Abstract
Background and aim
Portal hypertension is a common complication of chronic liver diseases responsible for most liver cirrhosis consequences. In patients with portal hypertension, oesophagogastric variceal bleeding is a leading cause of death. Most research has focused on high-risk gastroesophageal varices and bleeding, with only a few studies on early varices. However, early intervention of gastroesophageal varices was found to better improve the prognosis and reduce mortality, but there is still no relevant research. Ultrasonic endoscopy is a combination of endoscopy and ultrasonic imaging. It can gastroscopically detect varices around the oesophagus and stomach and detect oesophageal collateral veins and perforating veins earlier, which is helpful for the early diagnosis of varices. Therefore, this study aimed to explore the correlation between serum fibrosis markers and early gastroesophageal varices in compensated cirrhosis patients.
Methods
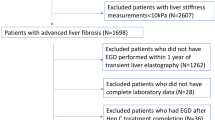
This study included 791 patients with compensated cirrhosis. The selected patients were categorized into three groups. The early gastroesophageal varices group included patients with gastroesophageal varices found by endoscopic ultrasonography but not by gastroscopy. The no gastroesophageal varices group underwent endoscopic ultrasonography and gastroscopy without varices. In addition, gastroesophageal varices can be detected with both techniques. Multiple logistic regression analysis explored the association of serum fibrosis markers with early gastroesophageal varices.
Results
Among the 791 compensated liver cirrhosis patients, 198 patients were without gastroesophageal varices, 279 patients had early gastroesophageal varices, 314 patients had gastroesophageal varices, and both techniques could detect varices. There was a positive correlation between serum fibrosis markers and early gastroesophageal varices. In univariate logistic regression analysis, the patients with early gastroesophageal varices had lower platelet counts (P = 0.034) and higher aspartate aminotransferase (P = 0.046), total bilirubin (P = 0.041), hyaluronic acid (P < 0.001), laminin (P < 0.001), type III procollagen (P = 0.005), type IV collagen (P = 0.002), liver stiffness measurement (P = 0.001), APRI (P = 0.019) and FIB-4 (P = 0.002). Multivariate analysis showed that laminin (OR 1.011; 95% CI 1.004-1.017, P = 0.001) was an independent risk factor for predicting early gastroesophageal varices in compensated cirrhosis patients.
Conclusion
Higher laminin was independently associated with early gastroesophageal varices in compensated cirrhosis patients.
Similar content being viewed by others
Introduction
Portal hypertension, defined as increased pressure in the portal venous system, is a major complication of liver cirrhosis [1]. Vasodilation of the splanchnic capillary beds and arterioles increases the portal blood flow, which, combined with an increase in the intrahepatic vascular resistance, increases the portal pressure [2]. Its complications, which include ascites, gastroesophageal varices, hepatic encephalopathy, and hepatorenal syndrome, cause significant morbidity and mortality [3]. Collaterals develop at the sites of communication between the portal and systemic circulation when the portal pressure increases above a threshold. The most significant collaterals are gastroesophageal varices [4, 5]. Anatomic studies have revealed that early gastroesophageal varices (GEVs) are dilated deep intrinsic veins in the submucosa of the distal oesophagus and proximal stomach of patients with portal hypertension [6, 7]. Patients with varices have a one-third probability of developing a variceal bleed 2 years after diagnosis, with a 20 to 40% mortality rate per episode [8]. Gastroesophageal variceal bleeding is a leading cause of death in patients with cirrhosis [9]. Therefore, early detection of early gastroesophageal varices significantly reduces mortality and medical costs and improves patient survival and prognosis. However, most current studies have focused on high-risk oesophageal and gastric varices and bleeding-related research.
