Abstract
Background
The mental health and well-being of GPs is a critical issue as they play a vital role in providing healthcare services to individuals and communities. Research has shown that GPs often face high levels of stress, burnout, and mental health problems due to their demanding work environment. During the COVID-19 pandemic, GPs faced additional challenges which further impacted their mental health and well-being. This study aims to investigate the impact of systemic work-related stressors on the level of well-being of GPs in Belgium during the pandemic, with a particular emphasis on identifying regional variations between Flanders, Wallonia, and Brussels-Capital.
Methods
Data were collected with a self-reported online questionnaire from 479 GPs Belgian practices between December 2020 and August 2021 as part of the international PRICOV-19 study that explored the organization of general practices during COVID-19 in 38 countries to guarantee safe, effective, patient-centered, and equitable care. Well-being was evaluated by the Mayo Clinic's expanded 9-item well-being index.
Results
The findings of this study reveal notable regional discrepancies in the degree of well-being experienced by Belgian GPs, with the Walloon region displaying the lowest level of well-being (37%) in a population highly susceptible to professional distress (57%). Among the key stressors contributing to such distress, financial difficulties among patients (p < 0.011), the fee-for-service payment system (p = 0.013), a lack of work-related purpose (p = 0.047), and inadequate work-life balance (p < 0.001) were identified as significant factors. When examining the influence of regional disparities, it was found that the sole significant interaction between work-related stressors and region regarding the probability of experiencing distress was related to the possibility of workload sharing among practice personnel.
Conclusion
The findings from this study underscore the imperative for more comprehensive research aimed at scrutinizing the differences in well-being across the three regions in Belgium and identifying the systemic factors that influence the practice environment, as opposed to exclusively concentrating on enhancing individual resilience.
Similar content being viewed by others
Background
The COVID-19 pandemic has precipitated an unparalleled global health crisis, severely challenging the resilience of health systems and professionals worldwide. In the face of this crisis, healthcare workers have been exposed to heightened risks of infection, increased psychological stress due to potential virus transmission to family and patients, and a significant surge in workloads [1]. These challenges have amplified the risk of burnout among healthcare professionals [1,2,3,4,5], including General Practitioners (GPs) – a group already vulnerable to burnout before the pandemic [2, 5, 6].
The pandemic has not only stressed the healthcare system but also necessitated a rapid and innovative reorganization of primary healthcare services [7, 8]. GPs, as key primary care providers, found themselves at the forefront of this transformative period [9, 10]. They navigated a complex landscape, simultaneously addressing acute COVID-19 cases and regular healthcare duties [11,12,13,14]. They rapidly adapted to evolving patient needs, integrated telemedicine, and upheld strict infection control standards [11,12,13,14,15]. Additionally, GPs constantly updated their practices based on changing guidelines [11] and served as key informers for patients about evolving public health directives [16].
Although many countries faced common challenges during the COVID-19 pandemic [17], the crisis also highlighted the influence of regional factors, including demographics, socio-economic disparities, and healthcare systems [18], particularly in federal states such as Belgium [19,20,21,22]. Belgium's healthcare governance, with responsibilities split between federal and federated authorities, provides a unique case study of this dynamic interplay [20,21,22]. In this structure, the regional governments of Wallonia, Brussels-Capital, and Flanders are responsible for managing primary healthcare. However, in response to the pandemic, the federal government adopted a more centralized approach, focusing on the development of comprehensive guidelines, such as social distancing, mask-wearing, testing protocols, and COVID-19 vaccine procurement and distribution strategies. Yet, the implementation of these guidelines and strategies varied greatly from region to region, leading to differences in their effectiveness [21, 23, 24]. By 2021, at the time of the survey, Belgium had experienced three waves of COVID-19 and was in its initial vaccination phase [25, 26]. During the resurgence of cases in early 2021, social distancing measures were implemented divergently across regions, leading to disparities such as varying curfew hours in Brussels-Capital, Flanders, and Wallonia [21, 23, 24]. In terms of vaccination, Brussels-Capital had the lowest rate, with 78% of adults fully vaccinated, far behind Flanders (93%) and Wallonia (88%) [26]. This situation necessitated the implementation of customized local vaccination programs, considering the unique urban and multicultural characteristics of Brussels, which differ from the broader regional landscapes of Flanders and Wallonia, encompassing both urban centers and rural areas [20, 21]. Another noteworthy example is the consistently higher COVID-19 standardized mortality rate throughout the crisis in Brussels-Capital [25]. This multifaceted landscape of regional differences in healthcare responses underlines the imperative of incorporating regional differences when assessing the impact of public health crises [20, 21].
