Abstract
Background
The lack of trust between patients and physicians has a variety of negative consequences. There are several theories concerning how interpersonal trust is built, and different studies have investigated trust between patients and physicians that have identified single factors as contributors to trust. However, all possible contributors to a trusting patient-physician relationship remain unclear. This review synthesizes current knowledge regarding patient-physician trust and integrates contributors to trust into a model.
Methods
A systematic search was conducted using the databases MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), and Eric (Ovid). We ran simultaneous searches for a combination of the phrases: patient-physician relationship (or synonyms) and trust or psychological safety. Six-hundred and twenty-five abstracts were identified and screened using pre-defined criteria and later underwent full-text article screening. We identified contributors to trust in the eligible articles and critically assessed whether they were modifiable.
Results
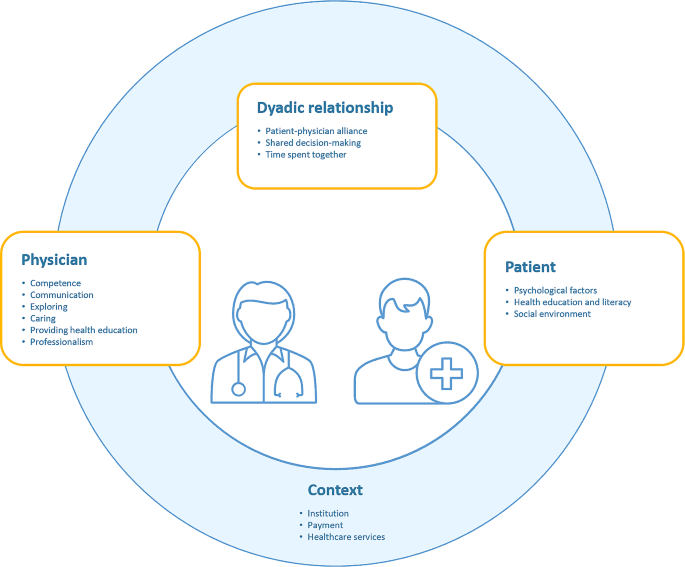
Forty-five articles were included in the review. Patient-centered factors that contributed modifiable promoters of trust included psychological factors, levels of health education and literacy, and the social environment. Physician-centered factors that added to a trusting patient-physician relationship included competence, communication, interest in the patient, caring, the provisioning of health education, and professionalism. The patient-physician alliance, time spent together, and shared decision-making also contributed to trusting relationships between patients and physicians. External contributors included institutional factors, how payments are made, and additional healthcare services.
Discussion
Our model summarized modifiable contributors to a trusting patient-physician relationship. We found that providing sufficient time during patient-physician encounters, ensuring continuity of care, and fostering health education are promising starting points for improving trust between patients and physicians. Future research should evaluate the effectiveness of interventions that address multiple modifiable contributors to a trusting patient-physician relationship.
Similar content being viewed by others
Introduction
Trust, as a cornerstone of human relationships, applies to the patient-physician relationship. Relationship building is a basic skill for the medical professional [1, 2]. There is evidence that trust between patients and doctors has a positive effect and, if trust is missing, leads to potentially negative consequences. A meta-analysis confirmed that trust was positively associated with improved health outcomes [3] in, for example, diabetes [4], cancer [5], and human immunodeficiency virus infections (HIV infections) [6]. Trust also increases positive behavioral outcomes in patients [7], such as treatment adherence [8, 9]. In contrast, low trust in physicians has been shown to negatively affect various patient health outcomes [4, 6, 10,11,12,13,14]. Economically, if trust in physicians is missing, it has adverse financial effects on healthcare systems [15]. Furthermore, a physician may be more likely to incur complaints when trusting relationships with patients are lacking [16].
In medicine, trust can be understood as being social or interpersonal [17, 18]. Social trust refers to individuals’ trust in institutions or systems, such as the healthcare system or physicians in general, while interpersonal trust refers to the trust between two individuals [18, 19]. Social trust is believed to affect interpersonal trust in medical settings [17, 18]. There are various theories of trust from different disciplines [20,21,22,23]. However, the most prominent interpersonal trust theory in psychology (and applied in medical settings) is from Mayer et al., who defined trust as the willingness of an individual to be vulnerable to the actions of another based on the expectation that the other will perform a particular action important to the trustor, irrespective of the ability to monitor or control the other party [24]. Their theory of interpersonal trust suggests that benevolence, integrity, ability, propensity to trust, and perceived risk are components of a trust relationship [24]. When applied to the patient-physician relationship, the physician’s ability, integrity, and benevolence act as contributors. At the same time, a patient’s propensity to trust—their willingness to trust others—and the perceived risk they take when trusting a physician are also important factors. However, the reality is likely more complex, and there are probably more contributors to a trusting patient-physician relationship than the theory proposes. While different evidence-based studies have investigated the patient-physician trust relationship, to our knowledge, there has been no synthesis of all the evidence-based contributors to the relationship. In 2000, there was a call for an empirical conceptualization of trust. Rather than single theories used to explain interpersonal patient-physician trust or studies investigating isolated contributors of trust, the idea was to synthesize empirical evidence concerning how patient-physician trust can evolve into a model [19]. A recent review on trust in the medical field has renewed the need for such an empirical conceptualization of patient-physician trust [25]. Therefore, this study aimed to summarize the empirical evidence, identify the contributors to a trusting patient-physician relationship, and integrate them into a model. This model can then be used to identify potential approaches and leverage points to improve patient-physician trust. The two main research questions were:
-
1.
Which factors contribute to a trusting patient-physician relationship?
-
2.
Which of these factors can act as potential leverage points to improve the patient-physician relationship?
