Abstract
Background/objectives
Recent studies show the potential role of dietary quality and quantity in predicting the risk of chronic diseases, such as liver disease, therefore, in the present study, we aimed to assess the association of diet quality index International (DQI-I) and diet quality index revised (DQI-R) and their main components with the odds of non-alcoholic fatty liver disease (NAFLD) in adult populations.
Methods
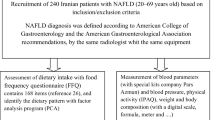
The current case-control study was conducted on 225 patients with NAFLD and 450 controls. Dietary intake was assessed using a validated 168-item food frequency questionnaire, and DQI-I and DQI-R were calculated in participants. Multi-variable logistic regression was used to examine the association of DQI-I and DQI-R and their components with the odds of NAFLD.
Results
The mean (SD) age and BMI of participants (53% men) were 38.1 (8.8) years and 26.8 (4.3) kg/m2, respectively. In the final model, each one SD increment in the DQI-I score was associated with decreased odds of NAFLD (OR = 0.63; 95%CI = 0.40–0.98) (P = 0.040). Also, of DQI-I components, high adequacy score was related to lower odds of NAFLD (OR = 0.16; 95%CI = 0.06–0.40) (P < 0.001). Also, our findings showed that participants in the highest tertile of DQI-R score had lower odds of NAFLD compared to the lowest tertile of DQI-R (OR = 0.24; 95%CI = 0.10–0.53) (P < 0.001). Furthermore, of DQI-R components, high moderation score are linked to a lower risk of NAFLD (OR = 0.17;95%CI = 0.07–0.43) (P < 0.001).
Conclusion
Our findings suggested that greater adherence to diet with a higher score of DQI-I and DQI-R may be associated with lower odds of NAFLD.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) prevalence has been increasing worldwide. A recent study using 245 articles involving 2,699,627 persons forecast that NAFLD prevalence will be 55.7% by 2040, a three-fold increase since 1990 and a 43.2% increase from 2020 [1]. Globally, the NAFLD-related deaths and disability-adjusted life years (DALYs) in 2019 increased by 80.2% and 62.9% compared with 1990, respectively [2]. Besides obesity, genetics, and inactivity, dietary factors are recognized as the main risk factors for NAFLD [3, 4]. Different aspects of diet such as nutrients [5], food items [6], food groups [7, 8], and dietary indices [9, 10] were shown to be associated with NAFLD. One important aspect of a diet is diet quality which is defined in different types and many pre-defined indices developed to measure the quality of a diet.
The diet quality index(DQI) was introduced by Patterson et al. in 1994 based on dietary recommendations from the 1989 National Academy of Sciences publication Diet and Health [11]; they created DQI using the composition of dietary intake of 8 components (total fat, saturated fat, cholesterol, fruit and vegetables, grains and legumes, protein, sodium, and calcium). Five years later, Haines et al. developed a revised version of DQI as DQR-R [12] based on dietary assessment using two completed 24-hour recalls in 3202 adults. DQI-R is composed of 10 components including 4 of the original DQI components (total fat, saturated fat, cholesterol, and calcium), fruit and vegetable as separate components, grains as a single category, iron that was replaced with protein, and dietary moderation and diversity as new components. Also, the reproducibility and validity of the DQI-R which was assessed by the food frequency questionnaire (FFQ) instrument confirmed later [13].
In 2003, Kim et al. developed a new version of DQI as DQI International (DQI-I) using the dietary data of the Chinese and US populations for global monitoring and exploration of diet quality across countries [14]. The DQI-I was developed based on four main categories including a variety of food groups, adequacy of some nutrients and food groups, moderation in intake of some nutrients, and overall balance in macronutrients and different types of fatty acids(FAs).
Over the past two decades, different research was designed to introduce and validates the DQI for different population groups based on periods of life such as children, adolescent, and elderly [15, 16], pregnant [17], or different diseases such as colorectal cancer [18] and diabetes(DM) [19], or different region such as DQI for Brazilians [20]. However, DQI as an instrument of diet quality, in a smaller number of studies has been assessed with the risk of cardiometabolic factors [21,22,23,24,25,26,27,28]. Funtikova et al. during a 10-year follow-up in adults indicated that higher DQI was beneficially related to lipid profile and waist circumference (WC) [21]. In another study in adolescents, higher adherence to a DQI adapted for Brazilian adolescents was associated with a better cardiometabolic profile in girls with normal weight; not in overweight/obese girls. In boys with overweight/obesity, higher DQI was associated with lower concentrations of total cholesterol and low-density lipoprotein cholesterol (LDL-c), but only LDL-C remained significant in boys with normal weight [24]. However, in a case-control study, Brazilian DQI revised and its components have not been associated with the development of breast cancer risk [22].
