Abstract
Background
Primary care plays a central role in most, if not all, health care systems including the care of vulnerable populations such as people who have been incarcerated. Studies linking incarceration records to health care data can improve understanding about health care access following release from prison. This review maps evidence from data-linkage studies about primary care use after prison release.
Methods
The framework by Arksey and O’Malley and guidance by the Joanna Briggs Institute (JBI) were used in this review. This scoping review followed methods published in a study protocol. Searches were performed (January 2012-March 2023) in MEDLINE, EMBASE and Web of Science Core Collection using key-terms relating to two areas: (i) people who have been incarcerated and (ii) primary care. Using eligibility criteria, two authors independently screened publication titles and abstracts (step 1), and subsequently, screened full text publications (step 2). Discrepancies were resolved with a third author. Two authors independently charted data from included publications. Findings were mapped by methodology, key findings and gaps in research.
Results
The database searches generated 1,050 publications which were screened by title and abstract. Following this, publications were fully screened (n = 63 reviewer 1 and n = 87 reviewer 2), leading to the inclusion of 17 publications. Among the included studies, primary care use after prison release was variable. Early contact with primary care services after prison release (e.g. first month) was positively associated with an increased health service use, but an investigation found that a large proportion of individuals did not access primary care during the first month. The quality of care was found to be largely inadequate (measured continuity of care) for moderate multimorbidity. There were lower levels of colorectal and breast cancer screening among people released from custody. The review identified studies of enhanced primary care programmes for individuals following release from prison, with studies reporting a reduction in reincarceration and criminal justice system costs.
Conclusions
This review has suggested mixed evidence regarding primary care use after prison release and has highlighted challenges and areas of suboptimal care. Further research has been discussed in relation to the scoping review findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
More than 10.7 million people are incarcerated globally [1]. The prison population is recognised by the United Nations as a vulnerable and marginalised group that may be subject to discrimination and exclusion after release [2]. Health care in prison differs between countries, and after release from incarceration, individuals will navigate different health services and systems [3,4,5]. Policies for health care after release from prison (including the transfer or sharing of medical information) may improve the transition to primary care, and continuity of care may expedite linkage with appropriate community services for individuals with low engagement during a time of increased vulnerability [5]. Co-ordinating re-entry into society after release from prison can be difficult, for example individuals may experience limitations in accessing health and social services, housing and employment [6]. Furthermore, there is an elevated risk of morbidity and mortality after release from incarceration [7,8,9,10].
Studies linking incarceration records to health care data can help identify trends and/or patterns in use of different health care settings following release from prison, determine facilitators/difficulties in accessing care and health-related or other outcomes, which can help profile people who are most at risk following release from prison. Research on emergency department attendance after release from prison and reason(s) for attending is important to help understand who is most likely to require urgent care and when. For example, a cohort study in Canada, reported higher rates of emergency department use during the two years after release compared to the general population, with rates highest in the week after release from prison [11]. Most emergency department visits in the 2 years post-release were classed as high urgency (and commonly related to injury and mental health disorders) [11].
This review focuses on primary care use after release from prison due to reports about access problems, low uptake and poor connectivity. For example, a retrospective cohort study in Canada linked prison correctional services data and health administrative data and reported a significantly lower primary care attachment (i.e. use of a community health centre, enrolment in a primary care model or history of primary care fee codes) among individuals during the two years before entry into prison and in the two years after release (in comparison to the general population) [12]. During the two years after release, approximately one-quarter of people with specific chronic conditions were not attached to primary care [12]. Using the same linked data cohort in Canada, a separate retrospective study reported that approximately two-thirds of women and three-quarters of men did not access primary care during the first month after release from prison [13]. However, the study reported a higher relative rate of primary care use among people in prison and post-release compared to the general population [13].
Purpose of this scoping review
The evidence around data-linkage studies of primary care use after release from prison has not been mapped and this review aims to address this gap. This review will be used to inform research undertaken by our ESRC-funded Administrative Data Research Centre (ADRC) about health after release from prison and therefore will focus on observational record-linkage studies in keeping with the remit of ADR UK. For example, the use administrative data and the ability to draw from multiple data sources can accurately assess health outcomes after prison release at various time points (i.e. first month or year) thereby maximising potential for timely intervention and post-release follow-up for at-risk individuals. In this review, we will scope the research literature on record linkage studies about primary care after prison release to identify, map and summarise studies, and will report, compare and comment on methodologies used to conduct this research, for example, study designs, outcomes and gaps in knowledge. This review may be used to inform future epidemiological research studies and targeted interventions for people at-risk following release from prison, leading to improvements in continuity of care.
Methods
Detailed methods for this scoping review have been published in a study protocol [14]. Five stages of the framework by Arksey and O’Malley were used in this review, and the Joanna Briggs Institute (JBI) guidance was consulted during the development stage [15, 16]. A completed Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist is provided in appendix 1) [17].
Stage 1: identifying the research questions
As published in the study protocol [14], the scoping review questions were:
-
1.
What is the scope of the research literature on record linkage studies about primary care after prison release?
-
2.
What methodologies are reported in these studies?
-
3.
What are the findings in relation to primary care contact by people released from prison (including any hand-over arrangements and accessing and using primary care) and any reported health or prison related outcomes?
-
4.
Where are the knowledge gaps in this area?
Stage 2: identifying relevant studies
A MEDLINE search strategy relating to (i) people who have been incarcerated and (ii) primary care was developed by JAC and MD, and refined by the Subject Librarian for the School of Medicine, Dentistry and Biomedical Sciences in Queen’s University Belfast (published with the study protocol [14]). Separate search strategies for EMBASE and Web of Science Core Collection were developed by JAC and MD. All search strategies used in this scoping review are provided in appendix 2. The literature databases were searched from January 2012 to March 2023 to review the most recent literature. The search strategies included publications available in English only (due to resources for translation). Grey literature was not searched as part of this review. References of included studies were screened by JAC to identify any additional publications.
