Abstract
Background
MicroRNA-21 (miR-21) is an oncogenic microRNA that regulates the expression of multiple cancer-related target genes. miR-21 has been associated with progression of some types of cancer. Metastasis-associated protein1 expression and loss of E-cadherin expression are correlated with cancer progression and metastasis in many cancer types. In advanced colorectal cancer, the clinical significance of miR-21 expression remains unclear. We aimed to investigate the impact of miR-21 expression in advanced colorectal cancer and its correlation with target proteins associated with colorectal cancer progression.
Methods
From 2004 to 2007, 277 consecutive patients with T3-4a colorectal cancer treated with R0 surgical resection were included. Patients with neoadjuvant therapy and distant metastasis at presentation were excluded. The expression of miR-21 was investigated by in situ hybridization. Immunohistochemistry was used to detect E-cadherin and metastasis-associated protein1 expression.
Results
High stromal expression of miR-21 was found in 76 of 277 (27.4%) colorectal cancer samples and was correlated with low E-cadherin expression (P = 0.019) and high metastasis-associated protein1 expression (P = 0.004). T3-4a colorectal cancer patients with high miR-21 expression had significantly shorter recurrence-free survival than those with low miR-21 expression. When analyzing colon and rectal cancer separately, high expression of miR-21 was an independent prognostic factor of unfavorable recurrence-free survival in T3-4a colon cancer patients (P = 0.038, HR = 2.45; 95% CI = 1.05-5.72) but not in T3-4a rectal cancer patients. In a sub-classification analysis, high miR-21 expression was associated with shorter recurrence-free survival in the stage II cancer (P = 0.001) but not in the stage III subgroup (P = 0.267).
Conclusions
Stromal miR-21 expression is related to the expression of E-cadherin and metastasis-associated protein1 in colorectal cancer. Stage II colorectal cancer patients with high levels of miR-21 are at higher risk for tumor recurrence and should be considered for more intensive treatment.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in Korea [1]. The prognosis of CRC is associated with tumor progression; five-year survival rates range from 93% to 8% [2]. There are many proposed serological and molecular markers as predictive and prognostic indicators of CRC; however, they are not widely accepted as providing reliable prognostic information due to a lack of reproducibility, validation and standardization among studies [3,4]. Therefore, there is a need to identify more reliable prognostic mediators of tumor progression and metastasis in order to define the behavior of CRC and improve postoperative treatment strategies.
MicroRNAs are small noncoding RNA molecules, 18-25 nucleotides in length, which post-transcriptionally regulate gene expression by binding to the 3’ untranslated regions of target messenger RNAs and play a central role in regulation of mRNA expression [5]. MicroRNAs have been shown to influence all cellular processes [6] and have a high degree of sequence conservation among distantly related organism, indicating their likely participation in essential biological processes [7]. Of note, microRNAs have been reported to have a marked influence on carcinogenesis through the dysregulation of oncogenes and tumor suppressor genes [8]. Cancer-related microRNAs typically show altered expression levels in tumors as compared to the level of expression in the corresponding normal tissue.
MicroRNA-21 (miR-21) is an oncogenic microRNA that regulates the expression of multiple cancer-related target genes, such as PTEN and PDCD4, and has been reported to be consistently up-regulated in various types of cancers, including colon, breast, lung, and stomach cancers [9-16]. MiR-21 is known to contribute to the regulation of apoptosis, cell proliferation and migration [9,11,17]. Moreover, miR-21 levels increase in the advanced stages of cancer, suggesting a central role for miR-21 in invasion and dissemination of cancer [12,14]. In CRC tissue samples, miR-21 expression is up-regulated during tumor progression and is also known to be associated with poor survival and response to chemotherapy [12,13,18]. However, the clinical significance of miR-21 expression in advanced CRC remains unclear.
In situ hybridization (ISH) for microRNA has an advantage over quantitative microRNA expression analysis platforms in that ISH allows for precise histological localization of microRNAs in formalin-fixed paraffin-embedded tissue blocks [19,20].
