Abstract
Background
IgG4-related disease (IgG4-RD) is a newly recognized autoimmune systemic disorder characterized by elevated levels of serum IgG4 and abundant infiltration of IgG4-positive plasmacytes in the affected organs. The liver, biliary system and pancreas are the most commonly affected organs. However, involvement of the digestive tract is very rare. To date, only a few cases of isolated gastric IgG4-RD have been reported.
Case presentation
We present a case of IgG4-RD of the liver, gallbladder, pancreas and duodenum, which was clinically misinterpreted and thereafter over-treated. A 52-year-old male presented with obstructive jaundice for 3 years, melena for 5 months and hematemesis for 10 days. Three years prior, the patient had undergone biopsies of pancreatic lesions, liver lesions, cholecystectomy and choledochojejunostomy. Histopathology showed chronic inflammatory changes. Endoscopy at admission revealed a duodenal ulcer with active bleeding. Despite medical management, the patient presented with repeated gastrointestinal bleeding. Upon evaluation, serum IgG4 levels were found to be elevated. Histopathology of the duodenal ulcer biopsy and repeated examination of the gallbladder and pancreatic and liver biopsies confirmed IgG4 positive plasma cell infiltration. A definitive diagnosis of IgG4-RD was made and steroid administration was initiated. At last follow up, 11 months to-the-day after initiating steroid treatment, the patient was asymptomatic.
Conclusions
Notably, IgG4-RD of multiple digestive organs is still very rare. As a systemic disease, it is characterized by the infiltration of IgG4-bearing plasma cells and raised IgG4 levels. Histopathology findings remain the diagnostic gold standard for this disorder.
Similar content being viewed by others
Background
IgG4-related disease (IgG4-RD) is a relatively recently recognized chronic multi-organ autoimmune disease of unknown origin with a tendency to develop lesions at multiple sites throughout the body [1]. It is known to affect various organs including the bile duct, pancreas, gallbladder, liver, lungs and salivary glands. It is characterized by elevated IgG4 levels in the serum and the affected tissues, lymphoproliferative infiltration and sclerotic fibrosis [2, 3]. Other typical features are occlusive phlebitis and rising IgG4-plasma cells levels [4, 5]. Clinically, it mimics malignancy in some patients, especially those with liver and pancreatic lesions and is often thought to necessitate surgical resection, sometimes leading to over-treatment [6, 7]. To date, only a few isolated cases of digestive IgG4-RD have been reported.
Case presentation
A 52-year-old male from southwest China presented with obstructive jaundice for 3 years, melena for 5 months and hematemesis for 10 days. The patient had been diagnosed with type 2 diabetes mellitus for 4 years, which was treated with metformin. The patient was a chronic tobacco (10 cigarettes per day) and alcohol consumer over the previous 20 years but had quit smoking and drinking for the past 3 years. Three years prior to admission to our hospital, he developed obstructive jaundice, which was investigated with abdominal computed tomography (CT) and revealed multiple hypodense lesions in the liver and pancreatic head mass. He underwent cholecystectomy, choledochojejunostomy and biopsies from the liver and pancreatic lesions. Histopathology revealed chronic cholecystitis with lymphocytic, plasmacytic and eosinophilic infiltration of the gallbladder, liver and pancreatic parenchyma.
The physical examination was unremarkable (height − 165 cm, weight – 50 kg). Laboratory tests revealed hemoglobin levels of 75 g/L, a platelet count of 80 × 109/L, 30.0 g/L albumin levels, and serum potassium levels of 3.20 mmol/L (Table 1). The fecal occult blood was positive.
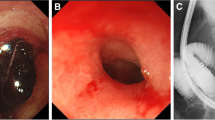
On the day of admission, the patient developed repeated painless hematemesis of about 2100 mL, which was associated with hypotension and tachycardia. He was resuscitated with intravenous, blood and norepinephrine infusions. Laboratory tests revealed hemoglobin levels of 47.5 g/L, platelet count levels of 38 × 109 L and serum albumin 25.8 g /L. The day after admission, the patient again developed hematemesis of about 500 mL, for which he was treated with somatostatin, terlipressin and pantoprazole infusion. Sengstaken-Blakemore tube were placed to hemostasis by compression and tube feeding hemostatic medicine. After 4 days of medical intervention, the patient’s gastrointestinal bleeding gradually stopped. Esophagogastroduodenoscopy revealed a duodenal ulcer (A1 stage) with active bleeding, gastric mucosal erosions and esophageal varices (mild). Contrast enhanced computed tomography of the abdomen with three-dimensional reconstruction exposed multiple nodular dense shadows with dilatation of the main pancreatic duct in the tail region (Fig. 1d). Images of the liver showed numerous hypodense nodules with mild contrast enhancement, ascites and intrahepatic bile duct dilatation (Fig. 1a). Additionally, there were multiple enlarged lymph nodes in the hepatoduodenal ligament around the abdominal aorta (Fig. 1b) and mesenteric lymph nodes with bilateral pleural effusion (Fig. 1c). In view of the liver disease with portal hypertension and esophagogastric varices, a transjugular intrahepatic portosystemic shunt (TIPS) procedure was performed under local anesthesia and regional portal hypertension, splenic vein and portal vein obstruction were detected. Subsequently, the patient re-bleed both 14 days and 20 days after admission, about 600 mL and 400 mL, respectively. The patient was treated with somatostatin, pantoprazole infusion and blood transfusion. Gastroscopy identified an ulcer (1.5 cm × 1.2 cm) in the anterior wall of the duodenal bulb that was not actively bleeding (Fig. 2a, Fig. 2b). Pathological examination of the ulcer biopsy verified a moderate degree of chronic mucosal inflammation.
