Abstract
Background
Rhabdomyosarcoma (RMS), especially primary pulmonary RMS, is an extremely rare type of soft tissue sarcoma in adults. Small bowel is an uncommon site for metastases.
Case presentation
This report described an unusual case of jejunum metastasis from primary pulmonary RMS causing intussusception in a 75-year-old man. The patient consulted for 2 weeks of continuous dyspnea. Chest computed tomography (CT) demonstrated a large mass involving the left lower lobe. Transthoracic biopsy confirmed the existence of pleomorphic RMS. Immunohistochemical studies showed positive findings about desmin and MyoD1. The results of gastroscopy, colonoscopy and abdominal CT were all negative. Positron emission tomography/CT demonstrated a fluorodeoxyglucose-reactive large lesion in the left lower lobe without metastatic lesions. The patient received synchronous chemoradiotherapy. After 9 months, the patient presented with intermittent upper abdominal pain with nausea and vomiting. CT showed small bowel dilatation secondary to intussusception. The patient subsequently received laparotomy, and the intussuscepted small bowel segment was resected. Histological examination revealed pleomorphic RMS involving the mucosa, submucosa, and muscular tissues.
Conclusions
RMS is highly aggressive and metastatic. The metastatic disease can rapidly progress to cause subsequent complications. The possibility of small bowel metastasis should be considered, although it is extremely rare.
Similar content being viewed by others
Background
Rhabdomyosarcoma (RMS) is a malignant skeletal muscle neoplasm. RMS is a common soft tissue sarcoma that occurs during childhood and adolescence, and it exists in the first 2 decades of life. By contrast, RMS is remarkably rare in adults. RMS accounts for < 1% of adult malignancies and < 3% of adult soft tissue sarcomas [1]. In addition, pleomorphic RMS is overrepresented in adult series. RMS in adults has a poor outcome compared with that in young individuals regardless of the implementation of multimodal therapies [2, 3]. RMS is commonly found in head and neck, genitourinary tract, and retroperitoneum [4]. Primary pulmonary rhabdomyosarcoma (PPR) is remarkably rare, and limited information about its clinicopathological features is reported in the literature [5,6,7,8]. RMS is highly invasive and metastatic. Metastases are mostly found in bones, bone marrows, lungs, or lymph nodes [9]. RMS metastases on the small bowel are few and far between. Herein, we present a case of jejunum metastasis due to PPR, causing intussusception in a 75-year-old man.
Case presentation
The subject was a 75-year-old man with chronic obstructive pulmonary disease for more than 20 years. The patient was a nonsmoker and had no history of other remarkable illnesses. The patient consulted due to 2 weeks of continuous dyspnea without fever, cough, hemoptysis, or chest pain. Lung auscultation revealed no wheezing sounds. Laboratory examinations, including complete blood count, electrolytes, renal function, liver function, and urinalysis, were negative. Chest computed tomography (CT) confirmed the presence of a large mass lesion of 5.8 cm × 4.4 cm that involves the left lower lobe (Fig. 1a and b). No lymphadenopathy or pleural effusion was observed. No mucosal lesions were identified through flexible fiberoptic bronchoscopy. CT-guided percutaneous transthoracic biopsy was conducted. Histological examination showed numerous compactly clustered small malignant cells with pleomorphism. A high mitotic rate was observed (Fig. 1c). Several rhabdomyoblasts were observed in the partial area. Immunohistochemistry showed that the cells were positive for desmin and MyoD1 and negative for c-KIT and S-100 protein, which were consistent with the diagnosis of pleomorphic RMS. Extension study was conducted through gastroscopy, colonoscopy, abdominal CT, and bone scan. The results were negative. The patient was referred for entire body fluorodeoxyglucose positron emission tomography (PET)/CT to exclude metastatic tumors. The result demonstrated a fluorodeoxyglucose-reactive large lesion in the left lower lobe with a maximum standardized uptake value of 12.8 without metastatic lesions. The patient could not bear surgical resection because of poor lung function. The patient received two cycles of vincristine/cyclophosphamide/actinomycin D chemotherapy combined with 40 Gy of intensity-modulated radiation therapy (IMRT). The patient opted to stop chemotherapy because of general weakness. After 6 months, abdominal ultrasound revealed large mass lesions in bilateral adrenal glands, which are suspected for metastasis, and the patient discontinued the therapy.
