Abstract
Background
Studies investigating the changes in short-chain fatty acids (SCFAs) in patients with ulcerative colitis (UC) have yielded inconsistent results. We performed a meta-analysis of studies that investigated the alterations in different SCFAs among UC patients to assess their role in the development of UC.
Methods
Three databases were searched for relevant studies published as of April 2021. Results are presented as standardized mean difference (SMD) with 95% confidence interval (95% CI).
Results
Eleven studies were included in the meta-analysis. Compared to healthy subjects, UC patients had significantly lower concentrations of total SCFAs (SMD = − 0.88, 95%CI − 1.44, − 0.33; P < 0.001), acetate (SMD = − 0.54, 95% CI − 0.91, − 0.17; P = 0.004), propionate, (SMD = − 0.37, 95% CI − 0.66, − 0.07; P = 0.016), and valerate (SMD = − 0.91, 95% CI − 1.45, − 0.38; P < 0.001). On subgroup analysis based on disease status, patients with active UC had reduced concentrations of acetate (SMD = − 1.83, 95% CI − 3.32, − 0.35; P = 0.015), propionate (SMD = − 2.51, 95% CI − 4.41, − 0.61; P = 0.009), and valerate (SMD = − 0.91, 95% CI − 1.45, − 0.38; P < 0.001), while UC patients in remission had similar concentrations with healthy subjects. Patients with active UC had lower butyrate level (SMD = − 2.09, 95% CI − 3.56, − 0.62; P = 0.005) while UC patients in remission had higher butyrate level (SMD = 0.71, 95% CI 0.33, 1.10; P < 0.001) compared with healthy subjects.
Conclusion
UC patients had significantly decreased concentrations of total SCFAs, acetate, propionate, and valerate compared with healthy subjects. In addition, inconsistent changes of certain special SCFAs were observed in UC patients with different disease status.
Similar content being viewed by others
Background
The term chronic inflammatory bowel disease (IBD) is mainly used to refer to Crohn’s disease (CD) and ulcerative colitis (UC). Crohn’s disease may involve any part of the gastrointestinal tract and typically affects all layers of the bowel wall, while UC is confined to rectum and colon and the pathological changes are typically limited to the mucosal layer [1]. The estimated incidence of CD and UC varies from 26 to 199 cases and 37 to 246 cases per 100,000 people, respectively [1]. The incidence of both diseases has shown an increasing trend in developing countries [2]. Though the etiology remains unclear, both genetic and environmental factors have been implicated in the pathogenesis of IBD. In addition, the dynamic balance between commensal microbiota as well as host defensive responses is believed to play an essential role in the pathogenesis of chronic IBD [3]. Previous studies have found altered microbiota in IBD patients compared to healthy subjects [4,5,6]. In addition, the disordered cellular metabolism in UC patients, including the oxidation of butyrate and the fermentation of short chain fatty acids (SCFA), showed a strong correlation with alteration of gut microbiota [7, 8].
Represented by acetate, propionate, and butyrate, SCFAs are mainly produced by intestinal microbial fermentation of undigested dietary carbohydrates, especially resistant starches and dietary fiber, and sometimes by dietary and endogenous proteins [9]. SCFAs are important not only for the normal intestinal biology [10] but also for the absorption of sodium and fluid in the colon and the proliferation of colonocytes [11]. Therefore, monitoring the changes in SCFAs concentration may be helpful to understand the relationship between impaired intestinal ecology and UC.
Considering that the SCFAs have an important impact on IBD, we performed a meta-analysis of published studies that investigated the alterations in SCFAs levels in UC patients.
Material and methods
Literature search and selection criteria
This meta-analysis was performed in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12]. PubMed, Embase, and Web of Science databases were systematically searched for studies published as of April 2021, using the following keywords: “inflammatory bowel disease”, “IBD”, “ulcerative colitis”, “UC”, “short chain fatty acid”, “SCFA”, “acetate”, “acetic acid”, “propionate”, “propionic acid”, “butyrate”, “butyric acid”, “valerate”, “valeric acid”, “lactate”, “lactic acid”, “metabolite”, and “metabolism”. No limitations were placed on the language of publication. The reference lists of related studies were manually searched to identify additional studies.
The inclusion criteria were: (1) study design: randomized controlled trials (RCT), cohort studies, case–control studies, or comparative studies; (2) study population: patients diagnosed with UC; (3) outcome measurement: SCFAs. The exclusion criteria were: (1) lack of cross-sectional comparison or longitudinal evaluation of SCFAs concentration; (2) single-arm studies, case series, animal experiments, and literature reviews; (3) Literature with incomplete or unusable data.
