Abstract
Background
The most prevalent stomach infection in the world is caused by Helicobacter pylori (H. pylori). Several pathogenicity genes, including cagA, vacA, babA2, dupA, iceA, and oipA, are associated with an increased risk of gastrointestinal disease such as peptic ulcer and stomach cancer. This research aims to determine the prevalence of different H. pylori genotypes and correlate their risk in the development of gastrointestinal diseases in the Ecuadorian population.
Methods
A cross-sectional research of 225 patients at the Calderón Hospital in Quito, Ecuador, was conducted. End point PCRs were run to determine the presence of 16S rRNA, cagA, vacA (m1), vacA (s1), babA2, dupA, iceA1, and oipA virulence genes. Chi-square test, odds ratios (OR) and 95% confidence intervals (CI) were utilized for the statistical analysis.
Results
H. pylori infection was present in 62.7% of people. Peptic ulcers were seen in 22.2% and malignant lesions in 3.6% of patients. Genes oipA (93.6%), vacA (s1) (70.9%), and babA2 (70.2%) were the most prevalent. cagA/vacA (s1m1) and cagA/oipA (s1m1) combinations were found in 31.2% and 22.7% of the cases, respectively. Acute inflammation has a significant correlation with the genes cagA (OR = 4.96 95% CI: 1.1–22.41), babA2 (OR = 2.78 95% CI: 1.06–7.3), and the cagA/oipA combination (OR = 4.78, 95% CI: 1.06–21.62). Follicular hyperplasia was associated with iceA1 (OR = 3.13; 95% CI: 1.2–8.16), babA2 (OR = 2.56; 95% CI: 1.14–5.77), cagA (OR = 2.19; 95% CI: 1.06–4.52), and the cagA/oipA combination (OR = 2.32, 95% CI: 1.12–4.84). The vacA (m1) and vacA (s1m1) genes were associated with gastric intestinal metaplasia (OR = 2.71 95% CI: 1.17–6.29) (OR = 2.33 95% CI: 1.03–5.24). Finally, we showed that cagA/vacA (s1m1) gene combination increased the risk of duodenal ulcer development (OR = 2.89, 95% CI 1.10–7.58).
Conclusion
This study makes a significant contribution by offering genotypic information regarding H. pylori infection. The presence of several H. pylori genes was associated with the onset of gastrointestinal illness in the Ecuadorian population.
Similar content being viewed by others
Introduction
Helicobacter pylori (H. pylori) is the microorganism responsible for the most common stomach infection worldwide. Currently, its prevalence is higher in Africa, South America, and Western Asia and is related to an increased incidence of gastric cancer [1]. In Latin America and Caribbean, H. pylori infection affects 48.36% of children and adolescents, reaching a prevalence of 69.26% in adulthood [2]. The high rate of infection in these countries is related to a high percentage of chronic complications, becoming a health problem of transcendental importance [1].
H. pylori infection and the emergence of gastric and duodenal ulcers as well as gastric adenocarcinoma are closely related. The exact mechanisms are still unknown since they are long-term processes influenced by dietary factors, the host's genetic vulnerability, environment influence and the virulence of the H. pylori strains [3]. Seven distinct strains of H. pylori can be distinguished based on their geographic origin according to the structure's high genetic variability [4, 5]. European, Australian, Asian, East Asian, North African, South African, and West African. The Colombian Andes have been revealed to have the European genotype, which was probably brought from that continent thousands of years ago [6].
The virulence of H. pylori is correlated with several pathogenicity genes (cagA, vacA, babA2, dupA, iceA, and oipA), whose proteins take part in colonization procedures, immune response evasion, and the presence of these genes has been considered to be a predictor of severe clinical consequences [7]. For instance, cytotoxin associated with gene A (CagA) can alter the cell cycle, induce apoptosis, and cause the release of interleukins that promote inflammation. The epigenetic alterations brought on by this toxin, such as histone hypermethylation, can also result in the downregulation of tumor suppressor genes [8]. It appears that the EPIYA-A, EPIYA-B, EPIYA-C, and EPIYA-D motifs in its C-terminal region are associated for virulence and carcinogenesis [9].
Gastric cells undergo several changes as a result of the vacuolating cytotoxin linked to gene A (VacA), including the formation of cytoplasmic vacuoles, permeabilization of the plasma membrane, mitochondrial fragmentation, and activation of kinase enzymes [10]. VacA presents three polymorphic areas, the signal region (s), intermediate region (i), and middle region (m). It has been shown that the vacA s1m1 genotype is the most hazardous due to its high production of toxins that result in the release of inflammatory chemicals that alter the gastric mucosa and increase the risk of gastric adenocarcinoma [11].