Loss of E-cadherin expression is associated with activation of epithelial-mesenchymal transition, invasion and metastasis in various cancers [21]. Conversely, expression of Metastasis-associated protein1 (MTA1) is correlated with cancer progression and metastasis in numerous cancer types, including CRC [22,23]. Previous studies on the association between MTA1 and E-cadherin have shown that MTA1 regulates E-cadherin expression through AKT activation in prostate cancer, and that low E-cadherin expression promotes cancer metastasis [21,24]. However, the exact role of these proteins in CRC remains unclear.
We investigated miR-21 expression using ISH in specimens from T3-4a CRC patients treated by surgical resection. We also evaluated the relationship between expression of miR-21, E-cadherin and MTA1 and their clinical significance as potential biomarkers for prognosis of T3-4a CRC patients.
Methods
Patients
From January 2004 until June 2007, a total of 526 consecutive patients underwent surgical resection for CRC at Seoul St. Mary’s Hospital. Of these, 277 patients with pathological T3 (invasion of the subserosa or pericolic/perirectal adipose tissue) or T4a (serosal invasion) cancer were selected for the study, based on the following inclusion criteria: (i) no neoadjuvant chemotherapy or radiation therapy, (ii) no evidence of direct invasion into adjacent structures or organs, (iii) no postoperative death within six weeks, and (iv) no distant metastasis at presentation. The patients consisted of 181 males and 96 females (mean age 63.0 years). Overall survival (OS) was defined as the time interval between surgery and death from any cause or the most recent follow-up date. Recurrence-free survival (RFS) was defined as the time from the date of surgery to the date of first cancer recurrence or the most recent disease-free follow-up. This study was approved by the Institutional Review Board of Seoul, St. Mary’s Hospital, The Catholic University of Korea. Written informed consent was obtained from all patients.
Tissue microarray construction
We constructed tissue microarrays from formalin-fixed, paraffin-embedded tissues as previously described [25,26]. Two 2-mm-diameter tissue cores were collected from each representative tumor specimen and inserted in a recipient paraffin block. The tissue microarray blocks were serially cut into 4-μm-thick sections for immunohistochemistry and 6-μm-thick sections for ISH.
Immunohistochemistry for E-cadherin and MTA1
Immunohistochemical staining was performed using specific antibodies against E-cadherin (4A2C7, Zymed, South San Francisco, CA), MTA1 (A-11, Santa Cruz Biotechnology, Santa Cruz, CA) and the Polink-2 plus polymer HRP detection system (Golden Bridge International, Mukilteo, WA, USA) according to each manufacturer’s protocol. The specificity of each antibody was confirmed using both Western blotting and immunocytochemistry in several cell lines with known protein expression status. Negative controls were performed by the substitution of the primary antibodies with normal mouse IgG at the same concentration as the primary antibodies. Multi-tissue blocks containing known-positive tumor tissues were used as positive controls. Staining was examined in triplicate by two gastrointestinal pathologists (CKJ and SHL) who were blinded to the clinicopathological data. Specimens with discordant interpretations were reviewed until an agreement was reached. Immunohistochemical staining results were only assessed by a semiquantitative score of staining intensity (0, no; 1, weak; 2, moderate; 3, strong staining) because nearly all positively-staining tumors showed a diffuse staining pattern for both proteins. These scores were subsequently used to group samples into two categories: low (0 or 1) and high staining (2 or 3). Membrane staining of E-cadherin was evaluated and scored as ‘2’ when tumor cells displayed staining intensity similar to that seen in normal colonic mucosa. MTA1 expression was evaluated as nuclear staining.
