Abstract
Background
We aimed to address the shortage of evidence regarding the safety of the local resection approach by comparing long-term oncological outcomes between patients managed by local resection and those who underwent radical resection.
Methods
This was a propensity-score matched cohort analysis study that included patients of all ages diagnosed with locally advanced rectal cancer (LARC) who had received neoadjuvant chemoradiotherapy (nCRT) at the Fujian Medical University Union Hospital and Fujian Medical University Affiliated Zhangzhou Hospital, China, between Jan 10, 2011, to Dec 28, 2021. Partial patients with a significant downstage of the tumor were offered management with the local resection approach, and most of the rest were offered radical resection if eligible.
Findings
One thousand six hundred ninety-three patients underwent radical resection after nCRT, and another 60 patients performed local resection. The median follow-up times were 44.0 months (interquartile range = 4–107 months). After propensity-core matching (PSM), in the Kaplan–Meier curves, local resection (n = 56) or radical resection (n = 211) was not significantly associated with 1-, 3-, and 5-year cumulative incidence of overall survival (OS) (HR = 1.103, 95% CI: 0.372 ~ 3.266), disease-free survival (DFS) ((HR = 0.972, 95% CI: 0.401 ~ 2.359), local recurrence (HR = 1.044, 95% CI: 0.225 ~ 4.847), and distant metastasis (HR = 0.818, 95% CI: 0.280 ~ 2.387) (all log-rank P > 0.05). Similarly, multivariate Cox regression analysis indicates that local excision still was not an independent risk factor for OS (HR = 0.863, 95% CI: 0.267 ~ 2.785, P = 0.805) and DFS (HR = 0.885, 95% CI: 0.353 ~ 2.215, p = 0.794).
Conclusion
Local resection can be a management option in selected patients with middle-low rectal cancer after nCRT for LARC and without loss of oncological safety at five years.
Similar content being viewed by others
Introduction
In recent years, neoadjuvant chemoradiotherapy (nCRT) combined with total mesorectal resection (TME) has become the standard treatment model for locally advanced rectal cancer (LARC) [1]. LARC after nCRT may have the potential to downstage the primary tumor and even sometimes induce a pathological complete response (pCR), which occurs in 10 ~ 30% of patients [2,3,4], which results in lower rates of local recurrence and increased survival rates [5]. As early as 2004, Habr-Gamma reported that for patients in clinical complete response (cCR) after nCRT for LARC, the “watch-and-wait (W&W)” strategy of rectum-preservation with close follow-up and salvage surgery, if necessary, could be implemented to safeguard oncologic efficacy and save costs for health-care systems [6]. On the other hand, radical resection usually requires the creation of a temporary or permanent stoma, negatively impacting patients' quality of life (QoL). But pCR and cCR might not be equivalent, at a median 24 month follow-up, tumor regrowth was found in 24.2% of patients who underwent W&W [7]. As growing interest has developed in rectum-sparing strategies, therefore, it has been proposed that those who are cCR or near-cCR undergo local resection as a rectum-preserving strategy and decide whether to preserve the rectum according to the post-local resection ypT stage combined with other factors to avoid non-pCR patients from entering negative W&W [7].
Several studies described the effect of local resection in patients who significantly downstage to nCRT for LARC. Results shown that rectum preservation could be achieved in 64.8 to 90.0% of patients with acceptable local control [8,9,10]. While the findings of these studies were encouraging, the evidence of the efficacy of these approaches was still limited. Most of the studies were small, had a single-center design, differed in patients' selection and definition of clinical response and long-term oncological outcome data were scarce.
The reasons, including but not limited to ethical, patient risk, and benefit circumstances that make it challenging to develop a randomized controlled trial for local resection versus radical resection in clinical practice. There for, based on a retrospective cohort analysis of patients from two sizeable colorectal consultation centers and used a propensity-core matching (PSM) analysis to reduce the bias in patient selection between two groups, we aimed to compare long-term oncological outcomes between patients managed by local resection with those who had underwent radical resection.