Despite the significance of these regional variations, no studies have compared the well-being of GPs across Belgium's three regions, especially considering the substantial changes in healthcare organizations. Furthermore, in Belgium, few studies have explored the impact of the pandemic on the mental health and well-being of GPs, who serve as foundational providers of patient-centered healthcare services. This study aims to investigate the impact of systemic work-related stressors on the level of well-being of GPs in Belgium during the pandemic, with a particular emphasis on identifying regional variations between Flanders, Wallonia, and Brussels-Capital.
Material and method
Study design and setting
This study is part of the PRICOV-19 project, a multi-country cross-sectional study headed by Ghent University, Belgium [27]. PRICOV-19 aims to evaluate to comprehensively evaluate the organization of primary care focusing on the continuity of high-quality care, changes in task roles, the impact on the well-being of health workers, and variations across different practice types and health systems. The study design and data handling protocol are described in the Data Management Plan registered at Ghent University [27]. Data were collected in 37 European countries and Israel. In Belgium, the study was inclusive of all three regions: the Dutch-speaking Flemish Region (FL), the bilingual Brussels-Capital Region (BR), and the French-speaking Walloon Region (WL).
Questionnaire development and data collection
Data collection was conducted through an online self-reported questionnaire among GP practices using the Research Electronic Data Capture platform (REDCap), which facilitated questionnaire hosting, distribution of invitations, and secure storage of participant responses [28]. The questionnaire was initially developed in English at Ghent University and included a pilot study with 159 GP practices in Flanders, Belgium. To address Belgium's multilingual context, it was translated into French and Dutch using a validated forward–backward method, ensuring the translations faithfully captured the nuances of the original English version, including the eWBI questions [27].
The questionnaire studied fifty-three items divided into six categories: (a) infection prevention; (b) patient flow for COVID-19 and non-COVID19 care; (c) dealing with new knowledge and protocols; (d) communication with patients; (e) collaboration within the practice and outside the practice; (f) characteristics of the respondent and the practice; and (g) well-being of the respondent. Well-being was evaluated by the Mayo Clinic expanded 9-item Well-being Index (eWBI).
Well-being assessment using the eWBI
The eWBI (Table 1) assesses distress across various dimensions including fatigue, feelings of burnout, low overall quality of life, suicidal ideation, meaning at work, and work-life balance. Participants respond to seven items with 'yes' (assigned 1 point) or 'no' (0 points). The remaining two items use a 7-point or 5-point Likert scale. For these, selecting 'strongly disagree' or 'disagree' adds a point, while 'agree' or 'strongly agree' subtracts a point. Neutral responses do not affect the score. A cumulative score of 2 or more indicates a risk of distress. This threshold is based on empirical evidence and statistical analysis, showing a significant correlation between specific score levels and increased risk of distress or mental health issues [29].
