results were expressed as Hazard Ratio (HR) for survival and Odds Ratio (OR) for dichotomous outcomes using RevMan 5.4.1.
Results
We included 6 trials with 683 patients. The risk of bias of included RCTs was from unclear to high risk. There were no significant differences between TACE and TAE for progression-free survival (HR 0.83, 95% CI 0.45–1.55; p = 0.57), overall survival (HR 1.10, 95% CI 0.90–1.35; p = 0.36), and objective response rate (OR 1.17, 95% CI 0.80–1.71; p = 0.42) without obvious publication bias. Sensitivity analyses confirmed the robustness of the results. TAE group reported similar or less adverse effects than TACE group in all the studies.
Conclusions
Our study demonstrated that TAE was as effective as TACE. Since TAE was simpler, cheaper and had less adverse effects than TACE, TAE should be a better choice in most cases where TACE was indicated for unresectable HCC.
Similar content being viewed by others
Background
Primary liver cancer is the sixth most commonly diagnosed cancer and the third leading cause of cancer death world-wide in 2020, with hepatocellular carcinoma (HCC) accounts for 75-85% [1]. Resection, ablation and transplantation are widely accepted as radical treatment, but only appropriate for minority patients with relatively early staged tumors [2]. For patients with tumors of intermediate and advanced stage, transarterial chemoembolization (TACE) [3, 4] and systemic therapies [5, 6] are first line choices respectively.
The first case of transarterial chemotherapy was happened by accidental administration of HN2 in to the branchial artery of a patient with Hodgkin’s disease. Since then, transarterial infusion chemotherapy has been applied for localized tumors [7, 8]. Ecker and his associates introduced Hepatic arterial infusion chemotherapy (HAIC) by insertion of catheter through gastroduodenal artery in open surgery in 1962. The patients were tolerated well without severe systemic symptoms [9]. In 1981, Patt and colleagues found prolonged survival associated with inadvertent occlusion of hepatic artery [10, 11]. In 1983, Yamada and associates reported transarterial embolization (TAE) in 120 cases of patients with unresectable hepatoma [12], and Konno combined HAIC and TAE with ethiodol together, named TACE for hepatoma [13]. Since then, both TAE and TACE were widely applied with different embolization agents and chemical drugs, but their effects were controversial [14,15,16,17,18,19] until two randomized controlled trials (RCT) with high quality in 2002 [3, 4] and one systematic review in 2003 approved the benefits of TACE [20]. After that, TACE became the first line therapy for patients with intermediate stage of hepatoma [2]. Since no RCT with high quality compared TAE with best supportive care, TAE was not as widely recommended by guidelines as TACE [21] and only applied for a minority of appropriate patients in real world. In fact, TAE achieved similar, if not superior, results for patients with unresectable HCC compared with TACE in several RCTs [4, 22,23,24,25,26]. In this systematic review, we will summarize the results of all RCTs comparing TAE vs. TACE for patients with unresectable HCC.
Methods
Criteria for considering studies for this review
Inclusion criteria: (i) Study design: only randomized controlled trials (RCT) were considered; (ii) Study population: >18 years old, without gender restrictions, diagnosed with unresectable HCC regardless of etiology; (iii) Therapy for HCC: transarterial chemoembolization compared with embolization alone regardless of types of embolization agents and chemical drugs; (iv) Results available on progression-free survival (PFS) or overall survival (OS). Exclusion criteria: Primary HCC was treated with radical therapy (resection, ablation or transplantation), systemic therapy (chemotherapy, targeted therapy or immune therapy) or other local reginal therapy (internal or external radiotherapy).
Search methods for identification of studies
We performed a systematic search of electronic databases (PubMed, EMBASE, Science Citation Index Expanded and Cochrane Library databases) for studies without language restriction (last literature search date: April 30, 2024). The search strategy was based on MeSH terms combined with free text words. The search strategies were given in Supplementary Table S1 and similar to our published work [27]. Reference lists of associated papers (included studies and relevant reviews) were checked as hand searching.
