Abstract
Background
The purpose of this study was to quantify how much of the burden of visual impairment (VI) and unmet need in Talagang, identified by Rapid Assessment of Avoidable Blindness (RAAB) survey data, has been addressed by Community Eye Health (CEH) programme efforts.
Methods
A RAAB survey was carried out in November 2018, with 2,824 participants in Talagang Tehsil, Punjab, Pakistan, aged 50 and over. Census data were used to extrapolate survey data to the population. Alongside this, a CEH programme was launched, consisting of community eye screening, and onward referral to rural health centres, secondary or tertiary ophthalmological services, as required. This health intervention aimed to address the eye care needs surfaced by the initial survey. From 2018 to 2022, 30,383 people aged 50 or over were screened; 14,054 needed referral to further steps of the treatment pathway and more detailed data collection. Programme data were compared to estimates of population unmet needs. Main outcome measures were prevalence of VI, and proportion of need met by CEH Programme, by cause and level of VI.
Results
Among those aged 50 and over, 51.0% had VI in at least one eye. The leading causes were cataract (46.2%) and uncorrected refractive error (URE) (25.0%). In its first four years, the programme reached an estimated 18.3% of the unmet need from cataract, and 21.1% of URE, equally in both men and women.
Conclusions
Robustly collected survey and programme data can improve eye health planning, monitoring and evaluation, address inequities, and quantify the resources required for improving eye health. This study quantifies the time required to reach eye health needs at the community level.
Similar content being viewed by others
Background
Globally, in 2020, it was estimated that 43.3 million people were blind (presenting visual acuity, VA, worse than 3/60 in the better eye), with nearly half of these cases due to cataract (17.0 million) or uncorrected refractive error (URE, 3.7 million) [1]. Cataract and URE combined are also responsible for 241.2 million of the 295.1 million people with moderate-severe visual impairment (VI). In addition, at least 509.7 million people are estimated to have near vision impairment due to uncorrected presbyopia. Cataract surgery and refractive correction are relatively simple interventions which could restore good vision to those affected. Provision of these services can be monitored via indicators including prevalence of VI, effective cataract surgical coverage (eCSC) and effective refractive error coverage (eREC) [2]. eCSC and eREC have been recommended by a WHO-led expert panel for assessment of eye care provision and Universal Health Coverage [3]. Standardised reporting allows consistent situational assessment, service planning, and comparison of groups and regions.
Relevant data is collected within the Global Vision Database/Vision Atlas [4], a key source of which is Rapid Assessment of Avoidable Blindness (RAAB) surveys [5, 6]. RAAB surveys assess prevalence and causes of VI in people aged 50 and over, as well as estimating cataract surgical coverage and identifying barriers to cataract treatment, and have been undertaken in over 80 countries. The over 50s age group is prioritised for screening when targeting those with cataract and vision impairment, as approximately 73% of blindness and visual impairment cases are in this group, with cataract being the leading cause [7].
Sequential RAAB surveys have been used to analyse service provision [8], and RAAB data has elsewhere been combined with Ministry of Health data regarding surgeries performed to allow review of eCSC [9].
Community-based eye care programmes can improve access to eye care, especially among low-income and rural patient groups [10]. Community eye health (CEH) programmes have been carried out in Pakistan with Peek Vision, who have previously demonstrated the use of appropriate data management and iterative programme change to allow for continuous programme improvement, including improved adherence to referral [11]. Comparison of data collected during these large-scale vision programmes and by RAAB surveys allows identification of groups which have been successfully reached by the programme, or missed, as well as projection of how much programme activity would be required to eradicate avoidable blindness and visual impairment in the region. Here we compare RAAB survey data from Talagang, Pakistan, with CEH programme data, to assess programme reach.
Methods
Visual impairment definitions
VI was defined as follows: early/mild: distance visual acuity (DVA) worse than 20/40 (6/12) but equal to or better than 20/60 (6/18); moderate VI: <20/60 (6/18), ≥ 20/200 (6/60); severe VI: <20/200 (6/60), ≥ 20/400 (3/60); and blindness: <20/400 (3/60), as per WHO/ICD-11 definitions. Moderate-severe VI (MSVI) therefore describes VA < 20/60 (6/18), ≥ 20/400 (3/60). As VA was measured monocularly, VI was assessed on a per-eye level, i.e. proportion of eyes with VI, and on a person level, based on VA in the better eye.
