Abstract
Introduction
Non-Communicable Diseases (NCDs) place a significant burden on India's healthcare system, accounting for approximately 62% of all deaths in the country in 2017. The southern Indian state - Kerala - has some of the highest rates of NCDs. Within the state, the fisherfolk community has a high prevalence of risk factors such as tobacco use and alcohol consumption. Working in the fisheries industry demands physical exertion, night shifts alongside extended periods of time at sea (for seafaring fisherfolk). Evidence is scant on how these conditions relate to the health-seeking experiences of fisherfolk, particularly in the context of NCDs. We conducted a qualitative study in two districts of Kerala to fill this gap.
Methods
In-depth individual and small group interviews– as per participant preference – with male and female fishing community members living with NCDs were conducted between October 2022 and February 2023 in two districts of Kerala. Interviews were conducted to explore community members’ experiences with health-seeking for NCDs. Transliterated English transcripts were coded using ATLAS.ti software and analysed using thematic analysis with inductive generation of codes, with indexing against Levesque, Harris, and Russell’s 2013 access to healthcare framework.
Results
Thirty-three interviews with 42 participants were conducted. We found that NCDs were usually diagnosed late- either when admitted/consulted for other illnesses or when the symptoms became unbearable. Health-seeking patterns differed between seafaring and inland fishing subgroups, who were sampled from two districts in the state. Seafaring fisherfolk preferred public facilities for regular checkups and medicines while in-land fisherfolk relied on private facilities, although it was considered expensive. Ability to seek care was impacted by the working hours of the health centre which did not suit their working hours. Health constaints and related expenses also impacted their financial status and occupation, with some opting for less strenuous jobs.
Conclusion
This study highlights the NCD-related health-seeking experiences of the fisherfolk community in Kerala, India. Fisherfolk reported self neglect, delayed diagnosis, cost and livelihood constraints owing to the onset of NCDs, even as dual practice and medicine access in the public sector were appreciated. Overall, larger studies and policymaking processes should consider in depth the experiences faced by particular economic groups like fisherfolk, who may face unique health and care-seeking challenges.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
The World Health Organization (WHO) defines Non-Communicable Diseases (NCDs) as conditions that develop over an extended period of time resulting from a combination of genetic, physiological, environmental, and behavioural variables [1]. NCDs are frequently linked to unhealthy dietary habits, lack of physical activity, and the consumption of excessive salt, tobacco, and alcohol [2, 3]. Living with NCDs could end up in sudden life-threatening health issues, for example, heart attacks, stroke, and cancers. The financial consequences of NCDs are dramatic: people end up exhausting their savings [4], losing their jobs [5], and ending in long-term debts [6].
NCDs pose a significant burden to India’s healthcare system; as per an analysis published in 2017, they accounted for approximately 62% of all deaths in the country [7]. As per the report, around 90% of premature deaths in the southern Indian state of Kerala were attributed to NCDs, which is among the highest levels of NCD burden in the country [7]. According to another study conducted in 2019, 82% of individuals aged 18–64 in Kerala had one or more risk factors for NCDs, and almost half had multiple risk factors [8].
Recognizing the growing incidence of NCDs, various initiatives have been introduced by the Indian government. This began with the National Programme for prevention & control of Cancer, Diabetes, Cardiovascular diseases & Stroke (NPCDCS), which was launched in 2010, giving thrust to secondary prevention in particular. By 2013, with the introduction of National Action Plan and thereafter Multisectoral Action Plan for NCDs, there was an increase in screening and early detection efforts while decentralizing NCD programs [9, 10]. Primary Health Centres (PHCs) in Kerala serve as the primary point of contact for individuals seeking healthcare services for NCDs. These centres offer consultations and diagnostics at a nominal price, making healthcare accessible to all socioeconomic groups. Additionally, medicines are provided free of cost, ensuring affordability and equitable access to essential healthcare resources for the community. In 2017, the Kerala government introduced a package of health reforms called Aardram, under which PHCs were renamed Family Health Centres (FHCs), with substantial service and human resource expansion [11, 12].
As per figures from 2020, Kerala hosts 335 fishing villages with over 185,000 seafaring fishermen and 51,000 inland fishermen active in the state [13]. Kerala’s fisherfolk community has been found to have high prevalence of risk factors such as tobacco use and alcohol consumption [14, 15]. Across India, studies suggest that this community possesses unique characteristics such as physical exertion, night shifts alongside extended periods of time at sea [16, 17]. Not only do these occupational exigencies set them apart from other workers, they specifically add to the NCD risk for this occupation group [15]. The effects are acute, but understudied: news coverage suggests that fisherfolk are frequently prone to heart attacks and injuries while at sea [18,19,20,21]. Along with other factors, early diagnosis and management of NCDs such as high cholesterol and blood sugar levels are crucial for the prevention of these fatal health challenges [22].
The health status of the community is compounded by income inequality and reliance on debt [23]. With reduced income and no alternative job opportunities, the fisherfolk are forced to continue to live in poverty [24]. Studies have traced the economic struggles of this community as the state has marched on a path towards globalized capitalism, broadly relying on a model of ‘accumulation by dispossession,’ with workers’ movements and the Catholic church offering some solidarity and resistance [25]. The unequal distribution of income and reliance on debt create additional stressors, which may lead to poorer health outcomes and limited access to healthcare resources [23]. One study found that in 2016, the Human Development Index value for Kerala’s marine fisherfolk was 9% points lower than that of the general population of the state, much closer to the average HDI of India (Kerala marine fisherfolk: 0.68, Kerala general population: 0.77, India general population: 0.64) [26]. Notwithstanding the introduction of various social security, welfare and direct benefit schemes for this occupational group, awareness, enrollment and impact of these appear to be low [27].
