Abstract
Background
Irritable bowel syndrome (IBS) is a functional bowel disease that is characterized by abdominal pain, discomfort, and changes in the frequency and form of stool without any organic pathology. In this study, the factors that affect the herbal treatment choices of IBS patients and their results were investigated.
Methods
Included in the study were 248 IBS patients who were over the age of 18. A questionnaire that comprised 25 questions was applied to the participants. Survey questions were asked to the participants regarding their age, place of birth, gender, educational status, demographic details, social standing, socioeconomic status and job, place of residence, and marital status. In addition, The participants were asked about which IBS symptoms they had, from whom they had received the recommendation for use of herbal products, whether the media had an effect on their selection of herbal products, and whether they had benefited from herbal products.
Results
It was observed that 41.1% of the patients with IBS who participated in the study used herbal medicine, 9.8% of whom used them regularly. It was found that the IBS patients participating in the study made their decision to use herbal products mostly based on the recommendations that they were given by acquaintances (57%) and the media (34%). When the patients were evaluated according to their gender, IBS was found to be more common in unemployed women who had a low level of education, while it was more common in working men (p = 0.015, P < 0.001, respectively). The IBS patients who were single used more herbal products that those who were married (P = 0.036). While the use of herbal herbs and oils was predominant in patients whose recommendation content comprised the media/internet and acquaintances, the herbal treatment content recommended by healthcare professionals consisted of traditional treatments and mixtures (P = 0.012). It was determined that a higher percentage of those who used herbal treatments lived in city centers when compared to those who did not (P < 0.001). In addition, it was determined that patients with constipation used herbal products more than those without (P < 0.001). Among the IBS patients, those who had diarrhea and those who were receiving medical treatment preferred to use significantly less herbal products (P = 0.007 and P = 0.041, respectively). It was found that the patients who visited the Gastroenterology Outpatient Clinic mostly used herbal therapy, while those who visited a family doctor used herbal therapy the least (P = 0.029 and P < 0.001, respectively).
Conclusion
The IBS patients revealed whose recommendations they followed when purchasing herbal products, which of the products they preferred, and how useful/beneficial they felt that these products were. In this regard, the addition of training curricula related to herbal treatment for professional healthcare workers will further raise awareness on this topic.
Similar content being viewed by others
Introduction
Irritable bowel syndrome (IBS) is a functional bowel disease that is characterized by abdominal pain, discomfort, and changes in the frequency and form of stool without any organic pathology. IBS is the most common gastrointestinal system disease in patients who have visited internal and surgical outpatient clinics [1, 2]. Its prevalence is increasing among individuals between the ages of 30 and 50. The disease is twice as common in women than in men worldwide, while this rate is 3 times more in Turkey [3, 4]. High socioeconomic status and modern living conditions have been identified as risks for IBS development [5]. The chronic nature of IBS and the lack of an effective treatment cause a loss of workforce and worsening of the quality of life of patients [6]. IBS physiopathology includes genetic factors, intestinal microbiota, impaired immune system regulation, changes in intestinal permeability, and bowel-brain interaction [7]. Rome IV criteria are used in the diagnosis of IBS [8]. The main goal of treatment is to relieve symptoms. Patients frequently use alternative and complementary treatments due to the chronic nature of the symptoms, inadequate treatment response, and medication side effects in IBS [9]. Complementary and alternative treatments for IBS include hypnosis, acupuncture, cognitive behavioral therapy, yoga, and herbal medicine. Herbal medicine has a therapeutic effect as well as side effects in IBS [9, 10]. Herbal products are usually used uncontrolled and without consulting a doctor or determining the correct dosage. A previous study found that the source of information of patients taking herbal therapy comprised other patients who had the same complaints, the media, the internet, their friends and relatives, spice merchants, and herbalists [11]. In this study, the factors that affect the herbal treatment choices of IBS patients and their results were investigated.