In addition, we critically assessed contributors based on how they are already implemented in healthcare systems and medical education.
Methods
As the research questions were too broad for a systematic or scoping review, a critical review with a systematic search approach was used to answer the first research question. Critical reviews focus on empirical research [26] to evaluate what is known about a specific topic and integrate it into a framework [26, 27]. They may use a systematic search strategy to integrate the strengths of systematic and critical reviews [27], including all relevant literature, to avoid biases.
Search strategy
We searched the databases MEDLINE (Ovid), Embase (Ovid), PsycINFO (Ovid), and ERIC (Ovid) for a combination of terms (or synonyms) referring to the patient-physician relationship and trust or psychological safety. Database searches were run simultaneously as multifile searches in Ovid. For the results, Ovid’s de-duplicator was used. No study or clinical trial registries or online resources were searched. No experts were contacted, nor was a citation search conducted. A reproducible search for all of the databases is as follows:
Embase (1974 to January 13, 2022), ERIC (1965 to May 2021), Ovid MEDLINE(R) ALL (1946 to January 13, 2022), APA PsycInfo (1806 to January Week 1, 2022).
-
1
(patient* adj2 physician* adj2 (relation* or alliance or rapport)).ti, ab.
-
2
(trust* or psychological safety).ti, ab.
-
3
1 and 2.
-
4
remove duplicates from 3.
We did not use any language, time period, study design, or other restrictions for the searches, and no search filters were used. The comprehensive literature search was run on January 13, 2022 and 630 articles were retrieved. An information specialist assisted in framing the research questions and provided information on the different types of reviews. Once a first draft of the search strategy was developed, multiple feedback rounds with the information specialist were conducted until the search strategy was finalized.
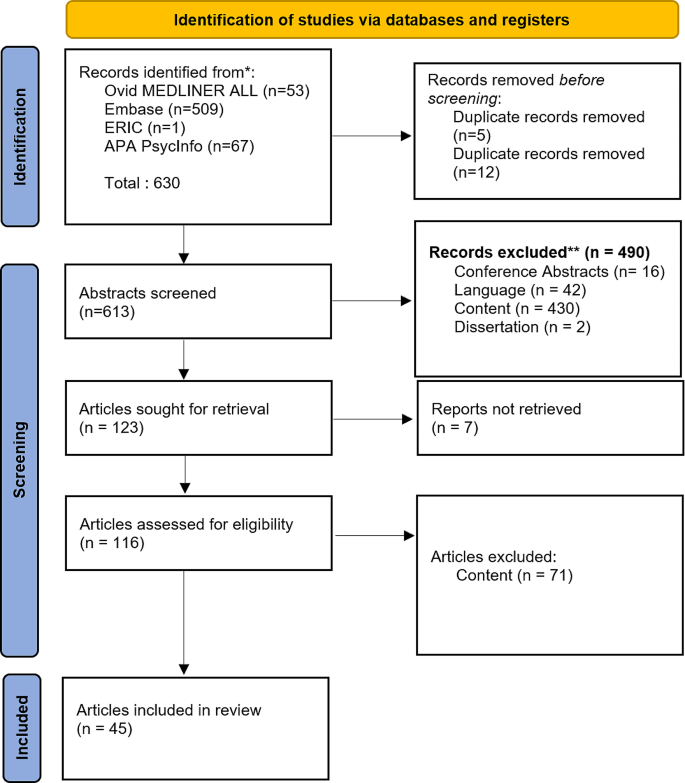
Screening process
Fifty-three records were retrieved from Ovid MEDLINER ALL, 509 from Embase, 1 from ERIC, and 67 from APA PsycInfo. In total, 630 records were found. As OVID’s de-duplication process did not identify all duplicates, any remaining duplicates were removed by SPL using EndNote’s duplicate identification strategy and a manual approach. After de-duplication, 613 articles remained, which were screened in two rounds. The first round was screened according to title and abstract. In the second round, 116 articles were evaluated for inclusion based on the full texts. SPL and RH did the screening, and AL decided when there were disagreements between SPL and RH. A study selection flowchart is shown in Fig. 1.
We included studies that reported factors contributing to a trusting relationship between patients and physicians and excluded those that only reported contributing factors between patients and health professionals other than physicians (or no contributors). We also included studies that explicitly measured trust between a patient and physician either quantitatively or qualitatively and excluded those with no measure of patient trust in physicians (e.g., only generalized patient trust or trust in other health professionals). We included quantitative, qualitative, and mixed methods papers and excluded dissertations and conference abstracts. Only articles in English and German were included.
Data synthesis and categorization
We first extracted the contributors mentioned in the studies as this review focused on integrating contributors to a trusting patient-physician relationship into an overall model. Extracted data included information on the setting, patients, physicians, how trust was operationalized, and which factors had a positive, negative, or no effect on the relationship. Contributors were then categorized into patient-related, physician-related, context-related, or patient- and physician-related factors. Study sizes and methods of measurement were highlighted. The factors were then synthesized, and the modifiable ones were extracted and displayed in a model.
Results
Forty-five heterogeneous studies reported factors contributing to a trusting patient-physician relationship. An overview of these studies, including the contributors to trust for each study, can be found in Appendix 1.
Patient-related factors
Several patient-related contributors to a trusting relationship were investigated, sometimes with contrasting results from different studies. These included demographic characteristics (gender, marital status, age, ethnicity, birthplace, and country of residence), health condition, health education and literacy, socioeconomic status, religious beliefs, social environment, psychological factors, and the patient’s health condition and status.