Data extraction
The following information was summarized in a pre-formatted spreadsheet: study design, author names, publication year, sample size, study setting, age, ethnicity, sex, diagnostic criteria for UC, disease extent, and the data of outcome measurements. The authors were contacted in case of any missing information.
Quality assessment
The overall quality of evidence in the included studies was assessed using the modified Newcastle–Ottawa Scale (NOS) [13]. The scale assesses the following three aspects: patient selection, comparability of the intervention/control group, and outcome assessment [13]. The highest NOS score is 9 points [13]. Studies with more > 5 points are regarded as high-quality studies [13].
Statistical analysis
Although the indicators reported in each study are the same, the detection methods and the units used for the measurement of SCFAs concentration were different among different studies. Therefore, the fecal SCFAs content in this meta-analysis was counted by absolute value. In order to eliminate the influence of absolute value and the difference of measurement units between studies, the effect size was calculated using standardized mean difference (SMD) with 95% confidence intervals (CIs). Heterogeneity among the included studies was assessed using the Cochran Q statistic and I2 statistic; P value < 0.1 or I2 > 50% was considered indicative of significant heterogeneity [14]. A random [15] or fixed-effects model [16] was applied to calculate the pooled estimate depending on the heterogeneity among the included studies. Sensitivity analysis was performed to test the potential sources of heterogeneity. Subgroup analysis was performed based on the disease status of UC. The data extracted from the studies included the active and/or remission status of UC (The specific diagnostic and activity criteria are listed in Table 1). Begg’s [17] and Egger’s test [18] were used to assess potential publication bias. Two-tailed P value < 0.05 were considered significant. STATA version 12.0 (Stata Corporation, College Station, TX, USA) was used for all analyses.
Results
Literature search and study selection
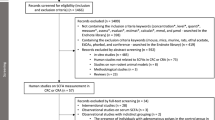
A total of 1964 publications were retrieved on keyword search of the databases. After elimination of duplicate publications, the titles/abstracts of 866 articles were screened. Of these, 846 records were excluded because of various reasons (unrelated to the present study, single-arm study, case series, animal experiments, and literature reviews). Finally, full-text of 20 articles were reviewed, of which 11 studies [4, 19,20,21,22,23,24,25,26,27,28] qualified all the inclusion criteria and were included in the meta-analysis (Fig. 1).
Study characteristics and quality assessment
The year of publication of the selected studies varied from 1982 to 2015. The main characteristics of the included studies are presented in Table 1. The selected studies included one cohort study and ten case–control studies [19]. Eight studies had described the diagnostic criteria of UC, which mainly included: clinical symptoms, laboratory data, endoscopy and histopathology. Eight studies had further analyzed UC patients with active disease and those in remission and the evaluation criteria for disease activity were: Partial MayoScore (n = 2), Clinical colitis activity index (n = 2), Criteria of Truelove and Witts (n = 2), loose stools including obvious blood and overt signs of inflammation at endoscopy (n = 1), mild/moderate/severe activity in the mucosa or inflammatory change on biopsy (n = 1). Six studies had specifically described the lesion sites of UC patients. Gas chromatography (GC) or gas–liquid chromatography (GLC) were the most commonly used methods for analysis of SCFAs in the included studies. All the selected studies had NOS scores of greater than 6, which indicated high quality.
Total SCFAs
Eight studies reported the data of total SCFAs [19, 20, 23,24,25,26,27,28]. The mean total SCFAs level in UC and control groups were 67.83 ± 31.11 and 85.60 ± 27.16, respectively. The summarized estimate indicated that the total SCFAs were significantly lower in the UC group when compared to the control group (SMD = − 0.88, 95% CI − 1.44, − 0.33; P < 0.001) (Fig. 2). Owing to significant heterogeneity among the included studies (I2 = 85.7%, P < 0.001), we conducted sensitivity analysis. After exclusion of one study with a small sample size [23], there was a slight change in the overall estimate (SMD = − 0.86, 95% CI − 1.45, − 0.42; P < 0.001); however, significant heterogeneity persisted (I2 = 81.7%, P < 0.001). After exclusion of one study with outliers [26], the combined WMD did not alter substantially (SMD = − 0.86, 95% CI − 1.38, − 0.27; P < 0.001); however, the heterogeneity remained significant (I2 = 78.5%, P < 0.001).