Cirrhotic patients must undergo routine gastroscopy. However, the scope of gastroscopy is limited to the intramucosal and submucosal blood vessels, and the haemodynamic changes in cirrhotic patients with portal hypertension is not understood. Endoscopic ultrasound (EUS) is a noninvasive method that can provide high-resolution anatomic images and can be used to determine the haemodynamic features of collateral vessels surrounding the distal oesophagus and upper stomach in patients with portal hypertension [10]. Therefore, when judging the changes in the collateral circulation of patients with portal hypertension, we can observe the oesophageal and gastric varices that can be seen under conventional gastroscopy and detect the vascular lesions inside and outside the oesophageal wall that cannot be seen under standard endoscopy. EUS can objectively be used to visualize gastroesophageal varices (GEVs) and is more sensitive than conventional endoscopy in detecting GEVs [6, 11, 12]. In Gin-Ho Lo’s study, EUS detected gastric varices (GV) in 28 patients (35%), while in routine endoscopy, only 6 patients (7%) were found to have GV who were noted to have GV by conventional endoscopy [13]. Changjun men et al. reported that a patient with hepatitis B cirrhosis, whose varices were not detected by plain endoscopy and whose oesophageal and gastric varices were detected by EUS, developed oesophageal and gastric variceal bleeding 6 months after the examination [14]. EUS is widely accepted as helpful in assessing oesophagogastric varices because it provides good delineation of the cross-sectional anatomy of the distal oesophagus and proximal stomach and can detect gastroesophageal varices along with periesophageal collateral veins, paraesophageal collateral veins, and perforating veins; therefore, EUS can detect gastroesophageal varices earlier than gastroscopy [15, 16]. Previous studies have also shown that EUS has more advantages in detecting oesophageal and gastric varices caused by portal hypertension and early liver fibrosis [6, 17]. According to Y. T. Lee’s research, the advantage of EUS is that it can provide information about venous abnormalities at the gastroesophageal junction due to the elevated portal vein pressure in patients with early cirrhosis [6]. In recent years, EUS technology has developed rapidly, and EUS has become more critical in diagnosing and treating portal hypertension-related varices. However, this examination is expensive, time-consuming, difficult to perform and has high technical requirements, and the patient can also feel pain during the test. It is difficult to repeat the examination and pursue long-term follow-up, and it cannot be widely popularized in clinical practice. The Baveno VII portal hypertension consensus suggests that the possibility of high-risk varices can be confirmed by liver stiffness and platelet tests to avoid unnecessary endoscopy [18]. However, no alternative noninvasive markers have been found for early portal hypertension. Therefore, it is of great significance to find a noninvasive marker to evaluate oesophageal and gastric varices in patients with compensatory cirrhosis.
Serum liver fibrosis markers include hyaluronic acid (HA), laminin (LN), type III procollagen, and type IV collagen. These four markers of liver fibrosis have been proven to be highly correlated with liver fibrosis in patients with chronic liver disease [19, 20]. It has been demonstrated that liver fibrosis markers have high predictive value for the diagnosis and prognosis of patients with chronic liver disease [21,22,23]. However, there are still few studies on the relationship between serum liver fibrosis markers and the severity and complications of oesophageal and gastric varices. Therefore, we conducted a retrospective cross-sectional study to evaluate the correlation between indicators of liver fibrosis and early gastroesophageal varices in patients with compensatory cirrhosis.
Methods
Study population
In this retrospective study, 791 patients with compensated cirrhosis were enrolled between November 2015 and December 2019. Eligible patients aged 18 years or older who were diagnosed with compensated cirrhosis according to imaging studies using ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI) and who had an irregular and nodular liver together with impaired liver synthetic function could receive a diagnosis of cirrhosis [24]. All patients completed oesophagogastroduodenoscopy (EGD), EUS, FibroScan, imaging, and laboratory examinations within 6 months before and after hospitalization. The exclusion criteria were as follows: 1. primary prevention with nonselective β-blockers or endoscopic ligation; 2. thrombosis of the cavernous transformation of the portal vein system; 3. history of malignancy (including hepatocellular carcinoma); and 4. incomplete clinical data.
This study protocol was approved by the Ethics Committee of Tianjin Second People’s Hospital and conformed to the 1975 Declaration of Helsinki principles. Informed consent was obtained from all patients. All methods were performed following relevant guidelines and regulations.