GP sampling and recruitment process
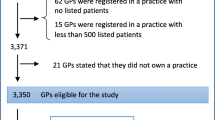
GPs were selected using a predefined recruitment procedure, with a preference for random selection according to the PRICOV-19 protocol [27]. A random sample of 1,477 Belgian GP practices was chosen from an updated listing on the INAMI/RIZIV web application, which included active GPs as of November 2020 [30]. Exclusion criteria for GPs included having qualified before 1980, being retired, or having low activity. Only one survey was conducted per GP practice. All selected GPs were contacted by phone, following a standardized procedure, to review their eligibility criteria and invite them to participate. This initial contact resulted in the participation of 370 GPs (participation rate of 25.1%). In addition, a convenience sample of 134 GPs was included through the networks of the research teams involved in the study. The total participation for the convenience sample study was 109 (participation rate of 81.3%). Data collection occurred between December 2020 and August 2021.
Data analysis and variables selection
Statistical analysis was performed on Belgian data using SPSS software version 27.0 for Windows (IBM Corp., Armonk, N.Y., USA). Data were analyzed using a stepwise approach (Fig. 1). Initially, the fifty-three items, serving as predictor variables, were classified into eight categories: practice population profile, patient's follow-up, workload management, adjustment in practice, practice characteristics, health care role, personal factors, and regulatory environment. This categorization was inspired from the National Academy of Medicine (NAM) conceptual model of factors affecting clinician well-being [31].
The second step identified and addressed potential multicollinearity. This involved examining the variables for co-dependence or high correlation, using the Chi-Square test to assess potential correlations within each category.
The third step involved selecting the most representative variable from correlated pairs. This selection was based on empirical evidence in the literature and the expertise of our research team, ensuring the most pertinent variables were included in our analysis.
Twenty-two independent variables (Table 2) out of fifty-three variables were selected for the binary regression analysis. The covariates scored on a Likert scale were continuous covariates and the others were categorical covariates.
These twenty-two independent predicting variables were included in the binary logistic regression independently of the category in which they were classified. The outcome variable in this study is the risk of being in distress, which is determined by a cumulative score of 2 or more on the 9-item Mayo Clinic (eWBI score ≥ 2.0) [29].
A binary logistic regression was performed to examine which variables were correlated to being at risk for distress. To explore the possible impact of the region on the effect of the predictor variables, potential interactions were incorporated into the regression and interactions were removed from the model one at a time (Table 3). Non-significant interactions were eliminated, so that any interaction terms making a statistically significant contribution to the interpretation of our model was identified. The results were considered significant at the 5% uncertainty level.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki. The Research Ethics Committee of Ghent University Hospital approved the protocol of the PRICOV-19 study (BC-07617). All participants gave their informed consent online.
Results
Description of the respondent sample
The number of respondents, 479 practices, was distributed among the regions as follows: 47 in BR (9.8%), 280 in FL (58.5%) and 152 in WL (31.7%) (Table 4). About two-fifths of the respondents (37.3%) were working in solo practices. In FL, the practices were more often duo or group practices compared to WL and BR (p < 0.001). GPs working in multidisciplinary practices were significantly higher in FL than in WL or BR (p = 0.016). Most of the respondent practices worked on a fee-for-service basis (91.0%). The payment system was not significantly different between the regions (p = 0.066). Regarding territorial location, 52.0% of the respondents were based in city-suburbs, 39.6% in mixed urban–rural areas, and only 8.4% in rural areas. Regarding the professional experience of GPs, 38.9% had less than 10 years of experience, 12.4% had 10 to 19 years of experience, 17.2% had 20 to 29 years of experience, and 31.3% had over 30 years of experience.
The eWBI reveals differences in well-being across regions, as illustrated in Fig. 2. While over half of the respondents (57.0%) were identified as being at risk of mental distress in the total Belgian sample, a significant difference was observed between regions. Specifically, the WL region reported a substantially higher rate of distress (72.9%) compared to the FL and BR regions, as indicated by the statistical significance (p < 0.001) presented in Table 5.
Factors predicting the level of well-being
Regarding the factors related to the level of well-being, none of the factors of the categories of workload management, regulatory environment, patients' follow-up, and adjustments in practice had a significant impact on the eWBI of Belgian GPs after controlling for all other variables in the binary logistic regression model. However, some of the items in the four other categories significantly influenced the risk of being at distress (Table 6).