Methods
Study design and participants
This study was a PSM and observational analysis of clinical practice across two colorectal cancer treatment centers in China [11]. We retrospectively collected information for 1911 patients with LARC after nCRT, between Jan 10, 2011, to Dec 28, 2021, from patients treated at the Fujian Medical University Union Hospital and Fujian Medical University Affiliated Zhangzhou Hospital, China.
Inclusion and exclusion criteria
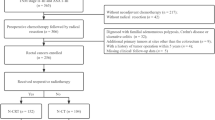
The inclusion criteria were as follows: ① pathologically confirmed rectal cancer; ② tumor response was re-evaluated after the last nCRT and the clinical stage was determined by two imaging experts as yc0 ~ III stage, which was determined according to the American Joint Committee on Cancer (AJCC) 8th edition colorectal cancer staging criteria; ③ completed nCRT combined with radical resection or local resection; ④ distance to the anal verge (DTAV) within 15 cm; ⑤ complete clinicopathological features and follow-up data, signed informed consent form of surgery [9, 10]. The exclusion criteria were as follows: ① distant organ metastasis before and after nCRT; ② death within 60 days after surgery; ③ first diagnosis combined with malignant tumors from another organ [9, 10] (Fig. 1).
Treatment
All patients received concurrent radiotherapy and concurrent oral fluorouracil-based chemotherapy during radiotherapy. The long-course radiotherapy dose was 45.0∼50.4 Gy 25∼28 times, and the short-course radiotherapy dose was 25 Gy 5 times. The neoadjuvant chemotherapy regimen was mFolFox6 (total fluorouracil 2600 mg/m2, calcium folinate 400 mg/m2, oxaliplatin 85 mg/m2) or Xelox (capecitabine 1000 mg/m2 bid, oxaliplatin 130 mg/m2). All patients underwent magnetic resonance imaging (MRI) re-evaluated within 8–12 weeks after the end of radiotherapy. Those who were regarded by the multidisciplinary team (MDT) to have: ① re-evaluated MRI suggests a significant downstage of the tumor (ycT0 ~ 2); ② tumor invading < 30% of the intestinal circumference; ③ tumor size < 3 cm; ④ preoperative negative circumferential resection margin (CRM) and extramural venous invasion (EMVI); ⑤Tumor within 10 cm distance to anal verge; ⑥ high-middle differentiation; ⑦ no evidence of lymph node enlargement on imaging before operative, were eligible for local resection and who meet the diagnostic criteria and strongly want to preserve the anus has fully explained the disease, explained the surgical method, and local resection was performed after obtaining informed consent, whereas most of the rest patients were offered radical resection if eligible—referred to as the standard pathway. Local resection was usually performed using transanal endoscopic microsurgery (TEM) surgery, which consisted of full-thickness resection of the tumor with a margin of 2 mm or more. When histological examination revealed insufficient pathological downstaging (ypT2 ~ 3), patients were advised to underwent complete radical resection within 2 to 3 weeks after local resection unless the patient clearly knows the risks and refuses radical surgery.
Follow-up
For patients who underwent radical resection, follow-up was following NCCN guidelines [12]. For patients managed by local resection, a more intensive follow-up protocol was used, consisting of the outpatient digital rectal examination, MRI (every 4 ~ 6 months in the first 2 years), examination under anesthesia or endoscopy, CT scan of the chest, abdomen, and pelvis, and at least two CEA measurements in the first 2 years, which was intended for early detection of possible local recurrence and/or distant metastasis (DM). For patients managed by radical resection, every three months the first three years, then every six months for the next two years, and annually after that. Physical examination, serum carcinoembryonic antigen (CEA) level, chest X-ray or computed tomography (CT), and abdominopelvic MRI or CT scans were performed at each follow-up visit. Colonoscopy was conducted annually after surgery. Positron emission tomography was performed when needed.
We calculated prognosis as the time from day 1 of concurrent surgery. local recurrence to the first recurrence at local pelvic or rectal wall, DM to the date of first distant metastasis; disease-free survival (DFS) to the first relapse at any site, death from any cause, or the date of the last follow-up visit, whichever occurred first; and overall survival (OS) to death from any cause. Followed up with patients until June 2022.