In situ hybridization for miR-21
ISH was performed using the miRCURY locked nucleic acid (LNA) microRNA Detection FFPE microRNA ISH Optimization Kit 2 (Exiqon, Vedbaek, Denmark) in a StatSpin ThermoBrite Slide Hybridizer (Fisher Scientific, Westwood, MA) as previously described [19]. We used a double-digoxigenin-labeled LNA miR-21 probe (Exiqon, sequence: 5′-TCAACATCAGT-CTGATAAGCTA-3′), a positive control LNA U6 snRNA probe (Exiqon, sequence: 5′- CACGAATTTGCGTGTCATCCTT-3′) and a negative control LNA scrambled microRNA probe (Exiqon, sequence: 5′- GTGTAACACGTCTATACGCCCA-3′). Tissue sections were counterstained with nuclear fast red. Semiquantitative assessment of the ISH staining results was performed by two pathologists (CKJ and SHL) who were unaware of the clinicopathological and immunohistochemical data. In all cases where disagreements occurred, a consensus was reached by the investigators. The intensity of the staining was scored as negative (0), weak (1), moderate (2), or strong (3), as previously described [27,28], and samples were subsequently grouped into two categories: low (0 or 1) and high (2 or 3) expression.
Statistical analysis
The relationships between the expression of miR-21, E-cadherin and MTA1 and the clinicopathological parameters were analyzed using the Chi-square test. Cumulative incidence curves for OS and RFS were plotted using the Kaplan–Meier method. The long-rank test was used to detect differences among groups. Multivariate analysis for OS and RFS was conducted using the Cox proportional hazard regression model. All statistical analyses were performed using SPSS, version 16 (SPSS Inc., Chicago, IL). A p value <0.05 was considered significant.
Meta-analysis for the association of miR-21 expression and patient survival
Two authors (CKJ and SHL) performed literature searches using PubMed, Embase databases and Google up to November 2014, and independently selected eligible articles. Inclusion criteria include 1) being related to the association between miR-21 expression and CRC prognosis, 2) original articles, and 3) sufficient RFS or OS data including hazard ratio (HR) with a 95% confidence interval (CI). We performed a meta-analysis of HR of the effect of miR-21expression on RFS or OS in colon or rectal cancer patients. Heterogeneity among studies was assessed using Cochran Q test and I2 values. A P < 0.10 or I2 > 50% was considered significant heterogeneity. If statistical heterogeneity was observed, the random effect model was used for meta-analysis. Otherwise, we used a fixed-effect model for the meta-analysis. Meta-analyses were performed using Comprehensive Meta Analysis Version 2.0 (Biostat Inc., Englewood, NJ).
Results
Demographic and clinicopathological variables of the study participants are listed in Table 1.
miR-21 expression by in situ hybridization
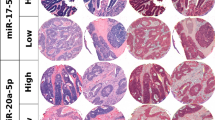
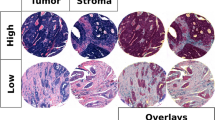
miR-21 expression was found to be predominantly localized to the stroma surrounding the tumor cells (Figure 1). High levels of miR-21 were found in 76 of 277 (27.4%) CRC specimens. There was no significant correlation between high miR-21 expression and the clinicopathological features of the patients (Table 1).
In situ hybridization for miR-21 and immunohistochemistry for E-cadherin and MTA1. (A) A representative 2 mm tumor tissue core from the colorectal cancer tissue microarray shows diffuse strong miR-21 expression in the stroma. (B) High-magnification image of insert in (A) shows that miR-21 signals are strong in the stromal cells of colorectal cancer but not in the tumor cells. Magnification x400. (C) Tumor cells show strong membranous expression of E-cadherin. Magnification x400. (D) Tumor cells show strong nuclear expression of MTA1. Magnification x400.
Correlation between miR-21 and MTA1/E-cadherin expression
The expression patterns of E-cadherin and MTA1 in stained tumor cells were membranous and nuclear, respectively (Figure 1). Low expression of E-cadherin was found in 109 of 277 (39.4%) CRCs, and high MTA1 expression was seen in 102 (36.8%) tumors. High miR-21 expression was significantly correlated with low E-cadherin expression (P = 0.019) and high MTA1 expression (P = 0.004) (Table 1). E-cadherin expression was negatively correlated with MTA1 expression (P = 0.005).
Recurrence-free survival and overall survival
In all 277 CRC patients, variables significantly associated with RFS included miR-21 expression (P = 0.010, Figure 2A), histological differentiation (P = 0.031), pT stage (P = 0.0005), lymph node metastasis (P = 0.00001), and serum CEA level (P =0.006) (Table 2). In a multivariate analysis, high levels of miR-21 (P = 0.007, HR = 2.24; 95% CI = 1.25-4.02), pT stage, lymph node metastasis, and serum CEA level were independent prognostic factors for unfavorable RFS (Table 3). However, the OS rate was not associated with the expression levels of miR-21, E-cadherin or MTA1.