Materials and methods
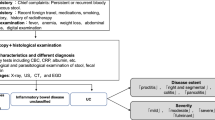
In this study, patients who applied to the Internal Medicine and Gastroenterology Outpatient Clinic of a tertiary referral hospital, between January and April 2018, were evaluated. Among these patients, those whose clinical situations were in line with the ROME IV criteria were included in the study [8]. Those with malignancy and inflammatory bowel disease, who were pregnant, or had any alarm symptoms (recent onset and rapid exacerbation of complaints, onset of symptoms after the age of 50, weight loss, fever, anemia, bloody defecation, symptoms awakening from sleep at night, family history of gastrointestinal cancer, antibiotics use, and travel history to countries with risk of infection) were excluded from the study. A questionnaire was applied to the patients who were accepted for participation in the study (Appendix).
Before the questionnaire was administered, the patients were informed about the aim of the study, verbal consent was obtained, and it was stated that they could withdraw from the study at any stage. The questionnaire included questions about the sociodemographic characteristics of the participants, IBS, and herbal therapy.
Statistical analysis
Statistical analysis of the data was performed using IBM SPSS Statistics 25.0 (IBM Corp., Armonk, NY, USA). The compliance of continuous numerical variables to normal distribution was tested using the Kolmogorov–Smirnov test. Among the descriptive statistics, the continuous numerical variables were presented as the mean ± standard deviation or median [minimum (min) – maximum (max)], while the categorical variables were presented as the frequency and percentage. While the difference between the groups in terms of the mean was evaluated using the student t test, the difference in terms of the median was evaluated using the Mann–Whitney U test. The categorical variables were analyzed using the Pearson chi square test. Unless otherwise stated, P < 0.05 was considered as statistically significant.
Results
The number of patients included in the study was 248, and of these, 139 were women (56%) and 109 (44%) were men. The mean age of the patients was 43.6 ± 13.5 years; the mean age of the women was 44.5 ± 13.0 years, while the mean age of the men was 42.4 ± 14 years. Only 41.1% of the patients were receiving herbal treatment, 9.8% of whom were using it regularly. Of the IBS patients, 46% were primary and secondary school graduates, 23.4% were high school graduates, and 20.2% were undergraduates. It was found that IBS was significantly more common in women who had low education than the men with the same educational background (P = 0.015). Considering their occupations, IBS was found to be significantly more common in women who did not work than in men who did (P < 0.001). Considering their marital status, 74.6% of the patients were married and 25.4% were single. It was found that the single patients used significantly more herbal products for IBS (P = 0.036). The patients were mostly residents of district centers (46%). The sociodemographic data of the patients are given in Table 1. The most common complaints among the patients on admission were abdominal distension (79%), constipation (70.6%), and abdominal pain (66.9%) (Table 2). The mean duration of time that the patients had typical IBS symptoms was 5 months (min: 3, max: 43). The number of outpatient clinic visits and the imaging characteristics are given in Table 3. While 87.1% of the patients did not use the medication that was given to them regularly, 1.6% used it regularly, and 11.3% did not receive any medical treatment (Table 4). Of the patients, 102 were receiving herbal therapy (41.1%), while 146 (58.9%) were not. Those who received herbal therapy mostly preferred a single herb (12.5%) or daily traditional solutions (12.5%), such as mint-lemon and linden. Apart from these, they used vegetable oils (10.1%) and herb mixtures from herbalists (5%), respectively. The patients did not have any detailed information about the ingredients of the mixtures that they bought from most of the spice merchants. In addition, traditional treatments generally vary depending on the society but are known by everyone, such as drinking mint and lemon tea for stomach pain and nausea, using fennel tea for abdominal pain, and using probiotic yogurt that contains olive oil and flaxseed for constipation. Other herbal herbs, concoctions (such as tea mixed with mint, fennel, ginger, chamomile, and cinnamon), and oils are herbal products that are usually prepared by the spice merchants. The information and suggestions that the patients received for the use of herbal therapy were mostly from their neighbors, relatives, and friends (57%). Other sources included the media/internet (34%) and health professionals (9%). While the use of herbal herbs and oils was predominant in patients whose content was the media/internet and acquaintances, the herbal treatment content recommended by healthcare professionals consisted of traditional treatments and mixtures (P = 0.012). While 23.5% of the patients found the herbal treatment to be ineffective, 22.5% stated that they found it to be weakly effective, and 54% found it to be effective (moderate and very effective). Moreover, 1 patient stated that s/he experienced life-threatening side effects. While 9.8% of the patients used herbal therapy regularly, 47.06% did not (Table 5). There was no significant relationship between the professions of the patients and the herbal therapy that they used (P = 0.774). There was no significant difference in terms of female and male gender in terms of herbal treatment usage (P = 0.573). It was found that those who received herbal therapy mostly lived in city centers (P < 0.001). Those suffering from diarrhea among the IBS patients preferred to use significantly fewer herbal products (P = 0.007). Patients who received medical treatment used herbal therapy less than the others (P = 0.041). It was found that the patients who visited the Gastroenterology Outpatient Clinic mostly used herbal therapy, while the patients who visited a family doctor used herbal therapy the least (P = 0.029, P < 0.001, respectively) (Table 6). There was no significant relationship between the types of herbal therapies used by the patients and the side effects of these treatments (P = 0.392) (Table 7). Patients with constipation preferred to use herbal therapy more than the patients without constipation (P < 0.001) (Table 8).