That said, across India as within Kerala, the fisherfolk community is quite heterogenous : seafaring fisherfolk work long hours in the sea, far away from the land, devoid of any facilities except for basic supplies like food and water, while inland fisherfolk spend their night fishing for their livelihood in their boats. Women in the fisherfolk community are involved in fish processing and selling activities [28]. They are also involved in other fishery-related labour such as repair of fishing nets, which is typically unpaid, rendering these workers unrecognised and unsupported as part of the fisheries sector [29]. The patriarchal structure prevalent in India, including Kerala, extends to fisherfolk communities, where traditional gender roles often designate the husband or son as the head of the family, with women playing a subsidiary role in household decision-making [30], notwithstanding the launch of several training programmes targeting women and women’s groups [31, 32]. This often can have implications for health – although this is not directly studied. For example, a study conducted among seafaring fisherfolk found that women were excluded from beachfront recreational activities, having instead to spend their time in commercial and familial tasks [30]. The role such socialising, physical activity, and leisure time may play in mitigating stress and risk factors for Non-Communicable Diseases (NCDs), was unexplored in this study.
More broadly, although the prevalence of NCD risk factors among the fishing community has been established in the literature [15, 33], a phenomenon also seen in a parent study (see Table 1) we conducted in the state from 2017 to 2022, there is little or no exploration of how the community seeks medical help, manages the NCDs and how it impacts them. We therefore conducted a sub-study to understand the healthcare experiences of the fisherfolk community living with NCDs with the scope of identifying opportunities to embed their needs into the existing healthcare system reform process.
Methods
Study setting and information about participants
A qualitative study was conducted with fisherfolk communities residing in Alappuzha and Kollam districts of Kerala. Both districts are home to large populations of fisherfolk – seafaring and inland. In Alappuzha, we interviewed seafaring fisherfolk living by the seashore. This site was located near a National Highway (NH), providing relatively convenient access to both public and private hospitals. The FHC was approximately 3 km away, while the Community Health Centre (CHC) was 6 km away. Numerous private clinics were in close proximity, with several private secondary hospitals clustered around the CHC. The NH location also allowed participants to use public buses for direct transportation to the medical college, about 10 km from the study site. Study participants from Kollam were engaged in inland fishing and resided near the lake. A private secondary hospital was within walking distance, and the FHC was 3 km from the study site. Similar to Alappuzha, participants in Kollam had access to nearby private clinics, some within walking distance from their homes. Kollam district is home to many private secondary and tertiary hospitals at the district centre which is more than 20 km away from the study site.
Male members of the fisherfolk community who were still engaged in the profession and were living with an NCD were considered eligible for the study. Their female counterparts who were living with an NCD were included irrespective of their profession. The selection of participants for this study involved careful consideration of specific NCDs for inclusion in the study. NCDs that have been found to be associated with acute health outcomes or risks such as diabetes, high blood pressure, high cholesterol, hyper/hypo thyroid, and asthma were considered as these were also commonly seen NCDs in the study sites. To capture the specific living conditions experienced while actively engaged in fishing, individuals who had retired from fishing as an occupation were intentionally excluded from the study. Individuals who had been diagnosed with an NCD within one month prior to the data collection period were excluded from the study, as we felt their experience living with an NCD may be short/nascent.
Data collection
Data was collected between October 2022 and February 2023. In-depth interviews were conducted either individually or in groups as per the preference of participants. Initially, participants were identified using purposive sampling with the help of system actors who were known to and trusted by the community members, such as Local Self Government (LSG) and community health workers, popularly known as ASHAs; and community leaders with whom we had established rapport through our larger study. Since it involved visiting participants’ houses to whom we were unknown, having system actors helped in availing a formal acknowledgment of the conduct of the study in their area and ascertaining the denominators of our intended population, helping us identify potential participants for the interview. In such a situation, their presence during the interview could not consistently be avoided. Mindful of the Hawthorne effect and other biases introduced due to the presence of system actors, further recruitment was done through snowballing techniques from participants interviewed. Face-to-face in-depth interviews were conducted by a trained qualitative researcher with postgraduate training in anthropology (SS) using the local language, Malayalam, at a place convenient to the participant. An interview guide modified from a previous similar study [36] was used for data collection (Interview guide attached as supplementary file 1). The guide covered a range of questions about their NCD health status, their preferred healthcare facility and the drivers of their choice, and their (and their family’s) healthcare journey and experiences related to the management of NCDs. Each participant was interviewed once and interviews were audio recorded with consent. During interviews, participants were assured of their comfort and right to refuse questions they weren’t comfortable with. When needed, the recording was paused to respect their privacy, and data was not included in the analysis. In five cases, family members, usually the spouse/son/daughter, who were also caregivers for the participants, joined the interview and provided details of the participants’ healthcare journey. Given that the interviews took place in their homes, this involvement was unavoidable. Interviews were conducted until data saturation was attained from all subgroups identified (seafaring fisherfolk community- male and female, in-land fishing community- male and female).
The audio files were outsourced to a paid, empaneled transcription company to transcribe and translate verbatim to English, with appropriate and verified assurances of privacy and confidentiality of the data. The English translation was cross-checked by SS for accuracy with the original audio in Malayalam.
In addition, field notes were taken during the interviews. We also field-noted informal conversations with other stakeholders including the Medical Officer (MO) of FHCs, LSG leaders, and community leaders who were contacted on a regular basis during the study.
Data analysis
Data analysis in this study employed a thematic analysis approach [37]. The data was meticulously coded line by line using ATLAS.ti software by SS and GB. Initially, a set of codes and code groups was established by modifying the codebook used in the previous study and using the topic guide of this study. The code book was subsequently discussed and refined based on inputs from other team members (DN, JJ) and finalized to facilitate further coding. Regular discussions were held to deliberate on the emerging codes resulting from additional analysis (major codes used have been provided in supplementary file 2). Findings were shared back with the community for member checking. Weekly meetings with the principal investigator and team were held throughout the duration of the study which facilitated widened perspectives and feedback for improving the study.