Outcomes
The primary endpoint was to evaluate the prognostic efficacy after local excision, characterized by DFS and OS. The secondary endpoint was to evaluate the impact on local recurrence and DM.
Statistical analysis
PSM analysis is a method used to reduce the bias in patient selection between two groups [11]. This approach attempts to construct a randomized experiment-like situation in a retrospective observational study, in which the selection bias is minimized as much as possible. We performed a PSM analysis to decrease the heterogeneity between the local resection and radical resection groups. The propensity scores of each patient were estimated using logistic regression. The following variables were included in the regression model: age, sex, ycT stage, ycN stage, ycTNM stage, radiation therapy courses, tumor regression grade (TRG), histopathology, DTAV, carcinoembryonic antigen (CEA), and carbohydrate antigen 19–9 (CA19-9). Each patient in the local resection group was matched 1:4 with a patient in the radical resection group (Caliper = 0.2). The PSM analysis was conducted using SPSS 26 (IBM SPSS Statistics, Chicago, IL, USA).
Before and after PSM, clinicopathological characteristics were compared between the two groups. The chi-Square or Fisher's exact test was used to analyze the categorical variables, whereas the rank-sum test was used for ranked data. Continuous data were compared using the student t test (data were shown as mean ± standard deviation). The survival outcomes were analyzed and compared using the Kaplan–Meier method. Multivariate analysis was performed using Cox proportional hazards regression (HR). A p-value < 0.05 was recognized as statistically significant.
Results
One thousand six hundred ninety-three eligible LARC patients were enrolled to the study, 1633 of them underwent radical resection after nCRT (i.e., the standard route), and another 60 patients were performed local resection. Before PSM, there were 4 of the 60 patients with local resection who showed pathology of ypT3 after local resection, all of whom underwent additional radical resection within 2–3 weeks according to the established procedural requirements but were still included in the local resection group group in order to truly reflect the true outcome of the local resection group and to ensure the reliability of the statistical results. 4 patients died during follow-up, 2 patients developed local recurrence of the rectal wall and underwent salvage radical resection, and 4 patients developed DM.
Patient characteristics
Baseline characteristics were shown in Table 1. Before PSM, compared with all patients who received radical resection, patients managed by local resection had tumors that were at an earlier ycT stage, ycN stage, and ycTNM stage, were less likely to had lower TRG, DTAV was lower (all p < 0.05). Radiotherapy doses received were clinically equivalent between treatment groups (Table 1 before PSM).
We derived paired cohorts for local resection versus radical resection (60 and 211 patients, respectively). These cohorts were well matched for key confoundersie, sex, age, ycT stage, ycN stage, ycTNM stage, TRG, histopathology, radiation therapy, CEA, CA19-9 and DTAV and were all comparable. Among locally resection patients, 87.5% (49/56) in yc0 ~ I stage, 5.4% (3/56) in yc II stage and 7.1% (4/56) in yc III stage, with DTAV less than 10 cm in all patients (Table 1 after PSM).
After PSM, Among locally resection patients, 66.1% (37/56) in ypT0, 7.1% (4/56) in ypT1, 19.6% (11/56) in ypT2 and 7.1% (4/56) in ypT3. Pathological assessment of lymph node metastasis status could not be obtained in locally resected patients and was determined to be Nx postoperatively. Patients who underwent radical resection had negative circumferential margins and complete resection of the tumor was obtained. During follow-up, there was no significant difference in the probability of local recurrence, DM, DFS, or death between the two groups (P > 0.05) (Table 2).
Survival outcomes
The median follow-up times were 44.0 months (interquartile range = 4 ~ 107 months). In the Kaplan–Meier curves, after PSM, local resection or radical resection was not significantly associated with 1-, 3-, and 5-year cumulative incidence of OS (HR = 1.103, 95% CI: 0.372 ~ 3.266), DFS (HR = 0.972, 95% CI: 0.401 ~ 2.359), local recurrence (HR = 1.044, 95% CI: 0.225 ~ 4.847), and DM (HR = 0.818, 95% CI: 0.280 ~ 2.387) (all log-rank P > 0.05) (Fig. 2A ~D).