General characteristics and laboratory investigations
Demographic data (age and sex) and laboratory results (routine blood tests, biochemistry tests, and immunology tests) were collected and analysed. Blood samples were collected 1 week before EUS and EGD. Albumin (ALB), aspartate aminotransferase (AST), serum alanine aminotransferase (ALT), and total bilirubin (TBIL) were detected by a Hitachi 7180 Automatic Biochemical Analyser (Hitachi, Ltd., Tokyo, Japan). According to the manufacturer’s recommendation, platelets (PLTs) were measured using a Sysmex XN-2000 haematology analyser (Sysmex Corporation, Kobe, Japan). Prothrombin time (PT) was performed by the clotting method on the automatic coagulometer “STAGO Compact” (“Diagnostica Stago,” France).
Serum markers of liver fibrosis were measured with AutoLumo A2000 Plus. The upper reference value of laminin ln was 130 ng/ml, the upper reference value of type III procollagen was 15 ng/ml, the upper reference value of hyaluronic acid was 120 ng/ml, and the upper reference value of type IV collagen was 95 ng/ml. The coefficient of variation CV (%) did not exceed 15%.
Assessment of varices
Two experienced operators performed the EGD using the equipment (Olympus CV-260SL, Japan). The variance was described according to the expert guidelines [24]. EUS was conducted by skilled professional doctors using the equipment (Olympus GF-UE260, Japan). According to the results of gastroscopy and endoscopic ultrasonography, the patients were divided into three groups: no gastroesophageal varices (negative on EUS and EGD); early gastroesophageal varices (positive on EUS and negative for EGD), and positive on EUS and EGD. In this study, we mainly focused on comparing the first two groups.
Transient elastography
Liver stiffness (LS) was measured by transient elastography (Echosens, Fibroscan 520, Paris, France) by two experienced practitioners with professional training. The right lobe of the liver was accessed while the patient was positioned with maximal right arm abduction during the operation. The measurements were considered valid if ten measurements were obtained with a 60% success rate of all the total measurements and with an interquartile range of less than 30%.
Spleen size
The patients fasted overnight and routinely underwent abdominal ultrasound examinations to measure the spleen size. Spleen diameters were reported and recorded. Ultrasound was performed by professional operators who did not know the clinical information about the patients.
Statistical analysis
SPSS statistical 26 (IBM, New York, USA) and MedCalc Statistical Software version 15.8 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2015). P < 0.05 was considered statistically significant. The Kolmogorov–Smirnov test was used to analyse whether continuous variables obeyed a normal distribution. The Kruskal–Wallis test was used for comparing nonparametric variables. The nonnormally distributed variables are expressed as the median (quartile 25, 75). The data for categorical variables are presented as the number (n) and proportion (%). The correlation between variables and early gastroesophageal varices was evaluated by Spearman correlation coefficient (r), chi-square test, and binary logistic regression analysis. The “enter” method was used for univariate logistic regression, and the statistically significant variables were included in the univariate logistic regression analysis. The receiver operating characteristic (ROC) curve of laminin was analysed for the prediction of early gastroesophageal varices by the DeLong method.
Results
General characteristics of the patients
A total of 791 compensated cirrhosis patients with a median age of 52 years were included in this study. In total, 716 (90.5%) patients were Child–Pugh class A, and 75 (9.5%) were Child–Pugh class B. According to the different aetiological classifications, there were 561 patients with hepatitis B (71%), 111 patients with hepatitis C (14%), and 119 patients with other liver diseases (15%). Further demographic data and laboratory blood markers of all patients are shown in Table 1.
General characteristics of the patients by gastroesophageal variceal severity
The included patients were divided into the non-GEV group by EUS(−) EGD(−), the early GEV group by EUS(+) EGD(−), and the EUS(+) EGD(+) group. Among the 791 patients, 314 (39.7%) patients with EUS(+) EGD(+), 279 (35.3%) had early GEVs, and 198 (25%) did not. We found that with the development of gastroesophageal varices, the total bilirubin (TBIL), liver stiffness (LS), serum liver fibrosis markers (hyaluronic acid, laminin, type III procollagen, and type IV collagen), aspartate aminotransferase-to-platelet ratio index (APRI) and fibrosis 4 score (FIB-4) were also increased significantly, as shown in Table 2. In this study, we mainly focused on the first two groups. TBIL, LS, APRI, FIB-4, and serum liver fibrosis markers were significantly higher in the early GEV group than those in the non-GEV group (P < 0.05), while PLT was significantly lower in the early GEV groups than that in the non-GEV group (P < 0.05). There was no significant difference in the other indexes between the first two groups (P > 0.05), as shown in Table 2.