Association between miR-21 expression and recurrence-free survival in patients with T3-4a colorectal cancer. Kaplan-Meier survival curves for recurrence-free survival in all (A), stage II (B) and stage III (C) cancer patients according to miR-21 expression status. (A) High miR-21 expression is associated with recurrence-free survival in colon cancer patients but not in rectal cancer patients. (B) For the 138 patients with stage II cancer, the association between high miR-21 expression and recurrence-free survival is statistically significant only in colon cancer patients. (C) Among 277 stage III cancer patients, high miR-21 expression is not associated with poor recurrence-free survival.
To further understand the association of prognostic factors and RFS according to the primary cancer site, we analyzed their HRs for RFS in colon and rectal cancer separately (Tables 3 and 4). High expression of miR-21 was associated with shorter RFS in patients with T3-4a colon cancer (n = 173, P = 0.005, Figure 2A), but not in patients with T3-4a rectal cancer (n = 104, P = 0.474, Figure 2A).
The T3-4a CRC patients were divided into subgroups according to American Joint Committee on Cancer stage. In the stage II (T3-4aN0M0) subgroup, we found that patients with high miR-21 expression level had a significantly shorter RFS time than those with low miR-21 level regardless of the primary site (colon cancer, P = 0.007; rectal cancer, P = 0.030, Figure 2B). However, in the stage III (T3-4aN1M0) subgroup, there was no significant difference in RFS between patients with high or low levels of miR-21 expression (colon cancer, P = 0.053; rectal cancer, P = 0.588, Figure 2C).
Meta-analysis
A total of 10 studies were included for the meta-analysis and their characteristics are summarized in Table 4 [13,18-20,29-34]. High heterogeneity was found in the analysis. For all CRC patients, high miR-21 expression was significantly associated with poor RFS (HR = 1.327, 95% CI = 1.053-1.673, Figure 3) and poor OS (HR = 1.272, 95% CI = 1.065-1.519, Figure 4). In subgroup analysis, the high miR-21 expression was significantly correlated with poor RFS and OS in colon cancer patients (HR = 1.423, 95% CI = 1.280-1.582; HR = 1.357, 95% CI = 1.102-1.672, respectively), but not in rectal cancer or CRC patients.
Forest plot of meta-analysis for the association of high miR-21 expression and recurrence-free survival in colorectal cancer patients. There is a statistically significant association between high miR-21 expression and poor recurrence-free survival in colon cancer patients. The observed association is not statistically significant in rectal cancer. CI, confidence interval; CC, colon cancer; RC, rectal cancer; CRC, colorectal cancer; RFS, recurrence-free survival.
Forest plot of meta-analysis for the association of high miR-21 expression and overall survival in colorectal cancer patients. High miR-21 expression is associated with poor overall survival in colon cancer patients but not in rectal cancer. CI, confidence interval; CC, colon cancer; RC, rectal cancer; CRC, colorectal cancer; OS, overall survival.
Discussion
In the present study, we detected high miR-21 expression in 27.1% (81 of 299) of T3-4a CRCs, and this was associated with low E-cadherin expression and high MTA1 expression. The multivariate analysis revealed that high miR-21 expression was an independent predictor of tumor recurrence in patients with T3-4a CRC.
We observed that miR-21 overexpression occurred in the stroma rather than in the actual tumor cells. Previous studies have reported that miR-21 predominantly localizes to fibroblast-like cells within the tumor-associated stroma of CRC, breast cancer and esophageal cancer [19,35,36]. Using high sensitivity TaqMan quantitative RT-PCR assays in microdissected tissue, Bullock et al. found that miR-21 expression was undetectable in CRC tumor cells but was present in the tumor-associated stroma [35]. Up-regulated miR-21 expression in CRC-associated stroma was associated with transforming growth factor TGF-β-dependent fibroblast-to-myofibroblast transformation and with decreased expression of reversion-inducing cysteine-rich protein with Kazal motifs [35]. The authors proposed that myofibroblast-derived factors mediated tumor progression, and that miR-21 promoted chemo-resistance and tumor invasion by increasing matrix metalloproteinase 2 activity [35]. These results suggest that miR-21 may regulate tumor progression through modulation of the tumor microenvironment.