Data collection and assessment of bias
Studies was screened according to the inclusion and exclusion criteria and data was extracted through a predesigned data extraction form by two authors independently. For duplicated publications, all the data was included but duplicated data was discarded if technically feasible but they were considered as one study. All included studies were assessed for methodological quality by two authors independently, as recommended by the Cochrane Hand book for RCTS [28]. Any disagreement between the two authors was resolved through discussion. OS was primary outcome. PFS, objective response rate (ORR) and adverse effects were secondary outcomes. We would contact and request the researchers to provide key missed information.
Statistical analysis
We performed this systematic review according to the Cochrane Handbook [28] and reported in line with the Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement [29]. Hazard ratio (HR) between two arms was applied as a summary statistic for time-to-event outcomes like PFS and OS whereas Odds ratio (OR) was applied for dichotomous outcomes. HR and its standard error of each trial was calculated by a method described by Tierney and colleagues [30].
HR/OR of individual trials were pooled into an overall HR/OR by random-effects model. In accordance with customary, an overall HR/OR < 1 favored the TACE group and the difference was considered statistically significant if the 95% CI of the HR/OR didn’t overlap 1. Funnel plots would be used to evaluate the publication bias if there were sufficient studies. Sensitivity analyses were used to evaluate the reliability of the results.
Two authors input the data into RevMan 5.4.1 (Cochrane Collaboration, Oxford, UK), and performed all the analysis independently.
Results
Description of studies
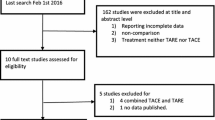
The study screening process is shown in Fig. 1. Six RCTs were included for this systematic review (Table 1) [4, 22,23,24,25,26]. Thirty six studies were excluded because they did not meet the inclusion criteria (Supplementary Table S2), including one just analyzed the data of patients who subsequently underwent liver resection (31/99, 31.3%) in each group after randomization [14], and another was not a randomized trial [31]. Three studies applied lipiodol or gelatin sponge [4, 22, 23] for embolization whereas others applied different kinds of microspheres [24,25,26]. Four RCTs used doxorubicin as chemical drugs for TACE [4, 22, 24, 26] and two studies used cisplatin [23, 25]. A total of 683 patients were included in this systematic review, among which 345 were in TACE-group whereas 338 in TAE-group. Child-Pugh Score was mainly A to B, and ECOG-PS (Eastern Cooperative Oncology Group-performance status) Score was mainly 0 to 1. But patients with tumors of BCLC (Barcelona Clinic Liver Cancer) stage A/B/C and etiology of HBV/HCV/alcohol were all included. The mean embolization number was from 1.37 to 3.1 for one patient (Table 1). The risk of bias of included RCT was from unclear to high risk (Fig. 2).
Effects of intervention
Pooling the data of six studies [4, 22,23,24,25,26] that assessed OS in 683 patients showed no significant difference between TACE and TAE (HR 1.10, 95% CI 0.90–1.35; p = 0.36), without significant between-study heterogeneity [X2 = 2.31, degrees of freedom (df) = 5; p = 0.80; I2 = 0%] (Fig. 3A). All the six studies reported ORR and pooled data showed no significant difference between TACE and TAE (OR 1.17, 95% CI 0.80–1.71; p = 0.42), without significant between-study heterogeneity [X2 = 6.50, df = 5; p = 0.26; I2 = 23%] (Fig. 3C). No significant publication bias was found by funnel plots (Fig. 4) for both OS and ORR. Only three studies reported PFS and pooled data showed no significant difference between two groups (HR 0.83, 95% CI 0.45–1.55; p = 0.57), with significant between-study heterogeneity [X2 = 9.04, df = 2; p = 0.01; I2 = 78%] (Fig. 3B). Funnel plot was not shown due to insufficient studies.
Sensitivity analysis
Sensitivity analyses of studies excluding studies with high risk of bias, or studies applied lipiodol or gelatin sponge as embolization materials, or studies applied microsphere as embolization materials (all of them were published after 2010), or studies applied doxorubicin as chemical drugs, still showed no significant difference between the TACE and TAE group (Table 2).
