Abstract
Background
Pancreatic panniculitis is a rare skin manifestation in pancreatic disease patients that most frequently develops on the lower legs. We report the unique case of a 68-year-old man who suffered from pancreatic panniculitis on his trunk associated with acute pancreatitis due to an intraductal papillary mucinous neoplasm.
Case presentation
A 68-year-old man complained of a 2-day history of a tender subcutaneous nodule on his trunk. Laboratory tests and abdominal contrast computed tomography were consistent with acute pancreatitis due to an intraductal papillary mucinous neoplasm. A skin biopsy of the nodule histologically displayed lobular panniculitis with characteristic “ghost cells”, which indicated pancreatic panniculitis.
Conclusions
In order to avoid a missed or delayed diagnosis, clinicians should bear in mind that pancreatic panniculitis can be the first manifestation of pancreatic disease when encountering subcutaneous nodules on the trunk.
Similar content being viewed by others
Background
Pancreatic panniculitis is a rare skin manifestation associated with pancreatic disorders that presents in approximately 3% of patients with acute or chronic pancreatic disease [1]. The disorder most commonly develops on the lower legs as ill-defined erythematous subcutaneous nodules. Such nodules are detected in up to 45% of patients with pancreatic panniculitis before recognition of the original pancreatic disease [1]. Accordingly, the chief complaint of the patient is sometimes erythematous nodule detection before abdominal symptoms. Clinicians therefore have the risk of overlooking the underlying pancreatic disease. We herein report the rare case of a 68-year-old man who had pancreatic panniculitis on his trunk associated with acute pancreatitis due to an intraductal papillary mucinous neoplasm (IPMN).
Case presentation
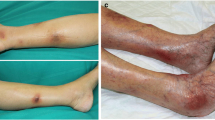
A 68-year-old male patient was referred to our hospital by his primary care physician for further evaluation of a painful subcutaneous nodule on his upper middle abdomen, which was suspected to be abdominal cellulitis. Five days before admission, he had suffered from epigastralgia, nausea, and anorexia. Four days before admission, his epigastralgia had improved. Two days prior to admission, he noticed an erythematous nodule on his abdomen. His chief complaint on admission to our hospital was the painful nodule on his abdomen. He had been under medical treatment with aspirin, atorvastatin, colestimide, nicorandil, and famotidine for past medical histories of coronary artery bypass grafting (CABG), appendectomy, and dyslipidemia. He had no allergies. He had smoked 1 pack per day for 33 years before quitting 15 years earlier. He habitually drank 20 g of ethanol per day, with no history of heavy drinking. On examination, his temperature was 38.8 °C, blood pressure was 144/74 mmHg, and pulse was 98/min with regular rhythms. A painful and tender erythematous nodule was palpable on his epigastrium at the lower edge of a postoperative scar from CABG. The nodule was 2.5 cm in diameter and surrounded by pale erythema (Fig. 1a). Laboratory tests revealed a white blood cell count elevation of 15,650/μL along with a C-reactive protein (CRP) abnormality of 24.4 mg/dL, with no amylase or lipase elevation (Table 1). Abdominal contrast computed tomography (CT) confirmed grade 1 acute pancreatitis (Fig. 2a) and a 20 mm multifocal cystic mass at the pancreatic body along with an 8 mm dilation of the main pancreatic duct, which were compatible with a diagnosis of IPMN (Fig. 2b). Thereafter, he commenced intravenous fluid infusion and antibiotic therapy. On hospital day 3, he became afebrile and showed improvements in inflammatory clinical parameters. A punched biopsy of the skin lesion on hospital day 4 revealed lobular panniculitis without vasculitis findings. Histological analysis uncovered focal necrosis of adipocytes and “ghost-like” cells with calcification surrounded by neutrophil-rich inflammatory infiltration, which indicated pancreatic panniculitis (Fig. 3). Intravenous fluid infusion and antibiotic therapy were continued until discharge on hospital day 12 for nodule pain disappearance along with CRP normalization. The erythematous nodule on his abdomen disappeared 1 week afterwards (Fig. 1b). The patient has been complaint-free without nodule recurrence or additional nodule appearance since his discharge 2 years prior. His IPMN status is routinely monitored every 3 months by imaging studies.