Abdominal computed tomography. Images of the liver showed numerous hypodense nodules with mild contrast enhancement, ascites and intrahepatic bile duct dilatation (a). There were multiple enlarged lymph nodes in the hepatoduodenal ligament around the abdominal aorta (b). Mesenteric lymph nodes with bilateral pleural effusion (c). Multiple nodular dense shadows with dilatation of the main pancreatic duct in the tail region (d)
When investigating the recurrent bleeds, serum IgG4(0.035–1.500 g/L)and IgG(8~ 15.5 g/L)were found to be 29.200 g/L and 24.50 g/ L respectively and IgG4 disease was suspected (Table 1). The patient’s prior surgical pathology specimens were retrieved for IgG4 immunohistochemical examination. Immunohistochemical staining revealed increased IgG-positive and IgG4-positive plasma cells in the liver lesions (IgG4 positive cells 30–60/ high power field (HPF); Fig. 3b), pancreas (IgG4 positive cells 30–80/HPF; Fig. 3d) and gallbladder (IgG4 positive cells 30–80/HPF; Fig. 3f). Staining of the duodenum ulcer biopsy also showed more than 100 IgG4-positive cells per HPF (Fig. 3h). Based on these findings, a definitive diagnosis of IgG4-RD was made.
Pathologic findings. a Diaminobenzidine staining of liver specimens revealed focal necrosis of the liver surrounded by fibrous tissue. The focal necrosis area revealed infiltration by lymphocytes, plasma cells and eosinophils. Peripheral hepatocytes were partially silt. b Immunoglobulin G (IgG) immunohistochemical staining showing increased numbers of IgG-positive plasma cells in the liver lesions (30–60/ high power field [HPF], × 400). c Diaminobenzidine staining of pancreas tissues revealed focal areas of glandular atrophy accompanied by lymphocyte, plasma cell and eosinophil infiltration and fibrous tissue hyperplasia. d IgG immunohistochemical staining showing increased numbers of IgG-positive plasma cells in the pancreas (30–80/HPF, × 400). e Diaminobenzidine staining of gallbladder tissue revealed chronic cholecystitis, focal lymphoid hyperplasia, formation of lymph follicles and infiltration of the gallbladder wall by the lymphocytes, plasma cells and eosinophils. f IgG immunohistochemical staining showing increased numbers of IgG-positive plasma cells in the gallbladder (30–80/HPF, × 400). g Hematin and yepin staining of duodenum tissue revealed lymphocytic, plasmacytic and neutrophilic infiltration of the inner layer of the duodenal mucosa with congestion and dilatation of the blood vessels. h IgG immunohistochemical staining showing increased numbers of IgG-positive plasma cells in the duodenum (> 100 /HPF, × 400)
The patient was administered 40 mg/d prednisone intravenously for 7 days without any side effects followed by oral prednisolone 40 mg/d for 1 week. Laboratory tests indicated a reduction in the serum IgG4 levels 8 days after initiating prednisone but the liver function continued to be impaired (Table 1). As the patient improved symptomatically, he was discharged on a regime of prednisolone and mycophenolate mofetil.
Since discharge until the time of writing, during the 11 monthly visits since starting steroid therapy, laboratory tests indicate significant improvements in the patient’s serum IgG4 subtype, liver function and hemogram tests (Table 1).
