Abstract
Background
Delayed gastric emptying (DGE) is one of the most frequent complications after pancreaticoduodenectomy (PD). This meta-analysis aimed to evaluate the effect of antecolic versus retrocolic reconstruction of gastro/duodenojejunostomy on DGE after PD.
Methods
Randomized controlled trials (RCTs) comparing antecolic versus retrocolic reconstruction of gastro/duodenojejunostomy on DGE after PD were eligible for inclusion. Pooled estimates of treatment effect were calculated using either the fixed effects model or random effects model.
Results
Five RCTs involving 534 randomized patients were eligible. The comparison of DGE showed no significant difference (odds ratio, 0.66; 95 % confidence interval, 0.32 to 1.33; P = 0.24). The antecolic and retrocolic groups also had comparable outcomes for clinical parameters related to DGE, other complications, hospital mortality, and length of hospital stay.
Conclusions
The route of gastro/duodenojejunostomy reconstruction has no impact on DGE after PD. Therefore, the choice of reconstruction route should be selected according to the surgeon’s preference.
Similar content being viewed by others
Background
With the refinements in surgical techniques, improvements in perioperative management, advancements in surgical instruments, pancreaticoduodenectomy (PD) has become a safer procedure with a reported operative mortality less than 5 % at high-volume centres. However, the incidence of morbidity approaches 30–65 % [1]. Delayed gastric emptying (DGE) is one of the most frequent morbidity after PD occurring in 19–57 % of patients [2]. It has been associated with longer duration of hospitalization and higher hospital costs.
Two reconstruction routes are usually used for gastro/duodenojejunostomy: the antecolic route or the retrocolic route. A meta-analysis published by Su et al [3] compared 5 studies [4–8] and concluded that antecolic reconstruction route was associated with a statistically significant decrease in the incidence of DGE following PD. However, this meta-analysis included three observational studies [4–6], which may introduce confounding and selection bias that often distort the findings. The randomised controlled trial (RCT) is the principal research design in the evaluation of medical interventions and is best confined to meta-analysis [9]. More recently, four RCTs have become available and reported that the route of gastro/duodenojejunostomy reconstruction does not influence the postoperative incidence of DGE or other complications after PD [10–13]. Therefore, the present meta-analysis provides an updated evaluation by pooling data that only come from the RCTs.
Methods
The study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) [14].
Study selection
Using Medline, EMBASE, OVID, and Cochrane database, a literature search was made for RCTs that evaluated the influence of an antecolic with a retrocolic gastro/duodenojejunostomy reconstruction on DGE after PD from the time of inception to November 2013. The Medical Subject Heading (MeSH) search terms were “pancreaticoduodenectomy” and “delayed gastric emptying.” Only studies on humans and in the English language were considered for inclusion. Reference lists of all retrieved articles were manually searched for additional studies.
Data extraction
Two reviewers (B.L. and L.W., respectively) independently extracted the following parameters from each study: first author, year of publication, study population characteristics, number of patients randomized with each procedure, and endpoints. All relevant text, tables and figures were reviewed for data extraction.
Criteria for inclusion and exclusion
RCTs that evaluated the influence of an antecolic with a retrocolic gastro/duodenojejunostomy reconstruction on DGE after PD were included in the study. Exclusion criteria were: animal studies, abstracts, letters, proceedings from scientific meetings, editorials and expert opinions, and non-randomized observational clinical studies.
Assessment of methodological quality
The RCTs were scored using the Jadad composite scale [15] in which each study was evaluated by examining 3 factors: randomization, blinding, and withdrawals and drop-outs reported within the study period. The quality scale ranges from 0 to 5 points, study having 3 or more score was considered to be of higher quality.
Endpoints
Primary endpoint was DGE. Secondary endpoints included other complications and length of hospital stay.
Statistical methods
Review Manager (RevMan) software 5.0 (Cochrane Collaboration) was used to conduct all analyses. Estimated effect measures were odds ratios (OR) for dichotomous variables and weighted mean difference (WMD) for continuous variables. If the study provided medians and interquartile ranges instead of means and SDs, the means and SDs were imputed according to the methods described by Hozo et al. [16] Pooled estimates were presented with 95 % confidence intervals (95 % CI). Pooled effect was calculated using either the fixed effects model or random effects model. Heterogeneity was evaluated by I2, with values over 50 % indicating considerable heterogeneity. Publication bias was assessed visually using a funnel plot, based on the result of DGE.
Results
Eligible studies
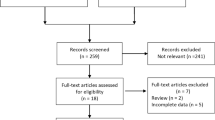
The process of identifying eligible literatures is shown in Fig. 1. The search strategy generated 6 RCTs. Two studies from the same group [8, 11], the most recent study that including more subjects was selected [11]. Finally, five articles were identified for inclusion [7, 10–13]. The two reviewers had 100 % agreement in their reviews of the data extraction.