Studies investigating the DQI-I relationship with cardiometabolic factors are scarce. Setayeshgar and her colleagues indicated that a 10-unit improvement in DQI-I score was associated with lower gain in central fat mass and body fat percent after a 2-year follow-up in Canadian children [25]. In another study, DQI-I was not associated with BMI and obesity in Chinese adults with DM [28].
To our knowledge, only one study in Hong Kong assessed the DQI-I relationship with NAFLD and indicated that a 10-unit decrease in DQI-I was associated with a 26% increase in the likelihood of having NAFLD [27]. Regarding the lack of studies investigating the DQI-I and DQI-R relationship with NAFLD and the discrepancy in previous findings of DQI with cardiometabolic factors, we aimed to investigate the DQI-I and DQI-R relationship with NAFLD using a case-control study among Iranian adults.
Materials and methods
Study population
The present study was conducted in the Metabolic Liver Disease Research Center a referral center affiliated with Isfahan University of Medical Sciences. NAFLD or non-NAFLD discrimination was ascertained using the findings of liver ultrasonography scan (USG) and gastroenterologist diagnosis. For this study, patients who were not on a special diet, did not have overt kidney or liver disease (Wilson’s disease, autoimmune liver disease, virus infection, and alcoholic fatty liver), did not have cardiovascular diseases (CVDs), severe gastrointestinal disease, malignancy, thyroid disorder, and autoimmune disease, and don’t use drugs that could be hepatotoxic or steatogenic were included. Also, participants who completed fewer than 35 FFQ items and reported under or over-reported daily energy intake (800 or 4,500 kcal/d) were excluded. Totally 225 newly diagnosed NAFLD patients and 450 controls aged 20–60 years were included for final analysis. The study details were previously reported elsewhere [6, 29].
Dietary assessment
Dietary data collection was conducted using a previously validated and reliable semi-quantitative 168-item FFQ [30]. Trained dietitians while were blind about NAFLD status, asked participants to report their average dietary intake of each item of FFQ during the last year as follows: never or less than once a month, 3–4 times per month, once a week, 2–4 times per week, 5–6 times per week, once daily, 2–3 times per day, 4–5 times per day, and 6 or more times a day. Standard Iranian household measures were used for converting each food item’s portion size into a gram scale [31]. Different food groups are computed by summing their subgroup food items. Daily energy and nutrient intake were computed using the United States Department of Agriculture’s (USDA) Food Composition Table (FCT). Moreover, Iranian FCT was used for some local foods that were not listed in USDA FCT [32].
Assessment of other variables
Participants’ weight and height were recorded by standard protocols. BMI was calculated as weight (kg) divided by height in square meters (m2). Information about age, sex, education level, family size, house acquisition, foreign travel, and, and smoking status was gathered via a demographic questionnaire.
The combination of five variables, including education (academic = 1 and non-academic education = 0), family size (≤ 4 people = 1, > 4 people = 0), house acquisition (house ownership = 1, Lack of ownership = 0), foreign travel (yes = 1, no = 0), and income (high = 1, low and moderate = 0) were used to compute socioeconomic status (SES) score. Based on the frequency of SES scores in our study population, participants with SES score of 0 and 1, 2, 3–5 were classified as high, moderate, and low SES, respectively.
Physical activity levels were recorded through face-to-face interviews using the International Physical Activity Questionnaire (IPAQ). All measurements were expressed as Metabolic Equivalents per week (METs/week).
Calculation of DQI-I
The DQI-I was calculated according to the method developed by Kim et al. [14]. The score ranges from 0 to 100 and a higher score represents better diet quality. DQI-I was described using four major aspects of the diet including variety (0–20 score), adequacy (0–40 score), moderation (0–30 score), and overall balance (0–10 score). Details of the DQI-I calculation have been described elsewhere [14].
Variety score calculated from overall food group variety (meat/poultry/fish/eggs; dairy/beans; grain; fruit; vegetable) with a score of 0–15 and within-group variety for protein source (meat, poultry, fish, dairy, beans, eggs) with a score of 0–5. The adequacy score consists of 8 components with 0–5 points in each of them including vegetable, fruit, grain, fiber, protein, iron, calcium, and vitamin C. Moderation score was calculated based on total fat, saturated fat, cholesterol, sodium, and free-calorie foods that each item scored 0–6 points based on their described cut-points. The overall balance was created by macronutrient ratio (carbohydrate:protein: fat) and fatty acid ratio (PUFA:MUFA: SFA) which scored by 0–6 and 0–4 points, respectively.