Stage 3: study selection
MEDLINE, EMBASE and Web of Science Core Collection searches were performed by JAC on 29th March 2023 with the results combined in Endnote (Reference Manager) and duplicate publications removed. The inclusion and exclusion criteria used to determine study eligibility (as per study protocol [14]) are provided in Table 1. Two authors (JAC and SM) independently screened titles and abstracts (step 1). Publications were subsequently screened in full (step 2), if the publication seemingly met the eligibility criteria in step 1, or if there was any uncertainty regarding eligibility. Two authors (JAC and SM) independently screened full publications in step 2, and any disagreements in eligibility were discussed with a third author (MD).
Stage 4: charting the data
In the protocol development, a data charting form was piloted by two authors [14]. Before conducting stage 4 of the review, the charting form was retested. Two authors (JAC and SM) extracted information from a sample of the included studies (n = 3) using the charting form and discussed the consistency and accuracy of the recorded data. These discussions resulted in further modifications to the charting form. The data charting form used in the review is provided in appendix 3. The two authors (JAC and SM) who tested the form, subsequently charted data from included publications independently. Any discrepancies in the charting forms were initially discussed by the two extracting authors (JC and SM); and any resulting disagreements were discussed with a third author (MD). Some corresponding authors of included publications were contacted for further information at this stage.
Stage 5: collating, summarising and reporting the results
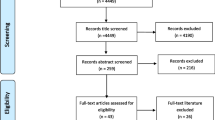
A flow diagram of the review process (including search results and study selection stages) is shown in Fig. 1. Information collated in the charting forms was entered into Microsoft Excel sheets for data management and cleaning. To answer the review questions, findings were mapped by methodology, key findings and gaps in research and summary tables (for example, key characteristics and methodological features of included studies) were populated.
Ethics approval and stakeholder engagement
Ethical approval was not required (as the review comprised publicly available sources of research). The review was discussed regularly at meetings with staff representatives from the Northern Ireland Healthcare in Prison Service (HIPS) including the Clinical Director and senior management of HIPS.
Results
A total of 1,339 publications (MEDLINE n = 189, EMBASE n = 523 and Web of Science Core Collection n = 627) were identified. Following the removal of 289 duplicate publications, 1,050 publications were screened by title and abstract (step 1). 63 publications were fully screened by reviewer 1. 87 publications were fully screened by reviewer 2. Following full screening, 28 publications were discussed with reviewer 3 (as a result of discrepancies between reviewer 1 and 2). Of the 28 publications screened by reviewer 3, 13 were excluded, 2 were included and the remaining 13 were discussed with reviewer 1 (as there was no agreement or an unsure decision remained). Of the 13 publications discussed, six were included and the remaining seven publications were excluded (reasons for exclusion were no data linkage [18,19,20,21,22,23] and no substantial data on primary care use [24]). Therefore, data were charted for 22 publications. However, five studies passed through the earlier screening stages but on closer inspection of the full text at data extraction stage, the paper(s) did not contain data about the key variables and outcomes of interest. The reasons for exclusion at this stage were: no results on health service use data [25], unclear data regarding where and when there were opportunities for this population to avail of primary care-based screening [26], medical care in study not restricted to primary care [27], primary care visits may have occurred before or after a participant’s involvement in correctional control [28], health data not restricted to primary care [29]. In total, 17 publications were included in the review. Reference lists of the 17 included studies were screened by one author (JAC); no additional publications were added to the review.
What is the scope of the research literature on record linkage studies about primary care after prison release?
The characteristics of the included studies are provided in Table 2. Of the 17 studies included in this review, 12 were published since 2019. The included publications were across 14 different journals; the most common journal was BMC Health Services Research (n = 3). The included studies were published across four different locations. The locations were Canada (n = 9), Australia (n = 3), USA (n = 3), The Netherlands (n = 1) and in one publication the location was not stated. Included publications investigated primary health care during the transition from prison to community living. The custodial settings differed between studies, for example, ‘prison’ was commonly reported, as was ‘provisional prison(s)’ e.g. representing all provincial correctional facilities, including jails, detention centres, and correctional centres. The most common health care use investigated in included studies was primary care visits (for example use, time to first contact and quality of care).
Further characteristics of the included studies are provided in Appendix 4, including sources of data. The number of participants ranged from 94 to 48,861 (Appendix 4). The largest studies were Kouyoumdjian et al. 2018 [13] and Kouyoumdjian et al. 2019 [12]. The smallest studies were Harvey et al. 2022 [33] and Wang et al. 2019 [43]. Age was reported in eight of the included studies but was not provided in five studies and was unclear in one study. Three studies reported the inclusion of ‘adults’ but did not specific a cut-off age (Appendix 4). Sex or gender was reported in all included studies (Appendix 4). Race or ethnicity was reported 14 studies (Appendix 4).
Five publications reported using a checklist or technique for quality assessment (Table 2). One study reported using Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement [30]. Two studies reported using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [36, 40]. Two studies reported using both STROBE and RECORD [12, 38].
What methodologies are reported in these studies?
The methodological features of the included studies are provided in Table 3. The study design was stated in all included publications. The most common design was a cohort study (n = 14). Other designs (as defined) included a propensity-matched study, a quasi-experimental study, and a randomised controlled trial (RCT). The most common method of data linkage was linkage by unique identifiers. The methods of data linkage were not reported in six of the included publications, although one study cited methods published in another study. The most common time periods examined after release from prison were one- or two-years follow-up. The years of linked data was provided in 16 publications (in one study the years were unclear). The earliest year of data linked was 2005 and the most recent was 2018.
Re-incarceration poses potential methodological issues for the study of primary care use. If a person returned to prison or had repeated incarcerations during the study follow-up period, the individual would have varied access to primary care services. For example, data would not be collected in primary care records during re-incarceration periods when individuals are in custody (rather than community). Dates of subsequent incarcerations may be used to determine when primary care could not be accessed by an individual, otherwise there may be an assumption that an individual was still living in the community setting but was not accessing primary care services. The number of repeat incarcerations over a defined study (and duration of time spent in custody), can provide insight into recidivism patterns, risk and outcomes (for example, increased risk of morbidity and mortality after release from prison). The methods used to address re-incarceration were excluding time spent in prison during re-incarceration [12, 30, 31, 39], censoring follow-up at re-incarceration [13, 35] e.g. right censoring the post-release follow up period at the earliest of death, loss of health insurance eligibility, re-admission to prison or two years post-release [13], using re-incarceration as a study outcome [37, 40, 42, 43], measuring the study exposure of interest (e.g. stimulant use disorder diagnosis) as time varying for each release from prison [41], and using interval-truncation for periods of re-incarceration(s) during the follow-up period (multivariate Andersen-Gill extension of a Cox proportional hazards model) as individuals were not ‘at-risk’ of using health services in the community setting while in custody [44]. However, some publications did not address repeated incarceration during the study period or methods were unclear [32, 34, 36, 38]. In one study, claims data were not covered during re-incarcerated [33].