A total of 534 patients were included in the meta-analysis: 267 in the antecolic group and 267 in the retrocolic group. Two studies were conducted in Japan [7, 11], one in India [10], one in the Netherlands [12], and one in Austria [13]. The sample size of each study varied from 40 to 246 patients. The characteristics of the included studies are shown in Table 1.
Outcomes assessed
Table 2 shows the results for the outcomes.
All studies provided information on the incidence of DGE, which occurred in 37.1 % of patients in the antecolic group versus 43.1 % of patients in the retrocolic group. Polled analysis showed that there was no significant difference between groups (OR 0.66, 95 % CI, 0.32 to 1.33; P = 0.24). Considerable heterogeneity was detected between studies (I2 = 57 %) (Fig. 2). In three studies [10–12], DGE was defined and graded according to the recommendations of the International Study Group of Pancreatic Surgery (ISGPS) [17]. Pooled analysis showed both overall DGE (OR 0.97, 95 % CI, 0.64 to 1.47; P = 0.89) and clinically significant DGE (grade B or C) (OR 0.93, 95 % CI, 0.60 to 1.46 P = 0.76) were not different with no significant heterogeneity.
Measures of the clinical parameters related to DGE were all comparable between groups: namely, time of removal of nasogastric tube (WMD 0.38, 95 % CI, -0.30 to 1.06; P = 0.27), requirement for reinsertion of nasogastric tube (OR 1.14, 95 % CI, 0.73 to 1.81; P = 0.56), requirement of prokinetics or anti/emetics(OR 0.84, 95 % CI, 0.53 to 1.32; P = 0.45), time of start of liquid diet (WMD 0.26, 95 % CI, -0.63 to 1.16; P = 0.56), and time of start of solid diet (WMD -0.90, 95 % CI, -1.91 to 0.10; P = 0.08). No significant heterogeneity was found between studies regarding these outcomes, except for the time of removal of nasogastric tube .
Measures of secondary endpoints were also not significantly different between the two groups: namely, pancreatic fistula (OR 1.05, 95 % CI, 0.69 to 1.61; P = 0.80) (Fig. 3), intra-abdominal abscess (OR 1.04, 95 % CI, 0.62 to 1.75; P = 0.88) (Fig. 4), hemorrhage (OR 0.74, 95 % CI, 0.37 to 1.48; P = 0.40) (Fig. 5), bile leakage (OR 1.09, 95 % CI, 0.48 to 2.51; P = 0.83) (Fig. 6), wound infection (OR 0.92, 95 % CI, 0.60 to 1.40; P = 0.70) (Fig. 7), reoperation (OR 0.49, 95 % CI, 0.22 to 1.09; P = 0.08) (Fig. 8), hospital mortality (OR 0.60, (95 % CI, 0.22 to 1.64; P = 0.32) (Fig. 9), and length of hospital stay (WMD 0.44, 95 % CI, -0.30 to 1.17; P = 0.25) (Fig. 10). No significant heterogeneity was found between studies regarding these outcomes.
Publication bias
The funnel plot for the primary outcome (DGE) was asymmetric, indicating the presence of publication bias (Fig. 11).
Discussion
DGE after PD is a frequent complication, which is usually managed by nasogastric drainage and nutritional support by parenteral or enteral routes, with or without prokinetics. Many efforts for reducing the incidence of DGE have been attempted; these include pyloric dilation [18], preservation of the left gastric vein [19], preoperative use of erythromycin [20], and prophylactic octreotide [21]. Other studies evaluated the clinical efficacy of reconstruction procedure of gastric emptying. As compared with Billroth II reconstruction, both Roux-en-Y and Billroth-I reconstructions were found to be associated with higher incidence of DGE [22, 23]. Two routes are usually used for Billroth II reconstruction after PD: the antecolic route or the retrocolic route. A meta-analysis reported the superiority of the antecolic route compared with the retrocolic route concerning the reduction of DGE [3]. However, a significant proportion of data in this meta-analysis came from nonrandomized studies, which may introduce confounding and selection bias that often distort the findings.
The present updated meta-analysis pooled five RCTs and provided clearly the best available evidence on the effect of reconstruction route concerning DGE. In contrast with previously published meta-analysis, the main finding is that the two routes after PD were equally efficient concerning DGE. There is wide variation definition of a DGE in the pancreatic surgery literature. In 2007, the ISGPS proposed a standardized definition of DGE [17]. Three of 5 RCTs used the ISGPS criteria and consistently found that the route of gastro/duodenojejunostomy reconstruction had no significant impact on the incidence and severity of DGE. The pooled data is also in concordance with these RCTs.