Correlations between serum liver fibrosis markers and the clinical characteristics of patients with negative EGD
The correlations between the serum liver fibrosis marker variables and clinical characteristics are summarized in Table 3. As expected, the serum liver fibrosis markers were positively correlated with ALT, AST, TBIL, PT, LS, APRI, FIB-4, and Child–Pugh (C-P) classification (P < 0.05) and negatively correlated with ALB and PLT (P < 0.05). The length and diameter of the spleen were positively correlated with hyaluronic acid, type III procollagen, and type IV collagen (P < 0.05). Hyaluronic acid, laminin, type III procollagen, and type IV collagen were positively correlated with early gastroesophageal varices (P < 0.05).
Analysis of risk factors associated with early GEVs
Binary logistic regression analysis explored the risk factors associated with early GEVs in patients with compensated cirrhosis. In the univariate analysis, the patients with early portal hypertension had lower PLT (P = 0.034), higher AST (P = 0.046), TBIL (P = 0.041), HA (P < 0.001), LN (P < 0.001), procollagen III (P = 0.005), collagen IV (P = 0.002), LS (P = 0.001), APRI (P = 0.019) and FIB-4 (P = 0.002). However, after the multivariate logistic regression analysis, it was found that LN was an independent risk factor for early GEVs in patients with compensated cirrhosis, with an odds ratio (OR) (95% confidence interval CI) of 1.011 (1.004, 1.018), P = 0.001. as shown in Table 4.
Analysis of the diagnostic performance of laminin using the ROC curve
The present study showed that laminin was an independent risk factor for early GEVs in patients with compensated cirrhosis. Then, to evaluate the diagnostic efficacy of laminin, we conducted a ROC curve analysis. The ROC curve (Fig. 1) showed that the best cut-off value for laminin was 93 ng/ml, with a 62.37% sensitivity, a 60.10% specificity, a positive predictive value (PPV) of 68.78%, and a negative predictive value (NPV) of 53.12% for the diagnosis of early GEVs (area under the curve [AUC] = 0.648, 95% CI 0.604-0.691; Table 5). Hence, we demonstrate that laminin levels were significantly associated with early gastroesophageal varices in patients with compensated cirrhosis, but the laminin levels might be inappropriate for diagnosing early GEVs.
Discussion
Previous research has focused on identifying noninvasive serological indications of high-risk oesophagogastric varices to reduce unnecessary endoscopy in patients. Many studies have now shown that noninvasive indicators, including platelet count, albumin, spleen size, and liver stiffness, are related to the severity of high-risk oesophagogastric varices and cirrhosis [25,26,27,28]. Noninvasive indications of early oesophagogastric varices are the subject of comparatively few investigations. Therefore, this study aims to develop noninvasive indicators of oesophagogastric varices, decrease unnecessary gastroscopy and endoscopic ultrasonography, improve prognosis, and reduce mortality and medical expenditures.
This study conducted a correlation analysis between serum liver fibrosis markers and clinical indicators. First, we discovered that serum liver fibrosis markers are related to other indicators of gastroesophageal varices, liver stiffness, APRI, and Fib-4, suggesting that serum liver fibrosis markers could be used as a substitute for other indicators in the prediction of gastroesophageal varices. Second, we found a correlation between serum liver fibrosis markers and early gastroesophageal varices, demonstrating that an increase in serum liver fibrosis markers could indicate the presence of gastroesophageal varices. We also discovered a correlation between serum markers of liver fibrosis and C-P class, suggesting that serum markers of liver fibrosis are related to the severity of cirrhosis [29].
In this study, we found that hyaluronic acid, laminin, type III procollagen, and type IV collagen were positively correlated with early gastroesophageal varices in the univariate analysis and that the increase in laminin concentration was independently correlated with early gastroesophageal varices in compensated liver cirrhosis patients in the multivariate analysis after adjusting for confounding factors. Therefore, we discussed the diagnostic value of laminin and found that it has a limited diagnostic value for early gastroesophageal varices. We may need a prospective study to evaluate its diagnostic performance.