What are the findings in relation to primary care contact by people released from prison (including any hand-over arrangements and accessing and using primary care) and any reported health or prison related outcomes?
A summary of the outcomes reported in the included studies is provided in Appendix 5. Most of the included studies reported primary care use during the follow-up period (including rates of use, visits, access, time to first contact, attachment, attending a general practice for a specific health problem and quality of care). Table 4 shows the investigations using data to report the primary care use after release from prison. Other reported outcomes included community dispensed medications, breast and colorectal cancer screening, timeliness of mental health services access and health care services costs.
A summary table of the reported results from the included studies is provided in Appendix 6. Findings are mapped by the following categories:
Primary care use
Of the 17 included studies, 13 studies investigated primary care use (including quality, attendance, engagement and attachment) after release from prison [12, 13, 30,31,32, 34,35,36,37, 39, 42,43,44].
A cohort study investigated multimorbidity and quality of primary care in the two years after release from prison [30]. The study reported that people with moderate (2–3 domains) and complex (≥ 4 domains) multimorbidity were more likely to have a high rate of primary care contact (defined as ≥ 9 contacts per-person/year) [30]. The study measured continuity of care via the Usual Provider Continuity Index (UPCI) and the index of Continuity of Care (COC) [30]. Complex multimorbidity was associated with adequate continuity of care [UPCI (AOR 1.83, 95%CI 1.20–2.80), COC (AOR = 1.87; 95%CI 1.22–2.84), and ≥ 1 long consultation (≥ 20 min) (AOR 2.52, 95%CI 1.59–4.00)] [30]. However, moderate multimorbidity was not associated with adequate continuity of care [(UPCI or COC) but was associated with ≥ 1 long consultation (AOR 1.64, 95%CI 1.14–2.39) in the two-year period after release from prison [30].
A cohort study investigated rates of GP attendance after release from prison [31]. GP attendance was higher for people after prison release than the general population (standardised rate ratios (SRR) 2.04, 95%CI 2.00-2.07) [31]. In the two-year follow-up after release, most people (87%) had ≥ 1 contact with a GP [31]. Among people released from prison, GP attendance rates were higher for people with a history of risky opiate use (Adjusted incidence rate ratios (IRRs) 2.09, 95%CI 1.65–2.65), diagnosis of a mental health condition (Adjusted IRR 1.32, 95%CI 1.14–1.53) or medication in prison (Adjusted IRR 1.82, 95%CI 1.58–2.10) [31]. However, people who have been incarcerated with a history of risky methamphetamine use had a lower GP attendance rate (Adjusted IRR 0.71, 95%CI 0.58–0.88) [31].
A cohort study examining mental and physical health conditions found complex health needs both before and after incarceration, with custody having neither a health deteriorating nor improving effect [32]. The study examined any GP contact for a specific health condition in a one-year period. The examination of health changes among males, pre- to post-incarceration, found only one statistically significant change, with males more likely to report circulatory problems in the year post-incarceration (compared to year pre-detention) (OR 1.36, 95%CI 1.04–1.79) [32]. There were no differences in the change in prevalence rates for health conditions from pre- to post-detention between males released from prison and controls [32]. Among females there was a significant difference in the changes in general and unspecified health problems (Ratio of Odds Ratios: OR 1.92, 95%CI 1.05–3.53) [32]. Among females, pre- to post-incarceration, the prevalence of general and unspecified health problems increased, but for the controls, the prevalence of such health problems decreased [32].
An observational study used survey data regarding incarceration history (as part of data-linkage) to determine the influence of primary care engagement on the relationship between incarceration history and blood pressure control [34]. People with recent incarceration were 1.5 times more likely to have uncontrolled blood pressure compared to people never incarcerated (AOR 1.57, 95% CI: 1.09–2.26; covariates adjusted for in this model included primary care engagement pre-survey) [34]. Primary care engagement post-survey was not associated with incarceration history (exposure) and uncontrolled hypertension (outcome) [34].
A cohort study examined rates of primary care use after release from prison for people with HIV [35]. Rates of primary care use among people with HIV released from prison were higher at 30, 90 and 365 days after release compared to control groups (controls were individuals released from prison HIV-negative, general population HIV-positive and general population HIV-negative) [35]. The study found that after release from prison, people with HIV experienced a longer time to first contact with HIV ambulatory care, and rates of health care use across health care settings were elevated [35].
A cohort study examined primary care use among people released from prison (compared to the general population) [13]. The study found that primary care use was high in prison and after release [13]. An investigation of the time to first contact with primary care after prison release found low access to primary care during the first month (for example, in the month after release, 66.3% of women and 75.5% of men had not used primary care; within three months after release, 50.5% of women and 62.9% of men had not used primary care, and within two years after release, 16.8% of women and 28.2% of men had not used primary care) [13].
A cohort study which examined the use of primary care in the two years prior to entering prison and two years after release found lower primary care attachment among people who have been incarcerated compared to the general population [12]. Attachment to primary care in two years after release was 63.0% in people released from prison and 84.4% in the general population corresponding period (P < .001) [12]. Attachment to any team-based primary care in the two years after release was 19.9% in people released from prison compared to 21.6% in the general population corresponding period (P < .001) [12].
A cohort study examined (1) the 30-day medical-surgical readmission to hospital for people who have been incarcerated and (2) access to care after hospital discharge including primary care [36]. Compared with the general population, people in prison were more likely to access primary care in the 7 days after hospital discharge and people recently released from prison were more likely to access emergency department care in the 30 days after hospital discharge [36].