Calculation of DQI-R
The DQI-R was computed based on the method described by Haines et al. [12]. They used ten components with 0–10 score for each of them including dietary intake of total fat, saturated fat, cholesterol, fruit, vegetables, grains, calcium, iron, dietary diversity, and dietary moderation.
Dietary diversity computed considering four main food groups with the maximum score of 2.5 including grains (7 subgroups), vegetables (7 subgroups), fruits (3 subgroups), and meat and dairy (7 subgroups) based on the cut-point equal to ¼ serving daily intake for each subgroup. We calculated the moderation score using three components with a maximum score of 2.5 for each of them including added sugar, discretionary fat, and sodium intake. As we did not have information on alcohol consumption to consider under the aspect of ‘moderation’. Therefore, the range of moderation score was 0 to 7.5 instead of 0 to 10 as originally proposed in the calculation. Totally DQI-R score ranged from 0 to 97.5 instead of 0 to 100. Details of the DQI-R calculation have been described elsewhere [12].
Statistical analysis
All statistical analysis was performed using Statistical Package Software for Social Science, version 21 (SPSS Inc., Chicago, IL, USA). The normality of variables was assessed by the Kolmogorov-Smirnov test and histogram chart. Population characteristics and dietary data were expressed as mean ± SD or median (25–75 interquartile range) for quantitative variables and percentages for qualitative variables. Comparing differences between cases and controls for continuous and categorical variables were assessed using independent sample t-test and chi-square test, respectively.
Participants were classified into tertiles based on the DQI-I, DQI-R, and some of their component cut-points among the control group. Also, the frequency of SD of mean intake of DQI-I, DQI-R, and some of their components was computed for each study participant. Multivariable logistic regression was performed to investigate the relationship between DQI-I, DQI-R, and some of their components and the odds of NAFLD. Analyses were conducted in a crude model, age and sex-adjusted model, and finally adjusted for BMI, physical activity, smoking, SES, and dietary intake of energy. The odds ratio (OR) and 95% confidence interval (CI) of NAFLD across tertiles of DQI-I, DQI-R, and some of their components were reported. We determined one SD of the DQI-I and DQI-R for individuals using SPSS software, which were considered as new variables named ZDQI-I and ZDQI-R in the data set. Then, the association of increasing each SD of DQI-I and DQI-R with the odds of NAFLD was determined using logistic regression with the adjustment of the effect of potential confounders. P-values < 0.05 were considered statistically significant.
Results
The mean ± SD of DQI-I and DQI-R in all study populations were 66.6 ± 8.3 (66.8 ± 7.9 in cases and 66.4 ± 8.5 among controls) and 76.2 ± 13.3 (75.0 ± 13.0 in cases and 76.8 ± 13.4 among controls), respectively.
Table 1 shows the general information and scores of DQI-I and its components (per 1000 kcal of energy intake) among cases and controls. Compared to the control group, NAFLD patients had significantly higher BMI, % smoking, family size, foreign travel, income, and better SES (P < 0.01), whereas had lower physical activity and house ownership (P < 0.01). For DQI-I and its components, Compared to the control group, NAFLD patients had a lower total variety score, a lower score of overall food group variety, and a higher score of variety for protein source (P < 0.01). Also, in NAFLD patients, total adequacy score, and adequacy scores for vegetables, fruits, fiber, protein, iron, calcium, and vitamin C were lower than the control group (P < 0.01). Furthermore, the total moderation score and moderation scores for cholesterol and free-calorie foods, and the total score of DQI-I in the case group were lower than the controls (P < 0.05).
Dietary data and scores of DQI-R and its components (per 1000Kcal of energy intake) in the cases and the controls are presented in Table 2. Compared to the control group, NAFLD patients had significantly lower scores of dietary cholesterol, vegetable, and iron, lower diversity of vegetables and fruits, and lower total moderation scores, lower moderation scores of added sugar and discretionary fat, and lower total score of DQI-R (P < 0.05), whereas energy intake in case group was significantly higher than controls (P < 0.01).
The association of DQI-I and its main components with the odds of NAFLD is indicated in Table 3. Although participants in the highest versus lowest tertiles of DQI-I, variety score, and moderation score showed significant inverse associations with the odds of NAFLD in crude and age and sex-adjusted models, after adjusting for BMI, smoking, physical activity, SES, and energy intake in the final adjusted model, there was no significant association between higher DQI-I (OR = 0.69, 95%CI(0.28–1.69); P-trend: 0.509), variety score (OR = 0.50, 95%CI(0.23–1.11); P-trend: 0.077), and moderation score (OR = 0.79, 95%CI(0.39–1.60); P-trend: 0.533) with the odds of NAFLD. However, participants in the highest vs. lowest tertile of adequacy score were associated with lower odds of NAFLD based on the crude model (OR = 0.43, 95%CI(0.28–0.65); P-trend < 0.001), age and sex-adjusted model (OR = 0.42, 95%CI(0.28–0.64); P-trend < 0.001), and the final adjusted model (OR = 0.16, 95%CI(0.06–0.40); P-trend < 0.001). According to results reported for three models of logistic regression analyses, the score of overall balance was not related to the odds of NAFLD.