Adverse effects
Meta-analysis comparing adverse effects could not be achieved due to lack of consistency in reporting. Kawai 1992 reported significant lower hemoglobin level in TACE group than TAE group whereas all the other blood cells and liver function, as well as abdominal pain and fever were similar in two groups [22]. Chang 1994 reported higher incidence of emesis in TACE group (75.4% vs. 9.6%) due to cisplatin whereas all the others like liver function and renal function were similar [23]. In Llovet 2002, one patient died due to septic shock in TACE group and TACE group also had higher number of treatment-related complications (11 vs. 7) [4]. Both postembolization syndrome and other complications were similar in Malagari 2010 and Brown 2016 [24, 26]. Meyer 2013 reported higher grade 3/4 adverse events in TACE group (83.7% vs. 60.5%) but similar quality of life between the two groups [25]. In summary, TAE group reported similar or less adverse effects than TACE group in all the studies. The detailed adverse events were shown in Supplementary Table S3.
Discussion
In this systematic review, six RCTs fulfilled our criteria. The risk of bias of included RCTs was from unclear to high risk. All the studies applied more than 1 procedure for each patient if possible or needed. The results showed that TAE was as effective as TACE for both PFS and OS, as well as ORR. Sensitivity analysis showed similar results in two groups regardless of embolization agents or chemical drugs or excluded studies with high risk of bias. But TAE group reported similar or less adverse effects than TACE group. Three of the six studies used lipiodol or gelatin sponge, alone or together as embolization agents [4, 22, 23], but for other three studies, one applied polyvinyl alcohol (PVA) microsphere [25] and the other two studies applied drug-eluting beads [24, 26]. Four studies applied doxorubicin whereas two studies employed cisplatin [23, 25]. Our results were similar to three published systematic reviews, which pooled published data and found no significant difference in mortality between the two groups [25, 32, 33]. But two [25, 32] of them did not apply HR as a summary statistic for time-to-event outcome like OS. And one most recent review [33] did not include one important RCT published in the Lancet [4], which we think totally fulfilled the inclusion criteria. We did not find any other published systematic review and meta-analysis focusing on this issue.
Since hepatic arterial infusion chemotherapy (HAIC) was introduced into clinic much earlier than TAE [9, 12], and its effects were also been fully improved and widely accepted [11, 34]. Undoubtedly, no one doubts the value of retaining chemotherapy during TAE. However, only continuous infusion of chemotherapy with small dose had obvious anti-cancer effects, which has been proved by two recent RCTs [35, 36]. In their studies, HAIC with FOLFOX (Oxaliplatin, Calcium folinate and 5-Fluorouracil) regimen even improved overall survival than TACE or sorafenib for patients with unresectable HCC. During the procedure of TACE, chemical drugs were injected into hepatic artery transiently. Though it’s widely believed that after the emulsion of anti-cancer drugs with lipiodol, the drugs can deposit into tumor tissue with lipiodol for a long time. No one can tell how many and how long the drugs deposited in situ. Not to mention the heterogeneity of tumors, the individual differences and technical inconsistency [37, 38]. According to our study and others TACE was not superior to TAE and HAIC, we speculated that either due to doxorubicin/cisplatin was not as effective as FOLFOX for HCC, or only a few drugs deposited into the tumor tissue. Another concern is about the extent of embolization. Traditional embolization aims to embolize as much tumor tissue as possible, which will leads to damage to liver function, even after introduction of super-selective embolization. This kind of strategy will limit the upper-amount numbers of procedure as well as the probability of successful conversion as hepatectomy requires adequate liver reserve. In order to overcome this dilemma, the combination of embolization of collateral feeding arteries with HAIC of main feeding artery should be a good strategy (TAE + HAIC) [39].
Some limitations of this study should be discussed. First of all, all included RCTs had unclear or high risk of bias. But the results were stable in between studies and according to sensitivity analysis. Second, significant between-study heterogeneity existed because of the different patients (etiology, characteristics of tumors, et al.), types of embolization agents and anti-cancer drugs as well as their doses, number of procedures for each patient as well as interval between each procedure. Though we applied random-effects model where appropriate and sensitivity analysis, but their credibility was decreased by relatively small number of included studies. Third, the definitions of outcomes were not the same in between studies since the earliest included study being published in 1992 and the latest published in 2016 (Supplementary Table S4). Fourth, only six RCTs fulfilled our including criteria. The sample size was not big enough. Fifth, PFS was not available for half of studies and pooling the data of adverse effects was not achieved despite the efforts made to contact the authors. Sixth, though we are confident the un-inferiority of TAE compared to TACE for unresectable HCC, but the exact reason is still not clear.