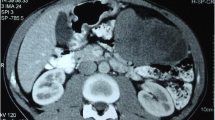
After 9 months, the patient was referred again to our hospital because of intermittent upper abdominal pain with nausea and vomiting. Physical examination showed that a large mass was palpable in the left abdomen. Bowel sounds were active. Laboratory data showed 2.1 mmol/L serum potassium. Abdominal CT showed small bowel dilatation secondary to entero-enteric intussusception (Fig. 2). The patient was given gastrointestinal decompression, potassium supplementation, and nutritional support treatment. Subsequently, laparotomy was performed, and a 15 cm segment of non-gangrenous intussusception was found in the jejunum with a 3 cm tumor forming the lead point of intussusception (Fig. 3a and b). No enlarged lymph nodes were observed in the mesentery of the affected small bowel. No other lesions were detected in the small bowel and colon. The affected segment of the small bowel was resected with end-to-end small bowel stapled anastomosis. Postoperative period was generally predictable. The histological examination of the surgical specimen revealed a pleomorphism malignant cell tumor that involved the mucosa, submucosa, and muscular tissues (Fig. 3c and d). Immunohistochemical studies were positive for desmin and MyoD1. These findings demonstrated that RMS originated in the lung. To date, the patient survived for 1 year after he was initially diagnosed and is currently under a good general condition.
a Intra-operative findings of jejuno-jejunal intussusception. b Intraluminal mass forming the pathologic lead point. c Histological examination of the surgical specimen with a pleomorphism malignant cell tumor that involves the mucosal, submucosal, and muscular tissues (hematoxylin and eosin stain, × 100). d Several mitoses are observed in one high-power field (hematoxylin and eosin stain, × 400)
Discussion and conclusions
RMS is a common soft tissue sarcoma in the pediatric population. RMS is initially believed to originate from skeletal muscles. However, RMS is currently known to arise from early rhabdomyoblasts that can be found in various locations throughout the body with varying degrees of differentiation [10]. RMS that originates from the lung is extremely rare. Limited information is reported about the clinicopathological features of adults with RMS in the literature. To our knowledge, only a limited number of studies focus on disease processes, diagnosis or treatment in children with rhabdomyosarcomas. Older patient age at presentation, unfavorable sites of the primary tumor, the size of the primary tumor, an alveolar subtype, and the presence of regional lymph node metastasis have been recognized as prognostic factors for rhabdomyosarcoma [11]. PPR should be diagnosed only after the possibility of metastatic RMS is excluded by extensive clinical examinations. In this case, the patient could not receive contrast-enhanced CT examination because of severe allergy to iodinated contrast medium. Extension study was achieved through gastroscopy, colonoscopy, abdominal CT, bone scan, and PET/CT to exclude metastatic tumors. The results were negative.
Approximately 20% of patients have distant metastases upon presentation, which is commonly found in lungs, bones, bone marrows, lymph nodes, and rare metastatic sites [11,12,13]. Metastases to the small bowel are extremely rare. This condition may be due to dense lymphatic tissues in the intestines, which contain a large amount of T lymphocytes. The general route of small bowel metastasis is believed to be hematogenous in the spinal vein, retroperitoneal mediastinum, and lymphatic metastasis of the mesentery. Most small bowel metastases are caused by primary tumors, such as malignant melanoma, colon cancer, and cervical cancer [14]. The prognosis of patients with small bowel metastases is fairly poor, and most of them are found in serious complications, such as perforation, obstruction, and hemorrhage. Intussusception is rare in adults, and most cases are due to a pathologic lead point within the bowel and are malignant in more than 50% of cases, which require surgery and resection of the affected bowel segment. The common cause of malignant lesions is mainly primary tumor, and limited reports are available about intussusception secondary to small bowel metastases [15, 16].