Discussion
IBS is a chronic functional disorder of the gastrointestinal tract that is characterized by abdominal pain, abdominal distension, diarrhea, and episodes of constipation, and it has a high prevalence and diverse etiology worldwide [9, 12]. The current approach in the treatment of this syndrome is to reduce the symptoms rather than eliminate the underlying causes of the disease. Although there are various pharmacological treatment options, due to the limited effectiveness, high cost, and side effects of these treatments, the use of herbal therapy has become more common worldwide. In the current study, patients who received no medical treatment, lived in city centers, and had a relatively low socioeconomic and cultural levels tended to receive herbal therapy. This study was not a community-based study, and the selection of those who wanted to participate in the survey from the patients who had applied to the outpatient clinics was considered as the reason why the gender difference was not evident in both the frequency of IBS and the use of herbal.
The Chinese herbal products that have been used in East Asia for thousands of years are examples of this treatment [13]. Acupuncture, which is a type of traditional medicine that has been mentioned frequently in the media, can also be used with herbal therapies, and in a study by Yan et al., the administration of herbal therapy together with acupuncture was found to be safe and effective [14]. As it is around the world, some of the patients herein who participated in the study tended to use herbs and traditional methods. Although the herbal therapies used were partially effective with a single use, it has been reported that the combinations created from these products can also be used, and this may be more beneficial [9]. It is also believed that many factors, such as the regular use of these products and the regular maintenance of medical treatment by the patient, affect the benefits obtained from herbal products. It was believed herein that regular treatment and follow-up can have a positive effect on IBS and herbal treatment, as in every disease. These products, which are also popular with IBS patients, have gained vast attention in the written, visual, and verbal media. Although most of the participants in the current study obtained their herbal product recommendations from their neighbors, relatives, and friends, the influence of the media in the selection of herbal products was also quite high. The patients obtained advisory information for these herbal therapies from the media rather than from health professionals. The effect/side effect profile of herbal therapies is not clear, as different herbal therapies may show different effects on patients, and these unpredictable effects have a wide spectrum, from acute renal failure to toxic hepatitis. It is obvious that the information given about these herbal products covered in the media may not be objective, non-commercial, or completely correct [15]. Unfortunately, because of commercial concerns or hearsay information about these products, for which safety and efficacy criteria are not clear, patients may be misled, and these products may cause various side effects or less beneficial effects than expected. A study by Munyaradzi et al. evaluated the effects of advertisements for herbal therapies on African societies and found that the headlines used in media-based advertisements and interesting statements about the product, even if not scientific information, affected the decisions of the patients [16]. It is thought that the herbal products used by IBS patients, which may be beneficial/harmful or have no effect in various situations, may deviate from their purpose due to the biased/unbiased promotion of the media and bilateral relations in daily life. The fact that the majority of patients who participated in the current study did not receive herbal therapy may be a result of these concerns.
Madisch A et al. reported in their study that 54% of primary care physicians were satisfied with the success of spasmolytic treatment, and 75% were satisfied with phyto-therapeutic agents and probiotics [17].