Conclusions
Despite these limitations listed above, our study still demonstrated that the anti-cancer effects of TAE were at least as well as, if not superior than TACE. Since TAE was simpler, cheaper and had less adverse effects than TACE, TAE should be a better choice in most cases where TACE was indicated for unresectable HCC. Recent studies demonstrated the advantage of HAIC than TACE, further studies should be focused on the combination of TAE and HAIC even systematic therapy in order to offset their respective disadvantages and achieve the best effect [40, 41].
Data availability
Data sharing is not applicable to this article as no new data were created or analyzed.
Data availability
All data used within this study have been publicly available. The corresponding author will consider sharing the dataset gathered upon request.
Abbreviations
- TACE:
-
transarterial chemoembolization
- HCC:
-
hepatocellular carcinoma
- TAE:
-
transarterial embolization
- RCTs:
-
randomized controlled studies
- HR:
-
Hazard Ratio
- OR:
-
Odds Ratio
- HAIC:
-
Hepatic arterial infusion chemotherapy
- PFS:
-
progression-free survival
- OS:
-
overall survival
- ORR:
-
objective response rate
- ECOG-PS:
-
Eastern Cooperative Oncology Group-performance status
- BCLC:
-
Barcelona Clinic Liver Cancer
- FOLFOX:
-
Oxaliplatin, Calcium folinate and 5-Fluorouracil
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380(15):1450–62.
Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, Fan ST, Wong J. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology (Baltimore MD). 2002;35(5):1164–71.
Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Sola R, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359(9319):1734–9.
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020;382(20):1894–905.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Klopp CT, Alford TC, Bateman J, Berry GN, Winship T. Fractionated intra-arterial cancer; chemotherapy with methyl bis amine hydrochloride; a preliminary report. Ann Surg. 1950;132(4):811–32.
Sullivan RD, Miller E, Sikes MP. Antimetabolite-metabolite combination cancer chemotherapy. Effects of intraarterial methotrexate-intramuscular Citrovorum factor therapy in human cancer. Cancer. 1959;12:1248–62.
Ecker RR, Cornell GN, Conn J, Cahow CE, Beal JM. Cancer chemotherapy for hepatic metastases by continuous hepatic artery influsion. Cancer Chemother Rep. 1962;16:531–6.
Patt YZ, Wallace S, Hersh EM, Hall SW, Menachem YB, Granmayeh M, McBride CM, Benjamin RS, Mavligit GM. Hepatic arterial infusion of Corynebacterium parvum and chemotherapy. Surg Gynecol Obstet. 1978;147(6):897–902.
Patt Y, Chuang V, Wallace S, Hersh E, Freireich E, Mavligit G. The palliative role of hepatic arterial infusion and arterial occlusion in colorectal carcinoma metastatic to the liver. Lancet (London England). 1981;1(8216):349–50.
Yamada R, Sato M, Kawabata M, Nakatsuka H, Nakamura K, Takashima S. Hepatic artery embolization in 120 patients with unresectable hepatoma. Radiology. 1983;148(2):397–401.
Konno T, Maeda H, Iwai K, Tashiro S, Maki S, Morinaga T, Mochinaga M, Hiraoka T, Yokoyama I. Effect of arterial administration of high-molecular-weight anticancer agent SMANCS with lipid lymphographic agent on hepatoma: a preliminary report. Eur J Cancer Clin Oncol. 1983;19(8):1053–65.
Takayasu K, Shima Y, Muramatsu Y, Moriyama N, Yamada T, Makuuchi M, Hasegawa H, Hirohashi S. Hepatocellular carcinoma: treatment with intraarterial iodized oil with and without chemotherapeutic agents. Radiology. 1987;163(2):345–51.
Kasugai H, Kojima J, Tatsuta M, Okuda S, Sasaki Y, Imaoka S, Fujita M, Ishiguro S. Treatment of hepatocellular carcinoma by transcatheter arterial embolization combined with intraarterial infusion of a mixture of cisplatin and ethiodized oil. Gastroenterology. 1989;97(4):965–71.