RAAB survey
During November and December 2018, a RAAB survey was carried out in the Talagang Tehsil, Chakwal District, Punjab, Pakistan. As per standard RAAB methodology, clusters were randomly and systematically identified, and then 50 people aged 50 or over were selected from within each cluster via compact segment sampling. This led to an initial sample of 2,889 people. Data were collected via door-to-door fieldwork at participants’ homes. Assessment included VA measurement via Tumbling E chart, and examination with torch and direct ophthalmoscope. Pinhole vision testing and ophthalmologist examination were carried out for those with VA < 6/12. Dilated examination was carried out in those for whom a cause of visual impairment could not be found on undilated examination. This allowed estimation of prevalence of blindness and VI, and causes. Data included refractive error and presbyopia prevalence, spectacle wear coverage, as well as cataract surgical coverage (CSC), place of surgery, and barriers to cataract surgery.
CEH programme
Alongside the RAAB survey, a CEH programme was launched in November 2018 in the same area, with collaboration between College of Ophthalmology and Allied Vision Sciences (COAVS), Peek Vision, and Christian Blind Mission (CBM). Communities were first sensitised by social organisers and Lady Health Visitors. Community eye screening was then carried out in Basic Health Units. Where indicated, screening participants were referred to rural health centres for refraction and provision of primary eye care. People with conditions requiring ophthalmological input were referred onwards to secondary or tertiary ophthalmological services. Hospitals were informed of referrals, and patients were sent automated text or voice messages reminding them of their appointments. The Peek software system was used to track this data, including the number of people screened, the screening quality, number of people referred, treated and non-attenders/left-behind groups. This allowed continuous improvement of the programme to improve uptake with a focus on equity and efficient use of the available resources. A more detailed summary of the programme has previously been described elsewhere [11].
Census data
Since the RAAB and CEH programmes were carried out, 2017 census data [12] has been made available regarding the Talagang population. This has been used in this analysis for extrapolation to regional magnitude of visual impairment and blindness.
Data security
The storage and transmission of this data was carried out in line with a Data Protection Agreement with the local stakeholders, and followed the European Union General Data Protection Regulation (GDPR).
Data analysis
RAAB7 software and Peek Capture smartphone application were used to collect data for the survey and community programmes respectively. Data from RAAB survey automated reports were obtained from the RAAB repository with permission of the PI of the project (COAVS, Lahore). Population age and gender composition of people living in Talagang Tehsil were obtained from 2017 census data and used to extrapolate RAAB sample results to the population who live in the survey area. Anonymised programme data and RAAB data were processed using Stata 14.0 (StataCorp, Texas, US), R studio (R Studio, Massachusetts, US) and Google Sheets (Google, California, US). R Shiny software (R Studio, Massachusetts, US) was used for further data management and figure creation.
Results
Magnitude of visual impairment: RAAB Survey
Of 2,889 people who were invited to participate, 2,824 (response rate = 97.8%) participated in the RAAB survey. A summary of the results of the survey is presented in Fig. 1.
Summary of RAAB data. (a) Prevalence of bilateral blindness - best corrected visual acuity (BCVA) < 3/60 in better eye by age and gender. (b) Causes of blindness and severe or moderate visual impairment in the better eye (BCVA < 20/60 (6/18)). (c) Barriers to cataract surgery in people with bilateral BCVA < 6/60 due to cataract, by gender. (d) Outcomes of cataract surgery: BCVA in operated eyes. Very good: BCVA ≥ 6/12, Good: 6/12 > BCVA ≥ 6/18, Borderline: 6/18 > BCVA ≥ 6/60, Poor: BCVA < 6/60
The sample prevalences of blindness, severe VI, moderate VI and early VI were 2.4% (95% CI: 1.6–3.3), 1.1% (95% CI: 0.7–1.5), 14.3% (95% CI:12.2–16.4), and 18.9% (95% CI: 15.3–22.5) respectively. In general, 42.8% of examined eyes (95% CI:39.6–46.0) and 36.7% of people (95% CI: 33.9–39.6), based on VA in the better eye, had any VI or blindness i.e. VA < 20/40 (6/12) with available correction.