In Table 3, the OR of NAFLD per each SD increment of DQI-I and its main components in different adjusted models are presented. Each SD increment of DQI-I and adequacy score was related to lower odds of NAFLD in all adjusted models; in the fully adjusted model, the OR (95%CI) of NAFLD per one SD increment of DQI-I and adequacy score were 0.63 (0.40–0.98) and 0.39 (0.24–0.65), respectively (P < 0.05). In the crude and age and sex-adjusted models, per one SD increment of moderation score, the odds of NAFLD significantly decreased, however, in the final adjusted model the significant association disappeared (OR = 0.83, 95%CI: 0.61–1.13; P-value: 0.260). In three models of logistic regression analysis, no significant association was observed between one SD increment of variety and overall balance scores and odds of NAFLD; in the multivariable model, the OR (95%CI) of NAFLD per one SD increment of variety and overall balance scores were 0.93 (0.67–1.28) and 1.14 (0.90–1.43), respectively (P > 0.05).
Table 4 shows the OR (95%CI) of NAFLD across tertiles of DQI-R and its main components and also per one SD of scores in 1000 Kcal of energy intake. Higher scores of DQI-R and dietary moderation score were associated with lower odds of NAFLD in all regression models; The OR (95% CI) of NAFLD for participants in the highest vs. lowest tertiles of DQI-R in the crude and final models respectively were 0.39 (0.25–0.59), P-trend:<0.001 and 0.24 (0.10–0.53), P-trend:<0.001. Also The OR (95% CI) of NAFLD for participants in the highest vs. lowest tertiles of dietary moderation score in the crude and final adjusted models were 0.34 (0.22–0.52), P-trend < 0.001 and 0.17 (0.07–0.43), P-trend < 0.001, respectively. However, in each three models of logistic regression analysis, the higher score of dietary diversity was not associated with the odds of NAFLD; in the final adjusted model, the OR (95%CI) of NAFLD in the highest vs. lowest tertile of dietary diversity score was 0.99 (0.46–2.15), P-trend: 0.920.
Furthermore, results of Table 4 showed that each SD increment of DQI-R and dietary moderation scores were associated with lower odds of NAFLD in all adjusted models; in the final adjusted model, the OR (95%CI) of NAFLD for DQI-R and dietary moderation score were 0.49 (0.34–0.70), P-value:<0.001 and 0.33 (0.21–0.51), P-value:<0.001, respectively. However, one SD increment in dietary diversity score was not associated with NAFLD in any of the logistic models; in the final adjusted model, the OR (95%CI) of NAFLD per one SD of dietary diversity score was 0.86 (0.64–1.16), P-value: 0.341.
Discussion
The current case-control study suggested that a diet with higher scores of DQI-I and DQI-R was associated with lower odds of NAFLD among Iranian adults. Also, the higher score of adequacy (as a DQI-I component) and higher score of dietary moderation (as a component of DQI-R) were related to lower odds of NAFLD. However, we observed no significant association between scores of variety, moderation, and overall balance as components of DQI-I and dietary diversity as a component of DQI-R with odds of NAFLD.
Our findings are consistent with the results of one observational study that assessed the possible relationship between DQI-I and the risk of NAFLD; the Chan et al. study reported that higher DQI-I was associated with a reduced likelihood of NAFLD in Hong Kong adults [27]. Also, the results of the current study are somewhat comparable with the results of investigations that focused on the association of DQI and risk of cardiometabolic disorders; consistent with our findings, the Setayeshgar et al. study indicated that a 10-unit improvement in DQI-I score was associated with lower gain in central fat mass and body fat percent after a 2-year follow-up in Canadian children. Also, they showed that among DQI-I components including variety, adequacy, moderation, and overall balance, only a higher adequacy score was associated with lower gain in fat mass index and body fat percent [25]; such a finding was also observed in our study and among DQI-I components, only higher adequacy score was related with lower odds of NAFLD. In addition, Funtikova et al. study suggested that higher DQI related to a higher level of high-density lipoprotein cholesterol (HDL-C), whereas an inverse association was observed between DQI and levels of waist circumference (WC), triglycerides (TG), and the TG to HDL-C ratio during a 10-year follow-up in adults [21]. The above-mentioned studies showed that higher DQI-I is a good instrument for predicting the reduction of body fat accumulation and hypertriglyceridemia. However, it seems that DQI-I has not been able to adequately estimate the risk of obesity and high BMI, because, in five previous studies among Iranian, Chinese, Canadian, and Spanish populations, no significant association was found between the higher score of DQI-I and BMI and obesity [21, 25, 28, 33].