The H. pylori outer membrane contains the blood group antigen-binding adhesin (BabA), which is encoded by the babA2 gene. BabA can detect the highly expressed Lewis b blood group antigen (Leb) in gastric cells [12]. BabA contributes to CagA's translocation via the type IV secretion system and signal transduction (T4SS), which causes the stomach mucosa to become severely inflamed. BabA has been linked to a higher incidence of chronic gastritis, distal gastric cancer, and peptic ulcers [13].
Duodenal ulcer risk has been linked to the gene dupA due to increased mucosal inflammation, neutrophil infiltration, and increased interleukin-8 (IL-8) expression in the antrum. Additionally, it has been linked to an increased risk of atrophy, gastric cancer, and intestinal metaplasia [14].
One candidate for a marker for peptic ulcer propensity is the A gene induced by contact with the epithelium (iceA). Although they share a location in the bacterial genome, their two variations, iceA1, and iceA2, are unrelated. Increased levels of IL-8 in the stomach mucosa have been related to peptic ulcer disease caused by infection with the iceA1 strain [15].
The oipA gene encodes an inflammatory outer membrane protein with activity for bacterial adhesion to the mucosa. Independent of other virulence factors, infection with the active OipA strain has been linked to an increased risk of duodenal ulcer [16].
Gastric cancer was the seventh leading cause of death in Ecuador in 2019 and was most prevalent in people between the ages of 30 and 64 [17]. Although H. pylori infection is a public health issue, in Ecuador, there is no research supporting the pathogenic role of the H. pylori virulence genes in the development of gastrointestinal diseases. Therefore, the purpose of this research is to determine the prevalence of different H. pylori genotypes and correlate their presence with the probability of developing gastrointestinal clinical and histological changes.
Materials and methods
Study design
A total of 225 patients who underwent gastrointestinal endoscopies at the Calderón Hospital in Quito, Ecuador, between August 2020 and February 2021 were included in this observational, cross-sectional study.
Inclusion and exclusion criteria
The included patients were adults over the age of 18, had not received any antibiotics or proton pump inhibitors at least one month before the endoscopic procedure, nor had they received treatment to eradicate H. pylori during the previous 12 months (see Fig. 1).
Data collection
The sociodemographic and clinical information were obtained from the patients who voluntarily accepted participate in the study. Gastric biopsies of the antrum, body, and incisura angularis were taken during the endoscopic examination for histological analysis in the pathological anatomy laboratory of the Calderón Hospital, following the modified Sydney protocol [18]. The Central University of Ecuador's "Dr. Rodrigo Fierro Benitez" Biomedicine Research Institute conducted molecular diagnostics and genotyping. The study was approved by the Ethics Committee for Research in Human Beings of the Central University of Ecuador (0121-SEISH-UCE-20) and the National Directorate of Health Intelligence of the Ministry of Public Health of Ecuador (MSP-DIS 2020–0135-O). An informed consent was obtained from the participants. Legally Authorized Representatives of illiterate participants provided informed consent for the study. In this case, the details of the study were explained verbally in the company of the legally authorized representative of the illiterate participants and the participant's fingerprint was placed on the informed consent.
Genotyping
Following the manufacturer's instructions, DNA was extracted from the antrum biopsy using the PureLink Genomic DNA kit (Cat. K1820-02, Invitrogen). The samples were eluted in 50 uL of buffer, and Nanodrop One was used to assessing their quality. The DNA samples were kept at -40 °C in concentrations of 30 ng/L. Using primers designed for the hypervariable zone (V4-V9) of the 16SrRNA region, polymerase chain reaction (PCR) was used to detect the presence of H. pylori. The cagA, vacA (m1), vacA (s1), babA2, iceA1, dupA, and oipA genes were subsequently tested in samples that had previously tested positive for H. pylori (see Table 1).
The GoTaq Green Master Mix (2X) (Cat. M7123, Promega), 0.2 to 0.5 uM of each primer, and 1 μL of DNA were combined to prepare the PCR reactions with a final volume of 25 µL per reaction. The parameters used for PCR amplification were similar to the references in Table 1. The thermocycler used for the amplification was a GeneAmp System 2700. (Applied Biosystem, USA). The PCR results were observed using electrophoresis in 1.5% TBE 1X agarose gels, which were stained with Sybr Safe and ran for 60 min at 100 V to determine the size of the bands.
Statistical analysis
Data are presented as total numbers and percentages, as appropriate. The chi-square test was used to analyze significant differences between the frequencies of sociodemographic variables (sex, age, education and ethnicities) and the result of H. pylori diagnostic and clinical/histopathological characteristics. Odds ratios (OR) and 95% confidence intervals (CI) were calculated to assess the association between gastric diseases and the presence of H. pylori genes (cagA, vacA (m1), vacA (s1), babA2, iceA1, dupA, oipA). Statistics were considered to be significant at p < 0.05. Software IBM, SPSS version 23 was utilized for the statistical analysis.