Causes of blindness were avoidable in 97.6% of patients; the most common causes of blindness and visual impairment were: untreated cataract, uncorrected refractive errors, diabetic retinopathy, glaucoma, posterior segment pathology and corneal opacities. In participants with untreated cataract, the main barriers to uptake of cataract surgery were fear (55.6%) and cost (38.9%). In those who had had cataract surgery, the outcome was good (18.4%) or very good (62.8%) in 81.3% of cases.
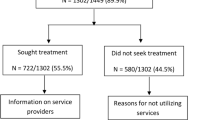
Implemented CEH programme
In Talagang, in the Community Eye Health (CEH) and School Eye Health programmes combined, between 2018 and 2022: 420,147 people were screened; 65,874 referred on to triage for further assessment; 31,454 people were prescribed spectacles, and 3,482 attended hospital services. Figure 2 shows an overview of the programme participants aged 50 or over, seen during the first four years of the Community Eye Health programme.
The eye health need surfaced by the RAAB survey and the amount of need that has been reached by the programme are compared in Table 1. Extrapolation of RAAB data estimates that 54.5% (39,233/71,950) of the 50 + population in Talagang had VI in at least one eye. 41.8% (30,090/71,950) of people had VI in their better seeing eye.
As shown in Table 1, there were an estimated 39,233 people who had any VI or blindness in at least one eye at the beginning of the programme. The RAAB survey and CEH programme combined screened 9,178 (1,381 + 7,797) of those people (23.4%) during the first four years. Figure 3 shows the proportion of VI which was reached by the programme, by visual acuity status. In most groups, the proportion of reach was between 20 and 26%, while the programme reached over a third of people with bilateral severe VI.
Figure 4 visualises the causes of blindness identified by RAAB survey and the distribution of eye conditions among the 513 blind people who were reached by programme. As shown in this figure, untreated cataract was the leading cause of blindness in 55% of cases in the survey and 61% of cases in the programme. URE was the second most common cause of VI (25.0%) but not a major cause of blindness.
As shown in Fig. 4, while cataract was the leading cause of blindness in both settings, the distribution of other causes differed between the programme and RAAB survey. The proportion of VI secondary to cataract or URE met by the programme is shown in Fig. 5: approximately 18.3% of cataract surgical need and 21.1% of need for refractive services in this area have been reached during the first 4 years of the programme (average 5% per year).
Discussion
South Asia has both the highest age-standardised prevalence of moderate-severe VI of any Global Burden of Disease region, and the largest absolute number of cases [1]. Effective refractive error coverage (eREC) describes the proportion of people with vision impairing refractive error or presbyopia, whose need has been sufficiently met, i.e. with refractive correction (spectacles or contact lenses) that resolves their vision impairment. There is vast global inequity in eREC, with 79.1% distance eREC in high-income countries, but only 9.0% in South Asia and 5.7% in Sub-Saharan Africa [6]. Despite South Asia bearing such a large proportion of VI need, it is underrepresented in research into eye health service improvement: for example, in a recent global scoping review, it was found that the majority of research into interventions to improve cataract services has been undertaken in high-income countries, with only 6.3% in South Asia (n = 9/143) [13]. Encouragingly, there has been significant improvement of eREC in the region over the last two decades [6].
Robustly collected survey data can be used to improve CEH programmes at all stages of the programme. Surveys carried out prior to programme initiation allow for better understanding of which conditions are likely to be seen in a region, and their magnitude. In this way, RAAB surveys can be used to help plan service provision [14, 15]. Comparison of repeated eye health surveys (undertaken before and after CEH programme interventions) has enabled assessment of the effectiveness of the programmes carried out in the intervening period, for example in Nigeria [16] and India [17].