Practice characteristics
Practice location (urban, suburban, rural, and mixed urban–rural) was not a factor that had a significant impact on eWBI. However, the region of the practice had an impact: a GP in BR had a higher probability of being at risk than a GP in FL (p = 0.047), while there was no significant difference in the probability of being at risk of distress between WL and FL. The payment system was also identified as a significant stressor. GPs working in a fee-for-service system had a higher probability of being at risk than those working in a capitation system. Multidisciplinary practice, being a training, and having sufficient protected time to review the new guidelines were not associated with a significant impact on the likelihood of being at risk for distress.
Practice population profile
Compared to the GPs who had the perception of treating a greater number of patients with financial problems compared to the average PC practice, those who had not this impression and treated an "equal" or "lower" number of patients with financial problems compared to the average PC practice had a lower probability (p = 0.011) of being at risk of distress (all other things being equal). There was no significant difference regarding the perception of treating patients with a chronic condition compared to the average PC practice.
Healthcare role
When GPs had to face increased responsibilities during the pandemic, this did not increase the probability of being at risk for distress (p = 0.056). The same observation applies to the need for further training for coping with amended responsibilities (p = 0.178). Nevertheless, high meaningfulness of work seemed to decrease the probability of being at risk for distress (p = 0.047).
Personal and professional life balance
A work schedule leaving enough time for family/personal time significantly decreased the probability of being at risk for distress (p < 0.001).
Region
The only significant interaction between work-stress-related factors and the region on the probability of being at risk of distress was the workload distribution between staff members in the practice. This effect was significantly lower in BR than in FL (p = 0.006), while there was no significant difference between WL and FL.
Discussion
The primary aim of this study was to investigate the impact of systemic work-related stressors on the well-being of GPs in Belgium during the pandemic, with a particular focus on identifying regional variations between Flanders, Wallonia, and Brussels-Capital. This research addresses a significant gap, given the scarcity of studies examining the pandemic's impact on the mental health of GPs in Belgium, especially against the backdrop of substantial changes in healthcare organizations.
The expanded 9-item Well-being Index (eWBI) was employed to assess well-being and distress, utilizing a specific score threshold (eWBI score ≥ 2.0) to identify GPs at risk of distress. This comprehensive approach aimed to cover various aspects of well-being, such as severe fatigue, suicidal ideation, feelings of burnout, quality of life, meaning at work, and work-life. By using the eWBI, the study provided a broader perspective on the well-being of GPs during the pandemic, moving beyond traditional measures like burnout alone. The use of the aggregate score (eWBI score ≥ 2.0) offered a holistic view of well-being, enabling standardized evaluation and cross-regional comparisons of individuals or populations [29, 32].
According to the study's findings, 57% of the Belgian GPs were considered at risk of professional distress during the period of December 2020 to August 2021. These results align with the PRICOV-19 study, indicating that 64% of European GPs were at risk of professional distress during the same period [32]. The study also showed that GPs with less experience, working in smaller practices, and treating more vulnerable populations, especially those caring for patients with financial difficulties, were particularly susceptible to distress [32].
In Belgium, key occupational factors negatively influencing GPs’ well-being included having more than average number of patients with financial problems, working on a fee-for-service basis compared to capitation. In contrast, finding meaning in work and having a good work-life balance were protective factors against overall distress. In 2021, the digital divide in Belgium was around 39%, a figure above the European average (34%), with only 53% of low-income households owning a laptop [33]. During the pandemic, the computerization of health care with increased use of tele- and video-consultations has thus excluded some patients from care, and those with a financial precarious background were particularly hit [34]. The difficulty in accessing care has made it more difficult for GPs to manage patients with the low income [35], a population showing a 38% higher use of GP homecare services compared to the highest income group before the health crisis in Belgium [33]. Several studies have also shown that GPs with a high share of patients with low incomes face more difficulties in managing their patients’ care because of their low health literacy, higher disease burden, increased health risks, and intertwined social determinants of health [36, 37]. It has also been reported that GPs working with low-income patients are exposed to a higher risk of burnout compared to GPs with a higher share of patients with high incomes [35,36,37]. The financial aspect of a GP’s patient base affects not only the health of the patient but also the well-being of the caregiver.