Venook AP, Stagg RJ, Lewis BJ, Chase JL, Ring EJ, Maroney TP, Hohn DC. Chemoembolization for hepatocellular carcinoma. J Clin Oncology: Official J Am Soc Clin Oncol. 1990;8(6):1108–14.
Vetter D, Wenger JJ, Bergier JM, Doffoel M, Bockel R. Transcatheter oily chemoembolization in the management of advanced hepatocellular carcinoma in cirrhosis: results of a western comparative study in 60 patients. Hepatology (Baltimore MD). 1991;13(3):427–33.
Groupe d’Etude et de Traitement du Carcinome H. A comparison of lipiodol chemoembolization and conservative treatment for unresectable hepatocellular carcinoma. N Engl J Med. 1995;332(19):1256–61.
Pelletier G, Ducreux M, Gay F, Luboinski M, Hagege H, Dao T, Van Steenbergen W, Buffet C, Rougier P, Adler M, et al. Treatment of unresectable hepatocellular carcinoma with lipiodol chemoembolization: a multicenter randomized trial. Groupe CHC. J Hepatol. 1998;29(1):129–34.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology (Baltimore MD). 2003;37(2):429–42.
Benson AB, D’Angelica MI, Abbott DE, Anaya DA, Anders R, Are C, Bachini M, Borad M, Brown D, Burgoyne A, et al. Hepatobiliary cancers, Version 2.2021, NCCN Clinical Practice guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(5):541–65.
Kawai S, Okamura J, Ogawa M, Ohashi Y, Tani M, Inoue J, Kawarada Y, Kusano M, Kubo Y, Kuroda C, et al. Prospective and randomized clinical trial for the treatment of hepatocellular carcinoma–a comparison of lipiodol-transcatheter arterial embolization with and without adriamycin (first cooperative study). The Cooperative Study Group for Liver Cancer Treatment of Japan. Cancer Chemother Pharmacol. 1992;31:S1–6.
Chang JM, Tzeng WS, Pan HB, Yang CF, Lai KH. Transcatheter arterial embolization with or without cisplatin treatment of hepatocellular carcinoma. A randomized controlled study. Cancer. 1994;74(9):2449–53.
Malagari K, Pomoni M, Kelekis A, Pomoni A, Dourakis S, Spyridopoulos T, Moschouris H, Emmanouil E, Rizos S, Kelekis D. Prospective randomized comparison of chemoembolization with doxorubicin-eluting beads and bland embolization with BeadBlock for hepatocellular carcinoma. Cardiovasc Interv Radiol. 2010;33(3):541–51.
Meyer T, Kirkwood A, Roughton M, Beare S, Tsochatzis E, Yu D, Davies N, Williams E, Pereira SP, Hochhauser D, et al. A randomised phase II/III trial of 3-weekly cisplatin-based sequential transarterial chemoembolisation vs embolisation alone for hepatocellular carcinoma. Br J Cancer. 2013;108(6):1252–9.
Brown KT, Do RK, Gonen M, Covey AM, Getrajdman GI, Sofocleous CT, Jarnagin WR, D’Angelica MI, Allen PJ, Erinjeri JP, et al. Randomized trial of hepatic artery embolization for Hepatocellular Carcinoma using doxorubicin-eluting microspheres compared with embolization with microspheres alone. J Clin Oncology: Official J Am Soc Clin Oncol. 2016;34(17):2046–53.
Sun P, Yang X, He RQ, Hu QG, Song ZF, Xiong J, Zheng QC. Antiviral therapy after curative treatment of hepatitis B/C virus-related hepatocellular carcinoma: a systematic review of randomized trials. Hepatol Res. 2014;44(3):259–69.
JPT H, MJ JTJCMCTL, P, editors. WV: Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane 2022, www.training.cochrane.org/handbook.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Aoyama K, Tsukishiro T, Okada K, Tsuchida T, Aiba N, Nambu S, Miyabayashi C, Yasuyama T, Higuchi K, Watanabe A. Evaluation of transcatheter arterial embolization with epirubicin-lipiodol emulsion for hepatocellular carcinoma. Cancer Chemother Pharmacol. 1992;31(Suppl):S55–59.