Discussion and conclusions
IgG4-RD was first described in patients with sclerosing cholangitis, known as autoimmune pancreatitis (AIP) type I. Subsequently, IgG4-RD was found to affect other organs [6]. At present IgG4-RD is believed to be a systemic disease and diagnostic criteria for IgG4-RD [8, 9] include: (1) single or multiple organs with diffuse or localized swelling, masses, nodules and/or hypertrophic lesions; (2) elevated serum IgG4 levels (≥135 mg/dL); and (3) histopathologic features that include marked lymphocytic and plasma cell infiltration and fibrosis, with IgG4-positive plasma cell infiltration (IgG4/IgG positive cell ratio of 40% and IgG4-positive plasma cells exceeding 10/HPF). Diagnosis of IgG4-related is confirmed when all of the following are fulfilled: (1), (2) and (3). Diagnosis is likely if criteria (1) + (3) are fulfilled, possible if (1) + (2) are fulfilled and unlikely if only (1) presents.
Notably, the biliary tract and pancreas are the organs most frequently affected by IgG4-RD [10]. Few studies have reported isolated cases of IgG4-RD in other digestive organs, such as in the esophagus, stomach, liver or duodenum [7].
A recent review of IgG4-RD cases reporting on gastrointestinal lesions showed that most patients present with multiple organ disease involvement, including the stomach, duodenum, liver, bile duct, esophagus, jejunum, lymph nodes and pancreas (Table 2). Six patients presented with obstructive jaundice as the main clinical manifestation [11,12,13,14,15,16] and others presented with varied clinical symptoms [17,18,19,20,21,22,23,24,25,26,27,28]. Gastrointestinal bleeding was not reported in any of the studies. Our patient had recurrent gastrointestinal bleeding due to a duodenal ulcer. The ulcer failed to heal with standard treatment. Serum IgG4 was elevated in most of the cases reviewed, similar to our case, though was normal in three reports [11, 13, 17] and was not reported in two cases [11, 18]. The diagnosis of IgG4-RD was based on a combination of features that include clinical parameters, serology, immunohistochemistry, imaging and histopathology. In the present case, the diagnosis of IgG4-RD was initially missed in the histological analysis of the liver and pancreatic biopsy and gallbladder samples. When IgG4-RD was suspected based on the clinical and laboratory findings, IgG4 immunostaining was undertaken and the IgG4-RD diagnosis was confirmed. In our literature review, there were eight patients treated through surgery, 10 patients by corticosteroids, two were given corticosteroids after surgery, and in two patient studies, the treatment course was not reported (Table 2). Our patient responded partially to steroid therapy and required other immunosuppressive agents for a complete and successful response.
IgG4-RD can affect multiple gastrointestinal organs simultaneously or over different time periods. The clinical manifestations can mimic malignancy or other benign diseases such as portal hypertension, acid peptic disease. A high index of suspicion is required to make an accurate diagnosis and avoid unnecessary surgical interventions.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase; ALB: albumin
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- DBIL:
-
Direct bilirubin
- ERCP:
-
Endoscopic retrograde cholangiography;
- HGB:
-
Hemoglobin
- IgG:
-
Immunoglobulin G
- IgG4:
-
Immunoglobulin G4 subtype
- IgG4-RD:
-
IgG4-related disease
- MRI:
-
Magnetic resonance imaging; PET: positron emission tomography
- PLT:
-
Platelet
- TBIL:
-
Total bilirubin
References
Decker L, Crawford AM. Orenzo GL, et al. IgG4-related Hypophysitis: case report and literature review. Cureus. 2016;8:e907.
Zhang W, Xue F, Liu MC, et al. 36 cases IgG4 related clinical analysis. [Chinese] Chinese. Journal of Nephrology. 2016;32:253–8.
Li YM, Wang H, Fang F, et al. IgG4 related clinical feature analysis. [Chinese] National Medical Journal of China. 2015;95:3281–4.
Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366:539–51.
Woo CG, Yook JH, Kim AY, et al. IgG4-related disease presented as a muralmass in the stomach. J Pathol Transl Med. 2016;50:67–70.
Masaki Y, Shimizu H, Nakamura TS, et al. IgG4-related disease: diagnostic methods and therapeutic strategies in Japan. J Clin Exp Hematop. 2014;54:95–101.
Koizumi S, Kamisawa T, Kuruma S, et al. Immunoglobulin G4-related gastrointestinal diseases, are they immunoglobulin G4-related diseases. WJG. 2013;19:5769–74.
Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Modern Rheumatology. 2012;22:21–30.
Umemura T, Zen Y. IgG4-related Hepatopathy. In: Umehara H, Okazaki K, Stone J, Kawa S, Kawano M, editors. IgG4-Related Disease. Tokyo: Springer; 2014. p. 205–9.
Hubers LM, Maillette de Buy LJ, Wenniger ME, et al. IgG4-associated cholangitis: a comprehensive review. Clin Rev Allergy Immunol. 2015;48:198–206.
Fong WW, Thumboo J, Azhar R, et al. IgG4-related disease in Singapore: a description of two cases and review of the literature. Int J Rheum Dis. 2013;16:93–7.