Chronic liver injury can result in fibrosis, characterized by the accumulation of extracellular matrix (ECM) in the liver. Hepatic stellate cells are activated by chronic liver cell injury. These cells acquire the fibrotic myofibroblast phenotype, resulting in collagen synthesis and per sinus contraction, leading to liver fibrosis and portal hypertension. Laminin is one of the major glycoproteins in the basement membrane. Hepatic stellate cells (HSCs) generate and deposit them in the liver’s basement membrane. The liver’s basement membrane is involved in biological tasks such as cell adhesion, matrix component interactions with collagen and glycosaminoglycans, cytoskeleton maintenance, and liver fibrosis [21, 30, 31]. The proportion of type I collagen, type III collagen, and laminin increases in the diseased state, while the mixture of laminin, type IV collagen, and proteoglycan increases in the ECM in normal liver [19, 30, 32]. According to several studies, serum liver fibrosis indicators are related to the severity of liver fibrosis caused by various aetiologies and are significant predictors of disease prognosis [33, 34]. In other research, the serum laminin concentration has also been related to gastroesophageal varices in cirrhosis. This study also found that the laminin concentration is related to early gastroesophageal varices in cirrhosis. Long Fei Wu’s study found that in a one-year prospective analysis, laminin and type IV collagen are possible predictors of rebleeding after oesophagogastric variceal surgery and are related to oesophageal and gastric varices [35].
This study has some limitations. First, this is a retrospective cross-sectional study, and we could not demonstrate a causal link between laminin and the risk of early oesophagogastric varices. A large-scale prospective survey is needed to further clarify the causal relationship between laminin and oesophagogastric varices. Not all patients received EUS examination and had their serum markers of liver fibrosis measured, which increases the possibility of bias. Second, liver biopsy is the gold standard for detecting liver fibrosis. However, invasive liver biopsy has some risks, including high technical requirements and low patient compliance. The patient may also experience pain during the examination. In addition, ultrasonography, CT, and MRI have been the most popular and well-validated noninvasive methods for assessing cirrhosis. Third, although there are standard procedures, there may be variability among the different observers.
In conclusion, we found that indicators of liver fibrosis were associated with early gastroesophageal varices, especially laminin, which was independently associated with early gastroesophageal varices in patients with compensatory cirrhosis. However, laminin has a limited diagnostic value for early gastroesophageal varices. Whether laminin can be used as a noninvasive reference index for monitoring gastroesophageal varices varies in patients with compensated needs to be further evaluated by a prospective study.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Change history
30 March 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12876-023-02714-6
Abbreviations
- EUS:
-
Endoscopic ultrasound
- GEVs:
-
Gastroesophageal varices
- GV:
-
Gastric varices
- EGD:
-
Esophagogastroduodenoscopy
- HA:
-
Hyaluronic acid
- LN:
-
Laminin
- CT:
-
Computed tomography
- MRI:
-
Magnetic Resonance Imaging
- ECM:
-
Extracellular matrix
- HSCs:
-
Hepatic stellate cells
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- TBIL:
-
Total bilirubin
- ALB:
-
Albumin
- PLT:
-
Platelet
- PT:
-
Prothrombin time
- LS:
-
Liver stiffness
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- C-P:
-
Child-pugh
- APRI:
-
Aspartate aminotransferase-to-Platelet Ratio Index
- FIB-4:
-
Fibrosis 4 Score
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
References
Mauro E, Gadano A. What's new in portal hypertension? Liver Int. 2020;40(Suppl 1):122–7.
Ginès P, Krag A, Abraldes JG, Solà E, Fabrellas N, Kamath PS. Liver cirrhosis. Lancet. 2021;398(10308):1359–76.
Simonetto DA, Liu M, Kamath PS. Portal hypertension and related complications: diagnosis and management. Mayo Clin Proc. 2019;94(4):714–26.
Seo YS. Prevention and management of gastroesophageal varices. Clin Mol Hepatol. 2018;24(1):20–42.
Groszmann RJ, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Planas R, Escorsell A, Garcia-Pagan JC, Patch D, Matloff DS, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353(21):2254–61.