Independent prognostic factors
We tested whether local resection was inferior to radical resection in the time-varying Cox model. Before PAM, the multivariate Cox regression analysis of OS and DFS were shown in Table 3, the sex, ycTNM stage, CA19-9, TRG, and DTAV has an independent effect on both OS and DFS. However, local resection was not an independent risk factor for OS (HR = 1.291, 95% CI: 0.466 ~ 3.547, p = 0.623) and DFS (HR = 1.189, 95% CI: 0.517 ~ 2.733, p = 0.683) noted not significantly differences.
After PSM, only ycN stage (HR = 9.600, 95% CI: 3.938 ~ 24.405, p < 0.001) and DTAV (HR = 0.344, 95% CI: 0.137 ~ 0.866, p = 0.023) has an independent predictor of OS. Otherwise, only ycN stage (HR = 2.568, 95% CI: 1.020 ~ 6.466, p = 0.045) and TRG (HR = 1.729, 95% CI: 1.148 ~ 2.604, p = 0.009) has an independent predictor of DFS. Similarly, local excision still was not an independent risk factor for OS (HR = 0.863, 95% CI: 0.267 ~ 2.785, P = 0.805) and DFS (HR = 0.885, 95% CI: 0.353 ~ 2.215, p = 0.794) (Table 4).
Owing to the potential for statistical bias due to multicollinearity, we considered that ypT and ycT staging could not be tested in the same regression model. We further included postoperative pathological outcomes in the Cox regression to verify the impact on long-term prognosis. We found that, like the previous results, the independent influences factors for OS remain to ycN stage and DTAV, for DFS remain to ycN stage and TRG in the multivariate Cox regression (all P < 0.05). Neither local resection nor ypT staging constituted an independent influence (Table 5).
Discussion
In this study, we enrolled LARC patients who underwent radical resection or local resection were and PSM analysis was used to evaluate the effect of local resection on prognosis. We demonstrated that local resection was not an independent risk factor for OS and DFS after nCRT for low-middle LARC. Specifically, compared with radical resection, the oncological safety of local resection, with no significant difference in local recurrence, DM, DFS, and OS between the two groups with significant downstage of the tumor.
In the 1980s, as the report of 'Holy plane’ in rectal cancer surgery elaborated on a resection technique based on the embryologic development of the hindgut, which has tremendously improved oncologic outcomes [13]. However, these improvements come with poor QoL, especially in patients with low-middle rectal cancer [14, 15]. Organ preservation is a new concept for LARC, which HabrGama introduced in 2004.9 [6]. Similar findings with a similar therapeutic approach demonstrating reproducibility [16,17,18]. However, it is a lack of reliable preoperative criteria to determine whether attain cCR accurately [17]. A systemic review analysis that included 682 patients on the oncologic and survival outcomes in the W&W approach demonstrated that the 3-year cumulative risk of local regrowth was 21.6% (95% CI: 16.0 ~ 27.8); in addition, salvage surgery was performed in 88% of patients, the long-term safety of this strategy remains to be validated [19]. There for, local resection of rectal cancer can be another option for organ preservation. The advantage would be histological confirmation of whether obtain pCR. TEM surgery could be used to accurately assess pathological response in case of a complete clinical response after nCRT [8]. A multicenter, randomized trial evaluated the long-term oncological of TEM in early distal rectal cancer, the actuarial 5-year local recurrence rate was 7.7%, with 5-year DFS and OS rates of 81.6% and 82.8%, respectively, which was not difference from that in radical resection group and with improved emotional well-being (mean score at follow-up = 86.9%, 95% CI: 79.2 ~ 94.7; P = 0.001) [16].
In our study, there were no difference between the local resection and radical resection groups in 5-year OS, DFS, local recurrence, and DM (all log-rank p > 0.05). Similar results were confirmed in other studies, the GRECCAR2 was the first multicenter, randomised trial to compare local resection with radical resection in downstage low rectal cancer. Encouraging oncological results were noted at 5 years' follow-up in 5-year local recurrence (7% vs. 7%, HR = 0.71, 95% CI 0.19 ~ 2.58, p = 0.60), DM (18% vs. 19%, HR = 0.86, 95% CI 0.36 ~ 2.06, p = 0.73), OS (84% vs. 82%, HR = 0.92, 95% CI 0.38 ~ 2.22, p = 0.85), DFS (70% vs. 72%, HR = 0.87, 95% CI 0.44 ~ 1.72, p = 0.68) respectively, providing no evidence of difference in oncological outcomes between local resection and radical resection [10].