Camma C, Schepis F, Orlando A, Albanese M, Shahied L, Trevisani F, Andreone P, Craxi A, Cottone M. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology. 2002;224(1):47–54.
Lawson A, Kamarajah SK, Parente A, Pufal K, Sundareyan R, Pawlik TM, Ma YT, Shah T, Kharkhanis S, Dasari BVM. Outcomes of Transarterial Embolisation (TAE) vs. Transarterial Chemoembolisation (TACE) for Hepatocellular Carcinoma: a systematic review and Meta-analysis. Cancers 2023, 15(12).
Sullivan RD, Norcross JW, Watkins E Jr. Chemotherapy of metastatic liver Cancer by prolonged hepatic-artery infusion. N Engl J Med. 1964;270:321–7.
Li QJ, He MK, Chen HW, Fang WQ, Zhou YM, Xu L, Wei W, Zhang YJ, Guo Y, Guo RP, et al. Hepatic arterial infusion of Oxaliplatin, Fluorouracil, and Leucovorin Versus Transarterial Chemoembolization for large Hepatocellular Carcinoma: a Randomized Phase III Trial. J Clin Oncology: Official J Am Soc Clin Oncol. 2022;40(2):150–60.
Lyu N, Wang X, Li JB, Lai JF, Chen QF, Li SL, Deng HJ, He M, Mu LW, Zhao M. Arterial chemotherapy of Oxaliplatin Plus Fluorouracil Versus Sorafenib in Advanced Hepatocellular Carcinoma: a biomolecular exploratory, randomized, phase III trial (FOHAIC-1). J Clin Oncology: Official J Am Soc Clin Oncol. 2022;40(5):468–80.
Lucatelli P, Burrel M, Guiu B, de Rubeis G, van Delden O, Helmberger T. CIRSE standards of practice on hepatic Transarterial Chemoembolisation. Cardiovasc Interv Radiol. 2021;44(12):1851–67.
Brown DB, Nikolic B, Covey AM, Nutting CW, Saad WE, Salem R, Sofocleous CT, Sze DY. Society of Interventional Radiology Standards of Practice C: Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vascular Interventional Radiology: JVIR. 2012;23(3):287–94.
Guo W, Gao J, Zhuang W, Wu Z, Li B, Chen S. Efficacy and safety of hepatic arterial infusion chemotherapy combined with transarterial embolization for unresectable hepatocellular carcinoma: a propensity score-matching cohort study. JGH open: Open Access J Gastroenterol Hepatol. 2020;4(3):477–83.
He MK, Liang RB, Zhao Y, Xu YJ, Chen HW, Zhou YM, Lai ZC, Xu L, Wei W, Zhang YJ, et al. Lenvatinib, toripalimab, plus hepatic arterial infusion chemotherapy versus lenvatinib alone for advanced hepatocellular carcinoma. Therapeutic Adv Med Oncol. 2021;13:17588359211002720.
Mei J, Tang YH, Wei W, Shi M, Zheng L, Li SH, Guo RP. Hepatic arterial infusion Chemotherapy Combined with PD-1 inhibitors plus Lenvatinib Versus PD-1 inhibitors plus Lenvatinib for Advanced Hepatocellular Carcinoma. Front Oncol. 2021;11:618206.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82002032 and No. 81700558); Pre-Research Fund for Free Innovation of Union Hospital, Huazhong University of Science and Technology (No. 02.03.2017-44 and No. 02.03.2017-59) and Fund for Independent Innovation of Huazhong University of Science and Technology (No. 2016YXMS247).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data curation, formal analysis and resources were performed by Guoliang Wang and Hao Liu. Ping Sun, Jinxiang Zhang and Qichang Zheng contributed to the study methodology and investigation. The first draft of the manuscript was written by Guoliang Wang. Jinxiang Zhang and Hao Liu commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, G., Zhang, J., Liu, H. et al. Embolization alone is as effective as TACE for unresectable HCC: systematic review and meta-analysis of randomized controlled trails. BMC Gastroenterol 24, 195 (2024). https://doi.org/10.1186/s12876-024-03282-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03282-z