Among the other practice characteristics with an impact on Belgian GPs’ well-being was the payment system. Our data showed that Belgian GPs who are paid retrospectively based on activity with a fee-for-service system were at higher risk of distress compared to GPs who are paid prospectively with the capitation system. This could be explained by the fact that, during the pandemic waves, most of the consultations were done remotely. In March 2020, around 70% of the consultations were done by teleconsultations in Belgium [38]. In several countries, it has been shown that the increase in teleconsultations was correlated with a decrease in GPs’ incomes especially in the GPs’ population working with the fee-for-service system [34, 39, 40]. Furthermore, when patients came back to practice, consultation required increased treatment preparedness leading to a decrease in the number of consultations and thus of income, and increased material expenditures, such as reorganizing practice, securing supplies, and buying protective materials, leading to additional spending [40]. In this study, GPs’ sample was mainly composed of GPs working on a fee-for-service-basis (91%). This could have had an impact on the data. However, our sample of GPs reflects the situation of physicians in Belgium, as GPs are mainly self-employed and paid for fee-for-service as reported by the FPS [41]. Furthermore, some studies highlighted an increased vulnerability to the risk of burnout among GPs working on a fee-for-service regiment, well before the pandemic [42]. Also, the capitation funding is recognized as allowing more time for meetings, coordination activities, and peer-to-peer collaboration than is possible with the fee-for-service [43]. Remuneration on a fee-for-service basis appears thus as a stressor in a period of pandemic.
The two individual factors that stand out the most from this study as having a significant impact on the level of well-being of GPs are protective factors: the meaning given to work and the fact of having a good work-life balance. The notion of meaning echoes the usefulness found in the function and responsibility that the job confers [44, 45]. A study by Shanafelt found that physicians who spend less than 20% of their professional time on the activity they consider most important are three times more likely to be burnt out than those who spend at least 20% of their professional effort on this activity [46]. A recent study focusing on GP trainees during the COVID-19 crisis showed that to have meaning in work was a key factor in preventing burnout [47]. Maintaining a mentally healthy workforce to ensure quality of care and patient safety in a period of high pressure may therefore depend, among other factors, on a workforce that is able to continue to find values in their work, despite the many changes introduced by the crisis, and to maintain a good balance between their work and private life [48, 49].
When analyzing the data at the regional level, a difference in GPs' level of well-being was observed between the three Belgian regions, with more than two-thirds of Walloon respondents classified as at risk of distress, whereas, for Flemish and Brussels respondents, this proportion was 49% and 54% respectively. One explanation for this difference between regions could have been linked to the differences in primary care organization between regions. In the French-speaking part of Belgium, the primary healthcare system lacks the same level of organization seen in Flanders [23, 50]. This structural difference had notable implications during the COVID-19 pandemic. Unlike Flanders, which adopted a more structured approach with primary care zones and well-defined roles for healthcare professionals [23, 50], Wallonia struggled to coordinate its pandemic response at the local level [20, 22, 23, 50]. This resulted in scattered efforts and a heavier reliance on GPs for testing and triage, potentially causing uneven responses and less effective pandemic management in Wallonia compared to Flanders [20, 50].