The pathogenesis of DGE after pancreatoduodenectomy has been proposed to be multifactorial: disruption of the vagal nerve system; ischemic injury to the antropyloric mechanism; and decreased plasma motilin stimulation caused by resection of the duodenum [20]. From a mechanical point of view, some researchers observed that a transient torsion or angulation of the reconstructed alimentary tract might contribute to DGE [24]. With antecolic reconstruction, the duodenal stump or distal stomach and the descending jejunal loop are set in a straight line. Torsion or angulation of the reconstructed alimentary tract can thus be avoided [25]. However, in case of retrocolic reconstruction, the risk of torsion or angulation can be diminished by suturing the duodenum or distal stomach to the transverse mesocolon [12]. Thus, one can understand that the reconstruction route has no measurable impact on the incidence and severity of DGE.
Regarding the operative technique, it has been suggested that DGE more likely occurs in patients who underwent pylorus-preserving pancreaticoduodenectomy (PPPD) (in comparison with classic Whipple PD). However, a recent meta-analysis of six RCTs showed an overall comparable rate of DGE for both techniques. [26] Also, the type of pancreatic anastomosis (pancreaticogastrostomy and pancreaticojejunostomy) was not significantly associated with DGE [27]. By contrast, there are growing evidences that other intraabdominal complications, such as pancreatic fistula, biliary fistula, intraabdominal collections or abscesses, have a critically influence on DGE. Park et al [28] found that DGE was significantly more frequent among patients with postoperative intraabdominal complications (41.7 % versus 8.8 %; P<0.0001). Similarly, in another report by Horstmann et al [29], DGE almost exclusively occurs as a consequence of other postoperative complications. These findings are supported by those of other reports [21, 30]. Hence, prevention of such complications might reduce the incidence of DGE.
This present analysis has some limitations. First, considerable heterogeneity was detected between studies regarding primary endpoint. The presence of heterogeneity is due to paper by Tani et al [7] in which incidence of DGE of 5 % in their antecolic group compared to 50 % in the retrocolic group (P<0.001). Apart from the fact that there were only 20 patients in each arm in this study, a total of 12/20 patients in the retrocolic group had at least one postoperative complication as compared to 3/20 in the antecolic group might have influenced their results [10]. Second, the number of studies included in this meta-analysis is small. Indeed, randomised trials in surgery are difficult to conduct [31]. Finally, funnel plot analysis suggested the possibility of publication biases. This may relate to our inclusion of English only studies.
Conclusions
Our meta-analysis did not observe a significant effect of the kind of reconstruction route on the incidence of DGE after PD. Moreover, we did not find any differences in terms of hospital stay, other complications, and mortality between two groups, underlining the safety of both procedures. Therefore, the choice of reconstruction route should be selected according to the surgeon’s preference.
References
Kawai M, Yamaue H. Analysis of clinical trials evaluating complications after pancreaticoduodenectomy: a new era of pancreatic surgery. Surg Today. 2010;40:1011–7.
Nikfarjam M, Kimchi ET, Gusani NJ, et al. A reduction in delayed gastric emptying by classic pancreaticoduodenectomy with an antecolic gastrojejunal anastomosis and a retrogastric omental patch. J Gastrointest Surg. 2009;13:1674–82.
Su AP, Cao SS, Zhang Y, et al. Does antecolic reconstruction for duodenojejunostomy improve delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? A systematic review and meta-analysis. World J Gastroenterol. 2012;18:6315–623.
Kurosaki I, Hatakeyama K. Clinical and surgical factors influencing delayed gastric emptying after pyloric-preserving pancreaticoduodenectomy. Hepatogastroenterology. 2005;52:143–8.
Murakami Y, Uemura K, Sudo T, et al. An antecolic Roux-en Y type reconstruction decreased delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Gastrointest Surg. 2008;12:1081–6.
Hartel M, Wente MN, Hinz U, et al. Effect of antecolic reconstruction on delayed gastric emptying after the pylorus-preserving Whipple procedure. Arch Surg. 2005;140:1094–9.
Tani M, Terasawa H, Kawai M, et al. Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg. 2006;243:316–20.
Chijiiwa K, Imamura N, Ohuchida J, et al. Prospective randomized controlled study of gastric emptying assessed by (13)C-acetate breath test after pylorus-preserving pancreaticoduodenectomy: comparison between antecolic and vertical retrocolic duodenojejunostomy. J Hepatobiliary Pancreat Surg. 2009;16:49–55.
Egger M, Schneider M, Davey Smith G. Spurious precision? Meta-analysis of observational studies. BMJ. 1998;316:140–14.