Studies found better mental and physical health status tended to positively affect the relationship—although this result was mixed. In several studies, a good general health condition and better self-reported health status were associated with increased trust towards the physician [28,29,30,31,32]. However, other studies found no correlation between self-reported health status and trust. For specific health conditions, low-risk adults without chronic illnesses had higher trust in their physicians than adults with risk factors such as diabetes or high lipid levels [33,34,35,36,37]. Disease progression, including relapses and lack of improvement of a medical condition, was negatively associated with trust [38, 39], whereas a shorter duration of illness increased trust in the physician [29]. However, two studies found no connection between trust, disease duration [40], and healing [36].
Patient health education and literacy levels were found to promote a trusting patient-physician relationship, with higher health education [41] and literacy [42] levels contributing to trust and low health literacy [43] hindering it.
Patient socioeconomic status, including occupation, employment, educational and income levels, and the presence or type of health insurance, were all potential contributors, with high (household) income and educational levels, having health insurance, and being employed positively related to trust; although, these findings were ambiguous. Religious belief was also associated with trust in physicians [31].
The social environment, including social support and the care experiences of family members, further contributed to a trusting patient-physician relationship. In particular, poor social support negatively influenced trust [43], as did dissatisfaction with the care of family members [44, 45].
The health locus of control was also associated with trust. This describes how a person views control of their health. An internal health locus of control suggests that the person sees oneself as controlling their health, whereas an external locus means that the person perceives external factors influencing their health.
Several patient psychological factors, including a propensity to trust, their coping mechanisms and attachment style, the health locus of control, and general trust in caregivers contributed to a trusting patient-physician relationship. Individuals who see powerful others as their health locus of control (i.e., believing other people, such as health professionals, can control their health) exhibited higher trust in physicians [46]. Poor coping styles hindered trust [43], while the willingness to reframe situations (a healthy coping style) added to a trusting patient-physician relationship [44]. For the most part, a general trust in doctors, caregivers, the healthcare system, or online health communities was associated with higher trust [47,48,49]. However, these findings were ambiguous regarding the propensity to trust. One study found that a patient’s propensity to trust predicted trust in their physician [50], although other studies did not find this connection [31, 36]. Table 1 summarizes all of the evidence concerning patient-related factors.
Physician-related factors
Demographic characteristics, competence, communication, exploring, caring, provisioning health education, reputation, professionalism, and availability were investigated as potential contributors to a trusting patient-physician relationship.
Demographic characteristics of the physician, such as age and gender, did not contribute to a trusting relationship, although these findings were ambiguous.
Physician competency, including the perceived competence of the physician by the patient [41, 44, 51, 55, 68,69,70], the physician being up-to-date in their specialization [71], and having more years of experience [71] helped to build a trusting relationship with patients. Communication skills, including general communication skills [29, 38, 44, 52, 70, 72, 73], compassion, listening to the patient [41, 44, 52], as well as nonverbal behavior such as good eye contact, providing undivided attention, open body language, and smiling [41, 44, 52, 73] also enhanced the trust relationship as did patient-centered [63, 74, 75], comprehensive care [30].
Physicians exploring a patient’s disease and problems [69], illness experiences [28], and the context of the patient [44, 68] promoted a trusting relationship along with caring behavior [52, 70, 75] such as empathy [50, 76] and compassion [41, 44, 69].
Provisioning health education to the patient contributed to a trusting relationship [38, 41, 64, 68, 69]; however, one study did not find any association between these factors [71].
We did identify physician reputation [71] and the reputation of their medical specialty [28, 34, 39] as contributing to a trusting relationship. Moreover, different aspects of professionalism [71, 73], such as honesty [51, 55, 69] and availability [41], contributed to a trusting patient-physician relationship, while being disrespectful, arrogant, or cynical were negatively associated with trust [41, 73, 75]. These results are summarized in Table 2.
Physician- and patient-related factors
Contributors related to the physician and patient were concordance, time spent together, the patient-physician alliance, and shared decision-making.
In relation to concordance, both gender and race were tested as promoters of trust; however, only gender concordance was identified as being a contributor [35, 41].
Time spent together included time spent in a single session, the overall time spent together, and the continuity of care. Most results indicated that more time spent together in a single session [28, 71, 73] (with the physician giving the patient enough time to explain the reason for the visit [77]) promoted trust, whereas physicians appearing rushed was a barrier to a trusting relationship [44]. If the duration of the relationship with the doctor was long-term [28, 36, 77], the patient had higher rates of follow-up visits [51] and more physician visits in general [37, 57]. Nevertheless, those findings were mixed, and not all studies found an association between the duration of a relationship with the doctor [40, 45] and the number of team visits [47, 48]. However, continuity of care [51] and continuity with one physician added to a trusting relationship [30].
Within the patient-physician alliance, alliances in shared decision-making [65] and having a good rapport [71] were found to enhance trust, while a patient’s perception of a physician’s distrust was a barrier [41]. Finding common ground [28] and shared identity [52] were tested but did not show any association with trust. In contrast, shared decision-making contributed to a trusting relationship that promoted trust in most studies [41, 42, 44]. These findings are summarized in Table 3.
Context-related factors
Context-related factors such as practice/institution, physician payments, and additional healthcare services were investigated as potential contributors to trusting relationships.
Most aspects of the practice or the institution were found to contribute to a trusting relationship, with easy accessibility [30] to the practice and a good reputation [71] promoting trust, while institutional betrayal [65] hindered it. The atmosphere of the practice also mattered. A good practice or organizational climate added to a trusting relationship [35], whereas perceived chaos hampered it [29]. Patients having enough physician choice also added to a trusting relationship [48], while managed care settings contributed to mistrust [41]. Inpatient settings enhanced trust compared to outpatient settings [59]. Regarding payments, situations where patients do not know how the physician is paid or the physician is paid by the number of office visits rather than a fixed salary [30] contributed to a trusting relationship. In contrast, public disclosure of payments was negatively associated with trust [78]. Additional health services such as addiction consultations [79], preventive services [77], and the coordination of specialty care [30] also contributed to patient-physician trust. These findings are summarized in Table 4.