Rungsakulkij N, Sornmayura P, Tannaphai P, et al. Isolated IgG4-related sclerosing cholangitis misdiagnosed as malignancy in an area with endemic cholangiocarcinoma: a case report. BMC Surg. 2017;17:17.
Cai J, Mou YP, Pan Y, et al. Immunoglobulin G4-associated cholangitis mimicking cholangiocarcinoma treated by laparoscopic choledochectomy with intracorporeal roux-en-Y hepaticojejunostomy. World J Surg Oncol. 2014;12:363.
Euch ME, Hddad S, Mahfoudhi M, et al. A case of type 1 autoimmune pancreatitis (AIP), a form of IgG4-related disease (IgG4-RD). Am J Case Rep. 2017;18:822–5.
Miki A, Sakuma Y, Ohzawa H, et al. Immunoglobulin G4-related sclerosing cholangitis mimicking hilar cholangiocarcinoma diagnosed with following bile duct resection: report of a case. Int Surg. 2015;100:480–5.
Sivakumaran Y, Le Page PA, Becerril-Martinez G, et al. IgG4-related sclerosing cholangitis: the cholangiocarcinoma mimic. ANZ J Surg. 2014;84:486–7.
Rodriguez EA, Williams FK. A mass in the junction of the body and tail of the pancreas with negative IgG4 serology: IgG4-related disease with negative serology. Am J Case Rep. 2015;16:305–9.
Kondo T, Uehara T. Immunoglobulin G4-related disease with fibroinflammatory lesions in the pleura, bile ducts and pericardium. CMAJ. 2016;188:972.
Yang L, Jin P, Sheng JQ. Immunoglobulin G4-related disease (IgG4-RD) affecting the esophagus, stomach,and liver. Endoscopy. 2015;47:E96–7.
Miyajima S, Okano A, Ohana M. Immunoglobulin G4-related hepatic inflammatory pseudotumor invading the abdominal wall. Clin J Gastroenterol. 2017;10:57–62.
Li Y, Zhou L, Zhao X, et al. The importance of IgG4 screening in patients diagnosed with primary sclerosing cholangitis in the past: a case rediagnosed as IgG4-SC after 10 years. Medicine (Baltimore). 2016;95(50):e5628.
Chen CT, Chiang CL, Huang HH. IgG4-related double duct sign mimicking pancreatic head cancer. QJM. 2016;109:207–8.
Inoue K, Okubo T, Kato T, et al. IgG4-related stomach muscle lesion with a renal pseudotumor and multiple renal rim-like lesions: A rare manifestation of IgG4-related disease. Mod Rheumatol. 2018;28:188–92.
Bulanov D, Arabadzhieva E, Bonev S, et al. A rare case of IgG4-related disease: a gastric mass, associated with regional lymphadenopathy. BMC Surg. 2016;16:37.
Takasumi M, Miyata M, Kuroda M, et al. Overlap of IgG4-related disease and primary biliary cirrhosis complicated with autoimmune thrombocytopenia. Internal Med. 2016;55:1387–92.
Kim S, Bae H, Choi M, et al. Isolated mass-forming IgG4-related cholangitis as an initial clinical presentation of systemic IgG4-related disease. J Pathol Transl Med. 2016;50:300–5.
Matsunaga K, Hayashi R, Otsuka T, et al. A case of IgG4-related disease complicated by duodenal bulbitis with IgG4-positive plasma cell infiltration. Endoscopy. 2014;46:E408–10.
Van de Ven AAJM, Seidl M, Drendel V, et al. IgG4-related disease in autoimmune lymphoproliferative syndrome. Clin Immunol. 2017;180:97–9.
Acknowledgements
We are grateful to Prof. Yin Gen of the Department of General Medicine, West China Hospital of Sichuan University for her contribution to the case.
Availability of data and materials
All data used and analysed during this study available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
DXX wrote the manuscript under the close supervision of FRH. FRH guaranteed the integrity of entire study. DXX prepared the literature search. DXX and FRH designed the study preliminarily and contributed to data acquisition and data analysis. ZJS and LRQ participated in the design and coordination of the study. All authors critically revised the manuscript and approved it.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article is a retrospective study and does not contain any studies with human subjects performed by any of the authors. So, the ethical approval was not necessary and West China Hospital of Sichuan University ethics committee can offer exempt ethical statement in support.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Deng, X., Fang, R., Zhang, J. et al. Multivisceral IgG4-related disease presenting as recurrent massive gastrointestinal bleeding: a case report and literature review. BMC Gastroenterol 18, 136 (2018). https://doi.org/10.1186/s12876-018-0867-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-018-0867-y