Results
Sociodemographic characteristics
The study included 225 patients who met the inclusion criteria. Histological diagnostic revealed H. pylori infection in 58.7% of the cases, in contrast to PCR where 62.7% of the participants confirmed the infection. Using the PCR results, we identified significant association between age and H. pylori infection, being more frequent in those under 40 years old. Gender, ethnicity, low level (illiterate, elementary and high school) and high level (University) of education did not appear to be significant factors (see Table 2).
Clinical and histological features
The endoscopic examination revealed that 22.2% of the patients had peptic ulcers (gastric or duodenal), which were more common in men (p = 0.042), in adults over 50 years (p = 0.034), and people with low level of education (p = 0.019). In particular, stomach ulcers occurred in 11.6% of patients, and duodenal ulcers in 13.8% (see Table 3).
74.7% of the patients had acute gastritis, and neither gender, age, education level, nor ethnicity showed any significant differences. In 97.8% of the patients, the histological diagnostic of chronic gastritis was established; the frequency was higher in the indigenous population (p < 0.001) (data not shown). A higher prevalence of lymphoid follicular hyperplasia was seen in patients under 40 (p < 0.001) and in those with a high level of education (p = 0.044), accounting for 31.6% of the cases. In 61.3% of the cases, gastric atrophy was identified; it was significantly prevalent among individuals over 50 years (p = 0.011). Intestinal metaplasia was detected in 28.9% of cases, the elderly individuals exhibiting a greater prevalence (p = 0.001). Gastric cancer was diagnosed in 3.6% of the cases, showing significant differences in Afro-American ethnicity (p = 0.013) (see Table 3). Half of the cases with stomach cancer were revealed to have malignant lesions of Borrmann type 3 and the other half to have high-grade adenomas.
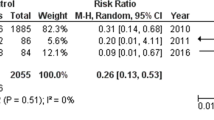
H. pylori genotypes and clinical characteristics
Greater prevalence was seen for the genes oipA (93.6%), vacA (s1) (70.9%), and babA2 (70.2%). cagA, vacA (m1), vacA (s1m1), iceA1, dupA and the combination cagA/oipA and cagA/vacA, (s1m1) were presented in less than 50% of the patients (see Table 4). The cagA gene was more common in adults between the ages of 40 and 50 (31.9%; p = 0.033) (data not shown). Moreover, we found that the cagA/vacA (s1m1) gene combination increased the risk of duodenal ulcer development (OR = 2.89, 95% CI 1.10–7.58). On the other hand, the presence of the genes cagA (OR = 0.22, 95% CI 0.05–0.98) and babA2 (OR = 0.25, 95% CI 0.09–0.67) were linked to a lower risk of developing stomach ulcers (see Table 4).
H. pylori genotypes and histopathological characteristics
The presence of the genes cagA (OR = 4.96, 95% CI 1.10–22.41), babA2 (OR = 2.78, 95% CI 1.06–7.30), and the combination of cagA/oipA genes (OR = 4.78, 95% CI 1.06–21.62) were found to increase the risk of developing acute gastric inflammation. In addition, we found that the genes cagA (OR = 2.19, 95% CI 1.06–4.52), iceA1 (OR = 3.13, 95% CI 1.20–8.16), babA2 (OR = 2.56, 95% CI 1.14–5.77), and the cagA/oipA combination (OR = 2.32, 95% CI 1.12–4.84) all increased the likelihood of having lymphoid follicular hyperplasia (see Table 4).
Finally, the odds of developing gastric intestinal metaplasia were considerably enhanced by the presence of the genes vacA (m1) (OR = 2.71, 95% CI 1.17–6.30) and vacA (s1m1) (OR = 2.33, 95% CI 1.03–5.24), while the odds of developing gastric atrophy were significantly decreased by the presence of iceA1 (OR = 0.33, 95% CI 0.12–0.91) (see Table 4).