Potential leverage points to improve a trusting relationship
We integrated the modifiable contributors to a trusting patient-physician relationship from each conceptual group into a model and identified potential leverage points for improving the relationship (Fig. 2).
Patient-centered leverage points
Within patient-centered factors, health education and literacy, the social environment, and psychological factors were modifiable. A patient who is better educated about health and can understand and use this education for themselves (health literacy) may form better trusting relationships with their physicians; thus, interventions should focus on improving health education and literacy. Patient psychological factors such as coping styles and health locus of control are other potential leverage points to increase trust within the relationship. The social environment, specifically receiving sufficient social support, was a further modifiable contributor to trust, indicating that targeted interventions should aim to improve patients’ social support systems.
Physician-centered leverage points
We identified physicians’ competence, communication skills, exploring, caring, the provisioning of health education, and professionalism as modifiable contributors to a trusting patient-physician relationship. For competence, being up-to-date in the specialization and perceived as competent are leverage points that could increase trust. Communication skills, including verbal and nonverbal behavior, exploring patient health, and professionalism, can also be learned and are, hence, modifiable. Caring, including empathy and compassion, is a skill that can be increased through interventions and also used to increase trust. In addition, physicians can be taught how to provide health education, and specific material can be provided to them for health education, which is another potential leverage point.
Patient and physician-centered leverage points
We identified shared decision-making, the patient-physician alliance, and time spent together as contributors that can be modified. Although time spent together and the continuity of care is context-dependent, awareness can be raised among physicians, and specific training can help the physician allow patients to explain the reason for their visit. Alliances and shared decision-making are skills taught during medical school: therefore, potential interventions already exist. Shared decision-making also includes healthcare professionals other than physicians. Therefore, one possible intervention strategy would be to foster interprofessional education and teamwork to support shared decision-making between patients and healthcare professionals.
Context-dependent leverage points
The healthcare system, provisioning of additional healthcare services, transparency regarding physician payment, and characteristics of the practice or institution (e.g., keeping a good institutional climate and having mechanisms to prevent institutional betrayal) are modifiable contributors; however, these strongly depend on the specific country. Furthermore, only a few studies have investigated contributors to a trusting relationship within this conceptual group. Therefore, the list of context-dependent contributors may be limited.
Discussion
We conducted a critical review with a systematic search strategy to identify evidence-based contributors to a trusting patient-physician relationship and integrated the modifiable contributors into a model. Our results confirm the existing theory of interpersonal trust [24], and, in line with this theory, we found that the physician’s caring (benevolence), competence and communication (ability), and professionalism (integrity) were contributors to a trusting patient-physician relationship. In addition, the physician’s exploring and provisioning of health education also contributed to a trusting relationship. We confirmed the importance of a patient’s propensity to trust as a psychological contributor and were able to add more psychological factors, including coping style and health locus of control. We further added the patient’s level of health education and literacy, and social environment as contributing factors and confirmed that, as the risk a patient must take concerning their health decreases, the easier it is for them to trust the physician. Our model further adds physician- and patient-related factors and the institutional context. The latter indicates the importance of including social trust in understanding interpersonal trust in medicine, as suggested by Mechanic [18]. One highly prominent factor was health education, which can be addressed by the physician, patient, and the context, which suggests that fostering health education is a promising intervention to increase trust.
Patients
Patient psychological factors such as coping styles and health locus of control are modifiable contributors to a trusting relationship. Previous studies have shown that coping styles can be improved for chronically ill patients [80], while other interventions can address a patient’s health locus of control and improve their social support systems. Furthermore, social support interventions have been shown to be effective in patients with different diseases [81,82,83]. Health education could be addressed through e-learning and by provisioning self-help groups that exchange ideas about diseases [84] with educational tools and teaching materials [85]. However, these interventions are system-related as the healthcare system must offer those interventions.
Medical education
Most physician-centered modifiable contributors to a trusting relationship fall under the scope of medical education. Competence is acquired and addressed through university education, graduate school, and continuing education. Communication skills are taught in medical education courses, and professionalism is addressed as a CanMED role [86]. Exploration is an important skill that is already part of communication curriculums [87] and is based on the common-sense model of illness [88]. Physicians can be taught to provide health education [89]; however, it is a skill that medical students find difficult to achieve [90]. Further intervention possibilities could address a physician’s ability to express compassion and empathy. A recent review summarized educational methods used to address medical student empathy [91], with simulation training shown to be an effective tool [92].
A practical example that implements the described practices can be found in the Presence 5 project, which teaches physicians to better listen to patients, explore their story and emotions, and connect with them. These teachings have had positive effects on the physicians’ attitude, compassion, communication, and exploring behavior [93, 94].
Patient- and physician-related factors
As with physician-related contributors to trust, patient- and physician-related promoters of trust could be addressed through medical education. Building an alliance with patients and learning about shared decision-making are skills taught in medical school [95]. The physician can also be made aware that spending sufficient time with a patient is relevant to building trust; however, the ability to modify this contributor is dependent on the healthcare and billing system.
Context-dependent contributors
We found that a transparent billing system and institution-related contributors such as reputation, medical practice atmosphere, accessibility, and additional healthcare services contributed to a trusting patient-physician relationship. A recent discussion on making health care more accessible can be found in Gupta et al. [96].