Conclusion
For IBS patients to use herbal products correctly and appropriately, they should be provided unbiased information about these herbal products. Relatives, neighbors, etc. In this regard, the addition of training curricula related to herbal treatment for professional healthcare workers will further raise awareness and it will increase the conscious use of herbal medicine in the treatment of IBS.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Hungin AP, Whorwell PJ, Tack J, et al. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40.000 subjects. Aliment Pharmacol Ther. 2003;17:643–50.
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–21.
Brandt LJ, Chey WD, et al. An evidence-based position statement on the management of irritable bowel syndrome: American Collage of Gastroenterology task force on irritable bowel syndrome. Am J Gastroenterol. 2009;104(Suppl 1):S1-35.
Houghton LA, Heitkemper M, Crowell MD, et al. Age, gender, and women’s health and the patient. Gastroenterology. 2016;150:1332–43.
Howell S, Talley NJ, Quine S, Poulton R. The irritable bowel syndrome has origins in the childhood socioeconomic environment. Am J Gastroenterol. 2004;99(8):1572–8. https://doi.org/10.1111/j.1572-0241.2004.40188.x (PMID: 15307879).
El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171–85.
Lacy BE, Chey WD, Lembo AJ. New and emerging treatment options for irritable bowel syndrome. Gastroenterol Hepatol (N Y ). 2015;11(4 Suppl 2):1–19.
Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150:1393–407.
Bahrami HR, Hamedi S, Salari R. Herbal medicines for the management of irritable bowel syndrome: a systematic review. Electron Phys. 2016;8(8):2719–25.
Spanier JA, Howden CW, Jones MP. A systematic review of alternative therapies in the irritable bowel syndrome. Arch Intern Med. 2003;163(3):265–74.
Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;10(4):177. https://doi.org/10.3389/fphar.2013.00177.
Rahimi R, Abdollahi M. Herbal medicines for the management of irritable bowel syndrome: a comprehensive review. World J Gastroenterol. 2012;18(7):589–600. https://doi.org/10.3748/wjg.v18.i7.589.
Bi Z, Zheng Y, Yuan J, Bian Z. The efficacy and potential mechanisms of Chinese herbal medicine on irritable bowel syndrome. Curr Pharm Des. 2017;23(34):5163–72. https://doi.org/10.2174/1381612823666170822101606.
Yan J, Miao ZW, Lu J, et al. Acupuncture plus Chinese herbal medicine for irritable bowel syndrome with diarrhea: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2019;2019:7680963. https://doi.org/10.1155/2019/7680963.
Peacock M, Badea M, Bruno F, et al. Herbal supplements in the print media: communicating benefits and risks. BMC Complement Altern Med. 2019;19(1):196. https://doi.org/10.1186/s12906-019-2602-9.
Munyaradzi M. Ethical quandaries in spiritual healing and herbal medicine: a critical analysis of the morality of traditional medicine advertising in southern African urban societies. Pan Afr Med J. 2011;10:6. https://doi.org/10.4314/pamj.v10i0.72212.
Madisch A, Labenz C, Hollenz M, Gross M, Labenz J. Therapiemanagement des reizdarmsyndroms in der hausarztpraxis : probiotika und phytotherapeutika kommen häufig erfolgreich zum einsatz [therapeutic management of irritable bowel syndrome in the family doctor’s practice - probiotics and phytotherapeutics are often used successfully]. MMW Fortschr Med. 2020;162(Suppl 5):7–13.
Acknowledgements
Thank you to our assistant and specialist doctor friends who have supported our work in the Internal Medicine Clinic.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
EG, NYC, SB, SK and OE: investigation, project administration, software, visualization, writing-review and editing, methodology. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ankara City Hospital No.1 Clinical Research Ethics Committee approval was received for this study at 25.11.2020, Approval number: E1-20-1312. Informed consent was obtained from all patients participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Helsinki declaration
The authors declared that this study is in accordance with the Helsinki Declaration.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The questionnaire about evaluatıon of knowledge and attıtude of persons wıth gastroenterologıcal complaınts:


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gemcioglu, E., Yılmaz Cakmak, N., Baser, S. et al. Factors affecting the use of herbal products in patients with Irritable Bowel Syndrome and their results: case–control study. BMC Gastroenterol 22, 43 (2022). https://doi.org/10.1186/s12876-022-02125-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02125-z