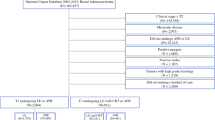
As the interest in local resection for rectal cancer increases, the accurate preoperative evaluation is extremely important, especially for lymph node metastasis status must be considered. A study utilized a nationwide cancer registry to establish incidence and predictors of nodal metastasis in early pathologic T-stage rectal cancers. The results were surprising, after receiving nCRT, LN positivity rates were 8.6% for ypT0, 12.9% for ypT1, and 21.4% for ypT2 tumors [20]. Indicated that the risk of LN metastasis increases with a higher path T stage, these findings must be carefully deliberated. Accordingly, a closer 3-year follow-up plan should be established and strictly enforced for local resection patients. Research has shown that MDT discussion contributes to improving the accuracy of MRI for the diagnosis of preoperative N stage was significantly higher than those without MDT (56.2% vs. 42.1%, P = 0.021), which was in favor of choosing a preferable therapy strategy [21]. Since pathologic examination of lymph node metastatic status in local resection patients will never be available, accurate preoperative evaluation as a suitable candidate for this procedure will affect the long-term prognosis of the patient, and we strongly recommend that all candidates initiate MDT discussions followed by decision making. In this study, 4 patients whose reassessment after nCRT was still highly suspicious of lymph node metastasis and rated as ycIII stage subjects underwent local resection and were required to be fully informed of the risks and offered an alternative radical resection choice before receiving this treatment.
Our study had several limitations. First, in China, there is significant heterogeneity in the occurrence of cancer and probability of death between different areas. Compared to other areas, colorectal cancer is more prevalent in the eastern area [22]. Data for this study were obtained at two large colorectal consultation centers in the eastern area of China, and characteristics may vary in other areas. Second, this study was based on a retrospective cohort analysis with some selection bias; patients with incomplete clinical data were excluded, and the probability of OS and DFS may be overestimated or underestimated. Third, there were inconsistencies in the doses of radiotherapy for patients in this study, but it has been suggested that preoperative short-course radiotherapy can also achieve excellent local control and favorable survival rates [23], and the effect of different radiotherapy doses can be effectively controlled in this study by using the baseline staging re-evaluated by MRI. Finally, post-treatment functional data were absent. In an Italian series of 46 patients managed by local resection, the data supported the hypothesis that post-treatment QoL and bowel function were better in patients managed by local resection than in those with radical resection [24]. This finding needs to be replicated in more extensive series.
Our study has several strengths. First, this was a large, reported cohort to be assessed for outcomes after local resection for LARC and the median follow-up times were 44.0 months (4–107 months). Second, this cohort represented clinical practice rather than specialist institutional practice. Third, as assessment of oncological safety requires examination of survival outcomes, comparator groups need to be matched for confounding factors, as done in our matched analysis, which was still incompletely addressed by previously randomized controls [8,9,10].
In conclusion, our study shown that local resection after nCRT for LARC was found to be safe. Local resection can be proposed in selected patients with middle-low rectal cancer with a significant downstage after nCRT and was not an independent risk factor for OS and DFS after nCRT for LARC. Preoperative MDT discussion and detailed evaluation are recommended for patients who are about to undergo local resection, and a close postoperative follow-up program is strictly enforced. A more extensive cohort study is warranted to validate the prognostic role of local resection for LARC after nCRT.
Availability of data and materials
All data obtained or analyzed during this work are included within the article.
References
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, et al. Rectal Cancer, Version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(7):874–901. https://doi.org/10.6004/jnccn.2018.0061.
Lorimer PD, Motz BM, Kirks RC, Boselli DM, Walsh KK, Prabhu RS, et al. Pathologic complete response rates after neoadjuvant treatment in rectal cancer: an analysis of the national cancer database. Ann Surg Oncol. 2017;24(8):2095–103. https://doi.org/10.1245/s10434-017-5873-8.