a A punched biopsy of the skin lesion revealed lobular panniculitis with focal necrosis of adipocytes. (hematoxylin and eosin staining, × 2 magnification. b The biopsy showed “ghost-like” cells with calcification surrounded by neutrophil-rich inflammatory infiltration (arrow). (hematoxylin and eosin staining, × 10 magnification)
Discussion and conclusions
Pancreatic panniculitis is a rare skin manifestation associated with pancreatic disease. In the clinical setting, panniculitis is noticed as erythematous, ill-defined, and/or red-brown nodules [2] that generally affect the lower limbs and buttocks, rarely the trunk and upper extremities [3]. Only 9 cases have been described of pancreatic panniculitis on the trunk [3,4,5,6,7,8,9,10,11]. We encountered a unique case of subcutaneous nodules on the abdomen with latent IPMN. Skin biopsy revealed the typical histological findings of pancreatic panniculitis of lobular neutrophilic necrotizing panniculitis intermingled with specific necrotic anucleate adipocytes, called “ghost cells” [12].
The mechanism of pancreatic panniculitis onset remains unknown. It is hypothesized that systemically released pancreatic enzymes such as amylase and lipase can cause lipolysis and fat necrosis [13, 14], resulting in pancreatic panniculitis as a specific clinical phenotype. However, several cases of pancreatic panniculitis with normal serum pancreatic enzymes have been reported [15, 16], as in the present case. One possible reason for our patient was that his pancreatic amylase had already peaked due to pancreatitis improvement since such pancreatitis symptoms as epigastralgia had improved 4 days before admission. Therefore, it is clinically important to consider pancreatic panniculitis in patients with subcutaneous nodules even in the absence of abdominal symptoms for underlying pancreatic disorders, regardless of pancreatic enzyme status. This may avoid a missed or significantly delayed diagnosis of primary pancreatic disease.
The main pancreatic diseases related to pancreatic panniculitis have been reported as acute or chronic pancreatitis, pancreatic carcinoma (ductal adenocarcinoma, acinar cell carcinoma, or neuroendocrine carcinoma), and IPMN. In the present case, the underlying pancreatic disease was acute pancreatitis due to IPMN. Zundler et al. reviewed that subcutaneous lesions were noted prior to the diagnosis of pancreatic disease in 48.9% of reported cases [3]. In terms of clinical course, the period between subcutaneous lesion appearance and the detection of abdominal disorders could be several months for pancreatic panniculitis [17]. Table 2 summarizes the literature on pancreatic panniculitis displaying subcutaneous nodules as a chief complaint before diagnosing pancreatic disease. We searched the English-written literature between 1994 and 2019 using the parameters “pancreatic panniculitis” and “subcutaneous fat necrosis AND pancreas” in PubMed to identify 56 reported cases. The site of the nodules was predominantly the leg, with some cases on the trunk or arm. It should be noted that the period between subcutaneous lesion appearance and detection of the pancreatic disease was up to 48 weeks, and the underlying pancreatic disorder was a pancreatic neoplasm in nearly half of patients. Of all reported cases summarized in Table 2, only 2 were described as latent IPMN presenting as pancreatic panniculitis [22, 41]. Pancreatic panniculitis could therefore serve as the impetus for an intensive search for pancreatic neoplasms in order to prevent a potentially long delay in diagnosis [17, 60].
In conclusion, clinicians should bear in mind that pancreatic panniculitis can be the chief complaint of pancreatic disease when encountering subcutaneous nodules on the trunk to prevent a missed or delayed diagnosis.
Availability of data and materials
N/A
Abbreviations
- Alb:
-
Albumin
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AMY:
-
Amylase
- APTT:
-
Activated partial thromboplastin time
- AST:
-
Aspartate aminotransferase
- BE:
-
Base excess
- BUN:
-
Blood urea nitrogen
- CABG:
-
Coronary artery bypass grafting
- CA19–9:
-
Carbohydrate antigen 19–9
- cCa:
-
Corrected calcium
- CEA:
-
Carcinoembryonic antigen
- Cre:
-
Creatinine
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- GGTP:
-
Gamma-glutamyltranspeptidase
- Hb:
-
Hemoglobin
- INR:
-
International normalized ratio
- IPMN:
-
Intraductal papillary mucinous neoplasm
- LDH:
-
Lactate dehydrogenase
- Neut:
-
Neutrophils
- N/D:
-
No data
- Over NL:
-
Over normal limit
- PT:
-
Prothrombin time
- RBC:
-
Red blood cells
- T-Bil:
-
Total bilirubin
- TP:
-
Total protein
- ULN:
-
Upper limit of normal
- WBC:
-
White blood cells
- WNL:
-
Within normal limit
References
Dahl PR, Su WP, Cullimore KC, Dicken CH. Pancreatic panniculitis. J Am Acad Dermatol. 1995;33(3):413–7.