We presented an evidence-based and comparable estimation of the magnitude of eye care needs and causes of vision impairment in a district level population, applying RAAB methodology. This allowed the CEH programme to establish a defined baseline against which to measure its progress towards eradicating avoidable blindness. After introduction of RAAB methodology in 2006, over 300 RAAB studies have been completed in low- and middle-income countries. Previous studies have assessed sequential RAABs alongside health systems/workforce programme data [16], and compared RAAB results with historical cataract surgical rate (CSR) programme data [18]. However, to the best of our knowledge, this is the first study that compares baseline RAAB data with subsequent programme reach to demonstrate the need met by an eye health programme in a defined population, and that which still needs to be reached.
Based on initial RAAB data, this programme reached almost 20% of previously unmet need due to the main causes of visual impairment, equally in both men and women. Regional variation is large; a previously published RAAB in Pakistan, carried out in Lahore, found VI prevalence to be remarkably low in the area: 1.9%, with a CSC of 84.0%[19]. However, even with such good service coverage, there was significant inequity between genders, with CSC of 94.1% for men, and 72.1% for women. Here, VI prevalence was found to be much higher in Talagang. The proportion of cataract and URE need reached by this programme was equitable between men and women, as shown in Fig. 5b.
Census data is usually required for extrapolation from survey results to national or regional magnitude. In this case, Pakistan’s census had been delayed, such that at the initial time of RAAB survey, the most recent formal national census with available data was from 1998. As the 2017 census data are now available, the estimated need is higher than it was initially. This reduces the estimated proportion of need which has been met by the programme, though they remain encouraging at 18.3% of cataract and 21.1% of URE (see Fig. 5).
Since the time of data extraction and analysis, more people may have attended hospital eye services and more of the pending need may have been met. Regardless, focusing on strengthening the last part of the referral system, i.e. hospital attendance following referral (Fig. 2), seems an area with room for further improvement in this context, to close the loop of eye care needs. This was flagged as a priority by ongoing monitoring and evaluation during the programme, and work has already been undertaken to tackle this [11]. As a newly implemented programme, approximately one fifth of people in need have been successfully reached so far, which is very encouraging for this early implementation phase.
The leading cause of blindness as demonstrated in Fig. 4 was untreated cataract both in survey and programme data (55% and 61%). There were however discrepancies between other common causes, especially corneal opacities, which were reported with much higher frequency during the RAAB survey than in the CEH programme. Of note, more details of diagnosis were provided in the RAAB, while in programme data more cases were categorised as “other”. Corneal causes of VI may have been reported as “other” in some cases, leading to this difference. Although epidemiological data collection is not the primary goal of a programme, this might imply potential for improvement in precision of data collection within the programme, and could represent a limitation in our results. Alternatively, as RAAB surveys are statistically powered for their primary outcome: prevalence of blindness, the RAAB estimates of distribution of causes may be less precise.
Study limitations include that our estimates of need were based on point prevalence estimates from the RAAB survey, without modelling of new case incidence or population growth during the study time frame, or reduction in cases due to death or treatment elsewhere. This avoided introduction of an extra layer of uncertainty within our estimates, but means that some new cases may not be included in the estimates.
Another interesting result to note is that the prevalences of visual impairment and blindness were similar in the RAAB results to the group which was screened as “not healthy” in the first stage of the programme (Table 1), and attended triage. There are various possible explanations for this. If screening is accurate, with minimal false negatives, then disproportionately more healthy people without visual impairment are attending for screening than people with visual impairment. Screening out many of the healthy people is then returning proportions to the population baseline. This could occur if it is easier for people with good vision to become aware of the programme or to attend (e.g. due to ease of travel). Focusing on community awareness and programme enrolment methods such that people with visual impairment are more likely to participate could increase the effectiveness of the programme in reaching the population in need.
Further research is ongoing in the form of data collection within the continued programme. Visual outcome of patients who have undergone cataract surgery or received refractive correction would be beneficial to allow analysis of the effectiveness of interventions: eREC and eCSC. A repeat RAAB later would add helpful information regarding the change in prevalence of blindness and VI by each cause, following intervention by the programme.