Beddy D, Hyland JM, Winter DC, Lim C, White A, Moriarty M, et al. A simplified tumor regression grade correlates with survival in locally advanced rectal carcinoma treated with neoadjuvant chemoradiotherapy. Ann surg oncol. 2008;15(12):3471–7. https://doi.org/10.1245/s10434-008-0149-y.
Mignanelli ED, de Campos-Lobato LF, Campos-Lobato LF, Stocchi L, Lavery IC, Dietz DW. Downstaging after chemoradiotherapy for locally advanced rectal cancer: is there more (tumor) than meets the eye? Dis colon rectum. 2010;53(3):251–6. https://doi.org/10.1007/DCR.0b013e3181bcd3cc.
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. New engl j med. 2001;345(9):638–46. https://doi.org/10.1056/NEJMoa010580.
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U, Silva e Sousa AH, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann surg. 2004;240(4):711–7. https://doi.org/10.1097/01.sla.0000141194.27992.32. (discussion 7-8).
Marchegiani F, Palatucci V, Capelli G, Guerrieri M, Belluco C, Rega D, et al. Rectal sparing approach after neoadjuvant therapy in patients with rectal cancer: the preliminary results of the ReSARCh trial. Ann Surg Oncol. 2022;29(3):1880–9. https://doi.org/10.1245/s10434-021-11121-8.
Bach SP, Gilbert A, Brock K, Korsgen S, Geh I, Hill J, et al. Radical surgery versus organ preservation via short-course radiotherapy followed by transanal endoscopic microsurgery for early-stage rectal cancer (TREC): a randomised, open-label feasibility study. Lancet Gastroenterol Hepatol. 2021;6(2):92–105. https://doi.org/10.1016/s2468-1253(20)30333-2.
Rullier E, Rouanet P, Tuech J-J, Valverde A, Lelong B, Rivoire M, et al. Organ preservation for rectal cancer (GRECCAR 2): a prospective, randomised, open-label, multicentre, phase 3 trial. The Lancet. 2017;390(10093):469–79. https://doi.org/10.1016/s0140-6736(17)31056-5.
Rullier E, Vendrely V, Asselineau J, Rouanet P, Tuech J-J, Valverde A, et al. Organ preservation with chemoradiotherapy plus local excision for rectal cancer: 5-year results of the GRECCAR 2 randomised trial. Lancet Gastroenterol Hepatol. 2020;5(5):465–74. https://doi.org/10.1016/s2468-1253(19)30410-8.
D’Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat med. 1998;17(19):2265–81. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19%3c2265::aid-sim918%3e3.0.co;2-b.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. NCCN Guidelines Insights: Rectal Cancer, Version 6.2020. J Natl Compr Canc Ne. 2020;18(7):806–15. https://doi.org/10.6004/jnccn.2020.0032.
Heald RJ. The “holy plane” of rectal surgery. J roy soc med. 1988;81(9):503–8. https://doi.org/10.1177/014107688808100904.
Pieniowski EHA, Palmer GJ, Juul T, Lagergren P, Johar A, Emmertsen KJ, et al. Low anterior resection syndrome and quality of life after sphincter-sparing rectal cancer surgery: a long-term longitudinal follow-up. Dis Colon Rectum. 2019;62(1):14–20. https://doi.org/10.1097/DCR.0000000000001228.
Fernandez LM, São Julião GP, Figueiredo NL, Beets GL, van der Valk MJM, Bahadoer RR, et al. Conditional recurrence-free survival of clinical complete responders managed by watch and wait after neoadjuvant chemoradiotherapy for rectal cancer in the international watch & wait database: a retrospective, international, multicentre registry study. Lancet Oncol. 2021;22(1):43–50. https://doi.org/10.1016/s1470-2045(20)30557-x.
Stijns RCH, de Graaf EJR, Punt CJA, Nagtegaal ID, Nuyttens J, van Meerten E, et al. Long-term oncological and functional outcomes of chemoradiotherapy followed by organ-sparing transanal endoscopic microsurgery for distal rectal cancer: the CARTS study. Jama surg. 2019;154(1):47–54. https://doi.org/10.1001/jamasurg.2018.3752.