We used Levesque, Harris, and Russell’s 2013 framework on accessing healthcare [38] for access to healthcare to summarise our results. This framework offers a comprehensive and dynamic understanding of access to care, identifying relevant determinants that impact access from a multilevel perspective. While the framework also considers factors related to health systems, institutions, organizations, and providers, our focus was on the individual, household, community, and population levels, so we included only these aspects in our analysis.
Ethics and consent
The Institutional Ethics Committee of the George Institute for Global Health approved this study with ethical clearance (Project Number 05/2019). Before initiating fieldwork, the LSG leaders and Medical Officers (MOs) at FHCs were informed about the study and the proposal was shared for their approval. Prior to participation in interviews, informed verbal consent was obtained from all participants, ensuring their understanding and voluntary involvement in the research. Confidentiality measures were strictly upheld, as only researchers were granted access to participants’ identifiable information, thereby safeguarding their privacy and data confidentiality.
Results
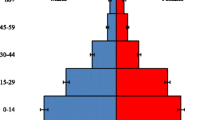
We conducted a total of 33 interviews with 42 participants in the age group of 42–72 years. Of the total, 24 were with inland fishing community (15 men and 9 women) and remaining 18 with seafaring community (8 men and 10 women). Hypertension (N = 22), high cholesterol (N = 17) and diabetes (N = 16) were the most common ailments experienced by participants. Hypo/Hyperthyroidism (N = 5) was also prevalent among women, more so in the seafaring community. Two participants had asthma. Table 2 provides detailed demographic details of the participants. Other ailments noted for the participants were stroke, disability, kidney issues, and injuries. Of 42 the participants, 26 had multimorbidity. We detail the healthcare experiences of inland and seafaring fisherfolk along their NCD management trajectory, using Levesque, Harris, and Russell’s 2013 framework on accessing healthcare (see Fig. 1).
Ability to perceive
Low awareness, mixed outreach for awareness-raising
Although highly prevalent in the community, NCDs were not conditions people proactively got checked for and diagnosed. Most of the participants did not know they had an NCD until they visited the hospital (OP/IP) owing to an acute health event. A male inland fisherman shared his experience- “I had an operation for hernia… It was then that I got to know that I have blood pressure and cholesterol. Since then, I have been undergoing treatment.” (I15M&F, high BP and high cholesterol).
There were also a few participants who consulted a doctor due to symptoms they faced early on. One participant was conscious of the impact of his alcohol intake on his health and hence would keep testing for NCDs.
There was greater outreach from the FHC in areas where seafaring fisherfolk lived. Participants reported that ASHAs and other field workers frequently visited their homes to monitor their health and urged them to visit the FHC if any issues were identified. A female participant from the seafaring community said: “They come every month and enquire if there are people with fever or any other health issues. If we say yes, they ask if we have medicines, even if it is for children. And they bring us medicines.” (S01F, high BP and high cholesterol). Conversely, this was not the case for inland fisherfolk, who rarely saw ASHAs or received such visits.
Preference for home-based care and remedies
Even when diagnosed, a few participants chose not to go for treatment at the hospital and treated it on their own based on knowledge passed down from elders or peers. A seafaring fisherman said-
When I first checked [for diabetes], I told them that I would do naturopathy (use of natural herbal medicines prepared at home). So we decided not to take allopathic medicines. We left the hospital fighting. I did not care about this for about 10 years. Then a check-up camp was conducted here… I was the first person to check… It was 400. (S09M&F, high BP and diabetes)
Homemade/home grown herbal preparation were also preferred by inland fishing community members for treating NCDs. The knowledge of homemade herbals was known by word of mouth, often passed down from previous generations. While many took these preparations alongside prescribed NCD medicines, others depended solely on herbal preparations, as mentioned by one of the inland fishermen,
When I started having sugar issues someone gave me some leaves and this plant. Since then, every morning, after brushing my teeth, I have one of those leaves. The taste of the leaf is very bitter. The bitterness stays in my teeth till the evening. Nobody eats these leaves, I eat them just because of the disease… These are medicines that are followed by our ancestors. The plant is here. If we plant just one, they will grow into a garden. (I14M, diabetes and high cholesterol)
Ability to seek
Delayed diagnosis, misdiagnosis
Since NCDs were typically checked for during acute health events, the diagnosis was often delayed, resulting in elevated NCD levels at the time of diagnosis. They were brushed off as a common ailment and neglected for a long time before the participants were finally diagnosed with an NCD. A woman from the seafaring community said-
At first, I used to get headaches and feel uneasy. I used to vomit. But we did not know that it was due to [blood] pressure issues, so we used to go and buy medicines for headaches from the store… We bought the medicines assuming that the headache was because of gas issues. Later we went to the hospital and when we did a check-up, the pressure was in the 200–220 range. (S11F, high BP)
An MO serving the seafaring community mentioned that there is a higher tendency for women to get diagnosed with NCDs early when compared to men in the community as they tend to be more aware of the ongoing symptoms. However, we did not see this distinction among our participants.
Prioritisation of family needs over self
Despite the necessity of medical attention, some participants admitted to neglecting their health due to caring for other sick family members who had exacerbated health conditions. An inland fisherman who was diagnosed with NCD said:
I have not gone [for consultation] yet since she (wife) is sick. She has uterus issues and cellulitis and has had two silent heart attacks. Since I have to take her to the hospital all the time, I have to suppress my health concerns. (I08M&F, high BP and high cholesterol)
Ability to reach
Public sector services available, but not timely, with indirect cost
There was substantial reliance on public facilities, more specifically FHC or CHC among seafaring fisherfolk. Participants who were engaged in seafaring relied heavily on the FHC in their area, as the treating doctor was perceived to be the best they could get. A woman from the seafaring community who visited the FHC said-
We go [to FHC] every month… For example, we bought medicine on the 25th of this month, so we have to go there on the 25th or 26th … and consult the doctor after which they will give us medicines. Even if he doesn’t go, one of us can go on his behalf and get the medicine (S09M&F, diabetes, high BP, and high cholesterol).