Lee YT, Chan FK, Ching JY, Lai CW, Leung VK, Chung SC, Sung JJ. Diagnosis of gastroesophageal varices and portal collateral venous abnormalities by endosonography in cirrhotic patients. Endoscopy. 2002;34(5):391–8.
Robertson M, Hayes P. Primary prophylaxis of variceal bleeding. Hepatol Int. 2018;12(1):1–5.
Smith A, Baumgartner K, Bositis C. Cirrhosis: diagnosis and management. Am Fam Physician. 2019;100(12):759–70.
Huang X, Fan X, Zhang R, Jiang S, Yang K, Chen S. Systemic inflammation and portal vein thrombosis in cirrhotic patients with gastroesophageal varices. Eur J Gastroenterol Hepatol. 2020;32(3):401–5.
Carneiro FOAA, Retes FA, Matuguma SE, Albers DV, Chaves DM, dos Santos MEL, Herman P, Chaib E, Sakai P, Carneiro D’Albuquerque LA, et al. Role of EUS evaluation after endoscopic eradication of esophageal varices with band ligation. Gastrointest Endosc. 2016;84(3):400–7.
Caletti G, Brocchi E, Baraldini M, Ferrari A, Gibilaro M, Barbara L. Assessment of portal hypertension by endoscopic ultrasonography. Gastrointest Endosc. 1990;36:S21–7.
Campos S, Poley JW, van Driel L, Bruno MJ. The role of EUS in diagnosis and treatment of liver disorders. Endosc Int Open. 2019;7(10):E1262–75.
Lo G-H, Lai K-H, Cheng J-S, Huang R-L, Wang S-J, Chiang H-T. Prevalence of paraesophageal varices and gastric varices in patients achieving variceal obliteration by banding ligation and by injection sclerotherapy. Gastrointest Endosc. 1999;49(4):428–36.
Men C, Zhang G. Endoscopic ultrasonography predicts early esophageal variceal bleeding in liver cirrhosis: a case report. Medicine (Baltimore). 2017;96(17):e6749.
Konishi Y, Nakamura T, Kida H, Seno H, Okazaki K, Chiba T. Catheter US probe EUS evaluation of gastric cardia and perigastric vascular structures to predict esophageal variceal recurrence. Gastrointest Endosc. 2002;55(2):197–203.
Lesmana CRA, Paramitha MS, Gani RA. The role of interventional endoscopic ultrasound in liver diseases: what have we learnt? Can J Gastroenterol Hepatol. 2021;2021:9948979.
Faigel DO, Rosen HR, Sasaki A, Flora K, Benner K. EUS in cirrhotic patients with and without prior variceal hemorrhage in comparison with noncirrhotic control subjects. Gastrointest Endosc. 2000;52(4):455–62.
de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C, Baveno VIIF. Baveno VII - renewing consensus in portal hypertension. J Hepatol. 2022;76(4):959–74.
Tsuchida T, Friedman SL. Mechanisms of hepatic stellate cell activation. Nat Rev Gastroenterol Hepatol. 2017;14(7):397–411.
Hikichi T, Obara K, Nakamura S, Irisawa A, Ohira H. Potential application of interventional endoscopic ultrasonography for the treatment of esophageal and gastric varices. Dig Endosc. 2015;27(Suppl 1):17–22.
Guéchot J, Serfaty L, Bonnand A-M, Chazouillères O, Poupon RE, Poupon R. Prognostic value of serum hyaluronan in patients with compensated HCV cirrhosis. J Hepatol. 2000;32(3):447–52.
Carrion JA, Fernandez-Varo G, Bruguera M, Garcia-Pagan JC, Garcia-Valdecasas JC, Perez-Del-Pulgar S, Forns X, Jimenez W, Navasa M. Serum fibrosis markers identify patients with mild and progressive hepatitis C recurrence after liver transplantation. Gastroenterology. 2010;138(1):147–158 e141.
Körner T, Kropf J, Gressner AM. Serum laminin and hyaluronan in liver cirrhosis: markers of progression with high prognostic value. J Hepatol. 1996;25(5):684–8.
Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749–61.