Garcia-Romero D, Vanaclocha F. Pancreatic panniculitis. Dermatol Clin. 2008;26(4):465–70 vi.
Zundler S, Erber R, Agaimy A, Hartmann A, Kiesewetter F, Strobel D, Neurath MF, Wildner D. Pancreatic panniculitis in a patient with pancreatic-type acinar cell carcinoma of the liver--case report and review of literature. BMC Cancer. 2016;16:130.
Ferri V, Ielpo B, Duran H, Diaz E, Fabra I, Caruso R, Malave L, Plaza C, Rodriguez S, Garcia L, et al. Pancreatic disease, panniculitis, polyarthrtitis syndrome successfully treated with total pancreatectomy: case report and literature review. Int J Surg Case Rep. 2016;28:223–6.
Rao AG, Danturty I. Pancreatic panniculitis in a child. Indian J Dermatol. 2010;55(2):185–7.
Sotoude H, Mozafari R, Mohebbi Z, Mirfazaelian H. Pancreatic panniculitis. Am J Emerg Med. 2014;32(8):944.e941–2.
Burland L, Green BL. A cutaneous manifestation of intra-abdominal disease. Bmj. 2014;349:g5492.
Rose C, Leverkus M, Fleischer M, Shimanovich I. Histopathology of panniculitis--aspects of biopsy techniques and difficulties in diagnosis. J Dtsch Dermatol Ges. 2012;10(6):421–5.
Cevasco M, Rodriguez JR, Fernandez-del Castillo C. Clinical challenges and images in GI: image 3. Pancreatic acinar cell carcinoma with subcutaneous fat necrosis. Gastroenterology. 2008;135(4):1054 1433.
Zhang MY, Tian BL. Pancreatic panniculitis and solid pseudopapillary tumor of the pancreas: a case report. World J Clin Cases. 2018;6(15):1036–41.
Ichiki T, Jinnai S, Nakagawa R, Kohda F, Furue M. Case of widespread fat necrosis that was caused by severe pancreatitis and histologically resembled pancreatic panniculitis. J Dermatol. 2017;44(8):979–81.
Laureano A, Mestre T, Ricardo L, Rodrigues AM, Cardoso J. Pancreatic panniculitis - a cutaneous manifestation of acute pancreatitis. J Dermatol Case Rep. 2014;8(1):35–7.
Dhawan SS, Jimenez-Acosta F, Poppiti RJ Jr, Barkin JS. Subcutaneous fat necrosis associated with pancreatitis: histochemical and electron microscopic findings. Am J Gastroenterol. 1990;85(8):1025–8.
Forstrom TL, Winkelmann RK. Acute, generalized panniculitis with amylase and lipase in skin. Arch Dermatol. 1975;111(4):497–502.
Robertson JC, Eeles GH. Syndrome associated with pancreatic acinar cell carcinoma. Br Med J. 1970;2(5711):708–9.
Jacobson-Dunlop E, Takiguchi R, White CR Jr, White KP. Fatal pancreatitis presenting as pancreatic panniculitis without enzyme elevation. J Cutan Pathol. 2011;38(6):455–7.
Lee WS, Kim MY, Kim SW, Paik CN, Kim HO, Park YM. Fatal pancreatic panniculitis associated with acute pancreatitis: a case report. J Korean Med Sci. 2007;22(5):914–7.
Guanziroli E, Colombo A, Coggi A, Gianotti R, Marzano AV. Pancreatic panniculitis: the "bright" side of the moon in solid cancer patients. BMC Gastroenterol. 2018;18(1):1.
Evans AC, Singhi AD, Zeh HJR, Bahary N, Brand RE. An unexpected etiology of pancreatic Panniculitis: a case report. J Pancreat Cancer. 2017;3(1):1–4.
Yoshihiro T, Nio K, Tsuchihashi K, Ariyama H, Kohashi K, Tsuruta N, Hanamura F, Inadomi K, Ito M, Sagara K, et al. Pancreatic acinar cell carcinoma presenting with panniculitis, successfully treated with FOLFIRINOX: a case report. Mol Clin Oncol. 2017;6(6):866–70.
Zhang G, Cao Z, Yang G, Wu W, Zhang T, Zhao Y. Pancreatic panniculitis associated with pancreatic carcinoma: a case report. Medicine. 2016;95(31):e4374.
Menzies S, McMenamin M, Barnes L, O'Toole D. Pancreatic panniculitis preceding acute pancreatitis and subsequent detection of an intraductal papillary mucinous neoplasm: a case report. JAAD Case Rep. 2016;2(3):244–6.