Recent studies have shown that high stromal miR-21 expression, as measured by ISH, is correlated with shorter RFS in stage II colon cancer [19,20]. In the analysis of OS in stage II colon cancer patients, Nielsen et al. [19] reported on the prognostic significance of miR-21; while Kjaer-Frifeldt et al. [20] were unable to show any significant impact on OS. In the present study using ISH, we found that stromal miR-21 expression was a prognostic factor for RFS in stage II CRC patients but not in stage III patients. Therefore, miR-21 overexpression may have an important role in tumor progression and recurrence prior to the development of lymph node or distant metastases. We found no prognostic value for miR-21 in our analysis of OS, which was calculated as the time from surgery to time of death from any cause.
In the stratified meta-analysis by tumor site, we found that high miR-21 expression was associated with shorter RFS and worse OS in colon cancer, but not in rectal cancer or CRC. The RFS results are consistent with findings of present study.
It has been reported that MTA1 regulates E-cadherin expression via AKT activation in prostate cancer, and that miR-21 is required for regulation of phosphorylated AKT expression in glioblastoma multiforme [24,37]. Xiong et al. suggested that miR-21 influences tumor biology through the PTEN/PI-3 K/Akt pathway in CRC [38]. In our immunohistochemical analysis of E-cadherin and MTA1expression, high MTA1 level was associated with low E-cadherin expression. The expression profiles of these proteins were also significantly correlated with miR-21 expression patterns. Taken together, these results led us to hypothesize that MTA1 may negatively regulate E-cadherin expression via high miR-21 expression in CRC. However, further studies will be needed to determine whether there is a direct role for miR-21 in regulation of MTA1 and E-cadherin expression.
Our study has some limitations including the retrospective, single-institution design and the lack of validation of these results in an independent CRC patient population. Thus, further prospective studies are needed to evaluate the prognostic significance of miR-21 expression.
Conclusion
miR-21 is overexpressed in the stroma of CRC specimens and has strong associations with the expression of E-cadherin and MTA1. A high level of miR-21 is an independent risk factor predictive of early tumor recurrence in T3-4a colon cancer and stage II CRC. Thus, CRC patients with miR-21 overexpression are at higher risk for tumor recurrence and may benefit from more intensive treatment.
Abbreviations
- CRC:
-
Colorectal cancer
- miR-21:
-
MicroRNA-21
- ISH:
-
In situ hybridization
- MTA1:
-
Metastasis-associated protein1
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- HR:
-
hazard ratio
- CI:
-
confidence interval
- LNA:
-
locked nucleic acid
References
Choi KS, Jun JK, Lee HY, Hahm MI, Oh JH, Park EC. Increasing uptake of colorectal cancer screening in Korea: a population-based study. BMC Public Health. 2010;10:265.
O'Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. Journal of the National Cancer Institute. 2004;96(19):1420–5.
George B, Kopetz S. Predictive and prognostic markers in colorectal cancer. Current oncology reports. 2011;13(3):206–15.
Jung SB, Lee HI, Oh HK, Shin IH, Jeon CH. Clinico-pathologic Parameters for Prediction of Microsatellite Instability in Colorectal Cancer. Cancer research and treatment : official journal of Korean Cancer Association. 2012;44(3):179–86.
Filipowicz W, Bhattacharyya SN, Sonenberg N. Mechanisms of post-transcriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet. 2008;9(2):102–14.
Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120(1):15–20.
Carrington JC, Ambros V. Role of microRNAs in plant and animal development. Science. 2003;301(5631):336–8.
Zhang B, Pan X, Cobb GP, Anderson TA. microRNAs as oncogenes and tumor suppressors. Dev Biol. 2007;302(1):1–12.