One healthcare system that addresses many of these factors is Canada’s patient-centered model: ‘the patient’s medical home.’ Under this model, patients can choose a physician they feel comfortable with and who will continuously manage their health care over their lifespan. Each physician is surrounded by a team that considers the patient’s situation and may provide additional healthcare services when needed. This model ensures that each patient receives comprehensive and accessible care that provides sufficient time with the physician and guarantees continuity of care [https://patientsmedicalhome.ca/, 97]. Over the long term, patient medical homes have led to better care, decreased costs, and more satisfaction for providers and patients [https://patientsmedicalhome.ca/, 97]. Other positive aspects of the patient’s medical home, aside from increased continuity of care and the availability of additional health care services, may lie within the aspect of time spent together [98] or improved disease progression [99], which is also addressed within the patient’s medical homes.
Strengths and limitations
The strength of this critical review lies in the systematic search approach, which only included papers that operationalized or specifically described trust. Despite this approach, we cannot ensure that we have included all empirical contributors to patient-physician trust that have been researched. While the systematic search did limit bias in the identified contributors within the critical assessment of what could be modifiable or not, the critical assessment could be biased through the author’s background. However, we discussed the process in depth as a team.
Our search strategy included psychological safety as a synonym for trust, as well as the terms rapport, alliance, and relationship. We checked indexed search terms to ensure the inclusion of relevant synonyms. In the past, trust was more conceptualized as rapport or alliance, whereas today, it is associated with a newer term: “psychological safety.” While we tried to include relevant search terms, we might have missed some, limiting the results.
While our search was not limited to patients trusting their physicians, most papers focused on this and excluded physicians’ trust in their patients. Dyadic analyses of patient-physician trust are scarce. However, Petrocchi et al. (2019) have begun investigating patient-physician trust as a dyad [100]. Some papers only reported correlations of trust with unmodifiable, less relevant, but easy-to-gather factors, such as sex or age. Thus, more contributors to trust may have yet to be investigated.
Implications for future research
Interestingly, many non-modifiable or insignificant contributors, such as physician or patient demographics, were investigated in almost every study we reviewed. However, the most promising contributors, such as health education, were barely explored. Future research should investigate modifiable and promising contributors to a trusting relationship that have, as yet, been barely researched, including patient psychological factors and additional healthcare services. Additionally, factors that have not been investigated should be addressed, including digitized healthcare settings and how telemedicine, chatbots, and video consultations affect patients’ trust in physicians. Further research should also focus on measuring how successful physician interventions are, as previous research and interventions have not increased patient trust [101, 102]. Future interventions should also consider multiple contributors to trust, as they are all related. For such interventions, the outcomes for each contributor should be evaluated first, with trust as a secondary outcome.
As the present review aimed to create a model of patient-physician trust, only studies that included trust between patients and physicians were included, with other healthcare professionals excluded. However, research has already acknowledged the importance of trusting relationships for all healthcare professionals [103], which should be further expanded. Thus, shared contributors to trust between healthcare professionals, their differences, and potential leverage points should also be identified.
Implications for practice
Our critical review has demonstrated that there are more contributors to a trusting patient-physician relationship than the theory of interpersonal trust proposes, and the context in which the patient-physician relationship takes place is highly relevant. One way to increase trust within the patient-physician relationship is to implement healthcare systems that are organized similarly to the Canadian ‘patient’s medical homes’ model. Changing the healthcare system is also an effective tool to simultaneously address multiple contributors to trust.
At the level of the institution, enhancing trust should focus on health education, which can be addressed through the implementation of self-help and support groups, providing high-quality health educational material, and training healthcare professionals.
At the physician level, we recommend taking as much time as possible for each patient to explore their perspective and current situation, organize (as much as possible) continuity of care, and ensure patient health education.
Conclusion
Using a systematic search, our model summarizes identified modifiable contributors to a trusting patient-physician relationship. Providing sufficient time during patient-physician encounters, ensuring continuity of care, and fostering health education are promising leverage points for improving trust between patients and physicians. Future research should evaluate the effectiveness of interventions that address multiple modifiable contributors to a trusting patient-physician relationship.
Data availability
The data (review search) of the current review are available from the corresponding author on reasonable request.
References
von Gunten CF, Ferris FD, Emanuel LL. The patient-physician relationship. Ensuring competency in end-of-life care: communication and relational skills. JAMA. 2000;284(23):3051–7.
Mahmud A. Doctor-patient relationship. Pulse. 1970;3(1):12–4.
Birkhauer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, Gerger H. Trust in the health care professional and health outcome: a meta-analysis. PLoS ONE. 2017;12(2):e0170988.
Alazri M, Neal R. The association between satisfaction with services provided in primary care and outcomes in type 2 diabetes mellitus. Diabet Med. 2003;20(6):486–90.
Mainous AG 3rd, Kern D, Hainer B, Kneuper-Hall R, Stephens J, Geesey ME. The relationship between continuity of care and trust with stage of cancer at diagnosis. Fam Med. 2004;36(1):35–9.
Preau M, Leport C, Salmon-Ceron D, Carrieri P, Portier H, Chene G, Spire B, Choutet P, Raffi F, Morin M. Health-related quality of life and patient-provider relationships in HIV-infected patients during the first three years after starting PI-containing antiretroviral treatment. AIDS Care. 2004;16(5):649–61.
Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(4):e94207.
Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47(3):213–20.
Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. J Fam Pract. 2005;54(4):344–52.
Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Pract. 2002;19(5):476–83.
Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. The relationship between method of physician payment and patient trust. JAMA. 1998;280(19):1708–14.
Balkrishnan R, Dugan E, Camacho FT, Hall MA. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41(9):1058–64.
Mainous AG 3rd, Kern D, Hainer B. The relationship between continuity of care and trust with stage of cancer at diagnosis. 2004.