Zhang X, Ding R, Li J, Wu T, Shen Z, Li S, et al. Efficacy and safety of the “watch-and-wait” approach for rectal cancer with clinical complete response after neoadjuvant chemoradiotherapy: a meta-analysis. Surg endosc. 2022;36(4):2233–44.
Smith JJ, Paty PB, Garcia-Aguilar J. Watch and wait in rectal cancer or more wait and see? JAMA Surg. 2020;155(7):657–8. https://doi.org/10.1001/jamasurg.2020.0226.
Dattani M, Heald RJ, Goussous G, Broadhurst J, Sao Juliao GP, Habr-Gama A, et al. Oncological and survival outcomes in watch and wait patients with a clinical complete response after neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and pooled analysis. Ann Surg. 2018;268(6):955–67. https://doi.org/10.1097/SLA.0000000000002761.
Russell MC, Chiang Y, Feig BW, Chang GJ, Rodriguez-Bigas MA, Skibber JM, et al. Lymph node metastasis in patients with early pathologic t stage rectal cancers: what does local excision leave behind? Ann Surg Oncol. 2012;19:S107-S. https://doi.org/10.1200/jco.2012.30.4_suppl.537.
Yu L, Wang L, Tan Y, Hu H, Shen L, Zheng S, et al. Accuracy of magnetic resonance imaging in staging rectal cancer with multidisciplinary team: a single-center experience. J Cancer. 2019;10(26):6594–8. https://doi.org/10.7150/jca.32685.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32. https://doi.org/10.3322/caac.21338.
Skora T, Nowak-Sadzikowska J, Martynow D, Wszolek M, Sas-Korczynska B. Preoperative short-course radiotherapy in rectal cancer patients: results and prognostic factors. J Radiat Oncol. 2018;7(1):77–84. https://doi.org/10.1007/s13566-017-0340-5.
Pucciarelli S, Giandomenico F, De Paoli A, Gavaruzzi T, Lotto L, Mantello G, et al. Bowel function and quality of life after local excision or total mesorectal excision following chemoradiotherapy for rectal cancer. Br J Surg. 2017;104(1):138–47. https://doi.org/10.1002/bjs.10318.
Acknowledgements
The authors thank all foundations for their support.
Funding
This study was supported by the Fujian Province, Zhangzhou City, the second session of young and middle-aged medical experts with real contribution subsidy funds (2021ZCHZ9); Natural Science Foundation of Fujian Province (2020J011030); Medical Science Research Foundation of Beijing Medical and Health Foundation (B20062DS); Fujian provincial health technology project (2020CXA025); Bethune Charitable Foundation (X-J-2018–004); Joint Funds for the innovation of science and Technology, Fujian province (2020Y9071).
Author information
Authors and Affiliations
Contributions
Protocol/project development: GW, YH, YG; Data collection or management: GW, HC, ZT, JY, MF, XX, QS, HT; Data analysis: GW, KY, YY; Manuscript writing/editing: GW. Other: YH and YG contributed equally to this work as co-corresponding authors; GW, KY, and YY contributed equally to this work and should be considered co-first authors. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and agreed to waive informed consent by the Medical Ethics Committee of Zhangzhou Affiliated Hospital of Fujian Medical University (Grant No. 2020LWB078) and the Medical Ethics Committee of Fujian Medical University Union Hospital (Grant No. 2022kY134). Also, the study was approved by the Medical Ethics Committee of Zhangzhou Affiliated Hospital of Fujian Medical University and the Medical Ethics Committee of Fujian Medical University Union Hospital. All methods were carried out in accordance with relevant guidelines and regulations (declaration of helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, G., Yao, K., Yang, Y. et al. Local resection versus radical resection after neoadjuvant chemoradiotherapy for patients with locally advanced rectal cancer: a propensity-score matched cohort analysis. BMC Gastroenterol 23, 205 (2023). https://doi.org/10.1186/s12876-023-02809-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02809-0