Meng F, Henson R, Wehbe-Janek H, Ghoshal K, Jacob ST, Patel T. MicroRNA-21 regulates expression of the PTEN tumor suppressor gene in human hepatocellular cancer. Gastroenterology. 2007;133(2):647–58.
Zhu S, Si ML, Wu H, Mo YY. MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1). J Biol Chem. 2007;282(19):14328–36.
Asangani IA, Rasheed SA, Nikolova DA, Leupold JH, Colburn NH, Post S, et al. MicroRNA-21 (miR-21) post-transcriptionally downregulates tumor suppressor Pdcd4 and stimulates invasion, intravasation and metastasis in colorectal cancer. Oncogene. 2008;27(15):2128–36.
Slaby O, Svoboda M, Fabian P, Smerdova T, Knoflickova D, Bednarikova M, et al. Altered expression of miR-21, miR-31, miR-143 and miR-145 is related to clinicopathologic features of colorectal cancer. Oncology. 2007;72(5–6):397–402.
Schetter AJ, Leung SY, Sohn JJ, Zanetti KA, Bowman ED, Yanaihara N, et al. MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. JAMA. 2008;299(4):425–36.
Qian B, Katsaros D, Lu L, Preti M, Durando A, Arisio R, et al. High miR-21 expression in breast cancer associated with poor disease-free survival in early stage disease and high TGF-beta1. Breast Cancer Res Treat. 2009;117(1):131–40.
Markou A, Tsaroucha EG, Kaklamanis L, Fotinou M, Georgoulias V, Lianidou ES. Prognostic value of mature microRNA-21 and microRNA-205 overexpression in non-small cell lung cancer by quantitative real-time RT-PCR. Clin Chem. 2008;54(10):1696–704.
Chan SH, Wu CW, Li AF, Chi CW, Lin WC. miR-21 microRNA expression in human gastric carcinomas and its clinical association. Anticancer Res. 2008;28(2A):907–11.
Yao Q, Cao S, Li C, Mengesha A, Kong B, Wei M. Micro-RNA-21 regulates TGF-beta-induced myofibroblast differentiation by targeting PDCD4 in tumor-stroma interaction. Int J Cancer. 2011;128(8):1783–92.
Shibuya H, Iinuma H, Shimada R, Horiuchi A, Watanabe T. Clinicopathological and prognostic value of microRNA-21 and microRNA-155 in colorectal cancer. Oncology. 2010;79(3–4):313–20.
Nielsen BS, Jorgensen S, Fog JU, Sokilde R, Christensen IJ, Hansen U, et al. High levels of microRNA-21 in the stroma of colorectal cancers predict short disease-free survival in stage II colon cancer patients. Clin Exp Metastasis. 2011;28(1):27–38.
Kjaer-Frifeldt S, Hansen TF, Nielsen BS, Joergensen S, Lindebjerg J, Soerensen FB, et al. The prognostic importance of miR-21 in stage II colon cancer: a population-based study. Br J Cancer. 2012;107(7):1169–74.
Fan L, Wang H, Xia X, Rao Y, Ma X, Ma D, et al. Loss of E-cadherin promotes prostate cancer metastasis via upregulation of metastasis-associated gene 1 expression. Oncol Lett. 2012;4(6):1225–33.
Toh Y, Nicolson GL. The role of the MTA family and their encoded proteins in human cancers: molecular functions and clinical implications. Clin Exp Metastasis. 2009;26(3):215–27.
Tuncay Cagatay S, Cimen I, Savas B, Banerjee S. MTA-1 expression is associated with metastasis and epithelial to mesenchymal transition in colorectal cancer cells. Tumour Biol. 2013;34(2):1189–204.
Wang H, Fan L, Wei J, Weng Y, Zhou L, Shi Y, et al. Akt mediates metastasis-associated gene 1 (MTA1) regulating the expression of E-cadherin and promoting the invasiveness of prostate cancer cells. PloS One. 2012;7(12):e46888.
Kang YG, Jung CK, Lee A, Kang WK, Oh ST, Kang CS. Prognostic significance of S100A4 mRNA and protein expression in colorectal cancer. J Surg Oncol. 2012;105(2):119–24.