Discussion
In this study, the prevalence of H. pylori infection was 58.7% when determined by histology and 62.7% when determined by PCR. Histology allows direct visualization of the bacteria and is recommended for primary diagnosis if upper endoscopy is required. PCR test offer comparable specificity and sensitivity to the histology test [24]. Previous studies conducted in Quito, Ecuador, found low prevalence rates of 40.2% and 42.4%, respectively [25, 26]. As in other studies, no gender-related differences were discovered. Moreover, our study did not find a link between H. pylori infection and low levels of education, in contrast to other studies that found such a correlation [27]. Importantly, we described a negative correlation between age and the prevalence of H. pylori; as a result, patients under the age of 40 had a higher frequency than those over the age of 50. This finding disagrees with a systematic review done in China that found that the prevalence increases with age [28]. This observation may be explained by the high rates of gastric atrophy and metaplasia also seen in our study, since these conditions reduce the stomach's bacterial burden due to the lack of sustenance [29]. Therefore, the early onset of gastric atrophy may account for the low incidence of H. pylori infection in elderly individuals.
Several studies have shown a link between H. pylori infection and either acute or chronic gastritis [30]. In the current investigation, we were able to confirm that patients who had both acute and chronic inflammation were significantly more likely to have H. pylori. (74.7% and 97.8%, respectively). Additionally, we identified that individuals over 50 years of age had higher rates of peptic ulcer, atrophy, and stomach metaplasia. This finding was consistent with earlier research done in Peru and China [31, 32]. It has been noted that intestinal metaplasia and a reduction in gastric secretion are related to the absence of H. pylori infection [33]. We confirmed that H. pylori infection had a protective effect against the development of gastric intestine metaplasia (OR 0.41; 95% CI: 0.23–0.75).
It is significant to note that MALT (mucosa-associated lymphoid tissue) lymphoma can develop as a result of the host's inflammatory immunological response to H. pylori infection. We found that lymphoid follicular hyperplasia was prevalent in this study at a frequency of 31.6%, which is consistent with other researchers' findings [34].
There is great geographic heterogeneity in the prevalence of H. pylori genotypes, which is linked to clinical manifestations that can be severe in some areas but less harmful or even non-aggressive in others [7]. A pathogenic strain's presence alone is insufficient to start a pathological process. For instance, several African cultures with a 100% prevalence of H. pylori infection and highly virulent strain (hspsafrica, hspwafrica, hpafrica2, hpneafrica) had low rates of stomach cancer. A condition referred to as " The African paradox" [35].
Due to their high virulence, the cagA and vacA genes are among the most studied. In our study, the cagA genotype, which is a marker of the existence and activity of the pathogenicity island (cagPAI), was uncommon (31.9%). The frequency of this gene varies greatly across the world between 60%—80% [36, 37]. We found a significant correlation between the cagA genotype and the emergence of acute gastric inflammation in this cohort (OR 4.96; 95% CI: 1.10—22.41). We also present evidence-linking cagA to stomach lymphoid follicular hyperplasia, which has the potential to develop into MALT lymphoma over time (OR 2.19; 95% CI: 1.06—4.52). Furthermore, numerous studies have shown a link between cagA and acid peptic disease, chronic atrophic gastritis, and stomach cancer [38, 39]. However, we did not find evidence of this relationship; we even found a protective effect of the presence of cagA gene and the development of gastric ulcer (OR 0.21; 95% CI: 0.04–0.98). This data might be related to the low prevalence found or the local strains' lower virulence. It is intriguing to learn that some H. pylori genes are apparently naturally disappearing from western populations, especially Cag-A positive strains, which are selectively eliminated because of their link to peptic ulcers [40].
In our research, the presence of the H. pylori vacA s1m1 genotype was 41.8%, which is quite comparable to the 42% reported by Shetty et al. in India [37]. Geographically, the m1 genotype is more common among the population of Africa and the m2 genotypes are equally distributed in Latin America and Europe [41]. The s1m1 genotype is crucial because of the large levels of toxin that this genotype secrets, which have been associated with serious lesions in the stomach. In this study, the development of gastric-intestinal metaplasia was linked to the vacA m1 and vacA s1m1 genotypes (OR 2.71, 95% CI: 1.17—6.30) (OR 2.33, 95% CI: 1.03—5.24). These findings are in line with research done in populations from Brazil and the Middle East, which links vacA s1 or m1 to the development of stomach cancer [38, 42].
iceA1 genotype has been linked to the onset of peptic ulcers due to the gene's ability to cause excessive production of the pro-inflammatory cytokine IL-8 [43]. When compared to studies from other nations, where its frequency is 53.3%, our study's prevalence of iceA1 (14.9%) is considerably low [36]. In the Brazilian population this gene was linked to the development of gastritis but not peptic ulcers [44]. In China and Egypt however, it was associated with peptic ulcers [15, 45]. In this research, we found that the iceA1 gene was associated with lymphoid follicular hyperplasia (OR 3.13; 95% CI: 1.20—8.16) rather than gastritis or peptic ulcer development.
The prevalence of the dupA gene was 48.9% in this study, which is comparable to the prevalence estimates in Belgium (43.7%) and South Africa (53.4%) [46]. Despite the dupA gene being suggested as a marker for peptic ulcers, our research, like that of other authors, was unable to validate this association [47].