A cohort study examined reincarceration of people with schizophrenia after release from custody with secondary outcomes investigating correctional events and health service use (including primary care) [37]. The study found that reincarceration was higher among people with schizophrenia [37]. People with schizophrenia had higher rates of all primary care health service use (i.e. primary care physician visits including all contact, and mental health–related and non-mental health–related contact) in the 5 years following release from custody compared to people without schizophrenia [37].
A cohort study compared the health of females following release from prison with two control groups: (1) males released from prison and (2) females in the general population [39]. The study found higher morbidity and specific psychiatric conditions among females who have been incarcerated compared with the control groups, and after release from prison, females had higher rates of primary care use in all periods (follow-up until 730 days post-release) compared to the controls [39].
A randomized controlled trial compared two interventions in primary care after release from prison: (1) a Transitions Clinic consisting of a primary care provider (who had experience working with people after incarceration) and a community health worker (with personal history of incarceration) and (2) an expedited primary care appointment at another clinic) [42]. The trial reported similar rates of primary care use in both arms (Transitions Clinic 37.7% vs. expedited primary care appointment 47.1%) after 12 months of follow-up [42]. However, the Transitions Clinic arm had lower rates of emergency department use compared to expedited primary care appointment (25.5% vs. 39.2%, P = .04) [42].
A quasi-experimental study examined the provision of enhanced primary care (Transitions Clinic Network (TCN) providing increased access to primary care services following release from prison) and criminal justice system contact [43]. The study found that people experiencing enhanced primary care after release from prison were less likely to return to prison for a parole or probation technical violation (AOR 0.38, 95%CI 0.16–0.93) and have fewer incarceration days (adjusted incidence rate ratio: 0.55, 95%CI 0.35–0.84) [43].
A cohort study investigated the relationship between primary care physician contact during the first month after prison release and health service use in the six months following release [44]. The study found that contact with primary care physician services early after prison release increased health service use [44]. Primary care physician contact in the first month after release was positively associated with hospital health services use (AHR 2.07, 95%CI 1.39–3.09), mental health services use (AHR 1.65, 95%CI 1.24–2.19), alcohol and other drug health services use (AHR 1.48, 95%CI 1.15–1.90) and further primary care physician service use (AHR 1.47, 95%CI 1.26–1.72) during a sixth month follow-up [44].
Mental health services access
One included study investigated mental health services access after release from prison [40]. The cohort study reported that mental health services access was associated with reduced reincarceration risk (HR 0.61, 95%CI 0.39–0.94) [40]. However, this risk was increased by each additional month post-release before access to mental health services [40]. The reincarceration risk was significantly higher for outpatient emergency care (mental health services) (HR 1.41, 95%CI 1.08–1.83) compared with outpatient primary care (mental health services) [40].
Community dispensed medications
Two studies examined community dispensed medications after release from prison [34, 41]. The first included study was an observational design which used mediation analyses to determine the influence of antihypertensive adherence (via pharmacy refill data) on the relationship between incarceration history and blood pressure control [34]. The study reported that recent incarceration was associated with uncontrolled blood pressure after release (in people with a history of hypertension) [34]. People with recent incarceration were 1.5 times more likely to have uncontrolled blood pressure compared to people never incarcerated (AOR 1.57, 95%CI: 1.09–2.26; covariates adjusted for in this model included primary care engagement prior to the survey) [34]. However, the adjusted odds ratio of recent incarceration compared to never incarceration was not significantly impacted with the addition of antihypertensive adherence (AOR 1.58, 95%CI: 1.09–2.27) [34]. The second included study that examined community dispensed medications after release from prison was a cohort study investigating the impact of stimulant use disorder diagnosis on post-release opioid agonist treatment dispensation [41]. The study reported that approximately one-quarter of individuals with an opioid use disorder received opioid agonist treatment dispensation within two days of release from prison [41]. Furthermore, the study found that individuals with mental illness (based on one hospital record/two outpatient records during one year for either anxiety, depression, schizophrenia, bipolar, personality or stress disorder) and stimulant use disorder were less likely to receive opioid agonist treatment post-release (AOR 0.73, 95%CI 0.64–0.84) [41].
Cancer screening
One included study investigated cancer screening after release from prison [38]. The cohort study reported lower levels of colorectal and breast cancer screening among people released from custody compared to the general population [38]. The study found that people released from custody were more likely to be overdue screening for colorectal (ARR 1.44, 95%CI 1.42–1.46) and breast cancer (ARR 1.99, 95%CI 1.83–2.17) compared with the general population, and more likely to still be overdue screening three years later [38].
Cost saving of primary care program
One included study investigated costs of a primary care program for people recently released from prison [33]. The propensity matched study evaluated the Transitions Clinic Network (TCN) programme, a comparison of existing community health centre and enhanced primary care, for people released from custody with a chronic health condition or > 50 years [33]. The study suggested that the enhanced primary care program reduced criminal justice system costs, with an estimated a 12-month return of $2.55 to the state for every invested dollar [33].
Where are the knowledge gaps in this area?
The review suggests knowledge gaps in this area relate to the location of studies. The included study locations were Canada, Australia, USA and The Netherlands. There were no studies from the United Kingdom, or Europe or low and middle income (LMIC) countries. More research is needed from other countries to make findings more generalisable. This review focused on primary care use and the search strategy incorporated terms around general practice, family practice, in addition to other community care for example, nurse practitioners, community pharmacy services, community dentistry and optometrists. Few studies were performed on the provision of care outside of general practice. Additional studies examining access to different healthcare services in the community among people after release from prison would give a clearer idea of challenges during transition from prison to community care. Table 5 describes the recommendations for further research in this area. Since most studies have been published in recent years, it was decided a posteriori to map the recommendations for future research (this was not a direct research question in this scoping review, and therefore was not part of the charting process of the included studies).