When attempting to identify the effect of the region on the impact of stressors or protective factors on GPs’ well-being, the only significant interaction on the probability of being at risk for distress was the workload distribution between staff members in the practice. While several studies have shown that teamwork and group cohesion are protective factors against burnout [17, 51], the results of this study did not confirm this observation. While the Flemish GP sample had the highest percentage of group practices (55%) and the Walloon sample the lowest percentage (22%), there was no significant difference in the protective effect of workload sharing within a practice between WL and FL. In contrast, workload sharing within a practice had a weaker protective effect on GP well-being in BR compared with FL. Thus, region was not explanatory on its own. In 2011, a review of the literature had already highlighted a large disparity between French- and Flemish-speaking regions, with French-speaking GPs being more dissatisfied with their profession overall and more exposed to the risk of emotional exhaustion [52]. The low level of professional well-being of French-speaking physicians may therefore reflect a pre-existing condition that predates the Covid-19 crisis.
Strengths and limitations
One of the strengths of the study is the use of a validated instrument for data collection.
The data shows that the GPs in our sample are distributed similarly to the overall distribution of GPs in Belgium according to the IMA-AIM Atlas 2021. For instance, in our study, 9.8% of GPs are from Brussels-Capital, 58.5% from Flanders, and 31.7% from Wallonia, which closely matches the IMA-AIM 2021 statistics that report 10.0% of GPs in Brussels-Capital, 58.0% in Flanders, and 32.0% in Wallonia [53].
Compared to the other participating countries, the Belgian response rates were slightly higher than the overall median value of 22.0% in PRICOV-19. However, some limitations should be noted. The participation to this study was entirely voluntary, which comes with a risk of self-selection bias and a rather small sample size. GP practices having a particular interest in the three main subject of this study (organization of care, quality of care and well-being during the pandemic) could have mainly participated.
Data were collected between December 2020 and Augustus 2021. This large period includes three waves of the COVID-19 pandemic in Belgium. This means that the exact time the questionnaire was answered might have affected the results and perception of the respondent towards the situation.
There are no studies in Belgium that address professional well-being in GPs and factors that might contribute to burnout. It is therefore difficult to assess whether the factors reported as having a significant effect on GPs' well-being were related to this extraordinary situation or whether they highlighted pre-existing weak links in the organisation of care.
The study's design did not allow to conduct sub-analyses based on the prevalence of COVID-19. Data collection spanned from December 2020 to August 2021, a period marked by significant changes in the COVID-19 situation. This evolving context made it challenging to perform meaningful sub-analyses at specific time points. A robust sub-analysis would require a large, consistent sample size at each time interval, a criterion difficult to fulfill given the challenges in recruiting and retaining GP participation.
Conclusion
This study offers an insight into the well-being of GPs in Belgium during the December 2020 to August 2021 period amid the COVID-19 pandemic. It sheds light on the challenges faced by Belgian GPs, with 57% of them at risk of professional distress, aligning with trends observed in other European regions, as demonstrated in the PRICOV-19 study. These findings emphasize significant stressors, including the perception of having patient facing financial struggles and the prevailing fee-for-service payment model. The study also uncovers the protective factors contributing to the well-being of GPs, including finding meaning in their work and achieving a healthy work-life balance.
Although a significant difference in the level of well-being was observed among regions, with Wallonia displaying the highest level of GPs at risk of distress, the region alone does not fully explain this difference. This suggests that pre-existing factors may contribute to the well-being disparities that existed before the COVID-19 crisis.
These findings underscore the importance of constructive collaboration between stakeholders on the ground and relevant authorities to develop customized action plans tailored to the organizational specificities of each region in Belgium. Such a collaborative approach is crucial for improving the situation and promoting the well-being of GPs in the country.
Availability of data and materials
The anonymized data is held at Ghent University and all raw data that could lead to the identification of the respondents were permanently removed. Reasonable request is required to access non-identifiable data by users who are external to the research teams involved. Access will be subject to a data transfer agreement and following approval from the principal investigator of the study.
Abbreviations
- GP:
-
General practitioner
- GP practice:
-
General practice
- PRICOV-19:
-
Quality and safety in PRImary care in times of COVid-19
- BCR:
-
Brussels-capital region
- FR:
-
Flemish region
- WR:
-
Walloon region
References
De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz S-A, Ellis L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. Available from: https://doi.org/10.1186/s12889-020-10070-3.