Tarn DM, Meredith LS, Kagawa-Singer M, Matsumura S, Bito S, Oye RK, Liu H, Kahn KL, Fukuhara S, Wenger NS. Trust in one’s physician: the role of ethnic match, autonomy, acculturation, and religiosity among Japanese and Japanese Americans. Ann Fam Med. 2005;3(4):339–47.
Quigley DD, Reynolds K, Dellva S, Price RA. Examining the business case for patient experience: a systematic review. J Healthc Manag. 2021;66(3):200–24.
Levinson W. Physician-patient communication. JAMA. 1994;272(20).
Goold SD. Money and trust: relationships between patients, physicians, and health plans. J Health Polit Policy Law. 1998;23(4):687–95.
Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74(2):171–89.
Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000;15(7):509–13.
Sisk B, Baker JN. A model of interpersonal trust, credibility, and relationship maintenance. Pediatrics. 2019;144(6).
Hardin R. Trust: Polity; 2006.
Garrett L. Betrayal of Trust - the collapse of global public health. Oxford University Press; 2003.
Siegrist M, Gutscher H, Earle TC. Perception of risk: the influence of general trust, and general confidence. J Risk Res. 2006;8(2):145–56.
Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Acad Manage Rev. 1995;20(3).
Taylor LA, Nong P, Platt J. Fifty years of trust research in health care: a synthetic review. Milbank Q. 2023;101(1):126–78.
Sutton A, Clowes M, Preston L, Booth A. Meeting the review family: exploring review types and associated information retrieval requirements. Health Info Libr J. 2019;36(3):202–22.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, McDaniel SH, Epstein RM. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42(11):1049–55.
Kowalski C, Nitzsche A, Scheibler F, Steffen P, Albert U-S, Pfaff H. Breast cancer patients’ trust in physicians: The impact of patients’ perception of physicians’ communication behaviors and hospital organizational climate. [References]: Patient Education and Counseling. Vol.77(3), 2009, pp. 344–348.; 2009.
O’Malley AS, Forrest CB. Beyond the examination room: primary care performance and the patient-physician relationship for low-income women. J Gen Intern Med. 2002;17(1):66–74.
Benjamins MR. Religious influences on trust in physicians and the health care system. Int J Psychiatry Med. 2006;36(1):69–83.
Nelms E, Wang L, Pennell M, Wewers ME, Seiber E, Adolph MD, Paskett ED, Ferketich AK. Trust in physicians among rural medicaid-enrolled smokers. JRural Health. 2014;30(2):214–20.
Bachinger SM, Kolk AM, Smets EM. Patients’ trust in their physician–psychometric properties of the Dutch version of the wake forest physician trust scale. Patient Educ Couns. 2009;76(1):126–31.
Marcinowicz L, Jamiolkowski J, Gugnowski Z, Strandberg EL, Fagerstrom C, Pawlikowska T. Evaluation of the trust in physician scale (TIPS) of primary health care patients in north-east Poland: a preliminary study. Family Med Prim Care Rev. 2017;19(1):39–43.
Bonds DE, Foley KL, Dugan E, Hall MA, Extrom P. An exploration of patients’ trust in physicians in training. J Health Care Poor Underserved. 2004;15(2):294–306.
Ruch W, Heintz S. Experimentally manipulating items informs on the (Limited) construct and criterion validity of the humor styles Questionnaire. Front Psychol. 2017;8:616.
Becker ER, Roblin DW. Translating primary care practice climate into patient activation: the role of patient trust in physician. Med Care. 2008;46(8):795–805.
Mack JW, Kang TI. Care experiences that foster trust between parents and physicians of children with cancer. Pediatr Blood Cancer. 2020;67(11):(no pagination).
Yang J, Lu Y, Liao X, Chang MP. Examining patient trust towards physicians between clinical departments in a Chinese hospital. PLoS ONE. 2021;16(11 November):(no pagination).
Aloba O, Mapayi B, Akinsulore S, Ukpong D, Fatoye O. Trust in physician scale: factor structure, reliability, validity and correlates of trust in a sample of Nigerian psychiatric outpatients. Asian J Psychiatry. 2014;11:20–7.
Cook KS, Kramer RM, Thom DH, Stepanikova I, Mollborn SB, Cooper RM. Trust and Distrust in Patient-Physician Relationships: Perceived Determinants of High- and Low-Trust Relationships in Managed-Care Settings. [References]: Kramer, Roderick M, editor; Cook, Karen S, editor. (2004). Trust and distrust in organizations: Dilemmas and approaches. (pp. 65–98). xii, 381 pp. New York, NY, US: Russell Sage Foundation; US.; 2004.
Dehghan H, Keshtkaran A, Ahmadloo N, Bagheri Z, Hatam N. Patient involvement in care and breast cancer patients’ quality of Life- a structural equation modeling (SEM) approach. Asian Pac J cancer Prevention: APJCP. 2018;19(9):2511–7.
Gupta C, Bell SP, Goggins K, Cawthon C, Nwosu SK, Schildcrout JS, Kripalani S. Health literacy is an independent predictor of physician distrust. Circulation Conference: American Heart Association. 2013;128(22 Suppl. 1).
Canavera K. Rebuilding trust. Patient Educ Couns. 2021;104(5):996–7.
Oguro N, Suzuki R, Yajima N, Sakurai K, Wakita T, Hall MA, Kurita N. The impact that family members’ health care experiences have on patients’ trust in physicians. BMC Health Serv Res. 2021;21(1):1122.
Brincks AM, Feaster DJ, Burns MJ, Mitrani VB. The influence of health locus of control on the patient-provider relationship. Psychol Health Med. 2010;15(6):720–8.
Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26.
Kao AC. Trust and agency: the patient-physician relationship in the era of managed care: dissertation abstracts international section A: humanities and social sciences. Vol.59(5-A),1998, pp. 1790.; 1998.