The results of the present study suggested that the moderation score of DQI-I can be a good indicator of detrimental nutrients and foods that may be related to NAFLD risk. Despite the inverse association of this score with odds of NAFLD in the age and sex-adjusted model, it seems that its effects were not as strong as the need to overcome the BMI and other confounders’ effects. However, an observational study conducted on Iranian patients with a history of myocardial infarction suggested that a higher moderation score of DQI-I was associated with a better lipid profile and lower WC [34]. In general, although the available limited results support the moderation score of DQI-I as a protective factor to prevent metabolic disorders and diseases, the results of our study suggest that the conclusion about the positive effect of this DQI-I component on reducing the NAFLD risk is still premature and there is a need to do more research on this subject.
In the current study, the variety score of DQI-I was not different among cases and controls, however, its components paradoxically were different in cases and controls, and by the way that NAFLD patients consumed more diverse protein sources, whereas consumed lower diverse food groups. This issue leads to a decrease in the strength of this index in observing a significant relationship with NAFLD in the final adjusted model of covariates. Controversy on the possible effect of the variety score of DQI-I on metabolic factors was observed in the Sharifi et al. study, as the score of DQI-I was not linked to levels of BMI and WC, whereas a higher score of this dietary index had a positive association with HDL-C and TGs and a negative association with LDL-C [34]. Also, generally different dietary diversity scores were assessed in two previous systematic reviews and meta-analyses and their pooled results showed no significant association between dietary diversity score and BMI, obesity, and lipid profile except for TGs [35, 36].
In the current study, the overall balance score of DQI-I and its components including the macronutrient ratio and the fatty acid ratio was not different between the case and control groups, and higher overall balance showed no significant association with odds of NAFLD. Definitely, total calorie intake has the main role in body weight regulation and consequently body composition [37]. However, the dietary macronutrient and the fatty acid ratio have been proposed as effective factors in body composition. A previous review study showed that the effects of dietary composition on fat storage in the liver are inconsistent [38]. Also, a meta-analysis of trials reported no differences in weight loss and changes in cardiovascular and diabetes risk factors with two different dietary compositions (low CHO diets vs. isocaloric balanced diets) which is related to overall balance score [39]. Moreover, the optimal proportions of dietary macronutrients in the prevention or treatment of NAFLD patients are unknown, and maintaining a eucaloric diet along with avoiding saturated fatty acids and simple sugars is supported by the literature [37].
To the best of our knowledge, this is the first study that assessed the DQI-R and its diversity and moderation components with the odds of NAFLD and found an inverse association between DQI-R and the moderation score of DQI-R with NAFLD. Our results partly are in line with the study by Ritter et al. who showed that higher adherence to a DQI adapted for Brazilian adolescents was associated with a better cardiometabolic profile in girls with normal weight; not in overweight/obese girls. In boys with overweight/obesity, higher DQI was associated with lower concentrations of total cholesterol and low-density lipoprotein cholesterol (LDL-C), but only LDL-C remained significant in boys with normal weight [24]. Although some other studies assessed diet quality index with other chronic diseases (CDs) such as breast cancer [22], cardiovascular risk factors [40], and mortality [26], their calculated DQI had considerable differences with DQI-R developed by Haines et al. [12], which we used in our study. The moderation score of the DQI-R in our study was calculated from added sugar, discretionary fat, and sodium intake. NAFLD patients had a significantly lower score of total moderation score, added sugar, and discretionary fat than the control group. Previous studies showed the adverse effects of added sugar [41] and high fat intake [42] on NAFLD. However, in the present study dietary diversity score of DQI-R did not differ among the case and control and showed no association with NAFLD. As we mentioned above, this result is a confirmation of two previous meta-analysis that observed any significant association between dietary diversity and metabolic factors [35, 36].