Gangavatiker R, Pal S, Javed A, et al. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled trial. J Gastrointest Surg. 2011;15:843–52.
Imamura N, Chijiiwa K, Ohuchida J, et al. Prospective randomized clinical trial of a change in gastric emptying and nutritional status after a pylorus-preserving pancreaticoduodenectomy: comparison between an antecolic and a vertical retrocolic duodenojejunostomy. HPB (Oxford) 2013. [Epub ahead of print]
Eshuis WJ, van Eijck CH, Gerhards MF, et al. Antecolic versus retrocolic route of the gastroenteric anastomosis after pancreatoduodenectomy: a randomized controlled trial. Ann Surg. 2014;259:45–51.
Tamandl D, Sahora K, Prucker J, et al. Impact of the Reconstruction Method on Delayed Gastric Emptying After Pylorus-Preserving Pancreaticoduodenectomy: A Prospective Randomized Study. World J Surg 2013. [Epub ahead of print]
Moher D, Liberati A, Tetzlaff J, The PRISMA Group, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6, e1000097.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodo. 2005;5:13.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Fischer CP, Hong JC. Method of pyloric reconstruction and impact upon delayed gastric emptying and hospital stay after pylorus-preserving pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:215–9.
Kurosaki I, Hatakeyama K. Preservation of the left gastric vein in delayed gastric emptying after pylorus-preserving PD. J Gastrointest Surg. 2005;9:846–52.
Yeo CJ, Barry MK, Sauter PK, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg. 1993;218:229–37.
Kollmar O, Moussavian MR, Richter S, et al. Prophylactic octreotide and delayed gastric emptying after pancreaticoduodenectomy: results of a prospective randomized double-blinded placebo-controlled trial. Eur J Surg Oncol. 2008;34:868–75.
Goei TH, van Berge Henegouwen MI, et al. Pylorus-preserving pancreatoduodenectomy: influence of a Billroth I versus a Billroth II type of reconstruction on gastric emptying. Dig Sur. 2001;18:376–80.
Shimoda M, Kubota K, Katoh M, et al. Effect of billroth II or Roux-en-Y reconstruction for the gastrojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled study. Ann Surg. 2013;257:938–42.
Ueno T, Tanaka A, Hamanaka Y, et al. A proposal mechanism of early delayed gastric emptying after pylorus preserving pancreatoduodenectomy. Hepatogastroenterology. 1995;42:269–74.
Sugiyama M, Abe N, Ueki H, et al. A new reconstruction method for preventing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. Am J Surg. 2004;187:743–6.
Diener MK, Knaebel HP, Heukaufer C, et al. A systematic review and meta-analysis of pylorus-preserving versus classical pancreaticoduodenectomy for surgical treatment of periampullary and pancreatic carcinoma. Ann Surg. 2007;245:187–200.
He T, Zhao Y, Chen Q, et al. Pancreaticojejunostomy versus Pancreaticogastrostomy after Pancreaticoduodenectomy: A Systematic Review and Meta-Analysis. Dig Surg. 2013;30:56–69.
Park YC, Kim SW, Jang JY, et al. Factors influencing delayed gastric emptying after pylorus-preserving pancreatoduodenectomy. J Am Coll Surg. 2003;196:859–65.
Horstmann O, Markus PM, Ghadimi MB, et al. Pylorus preservation has no impact on delayed gastric emptying after pancreatic head resection. Pancreas. 2004;28:69–74.
Sakamoto Y, Yamamoto Y, Hata S, et al. Analysis of risk factors for delayed gastric emptying (DGE) after 387 pancreaticoduodenectomies with usage of 70 stapled reconstructions. J Gastrointest Surg. 2011;15:1789–97.
McCulloch P, Taylor I, Sasako M, et al. Randomised trials in surgery: problems and possible solutions. BMJ. 2002;324:1448–51.
Acknowledgements
We thank Doctor Yanfang Zhao (Department of Health Statistics, Second Military Medical University, Shanghai, China) for her critical revision of the meta-analysis section.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YZ participated in the design and coordination of the study, carried out the critical appraisal of studies and wrote the manuscript. LW and JL developed the literature search, carried out the extraction of data, assisted in the critical appraisal of included studies and assisted in writing up. HL and BL carried out the statistical analysis of studies. All authors read and approved the final manuscript.
Yanming Zhou and Jincan Lin contributed equally to this work.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Zhou, Y., Lin, J., Wu, L. et al. Effect of antecolic or retrocolic reconstruction of the gastro/duodenojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a meta-analysis. BMC Gastroenterol 15, 68 (2015). https://doi.org/10.1186/s12876-015-0300-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-015-0300-8