Audrain-Pontevia AF, Menvielle L. Effects of interpersonal trust among users of online health communities on patient trust in and satisfaction with their physician. Int J Technol Assess Health Care. 2018;34(1):56–62.
Wu Q, Jin Z, Wang P. The Relationship between the physician-patient relationship, physician empathy, and patient trust. J Gen Intern Med. 2021.
Hillen MA, de Haes HC, Smets EM. Cancer patients’ trust in their physician-a review. Psychooncology. 2011;20(3):227–41.
Gopichandran V, Chetlapalli SK. Trust in the physician-patient relationship in developing healthcare settings: a quantitative exploration. Indian J Med Ethics. 2015;12(3):141–8.
Wang W, Zhang H, Washburn DJ, Shi H, Chen Y, Lee S, Du Y, Maddock JE. Factors influencing trust towards physicians among patients from 12 hospitals in China. Am J Health Behav. 2018;42(6):19–30.
Baidya M, Gopichandran V, Kosalram K. Patient-physician trust among adults of rural Tamil Nadu: a community-based survey. J Postgrad Med. 2014;60(1):21–6.
Hamelin ND, Nikolis A, Armano J, Harris PG, Brutus JP. Evaluation of factors influencing confidence and trust in the patient-physician relationship: a survey of patient in a hand clinic. Chirurgie De La main. 2012;31(2):83–90.
Zhao DH, Rao KQ, Zhang ZR. Patient trust in physicians: empirical evidence from Shanghai, China. Chin Med J. 2016;129(7):814–8.
Dong E, Liang Y, Liu W, Du X, Bao Y, Du Z, Jin M. Construction and validation of a preliminary Chinese version of the wake forest physician trust scale. Med Sci Monit. 2014;20:1142–50.
Gupta C, Bell SP, Schildcrout JS, Fletcher S, Goggins KM, Kripalani S. Predictors of health care system and physician distrust in hospitalized cardiac patients. J Health Communication. 2014;19(Supplement 2):44–60.
Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13(10):681–6.
Blanch-Hartigan D, van Eeden M, Verdam MGE, Han PKJ, Smets EMA, Hillen MA. Effects of communication about uncertainty and oncologist gender on the physician-patient relationship. Patient Educ Couns. 2019;102(9):1613–20.
Mainous AG 3rd, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001;33(1):22–7.
Gopichandran V, Wouters E, Chetlapalli SK. Development and validation of a socioculturally competent trust in physician scale for a developing country setting. BMJ Open. 2015;5(4):e007305.
Kushnir T, Bachner YG, Carmel S, Flusser H, Galil A. Pediatricians’ communication styles as correlates of global trust among jewish and bedouin parents of disabled children. J Dev Behav Pediatr. 2008;29(1):18–25.
Rawaf MM, Kressin NR. Exploring racial and sociodemographic trends in physician behavior, physician trust and their association with blood pressure control. J Natl Med Assoc. 2007;99(11):1248–54.
Shoemaker K, Smith CP. The impact of patient-physician alliance on trust following an adverse event. Patient Educ Couns. 2019;102(7):1342–9.
Holwerda N, Sanderman R, Pool G, Hinnen C, Langendijk JA, Bemelman WA, Hagedoorn M, Sprangers MAG. Do patients trust their physician? The role of attachment style in the patient-physician relationship within one year after a cancer diagnosis. Acta Oncol. 2013;52(1):110–7.
Aaraas IJ, Jones B, Gupta TS. [Norwegian and Australian physicians’ attitudes to adverse events]. Tidsskr nor Laegeforen. 2005;125(16):2204–6.
Berry LL, Parish JT, Janakiraman R, Ogburn-Russell L, Couchman GR, Rayburn WL, Grisel J. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6(1):6–13.
Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44(2):169–76.
Wolfson DB, Lynch TJ. Increasing trust in health care. Am J Manag Care. 2021;27(12):520–2.
Shaya B, Al Homsi N, Eid K, Haidar Z, Khalil A, Merheb K, Honein-Abou Haidar G, Akl EA. Factors associated with the public’s trust in physicians in the context of the Lebanese healthcare system: a qualitative study. BMC Health Serv Res. 2019;19(1):525.
Thom DH. Physicians’ trust in patients. JAMA - J Am Med Association. 2019;322(8):780–2.
Hendren EM, Kumagai AK. A matter of trust. Acad Medicine: J Association Am Med Colleges. 2019;94(9):1270–2.
Hillen MA, de Haes H, Stalpers LJA, Klinkenbijl JHG, Eddes EH, Butow PN, van der Vloodt J, van Laarhoven HWM, Smets EMA. How can communication by oncologists enhance patients’ trust? An experimental study. Ann Oncol. 2014;25(4):896–901.
El Malla H, Kreicbergs U, Steineck G, Wilderang U, El Sayed Elborai Y, Ylitalo N. Parental trust in health care - a prospective study from the children’s cancer hospital in Egypt. Psychooncology. 2013;22(3):548–54.
Weng HC. Does the physician’s emotional intelligence matter? Impacts of the physician’s emotional intelligence on the trust, patient-physician relationship, and satisfaction. Health Care Manage Rev. 2008;33(4):280–8.
Parchman ML, Burge SK. The patient-physician relationship, primary care attributes, and preventive services. Fam Med. 2004;36(1):22–7.
Kanter GP, Carpenter D, Lehmann LS, Mello MM. US nationwide disclosure of industry payments and public trust in physicians. JAMA netw. 2019;2(4):e191947.