Discussion
This scoping review identified and collated the most recent evidence from data-linkage studies about primary care use after release from prison; and mapped the evidence from the included studies by methodology, key findings and gaps in research. Evidence in this research area is growing with most of the included studies published since 2019. Included studies were conducted across four countries, and most used cohort designs to investigate primary care visits (for example, use, time to first contact and quality of care). The reporting of the descriptive characteristics of each sample varied across the included studies. Reporting and analysing socio-demographics in this study population is important to help identify patient groups who are engaging (or not) with primary care. For example, approximately half of the included studies reported age, most (n = 14/17) reported race/ethnicity, but all reported gender/sex (Appendix 4). In the included studies, most data sources were linked was by unique identifiers. The study period after release from prison varied between the included studies, however the most common time periods examined were one- or two-years follow-up. Although most studies did consider methods to address re-incarceration, different approaches were used for example, excluding time spent in prison during re-incarceration from follow-up, censoring follow-up at re-incarceration, using re-incarceration as a study outcome, measuring the study exposure at each release from prison and using truncation for re-incarceration(s) during the follow-up period. Re-incarceration has potential methodological issues for the study of primary care use i.e. by varying the access an individual has to primary health care services in the community. Furthermore, health-related factors have been identified as risk factors for re-incarceration in analyses adjusting for demographic and criminal justice factors [45]. Therefore, the differences in methods used to address re-incarceration may pose important consequences on the reported outcomes. Few included studies reported using a checklist or technique which allows transparency in methodological and reporting quality. With an apparent lack of use of reporting guidelines in this area, more rigorous documentation would help improve future evidence synthesis and is recommended.
There is mixed evidence regarding levels of primary care use for people after prison release (compared to the general population), for example, with variations reported among studies such as higher and lower use [12, 13, 31]. The review found higher primary care use among specific patient groups after release from prison, for example, history of risky opiate use, diagnosis of a mental health condition or medication in prison [31], individuals living with HIV [35] and people with schizophrenia [37]. Females who have been incarcerated had higher morbidity and specific psychiatric conditions compared with males released from prison and females in the general population, and higher rates of primary care use after release from prison [39]. Therefore, suggesting that high primary care attendance relates to a greater demand for health care within patient groups. The suggested higher rates of contact may allow health professionals to identify other health risks or opportunities for health promotion in this marginalised group. A positive finding from this review indicated good connectivity in that contact with primary care services early after release from prison increased health service use, generally [44]. However, there is evidence of low numbers of people accessing primary care during the first month post-release (e.g. one study reported that in the first month after release, around two-thirds of women and three-quarters of men did not access primary care) [13]. Timely access to primary care also includes medication dispensed after release from prison, for example, a study suggested that approximately one-quarter of individuals with an opioid use disorder received opioid agonist treatment dispensation within two days of release from prison [41].
Multimorbidity (two or more chronic conditions) is one of the major challenges facing developed health care systems; with risk factors including increasing age, lower socioeconomic status, living in more deprived areas and health behaviour (such as alcohol use, smoking and low physical activity) [46, 47]. There is a high prevalence of multimorbidity among prison population [30]. There was increased primary care contact for people with moderate or complex multimorbidity in the two years after release from prison compared to having no multimorbidity, and the quality of care was found to be largely inadequate for moderate multimorbidity, but adequate in people with complex multimorbidity [30]. Understanding patterns in multimorbidity in people leaving prison and health disparities, may help address issues in quality of care. There were lower levels of colorectal and breast cancer screening among people released from custody compared to the general population [38]. This finding would suggest suboptimal care for people in prison in regard to screening and potentially missed opportunities for the early detection of cancer and the provision of services for this vulnerable population. Some benefits from enhanced primary care programmes after release from prison were reported, for example, a reduction in reincarceration [43] and criminal justice system costs [33] and research into improving the transition from health care prison to the community is an important step to improving outcomes. The studies included in this review compared enhanced primary care via the Transitions Clinic Network (TCN) programme to individuals not exposed to the programme [33, 43]. The TCN programme facilitates primary care clinics to increase health care services access, improve health status, and lower reincarceration rates among people recently released from prison with chronic health condition(s) or are over 50 years old [18, 33]. The enhanced primary care model in the TCN consists of specialist community health workers with a history of incarceration (i.e. having lived in prison and had their own post-release experiences) as part of a primary care team addressing the needs of people during the transition from prison to community living [33, 43]. The TCN programme provides care for health conditions, including substance use disorders and mental health conditions, and addresses social determinants of health such as housing, food access and employment after release from prison [33, 43]. Patient navigation has been investigated in the general population and among people release from prison. For example, a scoping review of all patients without a regular source of primary care (provider/practice), i.e. general population, included 20 studies (published between 2000 and 2016) and found that patient navigators, i.e. a person/process facilitating a linkage between an individual requiring primary care and a primary healthcare provider, may improve access to primary care and patient-centred care across different healthcare settings [48]. A separate scoping review of interventions connecting individuals to substance use services after release from jail (including 14 studies; published between 2001 and 2021), found that four of the included studies used peer or patient navigation as the core intervention component [49].
Study strengths and limitations
This scoping review has several strengths. To our knowledge, this is the first review of record linkage studies about primary care utilisation after release from prison. The methods used follow the framework provided by Arksey and O’Malley and guidance by the Joanna Briggs Institute (JBI) [15, 16]. Other than additions to the data charting form, there have been no changes to the methods published in the study protocol [14]. This scoping review focused on data-linkage studies within the broader topic of primary care use after prison release, therefore findings specifically relate studies using linked data sources, and the results may be used to guide future research in this area. This scoping review has some limitations. The search strategy in this review used terms relating to ‘former’ incarceration to increase specificity, however, this may have reduced sensitivity and some publications may have been missed. Similarly, the search strategy used terms for general/family practice and other community healthcare services such as pharmacy, dentistry and optometry. It is possible that some studies may have been missed given the range of terms used across countries to describe primary care and related services. For example, a study by Sutherland et al. 2015 [50] was not included in our 1,050 publications screened by title and abstract in step 1 (i.e. publications identified by our search strategy) (Kinner, personal communication). The study (based in Australia) included 251 women (18–49 years) and used in prison baseline survey data (2008–2010) and prison medical records, linked to Pharmaceutical Benefits Scheme (PBS) claims data after release from prison (probabilistic linkage) [50]. The study reported dispensing of contraceptive medications within 30, 90 and 180 days of release from prison [50]. The study reported that contraceptive medication had been dispensed to 5 women (2%) at 30 days after release from prison; 9 women (4%) at 90 days after release, and 19 women (7.6%) by 180 days after release [50]. The specific health needs of women after release from prison highlights an important area for both research and policy for the provision of reproductive health in prison and after release. A search of publications by key authors in the field (as part of the search strategy) may have identified additional publications, however this is not a normal part of the scoping review process. The review did not include a search of the grey literature and was limited to publications available in English due to resources. Finally, the included studies were conducted in Canada, Australia, USA and The Netherlands, therefore impacting the generalisability of the review findings.