Jung W, Hong KD, Jung WY, Lee E, Shin BK, Kim HK, et al. SIRT1 Expression Is Associated with Good Prognosis in Colorectal Cancer. Korean J Pathol. 2013;47(4):332–9.
Chiyomaru T, Enokida H, Tatarano S, Kawahara K, Uchida Y, Nishiyama K, et al. miR-145 and miR-133a function as tumour suppressors and directly regulate FSCN1 expression in bladder cancer. Br J Cancer. 2010;102(5):883–91.
Lin Y, Zeng Y, Zhang F, Xue L, Huang Z, Li W, et al. Characterization of microRNA expression profiles and the discovery of novel microRNAs involved in cancer during human embryonic development. PloS One. 2013;8(8):e69230.
Zhang JX, Song W, Chen ZH, Wei JH, Liao YJ, Lei J, et al. Prognostic and predictive value of a microRNA signature in stage II colon cancer: a microRNA expression analysis. Lancet Oncol. 2013;14(13):1295–306.
Bovell LC, Shanmugam C, Putcha BD, Katkoori VR, Zhang B, Bae S, et al. The prognostic value of microRNAs varies with patient race/ethnicity and stage of colorectal cancer. Clin Cancer Res. 2013;19(14):3955–65.
Toiyama Y, Takahashi M, Hur K, Nagasaka T, Tanaka K, Inoue Y, et al. Serum miR-21 as a diagnostic and prognostic biomarker in colorectal cancer. J Natl Cancer Inst. 2013;105(12):849–59.
Chen TH, Chang SW, Huang CC, Wang KL, Yeh KT, Liu CN, et al. The prognostic significance of APC gene mutation and miR-21 expression in advanced-stage colorectal cancer. Colorectal Dis. 2013;15(11):1367–74.
Hansen TF, Kjaer-Frifeldt S, Christensen RD, Morgenthaler S, Blondal T, Lindebjerg J, et al. Redefining high-risk patients with stage II colon cancer by risk index and microRNA-21: results from a population-based cohort. Br J Cancer. 2014;111(7):1285–92.
Oue N, Anami K, Schetter AJ, Moehler M, Okayama H, Khan MA, et al. High miR-21 expression from FFPE tissues is associated with poor survival and response to adjuvant chemotherapy in colon cancer. Int J cancer. 2014;134(8):1926–34.
Bullock MD, Pickard KM, Nielsen BS, Sayan AE, Jenei V, Mellone M, et al. Pleiotropic actions of miR-21 highlight the critical role of deregulated stromal microRNAs during colorectal cancer progression. Cell death Dis. 2013;4:e684.
Alder H, Taccioli C, Chen H, Jiang Y, Smalley KJ, Fadda P, et al. Dysregulation of miR-31 and miR-21 induced by zinc deficiency promotes esophageal cancer. Carcinogenesis. 2012;33(9):1736–44.
Grunder E, D'Ambrosio R, Fiaschetti G, Abela L, Arcaro A, Zuzak T, et al. MicroRNA-21 suppression impedes medulloblastoma cell migration. Eur J Cancer. 2011;47(16):2479–90.
Xiong B, Cheng Y, Ma L, Zhang C. MiR-21 regulates biological behavior through the PTEN/PI-3 K/Akt signaling pathway in human colorectal cancer cells. Int J Oncol. 2013;42(1):219–28.
Acknowledgements
The authors acknowledge the financial support of the Catholic Medical Center Research Foundation made in the program year of 2012. This study was partially supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2013R1A2A2A01068570).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
WK participated in the design of the study, collected patient material and drafted the manuscript. JL and SO collected patient material and revised the manuscript critically for important intellectual content. SL and CJ performed the in situ hybridization and immunohistochemistry. CJ conceived of the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kang, W.K., Lee, J.K., Oh, S.T. et al. Stromal expression of miR-21 in T3-4a colorectal cancer is an independent predictor of early tumor relapse. BMC Gastroenterol 15, 2 (2015). https://doi.org/10.1186/s12876-015-0227-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-015-0227-0