Our study found a prevalence of babA2 of 70.2%, comparable to that of an Iranian study [48], but lower than that of Thailand (92%) [49]. In Western nations, but not in Asian nations, babA gene is linked to an increased risk of acid peptic illness [50]. Intriguingly, babA2 in our study showed a protective effect against the occurrence of gastric ulcers (OR 0.24; 95% CI: 0, 09–0, 67), but on the other hand, it was associated with the occurrence of acute inflammation (OR 2.78; 95% CI: 1.06—7.30) and lymphoid follicular hyperplasia (OR 2.56, 95% CI: 1.14—5.77). This discovery supports the observation made by Chen et al. [50].
Finally, our study revealed a high prevalence of the oipA gene (93.6%), similar to studies carried out in Venezuela (93.8%) and China (88.1%—100%) [23, 51]. The oipA genotype is significantly associated with an increased risk of acid peptic disease (OR = 3.97) and gastric cancer (OR = 2.43) [52, 53]. However, unlike several studies conducted internationally, we did not show this association.
The results of global genomic investigations are inconsistent and controversial. This study is another example of the genetic diversity of H. pylori observed by the different prevalences discovered. Which may be a reflection of demographic diversity, H. pylori strain-specific virulence factors, host genotype, and environmental factors such as diet [3].
Limitations
Due to the fact that the current study was conducted in a single medical facility, we cannot rule out the possibility of selection bias. To acquire data that may be extrapolated to the Ecuadorian population, it is also important to conduct studies with a larger population.
Technically speaking, the possibility of false negative findings should be a key factor to take into account. Factors including inaccurate biopsy taking, low bacterial DNA concentrations, and PCR failures might result in erroneous results. In this investigation, all procedures were carried out in accordance with defined handling and transport guidelines. The isolated DNA's quality and concentration were confirmed. Both positive and negative controls were used in the 16S rRNA-PCR (samples with and without H. pylori, as determined by histology and later confirmed by PCR). And, for genotyping, a specific band for each gene and non-amplification of the NTC (Non-template control) were the parameters used to validate the results.
Additionally, in line with the argument of the validation of our results, the frequencies we discovered are comparable to those reported by other study groups. However, H. pylori's genetic diversity must be taken into consideration.
Conclusion
This study presents the genotypic prevalence of H. pylori existing in Ecuadorian patients. The histological presence of acute gastric inflammation and follicular hyperplasia are associated to the genes cagA, babA2, iceA1 and cagA/oipA. The presence of vacA (m1) and vacA (s1m1) increased the risk of intestinal metaplasia. Finally, cagA/vacA (s1m1) is related with duodenal ulcer. Our findings suggest that the clinical course of the disease is influenced by the host's immune response, the presence of H. pylori virulence genes, and environmental variables.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- H. pylori :
-
Helicobacter pylori
- CagA:
-
Cytotoxin associated with gene A
- VacA:
-
Vacuolating cytotoxin linked to gene A
- BabA:
-
Blood group antigen-binding adhesin
- iceA :
-
A gene induced by contact with the epithelium
- PCR:
-
Polymerase chain reaction
- OR:
-
Odds ratios
- CI:
-
Confidence intervals
- MALT:
-
Mucosa-associated lymphoid tissue
- cagPAI:
-
Cag pathogenicity island
References
Hooi JKY, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9. https://doi.org/10.1053/j.gastro.2017.04.022.
Curado MP, de Oliveira MM, de Araújo Fagundes M. Prevalence of Helicobacter pylori infection in Latin America and the Caribbean populations: a systematic review and meta-analysis. Cancer Epidemiol. 2019;60:141–8.
Amieva M, Peek RM. Pathobiology of Helicobacter pylori-induced gastric cancer. Gastroenterology. 2016;150(1):64–78. https://doi.org/10.1053/J.GASTRO.2015.09.004.
Abadi AT, Ierardi E, Lee YY. Why do we still have Helicobacter Pylori in our Stomachs. Malays J Med Sci. 2015;22(5):70–5.
Hussain SA, Hamid S. Helicobacter pylori in humans: where are we now? Adv Biomed Res. 2014;3(1):63. https://doi.org/10.4103/2277-9175.125844.
Falush D, et al. Traces of human migrations in Helicobacter pylori populations. Science (80- ). 2003;299(5612):1582–5. https://doi.org/10.1126/science.1080857.
Sharndama HC, Mba IE. Helicobacter pylori: an up-to-date overview on the virulence and pathogenesis mechanisms. Braz J Microbiol. 2022;53(1):33–50. https://doi.org/10.1007/S42770-021-00675-0.