Acetate
Ten included studies reported the data of acetate [4, 19,20,21,22,23,24, 26,27,28]. The mean acetate level in UC and control groups were 47.15 ± 23.20 and 56.13 ± 20.23, respectively. Pooled result suggested that the acetate level in the UC group was significantly lower than that in the control group (SMD = − 0.54, 95% CI − 0.91, − 0.17; P = 0.004) (Fig. 3). There was significant heterogeneity among the ten studies (I2 = 72.2%, P < 0.001). On sensitivity analysis, exclusion of trials with small sample size or outliers did not change the result substantially; however, the heterogeneity was still found (data not shown).
We performed subgroup analysis based on the disease status of UC. Reduced acetate level was only seen in patients with active UC (SMD = − 1.38, 95% CI − 3.32, − 0.35; P = 0.015) but not in UC patients in remission (SMD = − 0.07, 95% CI − 0.76, 0.62; P = 0.841) (Fig. 3).
Propionate
Ten studies reported the data of propionate [4, 19,20,21,22,23,24,25, 27, 28]. The mean propionate levels in UC and control groups were 15.44 ± 9.57 and 18.12 ± 7.49, respectively. The propionate level in the UC group was significantly lower than that in the control group (SMD = − 0.37, 95% CI − 0.66, − 0.07; P = 0.016) (Fig. 4). There was significant heterogeneity among the studies in this respect (I2 = 61.5%, P = 0.005). However, no valuable information was found in the sensitivity analysis.
On subgroup analysis disaggregated by disease status, the propionate level was significantly reduced in patients with active UC (SMD = − 2.51, 95% CI − 4.41, − 0.61; P = 0.009), but not in UC patients in remission (SMD = 0.14, 95% CI − 0.72, 0.99; P = 0.756) (Fig. 4).
Butyrate
Ten studies reported the data of butyrate [4, 19,20,21,22,23,24,25, 27, 28]. The mean butyrate levels in UC and control group were 11.89 ± 6.62 and 14.41 ± 5.69, respectively. The butyrate level was comparable between the UC group and control group (SMD = − 0.37, 95% CI − 0.82, 0.07; P = 0.10) (Fig. 5). There was significant heterogeneity among the studies (I2 = 82.9%, P < 0.001).
On subgroup analysis disaggregated by disease status, the butyrate level was significantly lower in active UC patients (SMD = − 2.09, 95% CI − 3.56, − 0.62; P = 0.005), but higher in UC patients in remission (SMD = 0.71, 95% CI 0.33, 1.10; P < 0.001) (Fig. 5).
Valerate
Six studies had reported data of valerate [19, 23,24,25, 27, 28]. The mean valerate levels in the UC and control groups were 1.32 ± 1.24 and 2.17 ± 1.21, respectively. The valerate level in the UC group was significantly lower than that in the control group (SMD = − 0.91, 95% CI − 1.45, − 0.38; P < 0.001).
Publication bias
Analysis revealed no significant effect of publication bias on the results of the meta-analysis (Begg’s test: P = 0.115; Egger’s test: P = 0.327).
Discussion
In this study, we performed a meta-analysis of data from 11 studies to characterize the alterations in the levels of SCFAs in UC patients. Our results revealed significant decrease in total SCFAs, acetate, propionate and valerate in UC patients compared with healthy subjects. In addition, for certain special SCFAs, inconsistent alterations were found among the UC patients with different disease status. In particular, reduced levels of acetate and propionate were only observed in patients with active UC but not in those in remission. The butyrate level was significantly lower in patients with active UC, but higher in UC patients in remission.
Compared to the healthy population, the consumption of SCFAs, such as acetate and butyrate, was shown to be a distinguishing characteristic of CD patients [23]. SCFAs are usually generated by the fermentation of complex carbohydrates (including fiber, cellulose, and starches) by the intestinal bacteria [23]. The SCFAs, especially butyrate, play a crucial role in the energy supply of intestinal cell wall and stimulate the growth of epidermal cells [29]. Moreover, methylamine and trimethylamine, generated from food degradation in the intestine, have been found to be lower in the watery excreta of CD patients [30]. This indicates the destruction and dysbiosis of the normal bacterial ecology in patients with IBD. The dysbiosis in intestinal bacterial ecology may be attributed to the microbiota disruption caused by T lymphocytes, which are highly reactive to bacteria and promote inflammatory damage of the intestinal brush border [31]. This would impair the protective effect of the inflammatory epithelium barrier, and affect the absorption of nutrients. Compared with healthy subjects, patients with CD or UC show significantly higher amino acid content in the stool due to the malabsorption caused by inflammation.