The inverse relationship between a diet with higher score of DQI-I and DQI-R and NAFLD risk can be explained by some potential mechanisms and reasons; DQI-I and DQI-R have been created by considering the main food groups, some essential nutrients, and detrimental components of diet; so a higher score of these indices presents a diet rich in beneficial food groups and poor in detrimental dietary factors, which based on their unique characteristics and interaction with each other in the form of a dietary pattern, show their role in predicting the risk of metabolic disorders such as NAFLD. Higher diet quality has a generally positive correlation with all food groups and consequently more consumption of all essential and non-essential nutrients particularly fiber, protein, calcium, iron, vitamin C, w-3 fatty acids, and other antioxidant components such as vitamin A, polyphenols, and phytochemicals which previously showed an inverse association with NAFLD based on the anti-inflammatory properties, anti-oxidant effects, and prevention of adiposity [5,6,7,8, 29, 43]. On the other hand, it is negatively correlated with total fat, SFA, cholesterol, sodium, added sugars, and pro-inflammatory agents that showed adverse effects on metabolic factors [9, 41, 42].
The present study has some strengths; this is the first study that reported an association between DQI-R and its components and the odds of NAFLD in Iranian adults. Another strength is that dietary intake was assessed using locally validated questionnaires among the Iranian population, which were administered by trained and experienced dietitians through face-to-face interviews which minimized measurement errors. We acknowledge some limitations in the present study. First, because of the case-control design of this study, it is not possible to suggest a causal relationship. Second, the inevitable measurement error of FFQ or other unknown confounders may also affect our results. Third, another limitation of the current study was that the cases and controls were not matched based on important variables, such as age, gender, and BMI, however, it should be noted based on results reported in Table 1, no significant difference was observed in age and sex between the cases and controls. Also, the potential confounding effect of these variables mentioned above along with some other variables was controlled in the multivariable regression analysis. Finally, we did not have data on menopausal status, the number of pregnancies, hormonal conditions of participants, genetic data, etc. for further investigations.
Conclusions
In summary, the findings of this case-control study revealed a possible protective role of a diet with a higher score of DQI-I and DQI-R against the odds of NAFLD. Future studies using larger sample sizes and prospective designs need to address the DQI-I and DQI-R and their components with NAFLD and other chronic diseases.
Data availability
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
body mass index
- CDs:
-
chronic diseases
- CI:
-
confidence interval
- CVDs:
-
cardiovascular diseases
- DALYs:
-
disability-adjusted life years
- DM:
-
diabetes
- DQI:
-
diet quality index
- DQI-I:
-
DQI International
- Fats:
-
fatty acids
- FCT:
-
Food Composition Table
- FFQ:
-
food frequency questionnaire
- HDL-C:
-
high-density lipoprotein cholesterol
- IPAQ:
-
International Physical Activity Questionnaire
- LDL-c:
-
low-density lipoprotein cholesterol
- METs:
-
Metabolic Equivalents
- MUFA:
-
mono-unsaturated saturated fatty acid
- NAFLD:
-
non-alcoholic fatty liver diseases
- OR:
-
odds ratio
- PUFA:
-
polyunsaturated saturated fatty acid
- SD:
-
standard deviation
- SES:
-
socioeconomic status
- SFA:
-
saturated fatty acid
- USDA:
-
United States Department of Agriculture’s
- USG:
-
liver ultrasonography scan
- WC:
-
waist circumference
References
Le MH, Yeo YH, Zou B, Barnet S, Henry L, Cheung R, et al. Forecasted 2040 global prevalence of nonalcoholic fatty Liver Disease using hierarchical bayesian approach. Clin Mol Hepatol. 2022;28(4):841–50.
Jiang W, Mao X, Liu Z, Zhang T, Jin L, Chen X. Global Burden of Nonalcoholic Fatty Liver Disease, 1990 to 2019: findings from the global burden of Disease Study 2019. J Clin Gastroenterol. 2022.
Ko E, Yoon EL, Jun DW. Risk factors in nonalcoholic fatty Liver Disease. Clin Mol Hepatol. 2022.
Jahromi MK, Daftari G, Farhadnejad H, Tehrani AN, Teymoori F, Salehi-Sahlabadi A, et al. The association of healthy lifestyle score and risk of non-alcoholic fatty Liver Disease. BMC Public Health. 2023;23(1):973.
Salehi-Sahlabadi A, Teymoori F, Ahmadirad H, Mokhtari E, Azadi M, Seraj SS, et al. Nutrient patterns and non-alcoholic fatty Liver Disease in Iranian Adul: a case-control study. Front Nutr. 2022;9:977403.
Mokhtari E, Farhadnejad H, Salehi-Sahlabadi A, Najibi N, Azadi M, Teymoori F, et al. Spinach consumption and nonalcoholic fatty Liver Disease among adults: a case–control study. BMC Gastroenterol. 2021;21(1):196.
Bahrami A, Teymoori F, Eslamparast T, Sohrab G, Hejazi E, Poustchi H, et al. Legume intake and risk of nonalcoholic fatty Liver Disease. Indian J Gastroenterol. 2019;38(1):55–60.