Future research
The United Nation’s 2030 Agenda for Sustainable Development set goals and actions for people, planet and prosperity between 2015 and 2030 [51]. Although the health of the prison population is not reflected in the Sustainable Development Goal (SDGs) 2030, it has been advocated that improving the health of people in prison may directly/indirectly contribute to 15 of the total 17 SDGs [52]. The World Health Organisation defines that primary health care should be people centred, supporting needs such as health promotion, disease prevention, treatment, rehabilitation and palliative care [53]. More research is needed to examine whether all aspects of primary health care are being met after release from prison. Since most studies included in this review have been published in recent years, the recommendations for future research suggested by each paper have been summarised. This offers an opportunity to address the gaps in knowledge. In summary, the included studies suggested further research on health during all stages of an individual’s prison journey (including determining reasons for healthcare attendance and studies/interventions for specific conditions). More research is needed on the continuity of care, across all health and social service systems, and health outcomes after release from prison, and there is a need to address health promotion in the prison population, for example population cancer screening programs. Further work to understand the sharing of information between health care settings in the prison and community and methods around discharge planning could help identify challenges/solutions regarding the timeliness of primary care access. More work is required around primary care programmes after release from prison, e.g. engagement with community health workers and the long-term costs and benefits of primary care programs. The involvement of people with a lived experience of incarceration in research, including qualitative work, would provide better insight into the quality of life and well-being of individuals after release from prison. Finally, more studies are required across different countries to allow generalisability of findings.
Epidemiological population-based studies linking incarceration records and health care data can improve understanding around patterns of health care use, patient pathways such as people most at risk of not engaging with community care, facilitators/difficulties in accessing services, and health-related and other outcomes, to help profile people after release from prison. There is a need for research about aspects of pre-release healthcare management, for example, how to improve communication between prison and community healthcare providers and services in a transparent and accountable way that would facilitate early contact and the delivery of support after release; and to tap into the potential to implement innovative processes that would improve the transition of care for patient groups. The variant of the National Health Service (NHS) in each United Kingdom devolved nation is responsible for the organisation, provision and delivery of healthcare services (and in the case of Northern Ireland, for health and social services in Northern Ireland) for people in prison and in the community; and this arrangement presents an opportunity to understand and improve the connectedness of patient pathways from prison to community care services. Evidence synthesis of interventions to improve the health of people during incarceration and the first year after release has been reported. For example, a systematic review of randomised controlled trials included 95 studies [focused on substance abuse (N = 35), mental health (n = 28), infectious diseases (n = 18), health service use (n = 12) and chronic diseases (n = 2)] [54]. In most of the studies, the intervention was implemented during incarceration and the outcome was measured in the community after release [54]. Of the included interventions, 59 reported improved outcomes, and in 42 intervention studies outcomes were measured in the community after release [54]. Furthermore, linking data to interventions can be a strategy for loss to follow-up of marginalised populations, for example, by testing for selective biased attrition in trials and using record-linkage to administrative data for determining biased attrition [25].
Conclusions
This scoping review identified evidence from data-linkage studies about primary care use after release from prison. Most studies included in this scoping review were published in recent years and are largely cohort study designs. The review suggested mixed evidence regarding levels of primary care use for people after prison release and has highlighted major challenges and areas of suboptimal care. Recommendations for further research have been discussed.
Data availability
Availability of data and materialsNot applicable. A data charting form used for data extracted from the full texts publications has been provided as supplementary material (Appendix 3).
References
Fair and Walmsley. World prison population list, thirteenth edition. World Prison Brief. Institute for Criminal Policy Research; 2021.
United Nations. United Nations system common position on incarceration; 2021.
Patel K, Boutwell A, Brockmann BW, Rich JD. Integrating correctional and community health care for formerly incarcerated people who are eligible for medicaid. Health Aff (Millwood). 2014;33(3):468–73. https://doi.org/10.1377/hlthaff.2013.1164. PMID: 24590947; PMCID: PMC4028698.
McLeod KE, Butler A, Young JT, Southalan L, Borschmann R, Sturup-Toft S, Dirkzwager A, Dolan K, Acheampong LK, Topp SM, Martin RE, Kinner SA. Global prison health care governance and health equity: a critical lack of evidence. Am J Public Health. 2020;110(3):303–8. Epub 2020 Jan 16. PMID: 31944844; PMCID: PMC7002953.
Groenewegen P, Dirkzwager A, van Dam A, Massalimova D, Sirdifield C, Smith L, EFPC working group on Prison Health. The health of detainees and the role of primary care: position paper of the European Forum for Primary Care. Prim Health Care Res Dev. 2022;23:e29. PMID: 35574709; PMCID: PMC9112672.
Hu C, Jurgutis J, Edwards D, O’Shea T, Regenstreif L, Bodkin C, Amster E, Kouyoumdjian FG. When you first walk out the gates… where do [you] go? Barriers and opportunities to achieving continuity of health care at the time of release from a provincial jail in Ontario. PLoS ONE. 2020;15(4):e0231211. https://doi.org/10.1371/journal.pone.0231211. PMID: 32275680; PMCID: PMC7147766.
Merrall ELC, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105:1545–54.
Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 2012;102:e67–75.
Kinner SA, Forsyth S, Williams G. Systematic review of record linkage studies of mortality in ex-prisoners: why (good) methods matter. Addiction. 2013;108:38–49.
Cooper JA, Onyeka I, Cardwell C, Paterson E, Kirk R, O’Reilly D, Donnelly M. Record linkage studies of drug-related deaths among adults who were released from prison to the community: a scoping review. BMC Public Health. 2023;23(1):826. https://doi.org/10.1186/s12889-023-15673-0.
Tuinema J, Orkin AM, Cheng SY, Fung K, Kouyoumdjian FG. Emergency department use in people who experience imprisonment in Ontario, Canada. CJEM. 2020;22(2):232–240. https://doi.org/10.1017/cem.2019.401. PMID: 31526408.