In the present meta-analysis, we found a significant reduction in the concentrations of total SCFAs, acetate, propionate, and valerate [4, 32]. Peng et al. reported that the level of SCFA is related with an intracellular energy sensor which facilitates the maintenance of the intestinal barrier function [10]. Kumari et al. [22] further confirmed that the fluctuation in butyrate production was strongly associated with the changes in numbers of butyrate producers among UC patients. Shortage of available butyrate may impair the intestinal barrier function, increasing the risk of exposure of the luminal content to the immune system of the host, thereby exacerbating the immune response [10].
Kumari et al. [22] found that the UC fecal samples had significantly decreased producers as well as levels of butyrate and acetate. This demonstrated that the butyrate supply in the colon was impaired, which might result in insufficient energy for colonocytes. The energy deficiency hypothesis of IBD [33] was also supported by the re-emergence of bacteria producing butyrate during the remission phase with a synchronous increase in the concentration of butyrate. Butyrate as well as the bacteria producing butyrate have recently drawn enormous attention in microbiome research. In the present study, total SCFAs, butyrate, acetate, propionate, and valerate levels in UC patients were significantly reduced compared with healthy subjects. Moreover, Machiels et al. [20] also reported reduced concentrations of SCFAs in colonic lumen of patients with UC. Among the bacterial species producing propionate and butyrate, the populations of Phascolarctobacteria, Roseburia hominis, and Faecalibacterium prausnitzii were shown to be reduced in patients with UC [34, 35]. Considering that the SCFAs or prebiotics can increase the production of SCFAs, alleviate colitis, and protect the function of the intestinal mucosal barrier in UC patients, lack of SCFAs should be a high-risk factor for colitis.
Some limitations of our study should be acknowledged. First, the sample size of some of the included studies was relatively small. Small trials tend to overestimate the effect of an intervention compared to larger trials. Second, there was significant heterogeneity among the studies included in the meta-analysis. This was attributable to the differences in study design, disease status, disease extent, and the methods used for the analysis of SCFAs. Some studies had exclusively considered laboratory findings, clinical findings, or endoscopy findings, which may have led to selection bias regarding the dosage of SCFAs, as patients included in one study may well have different grades of disease severity and extent. Third, the components of SCFAs in UC patients may have been influenced by diet or medications, leading to bias in this meta-analysis.
Conclusions
In conclusion, the present study suggests that the concentrations of total SCFAs, acetate, propionate, and valerate are significantly reduced in UC patients compared with healthy subjects. In addition, inconsistent alterations of certain special SCFAs were observed among UC patients with different disease status. Due to the limited data, the relationship between the severity or extent of UC lesions and the type and dosage of SCFAs were not investigated in this meta-analysis. Similarly, the potential correlation of biological results and luminal extension with disease prognosis was not analyzed either; further studies focusing on these issues are needed.
Availability of data and materials
The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- SCFAs:
-
Short-chain fatty acids
- UC:
-
Ulcerative colitis
- SMD:
-
Standardized mean difference
- 95% CI:
-
95% Confidence interval
- IBD:
-
Inflammatory bowel disease
- CD:
-
Crohn’s disease
- NOS:
-
Newcastle–Ottawa Scale
- GC:
-
Gas chromatography
References
Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–17.
Cosgrove M, Al-Atia RF, Jenkins HR. The epidemiology of paediatric inflammatory bowel disease. Arch Dis Child. 1996;74:460–1.
Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–34.
Takaishi H, Matsuki T, Nakazawa A, Takada T, Kado S, Asahara T, et al. Imbalance in intestinal microflora constitution could be involved in the pathogenesis of inflammatory bowel disease. Int J Med Microbiol. 2008;298:463–72.
Sokol H, Seksik P, Rigottier-Gois L, Lay C, Lepage P, Podglajen I, et al. Specificities of the fecal microbiota in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:106–11.
Manichanh C, Rigottier-Gois L, Bonnaud E, Gloux K, Pelletier E, Frangeul L, et al. Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut. 2006;55:205–11.
Vernia P, Marcheggiano A, Caprilli R, Frieri G, Corrao G, Valpiani D, et al. Short-chain fatty acid topical treatment in distal ulcerative colitis. Aliment Pharmacol Ther. 1995;9:309–13.
Gibson GR. Physiology and ecology of the sulphate-reducing bacteria. J Appl Bacteriol. 1990;69:769–97.
Canani RB, Costanzo MD, Leone L, Pedata M, Meli R, Calignano A. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol. 2011;17:1519–28.
Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr. 2009;139:1619–25.
Scheppach W. Effects of short chain fatty acids on gut morphology and function. Gut. 1994;35:S35–8.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Wells G, Shea B, O’connell D, Peterson J, Welch V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 3rd Symposium on Systematic Reviews: Beyond the Basics. 2000:3–5.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
James SL, Christophersen CT, Bird AR, Conlon MA, Rosella O, Gibson PR, et al. Abnormal fibre usage in UC in remission. Gut. 2015;64:562–70.