Maurice JB, Brodkin E, Arnold F, Navaratnam A, Paine H, Khawar S, Dhar A, Patch D, O'Beirne J, Mookerjee R, et al. Validation of the Baveno VI criteria to identify low risk cirrhotic patients not requiring endoscopic surveillance for varices. J Hepatol. 2016;65(5):899–905.
Lubel JS, Angus PW. Modern management of portal hypertension. Intern Med J. 2005;35(1):45–9.
Zheng KI, Liu C, Li J, Zhao L, Zheng MH, Wang F, Qi X. Validation of Baveno VI and expanded Baveno VI criteria to identify high-risk varices in patients with MAFLD-related compensated cirrhosis. J Hepatol. 2020;73(6):1571–3.
Zhao L, Wang T, Guo C, Zhou L, Han P, Wang C, Ma Y, Wang J, Gao M, Li J. Modified and alternative Baveno VI criteria based on age for ruling out high-risk varices in patients with compensated cirrhosis. Hepatol Int. 2022.
Qi X, Liu X, Zhang Y, Hou Y, Ren L, Wu C, Chen J, Xia C, Zhao J, Wang D, et al. Serum liver fibrosis markers in the prognosis of liver cirrhosis: a prospective observational study. Med Sci Monit. 2016;22:2720–30.
El-Mezayen HA, Habib S, Marzok HF, Saad MH. Diagnostic performance of collagen IV and laminin for the prediction of fibrosis and cirrhosis in chronic hepatitis C patients: a multicenter study. Eur J Gastroenterol Hepatol. 2015;27(4):378–85.
Younesi S, Parsian H. Diagnostic accuracy of glycoproteins in the assessment of liver fibrosis: a comparison between laminin, fibronectin, and hyaluronic acid. Turk J Gastroenterol. 2019;30(6):524–31.
Jarcuska P, Janicko M, Veseliny E, Jarcuska P, Skladany L. Circulating markers of liver fibrosis progression. Clin Chim Acta. 2010;411(15-16):1009–17.
Halfon P, Bourliere M, Penaranda G, Deydier R, Renou C, Botta-Fridlund D, Tran A, Portal I, Allemand I, Rosenthal-Allieri A, et al. Accuracy of hyaluronic acid level for predicting liver fibrosis stages in patients with hepatitis C virus. Comp Hepatol. 2005;4:6.
Niemelä O, Risteli J, Blake JE, Risteli L, Compton KV, Orrego H. Markers of fibrogenesis and basement membrane formation in alcoholic liver disease. Gastroenterology. 1990;98(6):1612–9.
Wu LF, Xiang XX, Bai DS, Jin SJ, Zhang C, Zhou BH, Qian JJ, Jiang GQ. Novel noninvasive liver fibrotic markers to predict postoperative re-bleeding after laparoscopic splenectomy and azygoportal disconnection: a 1-year prospective study. Surg Endosc. 2021;35(11):6158–65.
Acknowledgements
We thank the medical staff at Tianjin Second People’s Hospital for their essential support and assistance with data collection.
Funding
This work was funded by Natural Science Foundation of Tianjin City (20JCYBJC01150); Tianjin Health Science and Technology Project (No. TJWJ2021QN063, No. TJWJ2021ZD010 and No. TJWJ2021MS034).
Author information
Authors and Affiliations
Contributions
Study concept and design (Ling Mei, Jia Li). drafting manuscript (Ling Mei, Ying Ma). statistical analysis (Qingling Chen, Ling Mei, Jie Liu). data collection (Lili Zhao, Li Zhou, Hang Yang, Jie Liu). the revision of the manuscript for important intellectual content (Ying Ma, Jia Li, Lili Zhao). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was approved by the Ethics Committee of Tianjin Second People’s Hospital and conforms to the principles of the 1975 Declaration of Helsinki. An informed consent was obtained from all patients. All methods were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Ying Ma should have been denoted as an equally contributing author instead of Jie Liu.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mei, L., Ma, Y., Zhao, L. et al. Correlation between serum liver fibrosis markers and early gastroesophageal varices among patients with compensated liver cirrhosis: a cross-sectional analysis. BMC Gastroenterol 22, 515 (2022). https://doi.org/10.1186/s12876-022-02546-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02546-w