Conclusions
In this study, we compared start line RAAB survey estimates directly to programme data, to assess programme reach. The programme reached an estimated 20.1% of all expected cases of blindness in the survey area (n = 513/2,556) in the first four years, 18.3% of the unmet need from cataract, and 21.1% of URE, equally in both men and women. In combination, the survey and programme reached 23.4% of people with VI. Use of survey data in this way allows for improved monitoring and evaluation, highlighting any inequities in who is accessing the programme, as well as enabling calculation of the proportion of need which has been met. This can help planners of eye care programmes to allocate resources and to estimate the required duration of a programme to meet existing backlogs.
Data availability
The data used during the current study may be available from the corresponding author on reasonable request.
Abbreviations
- CEH:
-
Community Eye Health
- COAVS:
-
College of Ophthalmology and Allied Vision Sciences
- CSC:
-
cataract surgical coverage
- DVA:
-
distance visual acuity
- eCSC:
-
effective cataract surgical coverage
- eREC:
-
effective refractive error coverage
- MSVI:
-
moderate-severe visual impairment
- RAAB:
-
Rapid Assessment of Avoidable Blindness
- URE:
-
uncorrected refractive error
- VA:
-
visual acuity
- VI:
-
visual impairment
- WHO:
-
World Health Organization
References
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489–551.
McCormick I, Mactaggart I, Bastawrous A, Burton MJ, Ramke J. Effective refractive error coverage: an eye health indicator to measure progress towards universal health coverage. Ophthalmic Physiol Opt. 2020;40(1):1–5.
Keel S, Müller A, Block S, Bourne R, Burton MJ, Chatterji S, et al. Keeping an eye on eye care: monitoring progress towards effective coverage. Lancet Glob Health. 2021;9(10):e1460–4.
Bourne R, Steinmetz J, Flaxman S et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the global burden of Disease Study. Lancet Glob Health. 2020. Accessed via the IAPB Vision Atlas (https://www.iapb.org/learn/vision-atlas)
Mactaggart I, Limburg H, Bastawrous A, Burton MJ, Kuper H. Rapid Assessment of Avoidable Blindness: looking back, looking forward. Br J Ophthalmol. 2019;103(11):1549–52.
Bourne RRA, Cicinelli MV, Sedighi T, Tapply IH, McCormick I, Jonas JB, et al. Effective refractive error coverage in adults aged 50 years and older: estimates from population-based surveys in 61 countries. Lancet Glob Health. 2022;10(12):e1754–63.
Mushumbusi E, Buchan J, Mactaggart I, Macleod D, Foster A. A systematic review of the proportion of blindness in the Population 50 years and older from Total Population-based surveys of blindness and visual impairment. Ophthalmic Epidemiol. 2022;29(2):164–70.
Jolley E, Cumaio M, Vilanculos A, Hassane I, Kimani K, Ogundimu K, et al. Changes in Eye Health and Service Coverage in Nampula, Mozambique between 2011 and 2018. Ophthalmic Epidemiol. 2022;29(1):91–9.
Reis T, Lansingh V, Ramke J, Silva JC, Resnikoff S, Furtado JM. Cataract as a Cause of Blindness and Vision Impairment in Latin America: Progress made and challenges beyond 2020. Am J Ophthalmol. 2021;225:1–10.
Solomon SD, Shoge RY, Ervin AM, Contreras M, Harewood J, Aguwa UT, et al. Improving Access to Eye Care: a systematic review of the literature. Ophthalmology. 2022;129(10):e114–26.
Khan AA, Talpur KI, Awan Z, Arteaga SL, Bolster NM, Katibeh M, et al. Improving equity, efficiency and adherence to referral in Pakistan’s eye health programmes: pre- and post-pandemic onset. Front Public Health. 2022;10:873192.
Pakistan Bureau of Statistics. Pakistan Census - Population by Single Year Age, Sex and Rural/Urban. https://www.pbs.gov.pk/sites/default/files/population/2017/results/04004.pdf; 2017. Accessed March 27, 2023.