Machiels K, Joossens M, Sabino J, De Preter V, Arijs I, Eeckhaut V, et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 2014;63:1275–83.
Roediger WE, Heyworth M, Willoughby P, Piris J, Moore A, Truelove SC. Luminal ions and short chain fatty acids as markers of functional activity of the mucosa in ulcerative colitis. J Clin Pathol. 1982;35:323–6.
Kumari R, Ahuja V, Paul J. Fluctuations in butyrate-producing bacteria in ulcerative colitis patients of North India. World J Gastroenterol. 2013;19:3404–14.
Marchesi JR, Holmes E, Khan F, Kochhar S, Scanlan P, Shanahan F, et al. Rapid and noninvasive metabonomic characterization of inflammatory bowel disease. J Proteome Res. 2007;6:546–51.
Hove H, Mortensen PB. Influence of intestinal inflammation (IBD) and small and large bowel length on fecal short-chain fatty acids and lactate. Dig Dis Sci. 1995;40:1372–80.
Bjerrum JT, Wang Y, Hao F, Coskun M, Ludwig C, Günther U, et al. Metabonomics of human fecal extracts characterize ulcerative colitis Crohn’s disease and healthy individuals. Metabolomics. 2015;11:122–33.
Vernia P, Caprilli R, Latella G, Barbetti F, Magliocca FM, Cittadini M. Fecal lactate and ulcerative colitis. Gastroenterology. 1988;95:1564–8.
Vernia P, Gnaedinger A, Hauck W, Breuer RI. Organic anions and the diarrhea of inflammatory bowel disease. Dig Dis Sci. 1988;33:1353–8.
Treem WR, Ahsan N, Shoup M, Hyams JS. Fecal short-chain fatty acids in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1994;18:159–64.
Scheppach W, Weiler F. The butyrate story: old wine in new bottles? Curr Opin Clin Nutr Metab Care. 2004;7:563–7.
Seibel BA, Walsh PJ. Trimethylamine oxide accumulation in marine animals: relationship to acylglycerol storage. J Exp Biol. 2002;205:297–306.
Oakes ME, Slotterback CS. What’s in a name? A comparison of men’s and women’s judgements about food names and their nutrient contents. Appetite. 2001;36:29–40.
Huda-Faujan N, Abdulamir AS, Fatimah AB, Anas OM, Shuhaimi M, Yazid AM, et al. The impact of the level of the intestinal short chain Fatty acids in inflammatory bowel disease patients versus healthy subjects. Open Biochem J. 2010;4:53–8.
Roediger WE. The colonic epithelium in ulcerative colitis: an energy-deficiency disease? Lancet. 1980;2:712–5.
Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146:1489–99.
Lepage P, Häsler R, Spehlmann ME, Rehman A, Zvirbliene A, Begun A, et al. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology. 2011;141:227–36.
D’Haens G, Sandborn WJ, Feagan BG, Geboes K, Hanauer SB, Irvine EJ, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007;132:763–86.
Truelove SC, Richards WC. Biopsy studies in ulcerative colitis. Br Med J. 1956;1:1315–8.
Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998;43:29–32.
Nikolaus S, Schreiber S. Diagnostics of inflammatory bowel disease. Gastroenterology. 2007;133:1670–89.
Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955;2:1041–8.
Acknowledgements
Dr Fei Yao is the wife of the first author (Hao-Ming Xu). Here we would like to thank Dr Yao for her support to our studies. In addition, we also thank CureEdit Inc. and Medjaden Inc. for data analysis and scientific editing.
Funding
This work was supported by the grants from the National Natural Science Foundation of China (81700487), Guangdong Medical Science and Technology Research Fund (A2019243), Guangzhou Planned Project of Science and Technology (201906010052, 202002020012, 202002030288, 202002030293), and Innovative Clinical Technique of Guangzhou (2019GX05). The funding bodies had no role in the design of the study, the collection, analysis, or interpretation of the data, or writing the manuscript.
Author information
Authors and Affiliations
Contributions
H.M.X., H.L.Z. and G.J.G. designed the study and drafted the manuscript; J.X., and Y.L.Z. interpreted the data and prepared figures and table; H.L.H. and Y.Q.N. designed and organized the study, interpreted the data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, HM., Zhao, HL., Guo, GJ. et al. Characterization of short-chain fatty acids in patients with ulcerative colitis: a meta-analysis. BMC Gastroenterol 22, 117 (2022). https://doi.org/10.1186/s12876-022-02191-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02191-3