Mirmiran P, Teymoori F, Farhadnejad H, Mokhtari E, Salehi-Sahlabadi A. Nitrate containing vegetables and dietary nitrate and nonalcoholic fatty Liver Disease: a case control study. Nutr J. 2023;22(1):3.
Farhadnejad H, Tehrani AN, Jahromi MK, Teymoori F, Mokhtari E, Salehi-Sahlabadi A, et al. The association between dietary inflammation scores and non-alcoholic fatty Liver Diseases in Iranian adults. BMC Gastroenterol. 2022;22(1):267.
Emamat H, Farhadnejad H, Poustchi H, Teymoori F, Bahrami A, Hekmatdoost A. The association between dietary acid load and odds of non-alcoholic fatty Liver Disease: a case-control study. Nutr Health. 2023;29(4):637–44.
Patterson RE, Haines PS, Popkin BM. Diet quality index: capturing a multidimensional behavior. J Am Diet Assoc. 1994;94(1):57–64.
Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index revised: a measurement instrument for populations. J Am Diet Assoc. 1999;99(6):697–704.
Newby PK, Hu FB, Rimm EB, Smith-Warner SA, Feskanich D, Sampson L, et al. Reproducibility and validity of the Diet Quality Index revised as assessed by use of a food-frequency questionnaire. Am J Clin Nutr. 2003;78(5):941–9.
Kim S, Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index-International (DQI-I) provides an effective tool for cross-national comparison of diet quality as illustrated by China and the United States. J Nutr. 2003;133(11):3476–84.
Serra-Majem L, Ribas L, Ngo J, Ortega RM, García A, Pérez-Rodrigo C, et al. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004;7(7):931–5.
Dorrington N, Fallaize R, Hobbs D, Weech M, Lovegrove JA. Diet Quality Index for older adults (DQI-65): development and use in predicting adherence to dietary recommendations and health markers in the UK National Diet and Nutrition Survey. Br J Nutr. 2022;128(11):2193–207.
Crivellenti LC, Zuccolotto DCC, Sartorelli DS. Development of a Diet Quality Index adapted for pregnant women. Rev Saude Publica. 2018;52:59.
Vulcan A, Ericson U, Manjer J, Ohlsson B. A Colorectal cancer diet quality index is inversely associated with Colorectal cancer in the Malmö diet and cancer study. Eur J Cancer Prev. 2019;28(6):463–71.
Golmohammadi M, Zarrin R, Ayremlou P. Adaptation and validity assessment of a diet quality index for patients with type 2 Diabetes. J Diabetes Metab Disord. 2020;19(2):1027–36.
Pires RK, Luft VC, Araújo MC, Bandoni D, Molina MDC, Chor D, et al. [Critical analysis of the revised diet quality index for the Brazilian population (DQI-R): its application in ELSA-Brasil]. Cien Saude Colet. 2020;25(2):703–13.
Funtikova A, Baena-Díez JM, Koebnick C, Gomez SF, Covas MI, Goday A, et al. Validity of a short diet-quality index to predict changes in anthropometric and cardiovascular risk factors: a simulation study. Eur J Clin Nutr. 2012;66(12):1369–71.
Godoy LM, Pinheiro MA, Godinho-Mota JCM, Vaz-Gonçalves L, Schincaglia RM, Martins KA, et al. Diet quality index and its components have not associated with the development of Breast cancer risk assessed by the diet quality index: a case-control study. Rev Bras Epidemiol. 2022;25:e220027.
Kranz S, Findeis JL, Shrestha SS. Use of the revised children’s Diet Quality Index to assess preschooler’s diet quality, its sociodemographic predictors, and its association with body weight status. J Pediatr (Rio J). 2008;84(1):26–34.
Ritter JDA, Cureau FV, Ronca DB, Blume CA, Teló GH, Camey SA, et al. Association between diet quality index and cardiometabolic risk factors in adolescents: study of Cardiovascular risks in adolescents (ERICA). Nutrition. 2021;90:111216.
Setayeshgar S, Maximova K, Ekwaru JP, Gray-Donald K, Henderson M, Paradis G, et al. Diet quality as measured by the Diet Quality Index-International is associated with prospective changes in body fat among Canadian children. Public Health Nutr. 2017;20(3):456–63.
Seymour JD, Calle EE, Flagg EW, Coates RJ, Ford ES, Thun MJ. Diet Quality Index as a predictor of short-term mortality in the American Cancer Society Cancer Prevention Study II Nutrition Cohort. Am J Epidemiol. 2003;157(11):980–8.
Chan R, Wong VW, Chu WC, Wong GL, Li LS, Leung J, et al. Diet-Quality scores and Prevalence of nonalcoholic fatty Liver Disease: a Population Study using Proton-magnetic resonance spectroscopy. PLoS ONE. 2015;10(9):e0139310.