Kouyoumdjian F, Kim M, Kiran T, Cheng S, Fung K, Orkin A, Kendall CE, Green S, Matheson FI, Kiefer L. Attachment to primary care and team-based primary care: retrospective cohort study of people who experienced imprisonment in Ontario. Can Fam Physician. 2019;65(10):e433–42. PMID: 31604754; PMCID: PMC6788664.
Kouyoumdjian FG, Cheng SY, Fung K, Humphreys-Mahaffey S, Orkin AM, Kendall C, Kiefer L, Matheson FI, Green SE, Hwang SW. Primary care utilization in people who experience imprisonment in Ontario, Canada: a retrospective cohort study. BMC Health Serv Res. 2018;18(1):845.
Cooper JA, Murphy S, Kirk R, O’Reilly D, Donnelly M. Record linkage studies of primary care utilisation after release from prison: a scoping review protocol. PLoS ONE. 2023;18(8):e0289218. https://doi.org/10.1371/journal.pone.0289218. PMID: 37624760; PMCID: PMC10456167.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis, JBI 2020.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Shavit S, Aminawung JA, Birnbaum N, Greenberg S, Berthold T, Fishman A, Busch SH, Wang EA. Transitions clinic network: challenges and lessons in primary care for people released from prison. Health Aff (Millwood). 2017;36(6):1006–1015. https://doi.org/10.1377/hlthaff.2017.0089. PMID: 28583958.
Spaulding AC, Messina LC, Kim BI, Chung KW, Lincoln T, Teixeira P, Avery AK, Cunningham M, Stein MS, Ahuja D, Flanigan TP. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013;17(Suppl 2):S203–211.
Walsh KB, Will J, Chyten-Brennan J. Community health care utilization patterns in transgender individuals who have been incarcerated. J Correctional Health Care. 2023;29(1):81–90.
Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, Simon-Levine D, Teixeira PA, Cruzado-Quinones J, Kling RN, Frew PM, Spaulding AC. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release.AIDS &. Behavior. 2013;17(Suppl 2):S128–136.
Wang EA, McGinnis KA, Long JB, Akgun KM, Edelman EJ, Rimland D, Wang KH, Justice AC, Fiellin DA. Incarceration and health outcomes in HIV-infected patients: the impact of substance use, primary care engagement, and antiretroviral adherence. Am J Addictions. 2015;24(2):178–84.
Williams CT, Kim S, Meyer J, Spaulding A, Teixeira P, Avery A, Moore K, Altice F, Murphy-Swallow D, Simon D, Wickersham J, Ouellet LJ. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav. 2013;17(Suppl 2):S195–202.
Snow KJ, Petrie D, Young JT, Preen DB, Heffernan E, Kinner SA. Impact of dual diagnosis on healthcare and criminal justice costs after release from Queensland prisons: a prospective cohort study. Aust J Prim Health. 2022;28(3):264–70.
Kinner SA, Lennox N, Williams GM, Carroll M, Quinn B, Boyle FM, Alati R. Randomised controlled trial of a service brokerage intervention for ex-prisoners in Australia. Contemp Clin Trials. 2013;36(1):198–206. Epub 2013 Jul 10. PMID: 23850859.
Kouyoumdjian FG, McConnon A, Herrington ERS, Fung K, Lofters A, Hwang SW. Cervical cancer screening access for women who experience imprisonment in Ontario, Canada. JAMA Netw Open. 2018;1(8):e185637. https://doi.org/10.1001/jamanetworkopen.2018.5637.
Lim S, Nash D, Hollod L, Harris TG, Lennon MC, Thorpe LE. Influence of jail incarceration and homelessness patterns on engagement in HIV care and HIV viral suppression among New York city adults living with HIV/AIDS. PLoS ONE. 2015;10(11):e0141912. https://doi.org/10.1371/journal.pone.0141912. PMID: 26599877; PMCID: PMC4657891.
MacKenzie O, Goldman J, Chin M, Duffy B, Martino S, Ramsey S, Jiménez MC, Vanjani R. Association of individual and familial history of correctional control with health outcomes of patients in a primary care center. JAMA Netw Open. 2021;4(11):e2133384. https://doi.org/10.1001/jamanetworkopen.2021.33384. PMID: 34748006; PMCID: PMC8576582.
Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS Behav. 2013;17(8):2644-53. https://doi.org/10.1007/s10461-011-0057-1. PMID: 21983697.
Calais-Ferreira L, Butler A, Dent S, Preen DB, Young JT, Kinner SA. Multimorbidity and quality of primary care after release from prison: a prospective data-linkage cohort study. BMC Health Serv Res. 2022;22(1):876.
Carroll M, Spittal MJ, Kemp-Casey AR, Lennox NG, Preen DB, Sutherland G, Kinner SA. High rates of general practice attendance by former prisoners: a prospective cohort study. Med J Aust. 2017;207(2):75–80.
Dirkzwager AJE, Verheij R, Nieuwbeerta P, Groenewegen P. (2021). Mental and physical health problems before and after detention: a matched cohort study. Lancet Reg Health-Europe 8.
Harvey TD, Busch SH, Lin HJ, Aminawung JA, Puglisi L, Shavit S, Wang EA. Cost savings of a primary care program for individuals recently released from prison: a propensity-matched study. BMC Health Serv Res. 2022;22(1):585.
Howell BA, Long JB, Edelman EJ, McGinnis KA, Rimland D, Fiellin DA, Justice AC, Wang EA. Incarceration history and uncontrolled blood pressure in a multi-site cohort. J Gen Intern Med. 2016;31(12):1496–502.
Khanna S, Leah J, Fung K, Antoniou T, Kouyoumdjian F. Health care utilization by people with HIV on release from provincial prison in Ontario, Canada in 2010: a retrospective cohort study. AIDS Care. 2019;31(7):785–92.
Kouyoumdjian FG, Lee JY, Orkin AM, Cheng SY, Fung K, O’Shea T, Guyatt G. (2020). Thirty-day readmission after medical-surgical hospitalization for people who experience imprisonment in Ontario, Canada: a retrospective cohort study. PLoS ONE 15(1).