Hayashi Y, et al. CagA mediates epigenetic regulation to attenuate let-7 expression in Helicobacter pylori-related carcinogenesis. Gut. 2013;62(11):1536–46. https://doi.org/10.1136/gutjnl-2011-301625.
Takahashi-Kanemitsu A, Knight CT, Hatakeyama M. Molecular anatomy and pathogenic actions of Helicobacter pylori CagA that underpin gastric carcinogenesis. Cell Mol Immunol. 2020;17(1):50–63. https://doi.org/10.1038/S41423-019-0339-5.
Kim IJ, Blanke SR. Remodeling the host environment: modulation of the gastric epithelium by the Helicobacter pylori vacuolating toxin (VacA). Front Cell Infect Microbiol. 2012;2:37. https://doi.org/10.3389/FCIMB.2012.00037.
Ricci. “Relationship between VacA toxin and host cell autophagy in Helicobacter pylori infection of the human stomach: a few answers, many questions,.” Toxins (Basel). 2016;8(7):203.
Roy R, Jonniya NA, Sk MF, Kar P. Comparative structural dynamics of isoforms of Helicobacter pylori adhesin baba bound to lewis b hexasaccharide via multiple replica molecular dynamics simulations. Front Mol Biosci. 2022;9:852895.
Ansari S, Yamaoka Y. Helicobacter pylori BabA in adaptation for gastric colonization. World J Gastroenterol. 2017;23(23):4158–69. https://doi.org/10.3748/wjg.v23.i23.4158.
Abadi ATB, Perez-Perez G. Role of dupA in virulence of Helicobacter pylori. World J Gastroenterol. 2016;22(46):10118–23. https://doi.org/10.3748/wjg.v22.i46.10118.
Abu-Taleb AMF, et al. Prevalence of Helicobacter pylori cagA and iceA genes and their association with gastrointestinal diseases. Int J Microbiol. 2018;2018:4809093. https://doi.org/10.1155/2018/4809093.
Matsuo Y, Kido Y, Yamaoka Y. Helicobacter pylori outer membrane protein-related pathogenesis. Toxins (Basel). 2017;9(3):101. https://doi.org/10.3390/TOXINS9030101.
Carrera S, Llumiquinga R. Registro Estadístico de Defunciones Generales INEC JUNIO 2020. Instituto Nacional de Estadística y Censos. 2020. https://www.ecuadorencifras.gob.ec. Accessed 14 June 2022.
Dixon MF, et al. Classification and grading of gastritis. the updated Sydney system. international workshop on the histopathology of gastritis, Houston 1994. Am J Surg Pathol. 1996;20(10):1161–81. https://doi.org/10.1097/00000478-199610000-00001.
Valenzuela S. Estudio epidemiológico en la población ecuatoriana de los factores de riesgo asociados a la infección con Helicobacter pylori. Repositorio Digital USFQ. 2016. https://repositorio.usfq.edu.ec/handle/23000/5905. Accessed 20 May 2020.
Chattopadhyay S, et al. Multiplex PCR assay for rapid detection and genotyping of Helicobacter pylori directly from biopsy specimens. J Clin Microbiol. 2004;42(6):2821–4. https://doi.org/10.1128/JCM.42.6.2821-2824.2004.
Atherton JC, Cao P, Peek RM, Tummuru MKR, Blaser MJ, Cover TL. Mosaicism in vacuolating cytotoxin alleles of helicobacter pylori. association of specific vacA types with cytotoxin production and peptic ulceration. J Biol Chem. 1995;270(30):17771–7. https://doi.org/10.1074/jbc.270.30.17771.
Delgado F. Comparación de genes de virulencia entre Helicobacter pylori y otras especies de Helicobacter en pacientes Ecuatorianos. Repositorio Digital USFQ. 2018. https://repositorio.usfq.edu.ec/handle/23000/7987. Accessed 20 May 2020.
Torres K, Valderrama E, Sayegh M, Ramírez JL, Chiurillo MA. Study of the oipA genetic diversity and EPIYA motif patterns in cagA-positive Helicobacter pylori strains from Venezuelan patients with chronic gastritis. Microb Pathog. 2014;76:26–32. https://doi.org/10.1016/j.micpath.2014.09.006.
Bordin DS, Voynovan IN, Andreev DN, Maev IV. Current Helicobacter pylori diagnostics. Diagnostics. 2021;11(8):1458. https://doi.org/10.3390/DIAGNOSTICS11081458.
Reyes Chacón J. A., et al. “Susceptibilidad antibiótica de Helicobacter pylori: un estudio de prevalencia en pacientes con dispepsia en Quito-Ecuador,.” Rev Colomb Gastroenterol. 2017;32(4):305.