Cheung LTF, Chan RSM, Ko GTC, Lau ESH, Chow FCC, Kong APS. Diet quality is inversely associated with obesity in Chinese adults with type 2 Diabetes. Nutr J. 2018;17(1):63.
Salehi-sahlabadi A, Teymoori F, Jabbari M, Momeni A, Mokari-yamchi A, Sohouli M, et al. Dietary polyphenols and the odds of non-alcoholic fatty Liver Disease: a case-control study. Clin Nutr ESPEN. 2021;41:429–35.
Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women. Am J Clin Nutr. 2007;85(3):910–8.
Ghaffarpour MH-RA, Kianfar H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran: Nashre Olume Keshavarzy. 1999;7(213):42–58.
Azar M. In: Sarkisian E, editor. Food composition table of Iran. Volume 65. Tehran: National Nutrition and Food Research Institute, Shaheed Beheshti University; 1980.
Alipour Nosrani E, Majd M, Bazshahi E, Mohtashaminia F, Moosavi H, Ramezani R, et al. The association between meal-based diet quality index-international (DQI-I) with obesity in adults. BMC Nutr. 2022;8(1):156.
Sharifi MH, Izadpanah P, Hosseini MM, Vojoudi M. Relationship between dietary variety, adequacy, moderation, and balanced diet and cardiovascular risk factors. BMC Nutr. 2022;8(1):20.
Salehi-Abargouei A, Akbari F, Bellissimo N, Azadbakht L. Dietary diversity score and obesity: a systematic review and meta-analysis of observational studies. Eur J Clin Nutr. 2016;70(1):1–9.
Qorbani M, Mahdavi-Gorabi A, Khatibi N, Ejtahed HS, Khazdouz M, Djalalinia S, et al. Dietary diversity score and cardio-metabolic risk factors: an updated systematic review and meta-analysis. Eat Weight Disord. 2022;27(1):85–100.
Pixner T, Stummer N, Schneider AM, Lukas A, Gramlinger K, Julian V et al. The role of macronutrients in the Pathogenesis, Prevention and Treatment of non-alcoholic fatty Liver Disease (NAFLD) in the Paediatric Population-A Review. Life (Basel). 2022;12(6).
Hashemi Kani A, Alavian SM, Haghighatdoost F, Azadbakht L. Diet macronutrients composition in nonalcoholic fatty Liver Disease: a review on the related documents. Hepat Mon. 2014;14(2):e10939.
Naude CE, Schoonees A, Senekal M, Young T, Garner P, Volmink J. Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS ONE. 2014;9(7):e100652.
Nouri F, Sadeghi M, Mohammadifard N, Roohafza H, Feizi A, Sarrafzadegan N. Longitudinal association between an overall diet quality index and latent profiles of cardiovascular risk factors: results from a population based 13-year follow up cohort study. Nutr Metab (Lond). 2021;18(1):28.
Zhang S, Li H, Meng G, Zhang Q, Liu L, Wu H et al. Added sugar intake and its forms and sources in relation to risk of non-alcoholic fatty Liver Disease: results from the TCLSIH cohort study. Br J Nutr. 2022:1–20.
Lian CY, Zhai ZZ, Li ZF, Wang L. High fat diet-triggered non-alcoholic fatty Liver Disease: a review of proposed mechanisms. Chem Biol Interact. 2020;330:109199.
Salehi-Sahlabadi A, Teymoori F, Mokhtari E, Taghiyar M, Hekmatdoost A, Mirmiran P. Dietary phytochemical index and the risk of non-alcoholic fatty Liver Disease: a case-control study among Iranian adults. Complement Ther Med. 2022;71:102881.
Acknowledgements
We appreciate the Isfahan University of Medical Sciences for their financial support of this study. The authors express their appreciation to all of the participants of this study.
Funding
Not funding.
Author information
Authors and Affiliations
Contributions
NN and FT conceptualized and designed the study. FT and HF analyzed and interpreted the data. NN, MKJ, and AS-s drafted the initial manuscript. PM supervised the project. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Informed written consent was obtained from participants. All procedures performed in studies involving human participants adhered to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics research committee approved the study’s protocol of the Isfahan University of Medical Sciences, Isfahan, Iran.
Consent for publication
Not applicable.
Conflict of interest
The authors declared there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Najibi, N., Jahromi, M.K., Teymoori, F. et al. International diet quality index and revised diet quality index relationship with non-alcoholic fatty liver disease: a case-control study. BMC Gastroenterol 23, 441 (2023). https://doi.org/10.1186/s12876-023-03082-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-03082-x