Mahentharan M, Kouyoumdjian FG, de Oliveira C, Iwajomo T, Simpson AIF, Jones R, Kurdyak P. Prevalence and predictors of Reincarceration after Correctional Center Release: a Population-based comparison of individuals with and without Schizophrenia in Ontario, Canada:Prevalence et predicteurs de la reincarceration apres la liberation d’un centre correctionnel: une comparaison dans la population-de personnes souffrant ou non de schizophrenie en Ontario. Can Can J Psychiatry - Revue Canadienne De Psychiatrie. 2021;66(4):376–84.
McConnon A, Fung K, Lofters A, Hwang SW, Kouyoumdjian FG. Colorectal and breast Cancer screening status for people in Ontario provincial correctional facilities. Am J Prev Med. 2019;56(4):487–93.
Norris E, Kim M, Osei B, Fung K, Kouyoumdjian FG. Health Status of females who experience incarceration: a Population-based Retrospective Cohort Study. J Women’s Health. 2021;30(8):1107–15.
Palis H, Hu K, Rioux W, Korchinski M, Young P, Greiner L, Nicholls T, Slaunwhite A. Association of Mental Health Services Access and Reincarceration among adults released from prison in British Columbia. Can JAMA Netw Open. 2022;5(12):e2247146.
Palis H, Zhao B, Young P, Korchinski M, Greiner L, Nicholls T, Slaunwhite A. Stimulant use disorder diagnosis and opioid agonist treatment dispensation following release from prison: a cohort study. Subst Abuse Treat Prev Policy. 2022;17(1):77.
Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102(9):e22–29.
Wang EA, Lin HJ, Aminawung JA, Busch SH, Gallagher C, Maurer K, Puglisi L, Shavit S, Frisman L. Propensity-matched study of enhanced primary care on contact with the criminal justice system among individuals recently released from prison to New Haven. BMJ Open. 2019;9(5):e028097.
Young JT, Arnold-Reed D, Preen D, Bulsara M, Lennox N, Kinner SA. Early primary care physician contact and health service utilisation in a large sample of recently released ex-prisoners in Australia: prospective cohort study. BMJ Open. 2015;5(6):e008021.
Thomas EG, Spittal MJ, Taxman FS, et al. Health-related factors predict return to custody in a large cohort of ex-prisoners: new approaches to predicting re-incarceration. Health Justice. 2015;3:10. https://doi.org/10.1186/s40352-015-0022-6.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. https://doi.org/10.1016/S0140-6736(12)60240-2. Epub 2012 May 10. PMID: 22579043.
Cezard G, McHale CT, Sullivan F, et al. Studying trajectories of multimorbidity: a systematic scoping review of longitudinal approaches and evidence. BMJ Open. 2021;11:e048485. https://doi.org/10.1136/bmjopen-2020-048485.
Peart A, Lewis V, Brown T, Russell G. Patient navigators facilitating access to primary care: a scoping review. BMJ Open. 2018;8:e019252. https://doi.org/10.1136/bmjopen-2017-019252.
Grella CE, Ostlie E, Watson DP, Scott CK, Carnevale J, Dennis ML. Scoping review of interventions to link individuals to substance use services at discharge from jail. J Subst Abuse Treat. 2022;138:108718. https://doi.org/10.1016/j.jsat.2021.108718.
Sutherland G, Carroll M, Lennox N, Kinner S. Prescribed contraceptives among woman after release from prison. Health Justice. 2015;3:8. https://doi.org/10.1186/s40352-015-0019-1.
United Nations. Transforming our world: the 2030 agenda for sustainable development. A/res/70/1. 2015.
Ismail N, Lazaris A, O’Moore É, Plugge E, Stürup-Toft S. Leaving no one behind in prison: improving the health of people in prison as a key contributor to meeting the sustainable development goals 2030. BMJ Global Health. 2021;6:e004252.
WHO. 2023. World Health Organisation. Home/Health topics/Primary health care. https://www.who.int/health-topics/primary-health-care#tab=tab_1. Accessed on 19.10.2023.
Kouyoumdjian FG, McIsaac KE, Liauw J, Green S, Karachiwalla F, Siu W, Burkholder K, Binswanger I, Kiefer L, Kinner SA, Korchinski M, Matheson FI, Young P, Hwang SW. A systematic review of randomized controlled trials of interventions to improve the health of persons during imprisonment and in the year after release. Am J Public Health. 2015;105(4):e13–33. https://doi.org/10.2105/AJPH.2014.302498. Epub 2015 Feb 25.
Acknowledgements
The authors would like to thank Richard Fallis, Subject Librarian, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, for reviewing the search strategy and providing guidance on the use of reference management software. The authors would like to acknowledge Professor Dermot O’Reilly’s significant role in the development of a research programme on prison and health in Northern Ireland. Dermot died in October 2023. He was a dear friend and the Director of the Administrative Data Research Centre Northern Ireland (ADRC NI) since 2014. He will be missed; his work on health inequalities will continue in his memory.
Funding
This work is funded by a grant awarded to the ADRC NI by the Economic and Social Research Council (ESRC) (grant number ES/W010240/1).
Author information
Authors and Affiliations
Contributions
Authors’ contributionsJAC, RK, DO’R, and MD conceived the scoping review idea. JAC and MD developed the scoping review questions and methods. JAC and SM piloted the data charting form as part of the study protocol. JAC performed the searches on the literature databases. JAC and SM screened all publication titles and abstracts independently. Subsequently, JAC and SM independently screened full publications and any discrepancies were resolved via discussion between JAC and MD. Before stage 4 of the review, the charting form was retested by JAC and SM. Subsequently, JAC and SM extracted information from all included publications independently. JAC and MD discussed the findings of included studies. JAC drafted the manuscript and MD and SM edited drafts of the manuscript. All co-authors (with the exception of DO’R (for reasons outlined in the acknowledgements) reviewed the manuscript and have given final approval for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cooper, J.A., Murphy, S., Kirk, R. et al. Data linkage studies of primary care utilisation after release from prison: a scoping review. BMC Prim. Care 25, 287 (2024). https://doi.org/10.1186/s12875-024-02527-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02527-w