The incidence of small bowel metastases is low, and misdiagnosis and missed diagnosis easily occur due to nonspecific symptoms. We reported the second case of small bowel intussusception caused by PPR metastasis, suggesting that the possibility of metastasis should be considered regardless of the rarity or site location [17]. Intussusception in adults should be investigated. In exploratory laparotomy, the intestinal tube should be thoroughly examined in terms of the presence of neoplastic lesions.
Abbreviations
- CT:
-
Computed tomography
- IMRT:
-
Intensity-modulated radiation therapy
- PET:
-
Positron emission tomography
- PPR:
-
Primary pulmonary rhabdomyosarcoma
- RMS:
-
Rhabdomyosarcoma
References
Nascimento AF. Rhabdomyosarcomas in adults: classification and differential diagnosis. Diagnostic Histopathology. 2008;14(11):538–45.
Fischer TD, Gaitonde SG, Bandera BC, et al. Pediatric-protocol of multimodal therapy is associated with improved survival in AYAs and adults with rhabdomyosarcoma. Surgery. 2018;163(2):324–9.
Dumont SN, Araujo DM, Munsell MF, et al. Management and outcome of 239 adolescent and adult rhabdomyosarcoma patients. Cancer Med. 2013;2(4):553–63.
Wasti AT, Mandeville H, Gatz S, et al. Rhabdomyosarcoma. Paediatr Child Health. 2018;28(4):157–63.
Choi JS, Choi JS, Kim EJ. Primary pulmonary rhabdomyosarcoma in an adult with neurofibromatosis-1. Ann Thorac Surg. 2009;88(4):1356–8.
Gupta A, Sharma MC, Kochupillai V, et al. Primary pulmonary rhabdomyosarcoma in adults: case report and review of literature. Clin Lung Cancer. 2007;8(6):389–91.
Gray JA, Nguyen GK. Primary pulmonary rhabdomyosarcoma diagnosed by fine-needle aspiration cytology. Diagn Cytopathol. 2003;29(3):181–2.
Comin CE, Santucci M, Novelli L, et al. Primary pulmonary rhabdomyosarcoma: report of a case in an adult and review of the literature. Ultrastruct Pathol. 2001;25(3):269–73.
Ferrari A, Dileo P, Casanova M, et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer. 2003;98(3):571–80.
Parham DM, Ellison DA. Rhabdomyosarcomas in adults and children: an update. Arch Pathol Lab Med. 2006;130:1454–65.
Kim JR, Yoon HM, Koh KN, et al. Rhabdomyosarcoma in children and adolescents: patterns and risk factors of distant metastasis. AJR Am J Roentgenol. 2017;209(2):409–16.
Ismail E, Issam L, Hamid M. Pituitary metastasis of rhabdomyosarcoma: a case report and review of the literature. J Med Case Rep. 2014;8:144.
Elomrani F, Touri S, Ouziane I, et al. Orbital rhabdomyosarcoma with skin metastasis: a case report. BMC Res Notes. 2014;7:670.
Marko L, Veronique B, Zoran K. Melanoma of the small intestine. The Lancet Oncology. 2009;10(5):516–21.
Kim HS, Shin JW, Kim GY, et al. Metastasis of hepatocellular carcinoma to the small bowel manifested by intussusception. World J Gastroenterol. 2006;12(12):1969–71.
Tan QT, Teo JY, Ahmed SS, et al. A case of small bowel metastasis from spinal Ewing sarcoma causing intussusception in an adult female. World J Surg Oncol. 2016;14:109.
Xi S, Tong W. Pleomorphic rhabdomyosarcoma metastasis to small intestine causing intussusception: a case report. Medicine (Baltimore) 2018; 97(51): e13648.
Acknowledgments
We would like to thank colleagues at the department of radiology and pathology in our hospital for providing the data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
XJ S supervised all aspects of this research, and KK S prepared the manuscript. Both authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was undertaken under the guidelines of the Ethics Committee of Jiangsu University. The authors have declared no ethical conflicts.
Consent for publication
Written informed consent of publication was obtained from the patient in the study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sun, Kk., Shen, Xj. Small bowel metastasis from pulmonary rhabdomyosarcoma causing intussusception: a case report. BMC Gastroenterol 19, 71 (2019). https://doi.org/10.1186/s12876-019-0990-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-019-0990-4