Vázquez P. Prevalencia por infección por Helicobacter pylori y asociación con patalogías gástricas en pacientes adultos de chequeo ejecutivo desde enero del 2010 hasta septiembre del 2012 del Hospital Metropolitano de Quito-Ecuador. 2013. https://repositorio.usfq.edu.ec/handle/23000/1503. Accessed 22 Oct 2022.
Bastos J, et al. Sociodemographic determinants of prevalence and incidence of Helicobacter pylori infection in Portuguese adults. Helicobacter. 2013;18(6):413–22. https://doi.org/10.1111/HEL.12061.
Ren S, et al. Prevalence of Helicobacter pylori infection in China: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37(3):464–70. https://doi.org/10.1111/JGH.15751.
Konturek PC, Kania J, Konturek JW, Nikiforuk A, Konturek SJ, Hahn EGH. pylori infection, atrophic gastritis, cytokines, gastrin, COX-2, PPAR gamma and impaired apoptosis in gastric carcinogenesis. Med Sci Monit. 2003;9(7):SR53–66.
Azer S, Akhondi H. Gastritis. StatPearls. 2022. https://www.ncbi.nlm.nih.gov/books/NBK544250/. Accessed 17 June 2022.
Montes P, Salazar S, Monge E. Cambios en la Epidemiologia de la Úlcera Péptica y su Relación con la Infección con Helicobacter Pylori. Hospital Daniel Carrion 2000–2005. 2007;27(4):382–388.
Lin S, et al. Association of dietary patterns and endoscopic gastric mucosal atrophy in an adult Chinese population. Sci Rep. 2019;9(1):16567. https://doi.org/10.1038/S41598-019-52951-7.
Craanen ME, Blok P, Dekker W, Ferwerda J, Tytgat GNJ. Subtypes of intestinal metaplasia and Helicobacter pylori. Gut. 1992;33(5):597–600. https://doi.org/10.1136/GUT.33.5.597.
Bashiri H, Esmaeilzadeh A, Vossoughinia H, Ghaffarzadegan K, Raziei HR, Bozorgomid A. Association between gastric lymphoid follicles (Precursor of malt lymphomas) and h. pylori infection at a referral hospital in Iran. Clin Exp Gastroenterol. 2019;12:409–13. https://doi.org/10.2147/CEG.S224823.
Holcombe C. Helicobacter pylori: the African enigma. Gut. 1992;33(4):429–31. https://doi.org/10.1136/GUT.33.4.429.
Feliciano O, et al. Prevalence of Helicobacter pylori vacA, cagA, and iceA Genotypes in Cuban patients with upper gastrointestinal diseases. Biomed Res Int. 2015;2015:753710.
Shetty V, Lingadakai R, Pai GC, Ballal M. Profile of Helicobacter pylori cagA & vacA genotypes and its association with the spectrum of gastroduodenal disease. Indian J Med Microbiol. 2021;39(4):495–9. https://doi.org/10.1016/j.ijmmb.2021.06.001.
Matos JI, De Sousa HAC, Marcos-Pinto R, Dinis-Ribeiro M. Helicobacter pylori CagA and VacA genotypes and gastric phenotype: a meta-analysis. Eur J Gastroenterol Hepatol. 2013;25(12):1431–41. https://doi.org/10.1097/MEG.0b013e328364b53e.
Park JY, Forman D, Waskito LA, Yamaoka Y, Crabtree JE. Epidemiology of Helicobacter pylori and CagA-positive infections and global variations in gastric cancer. Toxins (Basel). 2018;10(4):163. https://doi.org/10.3390/TOXINS10040163.
Konráðsson A, Andersen L, Oddsson E, Guðjónsson H, Thornjóðleifsson B. Prevalence of Helicobacter pylori and Cag-A strains in patients with duodenal ulcer in Iceland. Laeknabladid. 2003;89(7–8):595–7.
Ghose C, Perez-Perez GI, Van Doorn LJ, Domínguez-Bello MG, Blaser MJ. High frequency of gastric colonization with multiple Helicobacter pylori strains in Venezuelan subjects. J Clin Microbiol. 2005;43(6):2635–41. https://doi.org/10.1128/JCM.43.6.2635-2641.2005.
Pereira WN, et al. Association among H. pylori virulence markers dupA, cagA and vacAin Brazilian patients. J Venom Anim Toxins Incl Trop Dis. 2014;20(1):1. https://doi.org/10.1186/1678-9199-20-1/TABLES/2.