Participants engaged in inland fishing perceived government hospital treatment and facilities to be of substandard quality. Additionally, it was time-consuming and the operating hours of the FHC which were for first half of the day, usually until 12 pm/2 pm, were not matched with the times that fisherfolk could visit, given that they slept during the day and were working nights through early morning.
Visiting a public facility necessitated foregoing their daily wages as they had to abstain from work on that particular day. This was either for their own health needs or their family members for whom they were caregivers. A male inland fisherman said,
We have to take her every week to consult ENT for headache… Either I will take her or my son takes her… I cannot go with her after not sleeping. So I don’t go to work on those days. I cannot go out of the house if I have not slept the previous day. It is very difficult. – (I07M&F, high BP).
Owing to the private hospital’s relative proximity and superior facilities compared to the FHC, respondents expressed a preference for utilising the private hospital’s services.
Dual practice as access enabler
Many seafaring fisherfolk preferred going to private clinics run by public sector doctors in their homes. In fact, dual practice was highly prevalent among doctors in Alappuzha district and sought after for the treatment of general ailments. Seeking care from a public sector doctor’s private practice allowed for continued follow up and saved time, as at-home clinics would in general be less crowded than public facilities.
Some participants visited doctors in their private clinics, because the quality of care was perceived to be better than what they would receive at the public facility (linked again, to overcrowding in these facilities). As another male participant from the inland fishing community explained:
After consulting with the hospital, we took the doctor’s number and found his address… That is how we consulted there. The same was with cardiologists. We got good treatment after consulting at the doctor’s home. It is not about giving Rs.500 to the doctor. We get good treatment. (I15M&F, high BP and high cholesterol)
Ability to pay
Private sector timely, but unaffordable
Private facilities were available close to their places of residence and they received prompt service; therefore, they were less time-consuming. As a result, most preferred private facilities, even for non-emergency situations. However, visiting the private sector was expensive for the participants; which meant that sometimes people were forgoing treatment altogether or buying medicines from a private pharmacy without a consultation.
A woman from the inland fishing community, who had difficulty maintaining her and her husband’s medications due to financial issues, said-
Sometimes, when we don’t have enough money to go to the doctor’s, we buy the medicine from the local medical store. But those medicines are of a different brand and aren’t really effective… See, if it (hospital) is somewhere near here, we could limit our expenses… We didn’t even have the money to go to the doctor since we would [also] have to pay for our consultation fees; we just showed his prescription in the medical store and bought the medicine. (I16M&F, high cholesterol)
Receiving care in a private clinic would incur additional costs, as drugs would have to be procured from private pharmacies. When people could not afford this anymore, some switched treatment to visiting FHCs where drugs could be procured for free. This also happened in the case of a woman from the seafaring fishing community:
Now we don’t go to their (doctors') houses anymore. Two times we tried doing that but we cannot afford the medicines they prescribe. Since we get the medicines free of cost at the hospital, we prefer that… So we stopped going there and we continued going to government hospitals. (S01F, diabetes, high cholesterol)
Chronic ailments costly over time
Managing NCDs required continuous and expensive care-seeking, particularly when seeking private healthcare. Some participants revealed having to borrow money for their regular check-ups and the financial pressures they faced in trying to keep up with their medications while also sustaining the health and wellbeing of family members, as mentioned by a woman from inland fishing community:
I have to buy my medicines monthly. Yesterday I had to pawn my earrings to purchase medicines. We were going through a difficult time, so we were forced to pawn the earrings. We will take it back when we get some money. That’s how we manage. Nowadays, it’s tough. We can manage because of the ration shop. (I16M&F, high cholesterol)
Another woman from the seafaring community said-
If we go to work for 10–15 days, we might get only Rs.200–300 [in total]. How can we survive with that money when we have to educate two children and look after our old parents? We can’t survive with that money. We also have to buy our medicines. We need to have a substantial amount to purchase medication for three months. And the rate for these medicines increase or decrease by Rs.150 or Rs.180. If our children fall ill, we must also take them to the hospital. We somehow manage to survive with the little we get. But we know that the sea goddess won’t turn her back on us. (S06F, thyroid)
One strategy employed was refilling prescriptions at the FHC as they would be free. This was drawing some participants back to the public sector although they were not satisfied with the quality.
When we arrived at [name of private hospital removed], the [blood] pressure was high. They gave the medicines for asthma/breathlessness and [high blood] pressure… We had a lot of liabilities. We had a lot of financial liabilities after we married off our daughters… and that is when I went to the Government hospital… I thought that I would not be going there again. The medicine they gave had a very low dosage. (I05M, high blood pressure and asthma)
Ability to engage
Difficulties accommodating lifestyle changes
Considering a lifelong impact of the NCD, several participants shared how they changed their lifestyle after being diagnosed with an NCD. They mentioned quitting smoking, engaging in physical exercise, and altering their diet. For instance, an inland fisherman said, “I asked them if it was because of alcohol. I drink a lot of alcohol. And they told me to stop smoking, so I quit smoking. I haven’t smoked at all this year.” (I05M, high BP) Other participants reflected:
[My] cholesterol was slightly above the limit. I was asked to walk 45 min in the morning… I walk at five in the morning. After walking I will wait for some time because of leg pain. (S05F, thyroid)
First thing is that because of the sugar issue, I can’t eat anything properly. I would have rice for lunch and two wheat dosas for breakfast and dinner. That is the only food I have. When I went to the doctor they said I shouldn’t eat anything [unhealthy]. So I am not eating much these days. (I10M, diabetes)
Challenges with medication adherence
Medicines were sometimes not adhered to as prescribed. One male participant from the inland fishing community abstained from having the medicines, as it required him to stop alcohol consumption.