Ng CH, Lim WY, Lee SS. Radiological features of a rare case of pancreatic panniculitis presenting in bilateral lower extremities. J Radiol Case Rep. 2016;10(4):1–7.
Beveridge M, Pei S, Tsoukas MM. Pancreatic panniculitis in a pancreas-kidney transplant patient resolved after immunosuppression increase: case report and review of literature. JAAD Case Rep. 2015;1(2):101–5.
Ito T, Moriuchi R, Kikuchi K, Shimizu S. Pancreatic panniculitis. BMJ Case Rep. 2015;2015. https://doi.org/10.1136/bcr-2014-206980.
Mahawish K, Iyasere IT. Pancreatic panniculitis. BMJ Case Rep. 2014;2014. https://doi.org/10.1136/bcr-2014-204290.
Omland SH, Ekenberg C, Henrik-Nielsen R, Friis-Moller A. Pancreatic panniculitis complicated by infection with Corynebacterium tuberculostearicum: a case report. IDCases. 2014;1(3):45–6.
Souza FH, Siqueira EB, Mesquita L, Fabricio LZ, Tuon FF. Pancreatic panniculitis as the first manifestation of visceral disease--case report. An Bras Dermatol. 2011;86(4 Suppl 1):S125–8.
Colantonio S, Beecker J. Pancreatic panniculitis. CMAJ. 2012;184(2):E159.
Zheng ZJ, Gong J, Xiang GM, Mai G, Liu XB. Pancreatic panniculitis associated with acinar cell carcinoma of the pancreas: a case report. Ann Dermatol. 2011;23(2):225–8.
Madarasingha NP, Satgurunathan K, Fernando R. Pancreatic panniculitis: a rare form of panniculitis. Dermatol Online J. 2009;15(3):17.
Hudson-Peacock MJ, Regnard CF, Farr PM. Liquefying panniculitis associated with acinous carcinoma of the pancreas responding to octreotide. J R Soc Med. 1994;87(6):361–2.
Pfaundler N, Kessebohm K, Blum R, Stieger M, Stickel F. Adding pancreatic panniculitis to the panel of skin lesions associated with triple therapy of chronic hepatitis C. Liver Int. 2013;33(4):648–9.
Kirkland EB, Sachdev R, Kim J, Peng D. Early pancreatic panniculitis associated with HELLP syndrome and acute fatty liver of pregnancy. J Cutan Pathol. 2011;38(10):814–7.
Gandhi RK, Bechtel M, Peters S, Zirwas M, Darabi K. Pancreatic panniculitis in a patient with BRCA2 mutation and metastatic pancreatic adenocarcinoma. Int J Dermatol. 2010;49(12):1419–20.
Borowicz J, Morrison M, Hogan D, Miller R. Subcutaneous fat necrosis/panniculitis and polyarthritis associated with acinar cell carcinoma of the pancreas: a rare presentation of pancreatitis, panniculitis and polyarthritis syndrome. J Drugs Dermatol. 2010;9(9):1145–50.
Tran KT, Hughes S, Cockerell CJ, Yancey KB. Tender erythematous plaques on the legs. Pancreatic panniculitis (PP). Clin Exp Dermatol. 2010;35(3):e65–6.
Beyazıt H, Aydin O, Demirkesen C, Derin D, Süt P, Emre A, Mandel N. Pancreatic panniculitis as the first manifestation of the pancreatic involvement during the course of a gastric adenocarcinoma. Med Oncol. 2011;28(1):137–9.
Sagi L, Amichai B, Barzilai A, Weitzen R, Trau H. Pancreatic panniculitis and carcinoma of the pancreas. Clin Exp Dermatol. 2009;34(5):e205–7.
Marsh Rde W, Hagler KT, Carag HR, Flowers FP. Pancreatic panniculitis. Eur J Surg Oncol. 2005;31(10):1213–5.
Gahr N, Technau K, Ghanem N. Intraductal papillary mucinous adenoma of the pancreas presenting with lobular panniculitis. Eur Radiol. 2006;16(6):1397–8.
Berkovic D, Hallermann C. Carcinoma of the pancreas with neuroendocrine differentiation and nodular panniculitis. Onkologie. 2003;26(5):473–6.
Echeverría CM, Fortunato LP, Stengel FM, Laurini J, Díaz C. Pancreatic panniculitis in a kidney transplant recipient. Int J Dermatol. 2001;40(12):751–3.
Ball NJ, Adams SP, Marx LH, Enta T. Possible origin of pancreatic fat necrosis as a septal panniculitis. J Am Acad Dermatol. 1996;34(2 Pt 2):362–4.