Muhit M, Wadud Z, Islam J, Khair Z, Shamanna BR, Jung J, Khandaker G. Generating evidence for Program Planning: Rapid Assessment of Avoidable blindness in Bangladesh. Ophthalmic Epidemiol. 2016;23(3):176–84.
Taryam MO, Rabiu MM, Muhammad N, Oladigbolu K, Abdurrahman H. Prevalence and causes of blindness and visual impairment; and cataract surgical services in Katsina state of Nigeria. Br J Ophthalmol. 2020;104(6):752–6.
Muhammad N, Adamu MD, Mpyet C, Bounce C, Maishanu NM, Jabo AM, Rabiu MM, Bascaran C, Isiyaku S, Foster A. Impact of a 10-Year Eye Care Program in Sokoto, Nigeria: changing pattern of prevalence and causes of blindness and visual impairment. Middle East Afr J Ophthalmol. 2019;26(2):101–6.
Guruprasad BS, Krishnamurthy D, Narendra DP, Ranganath BG, Shamanna RB. Changing scenario of cataract blindness in Kolar District, Karnataka, South India. The utility of rapid assessment of avoidable blindness in reviewing programs. Ophthalmic Epidemiol. 2013;20(2):89–95.
Pawiroredjo JC, Minderhoud J, Mans DR, Themen HC, Bueno de Mesquita-Voigt AT, Siban MR, Forster-Pawiroredjo CM, Moll AC, van Nispen RM, Limburg H. The cataract situation in Suriname: an effective intervention programme to increase the cataract surgical rate in a developing country. Br J Ophthalmol. 2017;101(2):89–93.
Yoshizaki M, Ramke J, Zhang JH, Aghaji A, Furtado JM, Burn H, et al. How can we improve the quality of cataract services for all? A global scoping review. Clin Exp Ophthalmol. 2021;49(7):672–85.
Jolley E, Buttan S, Engels T, Gillani M, Jadoon MZ, Kabona G, et al. Prevalence of Visual Impairment and Coverage of Cataract Surgical services: associations with Sex, disability, and Economic Status in five Diverse sites. Ophthalmic Epidemiol. 2020;27(6):429–37.
Acknowledgements
The authors would like to acknowledge all contributors to the RAAB survey, the Talagang CBM/Peek CEH programme and similar global programmes working to tackle avoidable visual impairment, including community health workers, social organisers, Lady Health Visitors, and programme participants.
Funding
The RAAB survey and eye health programme described in this study were financially supported by CBM International. No specific funding was obtained for this analysis. The publication of this work was supported by the National Institute for Health Research (NIHR) (using the UK’s Official Development Assistance (ODA) Funding) and Wellcome [215633/Z/19/Z] under the NIHR-Wellcome Partnership for Global Health Research. The views expressed are those of the authors and not necessarily those of Wellcome, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
MZJ, ZHA, MM, RY and SLA were involved in the design of the survey/programme and data acquisition. MK, SLA, AB and EW were involved in the conception of the work. AB and SLA provided infrastructure and training for digital data collection, data records and transmission of data. MK performed data analysis and prepared the figures. EW and MK wrote the manuscript. All authors were involved in the review of the text and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Research followed the tenets of the Declaration of Helsinki. Data storage and transmission in the RAAB survey and the CEH programmes were conducted in compliance with a Data Protection Agreement (DPA) and aligned with the European Union General Data Protection Regulation (GDPR). The study was approved by the Ethical Review Board of the College of Ophthalmology and Allied Vision Sciences (COAVS), with permissions obtained from stakeholders for data usage while ensuring anonymity.
Consent to participate
Not applicable. Written consent from participants was not required, in line with national legislation and institutional requirements.
Competing interests
The authors have made the following disclosures: AB: Co-founder - Peek Vision; SLA, EW and MK: Financial support - Peek Vision; ZA: Financial support - CBM International. No personal financial support related to this manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jadoon, M.Z., Awan, Z., Moin, M. et al. Assessment of eye health programme reach by comparison with rapid assessment of avoidable blindness (RAAB) survey data, Talagang, Pakistan. BMC Prim. Care 25, 250 (2024). https://doi.org/10.1186/s12875-024-02503-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02503-4