So when I bought the prescription here, they said that I should be having this medicine and while having these medicine I shouldn’t drink [alcohol]. I bought the medicines but I never have them. (I14M, diabetes and high cholesterol)
A few participants reported that they take the medicine along with them and consume it if they feel any uneasiness. These were sometimes the medications prescribed for NCDs to be taken every day but were not consumed in the prescribed manner. Others also carried over-the-counter prescriptions for these emergencies.
Occupational restrictions
The nature of NCDs also affected their occupation within the fishing industry; while some of their colleagues stopped working altogether, participants narrated that they took up less strenuous jobs or worked intermittently. An inland fisherman living with diabetes mentioned-
I have diabetes and arthritis. I was told by two hospitals that I should not work anymore. They told me not to go fishing anymore… or do any physical jobs. I took ayurvedic treatment for two months before starting to work again. (I09M, diabetes)
Other respondents from the seafaring community mentioned-
I used to go to work, but I quit after I was diagnosed with this disease. It has been 8 years. I used to go to peel prawn skin. Women who are older than me go there. There is a stench in our workspace so if I get dizzy or giddy it is hard to take me to hospital. So, my son asked me to not go there anymore. Even my husband won’t allow me to go there. (S11F, high BP)
I worked on the boat for eight to ten years (where fishermen worked for 10-15 days in the sea and came back with a yield)… I stopped because of this disease (Diabetes)… now I go on those small catamaran boats. (S09M&F, diabetes and high BP)
Those who continued to work often had to miss some days of working on a regular basis when they went for regular check-ups or if the illness worsened. An inland fisherman said “I stopped going [for work] for the last two weeks. [I had] diabetes, urinary infection, low level of potassium in body – because of these issues I was in the hospital for a week.” (I14M, diabetes and high cholesterol). Another fisherman mentioned- “The frequency of going to work is less nowadays because I am unwell. I go to work whenever they call me. But still, I am not well.” (S13M, high BP).
Discussion
Studies indicate a high prevalence of NCDs among the fisherfolk community in India [15, 16]. Through this study, where we looked at the healthcare experiences of fisherfolk communities when seeking care for NCDs, employing Levesque and colleagues’ framework, which assessed a series of abilities: to perceive, to seek, to reach, to pay, and to engage. We found that many participants were unaware of their NCDs while others relied on self care or home remedies. When seeking care, delayed or misdiagnosis was common, even as participants reported prioritising family obligations and needs over their care. When finally seeking care, participants noted long delays in the public sector, mitigated in situations where public providers also had private practice. This created a kind of continuum of provider for them as they traversed into the private sector, where care, while costly, was seen to require less time. Indeed, trajectories of diagnosis were seen to be similar for both the communities but the treatment seeking pathways differed. Sea-faring fisherfolk relied on public facilities like FHC for free medicines, while inland fishing participants preferred private clinics. Most concurred, though that private sector care was expensive and for some, unaffordable. Diagnosis of NCDs also led to difficult modifications in lifestyle, a host of medication adherence challenges, and occupational restrictions, which were seen as a major difficulty for the community.
We found that late diagnosis of NCDs was common among the community and at times, the presence of NCDs was known at an advanced stage. Delayed diagnosis can have profound consequences, as it may lead to a more advanced stage of the disease, complicating treatment and reducing overall chances of recovery [39].
Within the context of our study, a subset of participants openly acknowledged instances of neglecting their own health. This lapse was often attributed to the competing demands of daily life, occupational pressures, or the demanding responsibilities of caring for unwell family members. It underscores the complex interplay of caregiving roles and individual health management.
The significant variation in facility preference (public or private) was influenced by a multitude of factors. While service quality played a pivotal role, considerations such as service hours, availability, and timeliness also played a contributing role. Although not directly related by the participants, there seemed to be a direct relation to outreach activities by the ASHA workers and preference for availing the public healthcare facility, as ASHAs regularly visited and delivered medicines in Alappuzha, whereas in Kollam, their activity was minimal. Studies have shown that patient/public and health facility provider interactions influence the perceived quality of healthcare services [40]. It is possible, therefore, that the availability or lack of outreach activities by the public healthcare facilities influenced the perceptions of the community on the quality of healthcare provided which in turn influenced their preference for seeking healthcare. This was consistent with the findings of our larger study where various groups that were identified to be “vulnerable” by the system actors preferred facilities with better resources including outreach activities [36].
Our findings showed that seeking treatment in a public hospital is time-consuming, primarily attributable to the large number of patients in outpatient clinics. The existing infrastructure and human resources are unable to adequately manage the patient influx, consequently leading to prolonged waiting periods for individuals seeking medical attention [41]. This is further compounded by the limited working hours and facilities at the primary and sub-health centres leading patients to use services at higher facilities which already have a high traffic of patients [42]. As a result, patients often experience feelings of frustration and dissatisfaction due to the chaotic and impersonal nature of care delivery in such settings [41, 43, 44].
In an effort to avoid the overcrowded conditions, some participants in our study opted to visit public healthcare practitioners who maintained private clinics of their own. This dual practice phenomenon is present throughout the world in different forms. While some countries allow such practices, viewing them as a means to alleviate strain on public healthcare systems, others have implemented complete bans raising concerns about equity and resource allocation within the healthcare system [45]. In the Indian context, while a complete ban is not in place, such practice has been associated with negative impacts such as non-availability of doctors in public facilities during their working hours and lower quality of care [46, 47]. A novel finding of our study was that, notwithstanding supply constraints and concerns, fisherfolk participants saw dual practice as a kind of flexibility that gave them wider access to doctors that could accommodate their schedules, even if at some out of pocket expense.