Cheng KS, Stansby G, Law N, Gardham R. Recurrent panniculitis as the first clinical manifestation of recurrent acute pancreatitis secondary to cholelithiasis. J R Soc Med. 1996;89(2):105p–6p.
Choi HJ, Kim KJ, Lee MW, Choi JH, Moon KC, Koh JK. Pancreatic carcinoma-associated subcutaneous fat necrosis improved by palliative surgery. J Dermatol. 2004;31(7):584–6.
Ashley SW, Lauwers GY. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 37-2002. A 69-year-old man with painful cutaneous nodules, elevated lipase levels, and abnormal results on abdominal scanning. N Engl J Med. 2002;347(22):1783–91.
Shbeeb MI, Duffy J, Bjornsson J, Ashby AM, Matteson EL. Subcutaneous fat necrosis and polyarthritis associated with pancreatic disease. Arthritis Rheum. 1996;39(11):1922–5.
Mehringer S, Vogt T, Jabusch HC, Kroiss M, Fürst A, Schölmerich J, Messmann H. Treatment of panniculitis in chronic pancreatitis by interventional endoscopy following extracorporeal lithotripsy. Gastrointest Endosc. 2001;53(1):104–7.
Azar L, Chatterjee S, Schils J. Pancreatitis, polyarthritis and panniculitis syndrome. Joint Bone Spine. 2014;81(2):184.
Kotilainen P, Saario R, Mattila K, Nylamo E, Aho H. Intraosseous fat necrosis simulating septic arthritis and osteomyelitis in a patient with chronic pancreatitis. Arch Orthop Trauma Surg. 1998;118(3):174–5.
Ohno Y, Le Pavoux A, Saeki H, Asahina A, Tamaki K. A case of subcutaneous nodular fat necrosis with lipase-secreting acinar cell carcinoma. Int J Dermatol. 2003;42(5):384–5.
Martinez-Mera C, Alfageme Roldán F, Suarez Massa D, Roustan Gullón G. Ultrasound of pancreatic panniculitis. Skin Res Technol. 2018;24(4):704–6.
Graham PM, Altman DA, Gildenberg SR. Panniculitis, pancreatitis, and polyarthritis: a rare clinical syndrome. Cutis. 2018;101(1):E34–e37.
Lengfeld J, Kneitz H, Goebeler M, Kolb-Mäurer A. Panniculitis due to pancreatic disease. J Dtsch Dermatol Ges. 2015;13(8):807–9.
King T, Rabindranathnambi R, Van Schalkwyk GS. An uncommon cause of panniculitis. Clin Exp Dermatol. 2018;43(3):351–3.
Tica I, Niculescu C, Mocanu L, Iliescu MG, Tica VI, Niculescu Z. Nodular subcutaneous lesion - an alarming sign for an upcoming pancreatic disorder. Romanian J Morphol Embryol. 2019;60(4):1343–7.
Kang DJ, Lee SJ, Choo HJ, Her M, Yoon HK. Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome: MRI features of intraosseous fat necrosis involving the feet and knees. Skelet Radiol. 2017;46(2):279–85.
Kim EJ, Park MS, Son HG, Oh WS, Moon KW, Park JM, Kang CD, Lee S. Pancreatitis, Panniculitis, and polyarthritis syndrome simulating cellulitis and gouty arthritis. Korean J Gastroenterol. 2019;74(3):175–82.
Beltraminelli HS, Buechner SA, Hausermann P. Pancreatic panniculitis in a patient with an acinar cell cystadenocarcinoma of the pancreas. Dermatology. 2004;208(3):265–7.
Acknowledgements
We greatly appreciated Drs. Keiko Shibata, Soichiro Shibata, Koujiro Tokutake, Toru Fujisawa, Hiromitsu Mori, and Yoshiaki Matsuda for their helping to see the patients as one team. We thank Trevor Ralph for his English editorial assistance.
Funding
N/A
Author information
Authors and Affiliations
Contributions
YY and SJ, conception and design of the research, and writing the paper; YY, TI, MM, SW, management of the case, making the clinical diagnosis and collection of all data; TI, MM, and SW, data interpretation; SJ and TU, revision of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval by committee was not required for this case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yamashita, Y., Joshita, S., Ito, T. et al. A case report of pancreatic panniculitis due to acute pancreatitis with intraductal papillary mucinous neoplasm. BMC Gastroenterol 20, 286 (2020). https://doi.org/10.1186/s12876-020-01430-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-020-01430-9