Xu Q, Blaser MJ. Promoters of the CATG-specific methyltransferase gene hpyIM differ between iceA1 and iceA2 Helicobacter pylori strains. J Bacteriol. 2001;183(13):3875–84. https://doi.org/10.1128/JB.183.13.3875-3884.2001.
Gatti LL, et al. Prevalence of Helicobacter pylori cagA, iceA and babA2 alleles in Brazilian patients with upper gastrointestinal diseases. Acta Trop. 2006;100(3):232–40. https://doi.org/10.1016/J.ACTATROPICA.2006.08.014.
Huang X, Deng Z, Zhang Q, Li W, Wang B, Li M. Relationship between the iceA gene of Helicobacter pylori and clinical outcomes. Ther Clin Risk Manag. 2016;12:1085–92. https://doi.org/10.2147/TCRM.S107991.
Idowu A, et al. Detection of Helicobacter pylori and its virulence genes (cagA, dupA, and vacA) among patients with gastroduodenal diseases in Chris Hani Baragwanath Academic Hospital, South Africa. BMC Gastroenterol. 2019;19(1):73. https://doi.org/10.1186/S12876-019-0986-0.
Argent R. H., Burette A, Miendje Deyi V. Y., Atherton J. C. “The presence of dupA in Helicobacter pylori is not significantly associated with duodenal ulceration in Belgium, South Africa, China, or North America,.” Clin Infect Dis. 2007;45(9):1204–6.
Dabiri H, et al. Prevalence of Helicobacter pylori vacA, cagA, cagE, oipA, iceA, babA2 and babB genotypes in Iranian dyspeptic patients. Microb Pathog. 2017;105:226–30. https://doi.org/10.1016/J.MICPATH.2017.02.018.
Chomvarin C, et al. Prevalence of Helicobacter pylori vacA, cagA, cagE, iceA and babA2 genotypes in Thai dyspeptic patients. Int J Infect Dis. 2008;12(1):30–6. https://doi.org/10.1016/J.IJID.2007.03.012.
Chen MY, He CY, Meng X, Yuan Y. Association of Helicobacter pylori babA2 with peptic ulcer disease and gastric cancer. World J Gastroenterol. 2013;19(26):4242–51. https://doi.org/10.3748/wjg.v19.i26.4242.
Zhao Q, et al. Prevalence of Helicobacter pylori babA, oipA, sabA, and homB genes in isolates from Chinese patients with different gastroduodenal diseases. Med Microbiol Immunol. 2020;209(5):565–77. https://doi.org/10.1007/S00430-020-00666-2.
Yamaoka Y, Kikuchi S, ElZimaity HMT, Gutierrez O, Osato MS, Graham DY. Importance of Helicobacter pylori oipA in clinical presentation, gastric inflammation, and mucosal interleukin 8 production. Gastroenterology. 2002;123(2):414–24. https://doi.org/10.1053/GAST.2002.34781.
Liu J, He C, Chen M, Wang Z, Xing C, Yuan Y. Association of presence/absence and on/off patterns of Helicobacter pylori oipA gene with peptic ulcer disease and gastric cancer risks: a meta-analysis. BMC Infect Dis. 2013;13:555. https://doi.org/10.1186/1471-2334-13-555.
Acknowledgements
To the Central University of Ecuador for its financial support. To Dr. Manuel Baldeón for his expertise and advice.
Funding
This work was supported by Central University of Ecuador.
Author information
Authors and Affiliations
Contributions
SBF: Conceptualization. Formal analysis. Writing-Original Draft. Writing-Reviewing and Editing. MSP: Investigation. Formal analysis. Writing-Original Draft. Writing-Reviewing and Editing. YVA: Investigation. Project administration. Formal analysis. Writing-Original Draft. RBO: Conceptualization. Writing-Reviewing and Editing. LBR: Supervision. Writing-Original Draft. Writing-Reviewing and Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee for Research in Human Beings of the Central University of Ecuador (February 2020; 0121-SEISH-UCE-20) and the National Directorate of Health Intelligence of the Ministry of Public Health of Ecuador (March 2020; MSP-DIS 2020–0135-O). An informed consent was obtained from the participants. Legally Authorized Representatives of illiterate participants provided informed consent for the study. In this case, the details of the study were explained verbally in the company of the legally authorized representative of the illiterate participants and the participant's fingerprint was placed on the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bustos-Fraga, S., Salinas-Pinta, M., Vicuña-Almeida, Y. et al. Prevalence of Helicobacter pylori genotypes: cagA, vacA (m1), vacA (s1), babA2, dupA, iceA1, oipA and their association with gastrointestinal diseases. A cross-sectional study in Quito-Ecuador. BMC Gastroenterol 23, 197 (2023). https://doi.org/10.1186/s12876-023-02838-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02838-9