Implications for research
The unique experience of dual practice in our study certainly warrants further study. Much research has focused on the system level impacts of dual practice: positive associations include improved access and range of services, as well as doctor satisfaction [47]. Overall, there appears to be little to no emphasis on how patients experience this phenomenon. Further, many of the conclusions drawn about dual practice, a 2017 review has found, are not empirical [48]. This is a ripe area for research. The ways in which caregiving roles interfere with care-seeking also requires further study. While it is conceivable that all family members could be included in the pursuit of a “healthy family,” there are likely to be gendered restrictions and internal household priority-setting that precludes such an approach. Understanding intra-familial and community norms/dynamics related to care-seeking would help shed light on this. Indeed in studies elsewhere in the world, there are reports of feminization of care-giving [49]. Yet, in our study, male members also reported having to neglect their health, although further study would be needed to more rigorously explore the gender dynamics of NCD management and addressing health and well-being within households. A more robust methodological approach, like ethnography, that can examine the macro-level features of economic insecurity and weathering, as well as meso and micro level risk factors for NCDs, would help to paint a more complete and accurate picture of NCD risk and care-seeking among various communities of fisherfolk.
Implications for policy
Our modest study revealed a convergence of self neglect, delayed diagnosis, cost and livelihood constraints owing to the onset of NCDs among Kerala fisherfolk. Such a complex of factors necessitates targeted, but also comprehensive policy approaches. Policy interventions directed towards working populations like fisherfolk should prioritise not only immediate (and likely shared) health concerns of the community such as improved access to quality healthcare services but also provide support for those adapting their occupations due to health challenges. The two communities involved in this study, although fisherfolk, were different in the way they sought care for their ailments. These differences could have been influenced by how they were geographically placed or other cultural factors in addition to the differences in the availability and accessibility of public healthcare facilities in the community. Further, other supply side policy options – for instance related to human resources (where it is recommended to restrict private practice altogether or offer non-performing allowances for public providers [50]) would have to be weighed against the access gaps this could introduce for fisherfolk. Upstream policy interventions – related to welfare, livelihood, etc., could be assessed for their health impacts and with greater inputs from community members, could be prepared for refinement and re-design.
Limitations
This was a pilot study conducted with limited resources. For one, fisherfolk with NCDs who shifted away from their occupation or transitioned to less strenuous roles within the fishing sector were excluded from the sample, as we were sampling those who were actively in fishing at the time of interviews. However, this population may offer important insights about how NCDs impact health and livelihoods. During recruitment, reasons cited for such transitions, including age and physical limitations, were interconnected with the prevalence of NCDs, as noted by a study which found association between advancing age and the occurrence of NCDs among fishermen, emphasizing the intricate relationship between occupational factors and health outcomes in this community [15]. This, along with other factors such as climate change, have challenged the sustainability of the occupation [51]. Occupation and health related issues in the fisherfolk community remain understudied and are a critical area of further work. The unavoidable presence of family members during interviews could have influenced the participant’s responses in the interview due to existing family dynamics. However, considering that in the Indian context family members have a major role to play in care seeking for the patient, we found that they were insightful with their presence. Therefore, at times this can be a strength and other times it can be a limitation.
Conclusion
This study found significant challenges in NCD healthcare-seeking across the care continuum for two groups of fisherfolk in Kerala. Fisherfolk reported self neglect, delayed diagnosis, cost and livelihood constraints owing to the onset of NCDs, even as dual practice and medicine access in the public sector were appreciated. Demand side explorations of the impact of dual practice warrant further study, as does the role of intrahousehold decision-making related to health. Upstream policy interventions that could address the economic and livelihood related impacts of NCD care-seeking require both research and policy attention. Overall, larger studies and policymaking processes should consider in depth the experiences faced by particular economic groups like fisherfolk, who may face unique health and care-seeking challenges.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- NCDs:
-
Non-Communicable Diseases
- WHO:
-
World Health Organization
- UHC:
-
Universal Health Coverage
- LSG:
-
Local Self-Governement
- MO:
-
Medical Officer
- FHC:
-
Family Health Centre
- CHC:
-
Community Health Centre
References
World Health Organization. Non communicable diseases. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. Cited 2022 Aug 16.
Alliance NCD, The George Institute for Global Health. Paying the price: a deep dive into the household economic burden of care experienced by people living with noncommunicable diseases. Geneva: NCD Alliance; 2023. https://ncdalliance.org/resources/paying-the-price-a-deep-dive-into-the-household-economic-burden-of-care-experienced-by-people-living-with-NCDs.
Banatvala N, Bovet P. Noncommunicable Diseases: A Compendium. 1st ed. London: Routledge; 2023. Available from: https://www.taylorfrancis.com/books/9781003306689. Cited 2023 Mar 14.
Valtorta NK, Hanratty B. Socioeconomic variation in the financial consequences of ill health for older people with chronic diseases: a systematic review. Maturitas. 2013;74(4):313–33.
Kochovska S, Luckett T, Agar M, Phillips JL. Impacts on employment, finances, and lifestyle for working age people facing an expected premature death: a systematic review. Palliat Support Care. 2018;16(3):347–64.
Murphy A, McGowan C, McKee M, Suhrcke M, Hanson K. Coping with healthcare costs for chronic illness in low-income and middle-income countries: a systematic literature review. BMJ Glob Health. 2019;4(4):e001475.
Indian Council of Medical Research, Public Health Foundation of India, and Institute for Health Metrics and Evaluation. India: Health of the Nation’s States- The India State-Level Disease Burden Initiative. New Delhi: ICMR, PHFI, and IHME; 2017.