King C, Collins D, Patten A, Nicolaidis C, Englander H. Trust in hospital physicians among patients with substance use disorder referred to an addiction consult service: a mixed-methods study. J Addict Med. 2021;09.
de Ridder D, Schreurs K. Developing interventions for chronically ill patients: is coping a helpful concept? Clin Psychol Rev. 2001;21(2):205–40.
van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns. 2005;59(1):1–12.
Lian OS, Rottingen JA. [The physicians–homo economicus or homo sociologicus?]. Tidsskr nor Laegeforen. 2002;122(17):1682–5.
Guillory J, Chang P, Henderson CR Jr., Shengelia R, Lama S, Warmington M, Jowza M, Waldman S, Gay G, Reid MC. Piloting a text message-based social support intervention for patients with chronic pain: establishing feasibility and preliminary efficacy. Clin J Pain. 2015;31(6):548–56.
Ghasemi M, Hosseini H, Sabouhi F. Effect of peer group education on the quality of life of elderly individuals with diabetes: a randomized clinical trial. Iran J Nurs Midwifery Res. 2019;24(1):44–9.
Delmas A, Clement B, Oudeyer P-Y, Sauzéon H. Fostering health education with a serious game in children with asthma: pilot studies for assessing learning efficacy and automatized learning personalization. Front Educ. 2018;3.
Verkerk MA, de Bree MJ, Mourits MJ. Reflective professionalism: interpreting CanMEDS’ professionalism. J Med Ethics. 2007;33(11):663–6.
Wissenschaften SAM. Kommunikation im medizinischen alltag. Ein Leitfaden für die Praxis. In.: Schweizerische Akademie der Medizinischen Wissenschaften (SAMW); 2019.
Diefenbach MA, Leventhal H. The common-sense model of illness representation: theoretical and practical considerations. J Social Distress Homeless. 2016;5(1):11–38.
Tresolini CP, Stritter FT. An analysis of learning experiences contributing to medical students’ self-efficacy in conducting patient education for health promotion. Teach Learn Med. 1994;6(4):247–54.
Benbassat J. Undesirable features of the Medical Learning Environment: a narrative review of the literature. Adv Health Sci Educ. 2013;18(3):527–36.
Sinclair S, Kondejewski J, Jaggi P, Dennett L, Roze des Ordons AL, Hack TF. What is the state of compassion education? A systematic review of compassion training in health care. Acad Med. 2021;96(7):1057–70.
Karvelyte M, Rogers J, Gormley GJ. Walking in the shoes of our patients’: a scoping review of healthcare professionals learning from the simulation of patient illness experiences. Adv Simul (Lond). 2021;6(1):43.
Shankar M, Henderson K, Garcia R, Li G, Titer K, Acholonu RG, Essien UR, Brown-Johnson C, Cox J, Shaw JG et al. Presence 5 for racial justice workshop: fostering dialogue across medical education to disrupt anti-black racism in clinical encounters. MedEdPORTAL. 2022;18:11227.
Brown-Johnson C, Cox J, Shankar M, Baratta J, De Leon G, Garcia R, Hollis T, Verano M, Henderson K, Upchurch M, et al. The Presence 5 for racial justice framework for anti-racist communication with black patients. Health Serv Res. 2022;57(Suppl 2):263–78.
Durand MA, DiMilia PR, Song J, Yen RW, Barr PJ. Shared decision making embedded in the undergraduate medical curriculum: a scoping review. PLoS ONE. 2018;13(11):e0207012.
Gupta R, Binder L, Moriates C. Rebuilding trust and relationships in medical centers: a focus on health care affordability. JAMA. 2020;324(23):2361–2.
Jackson GL, Powers BJ, Chatterjee R, Bettger JP, Kemper AR, Hasselblad V, Dolor RJ, Irvine RJ, Heidenfelder BL, Kendrick AS, et al. The patient centered medical home. A systematic review. Ann Intern Med. 2013;158(3):169–78.
Takach M. Reinventing Medicaid: state innovations to qualify and pay for patient-centered medical homes show promising results. Health Aff (Millwood). 2011;30(7):1325–34.
Klitzner TS, Rabbitt LA, Chang RR. Benefits of care coordination for children with complex disease: a pilot medical home project in a resident teaching clinic. J Pediatr. 2010;156(6):1006–10.
Petrocchi S, Iannello P, Lecciso F, Levante A, Antonietti A, Schulz PJ. Interpersonal trust in doctor-patient relation: evidence from dyadic analysis and association with quality of dyadic communication. Soc Sci Med. 2019;235:112391.
Thom DH. Training physicians to increase patient trust. J Eval Clin Pract. 2000;6(3):245–53.
Thom DH, Bloch DA, Segal ES. An intervention to increase patients’ trust in their physicians. Acad Med. 1999;74(2):195–8.
Rasiah S, Jaafar S, Yusof S, Ponnudurai G, Chung KPY, Amirthalingam SD. A study of the nature and level of trust between patients and healthcare providers, its dimensions and determinants: a scoping review protocol. BMJ Open. 2020;10(1):e028061.
Acknowledgements
We would like to thank the information specialist team at the library of the medical faculty of Bern. They supported the development of our research question and a search strategy. We also thank Adrian Michel (mediamatician) for the model illustration. The preliminary results of this review were presented at the European Health Psychology Conference on August 27, 2022 in Bratislava.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
S. P. L. conzeptualization, methodology, formal Analysis, writing original draft, visualization, supervisionR. H. formal Analysis, visualizationY. B. formal Analysis, visualization. A.L. conzeptualization, methodology, formal Analysis, writing review & editing, visualization, supervision. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lerch, S.P., Hänggi, R., Bussmann, Y. et al. A model of contributors to a trusting patient-physician relationship: a critical review using a systematic search strategy. BMC Prim. Care 25, 194 (2024). https://doi.org/10.1186/s12875-024-02435-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02435-z