Sarma PS, Sadanandan R, Thulaseedharan JV, Soman B, Srinivasan K, Varma RP, et al. Prevalence of risk factors of non-communicable diseases in Kerala, India: results of a cross-sectional study. BMJ Open. 2019;9(11):e027880.
National action plan and monitoring framework for prevention and control of noncommunicable diseases (NCDs) in India. Ministry of Health and Family Welfare, Government of India. Developed through the WHO-Government of India 2012–2013 biennial work plan. World Health Organization. Available from: https://www.iccp-portal.org/sites/default/files/plans/National_Action_Plan_and_Monitoring_Framework_Prevention_NCDs.pdf.
Ministry of Health and Family Welfare, Government of India. National multisectoral action plan for prevention and control of non-communicable diseases. New Delhi; 2017. Available from: https://main.mohfw.gov.in/sites/default/files/National%20Multisectoral%20Action%20Plan%20%28NMAP%29%20for%20Prevention%20and%20Control%20of%20Common%20NCDs%20%282017-22%29_1.pdf. Cited 2022 Sep 15.
Nambiar D, Sankar DH, Negi J, Nair A, Sadanandan R. Monitoring universal health coverage reforms in primary health care facilities: creating a framework, selecting and field-testing indicators in Kerala, India. PLoS One. 2020;15(8):e0236169.
NHSRC. National Health Systems Resource Centre. Operational guidelines for comprehensive primary health care through health and wellness centers | National Health Systems Resource Centre. 2018. Available from: https://nhsrcindia.org/node/736. Cited 2023 Feb 14.
Fisheries handbook 2020. Kerala: Department of Fisheries, Government of Kerala; 2020. Available from: https://fisheries.kerala.gov.in/sites/default/files/inline-files/FISHERIES%20HAND%20BOOK%202020_1.pdf.
Annadurai K, Balan N, Ranaganathan K. Non-communicable disease risk factor profile among fishermen community of Kancheepuram district, Tamil Nadu: a cross sectional study. Int J Community Med Public Health. 2018;5(2):708–13.
Doddamani A, Ballala ABK, Madhyastha SP, Kamath A, Kulkarni MM. A cross-sectional study to identify the determinants of non-communicable diseases among fishermen in Southern India. BMC Public Health. 2021;21(1):414.
Annadurai K. Health seeking behavior on child care among fishermen community of Kovalam Village, Tamil Nadu, India. Online J Health Allied Sci. 2015. Available from: https://www.semanticscholar.org/paper/Health-Seeking-Behavior-on-Child-Care-Among-of-Annadurai/afc2b081f35bfc8613ad5570ac915c55bc48b2db. Cited 2022 Aug 5.
Neethiselvan R, Gayathri S, Shanmughapriya P. Assessment of health seeking behaviour among fishermen community in Puducherry. Int J Community Med Public Health. 2021;8(2):732–6.
145 Fishermen died at sea in 5 years in Thiruvananthapuram; highest in Kerala. The Times of India; 2021. https://timesofindia.indiatimes.com/city/thiruvananthapuram/145-fishermen-died-at-sea-in-5-years-highest-in-kerala/articleshow/87842439.cms. Cited 2022 Jun 28.
The New Indian Express. Alappuzha: boat accident leaves Tharayilkadavu devastated. 2021. https://www.newindianexpress.com/states/kerala/2021/sep/03/alappuzha-boat-accident-leaves-tharayilkadavu-devastated-2353547.html. Cited 2022 Jun 28.
The New Indian Express. Kerala: speed boat driver’s daredevilry saves three fishermen from choppy sea. 2021. https://www.newindianexpress.com/states/kerala/2021/sep/13/kerala-speed-boat-drivers-daredevilry-saves-three-fishermen-from-choppy-sea-2358051.html. Cited 2022 Jun 28.
Vizhinjam boat accident: bodies of two more fishermen recovered. The Hindu; 2021. https://www.thehindu.com/news/national/kerala/vizhinjam-boat-accident-bodies-of-two-more-fishermen-recovered/article34655345.ece. Cited 2022 Apr 18.
Al-Mawali A. Non-communicable diseases: shining a light on cardiovascular disease, Oman’s Biggest Killer. Oman Med J. 2015;30(4):227–8.
Asawa K, Pujara P, Tak M, Nagarajappa R, Aapaliya P, Bhanushali N, et al. Oral health status of fishermen and non-fishermen community of Kutch district, Gujarat, India: a comparative study. Int Marit Health. 2014;65(1):1–6.
Kurien J. Overcoming factors of unsustainability and overexploitation in fisheries: selected papers on issues and approaches. In: Overcoming factors of unsustainability and overexploitation in fisheries: selected papers on issues and approaches. Rome: Food and agriculture organization of the united nations; 2004. https://www.fao.org/4/a0312e/A0312E17.htm. Cited 2024 May 30.
Devika J. Surviving in contemporary Kerala: reflections from recent research in a Fisher Village. Dev Change. 2017;48(2):364–86.
Salim SS, Sathianandan TV, Mohamed KS, Narayankumar R, Athira NR. A Fisher Development Index (FDI) for assessing human development in marine fishers of Kerala, India. Environ Dev Sustain. 2024. https://doi.org/10.1007/s10668-024-04923-9. Cited 2024 May 30.
Sheeja SR, Rahi TB, Ajay A. State led social security and inclusion of marine fisherfolk: analyzing the case of Kerala, India. Mar Policy. 2023;147:105392.
Samantray K, Pathak SC. An overview of women in the Indian fisheries sector and suggestions for improvement of their socioeconomic status. In: International Symposium on Women in Asian Fisheries. Chiang Mai: ICLARM-The World Fish Centre; 1998.
Recognizing the invisible role of women in India’s fisheries. 2022. https://blogs.dal.ca/openthink/recognizing-the-invisible-role-of-women-in-indias-fisheries/. Cited 2022 Jun 28.
Devika J. Land, Politics, Work and Home-life at Adimalathura: Towards a Local History. Centre for Development Studies; 2014. p. 64.
Sruthi P, Jayalal L, Gopal N. Gender roles in fisheries along the vembanad estuarine system. Asian Fish Sci. 2016;29S (Gender in Aquaculture and Fisheries: The Long Journey to Equality):193–203.
Shyam SS, Geetha R. Empowerment of fisherwomen in Kerala – an assessment. Indian J Fish. 2013;60(3):73–80.
Rane PP, Narayanan P, Binu V, Unnikrishnan B. Prevalence of tobacco and alcohol consumption among fishermen in Udupi Taluk’ Karnataka, India: a cross-sectional study. Asian Pac J Cancer Prev. 2016;17(4):1733–7.
The George Institute for Global Health. Assessing equity of universal health coverage in India: From data to decision-making using mixed methods. Available from: https://www.georgeinstitute.org/projects/assessing-equity-of-universal-health-coverage-in-india-from-data-to-decision-making-using. Cited 2024 Jan 31.
Joseph J, Sankar H, Benny G, Nambiar D. Who are the vulnerable, and how do we reach them? Perspectives of health system actors and community leaders in Kerala, India. BMC Public Health. 2023;23(1):748.
Surendran S, Joseph J, Sankar H, Benny G, Nambiar D. Exploring the road to public healthcare accessibility: a qualitative study to understand healthcare utilization among hard-to-reach groups in Kerala, India. Int J Equity Health. (in press).
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847.
Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18.
Bhor N. Care-seeking practices for non-communicable chronic conditions in a low-income neighborhood in Southern India. PLOS Glob Public Health. 2023;3(6):e0002074.
Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manag. 2014;3(2):77–89.
Agarwal SK. Healthcare in India and violence against doctors: the missing links. Indian J Nephrol. 2019;29(4):221–31.
Bajpai V. The challenges confronting public hospitals in India, their origins, and possible solutions. Adv Public Health. 2014;2014:e898502.
Overflowing patient pool in understaffed hosp. The Times of India; 2023. Available from: https://timesofindia.indiatimes.com/city/mumbai/overflowing-patient-pool-in-understaffed-hosp/articleshow/102706123.cms. Cited 2024 Jan 31.
Mishra S. Hospital overcrowding. West J Med. 2001;174(3):170.
García-Prado A, González P. Policy and regulatory responses to dual practice in the health sector. Health Policy. 2007;84(2):142–52.
Hoogland R, Hoogland L, Handayani K, Sitaresmi M, Kaspers G, Mostert S. Global problem of physician dual practices: a literature review. Iran J Public Health. 2022;51(7):1444–60.
Hipgrave DB, Hort K. Dual practice by doctors working in South and East Asia: a review of its origins, scope and impact, and the options for regulation. Health Policy Plan. 2014;29(6):703–16.
Moghri J, Rashidian A, Arab M, Akbari Sari A. Implications of dual practice among health workers: a systematic review. Iran J Public Health. 2017;46(2):153–64.
Alves EV, da Flesch C, Cachioni LD, Neri M, Batistoni AL. The double vulnerability of elderly caregivers: multimorbidity and perceived burden and their associations with frailty. Rev Bras Geriatr E Gerontol. 2018;21:301–11.
Manoj Kadambad. Kerala to rein in private practice of government doctors. Onmanorama. 2023. Available from: https://www.onmanorama.com/news/kerala/2023/08/13/strict-action-to-restrict-private-practice-by-government-doctors.html. Cited 2024 May 22.
How climate change is destroying fishing livelihoods in Kerala. Available from: https://www.indiatoday.in/india-today-insight/story/how-climate-change-is-destroying-fishing-livelihoods-in-kerala-1977330-2022-07-19. Cited 2023 Sep 30.
Acknowledgements
This work was supported by the Wellcome Trust/DBT India Alliance Fellowship (Grant number IA/CPHI/16/1/502653) awarded to Dr. Devaki Nambiar. We express our gratitude to our interview participants who shared their thoughtful reflections with us and for making time out of their busy schedules. We are also grateful for the support of the Kerala Department of Health and Family Welfare as well as various Local Self Government Institutions in Kerala and other key informants in the community.
Funding
This study was funded by Wellcome Trust/DBT India Alliance Fellowship (https://www.indiaalliance.org) (Grant number IA/CPHI/16/1/502653) awarded to Dr. Devaki Nambiar.
Author information
Authors and Affiliations
Contributions
SS contributed to study design and inception, data collection, coding and analysis, writing and finalising the manuscript. GB contributed to coding and data analysis and reviewing of manuscript. JJ contributed to data analysis and reviewing of manuscript. DN contributed to study design and inception, supervision of study, data analysis, reviewing and finalising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Ethics Committee of the George Institute for Global Health approved this study with ethical clearance (Project Number 05/2019) which abides by the Declaration of Helsinki and 2017 guidelines of Indian Council of Medical Research (ICMR). Before initiating fieldwork, the LSG leaders and MOs at primary healthcare centers were informed about the study, and the proposal was shared for their approval. Prior to participation in interviews, informed verbal consent was obtained from all participants, ensuring their understanding and voluntary involvement in the research. Confidentiality measures were strictly upheld, as only researchers were granted access to participants' identifiable information, thereby safeguarding their privacy and data confidentiality
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Surendran, S., Benny, G., Joseph, J. et al. Navigating delayed diagnoses, self-neglect, and lost livelihoods: a qualitative exploration of fisherfolk’s health perspectives and management of non-communicable diseases in Kerala, India. BMC Prim. Care 25, 354 (2024). https://doi.org/10.1186/s12875-024-02575-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02575-2