Karuna C, Palmer V, Scott A, Gunn J. Prevalence of burnout among GPs: a systematic review and meta-analysis. Br J Gen Pract. 2022;72(718):e316-24. Available from: https://doi.org/10.3399/BJGP.2021.0441.
Freeborn DK. Satisfaction, commitment, and psychological well-being among HMO physicians. West J Med. 2001;174(1):13–8. Available from: https://doi.org/10.1136/ewjm.174.1.13.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–81. Available from: https://doi.org/10.1016/S0140-6736(16)31279-X.
Shanafelt TD. Physician well-being 2.0: Where are we and where are we going? Mayo Clin Proc. 2021;96(10):2682–93. Available fromhttps://doi.org/10.1016/j.mayocp.2021.06.005.
Le Burnout des médecins généralistes : prévention et prise en charge. Fgov.be. Available from: https://kce.fgov.be/fr/publications/tous-les-rapports/le-burnout-des-medecins-generalistes-prevention-et-prise-en-charge. Accessed 7 Nov 2023.
Groenewegen P, Van Poel E, Spreeuwenberg P, Batenburg R, Mallen C, Murauskiene L, et al. Has the COVID-19 pandemic led to changes in the tasks of the primary care workforce? An international survey among general practices in 38 countries (PRICOV-19). Int J Environ Res Public Health. 2022;19(22):15329. Available from: https://doi.org/10.3390/ijerph192215329.
Belche JL, Joly L, Crismer A, Giet D et al. Résilience et réactivité de la médecine générale durant la pandémie COVID-19. Revue Méd de Liège. 2020;75(S1). Available from: https://orbi.uliege.be/bitstream/2268/259412/1/2020S1_05%281%29.
Khan N, Jones D, Grice A, Alderson S, Bradley S, Carder P, et al. A brave new world: the new normal for general practice after the COVID-19 pandemic. BJGP Open. 2020;4(3):bjgpopen20X101103. Available from: https://doi.org/10.3399/bjgpopen20x101103.
Thornton J. Covid-19: how coronavirus will change the face of general practice forever. BMJ. 2020;368:m1279. Available from: https://doi.org/10.1136/bmj.m1279.
Chen FM. COVID-19 and family doctors. Fam Med. 2020;52(4):306–7. Available from: https://doi.org/10.22454/FamMed.2020.515917.
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582.
Wanat M, Hoste M, Gobat N, Anastasaki M, Böhmer F, Chlabicz S, et al. Transformation of primary care during the COVID-19 pandemic: experiences of healthcare professionals in eight European countries. Br J Gen Pract. 2021;71(709):e634-42. Available from: https://doi.org/10.3399/BJGP.2020.1112.
Tsopra R, Frappe P, Streit S, Neves AL, Honkoop PJ, Espinosa-Gonzalez AB, et al. Reorganisation of GP surgeries during the COVID-19 outbreak: analysis of guidelines from 15 countries. BMC Fam Pract. 2021;22(1):96. Available from: https://doi.org/10.1186/s12875-021-01413-z.
Li E, Tsopra R, Jimenez G, Serafini A, Gusso G, Lingner H, et al. General practitioners’ perceptions of using virtual primary care during the COVID-19 pandemic: An international cross-sectional survey study. PLOS Digit Health. 2022;1(5):0000029. Available from: https://doi.org/10.1371/journal.pdig.0000029.
Amara PS, Platt JE, Raj M, Nong P. Learning about COVID-19: sources of information, public trust, and contact tracing during the pandemic. BMC Public Health. 2022;22(1):1348. Available from: https://doi.org/10.1186/s12889-022-13731-7.
Jefferson L, Heathcote C, Bloor K. General practitioner well-being during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2023;13(2):e061531. Available from: https://doi.org/10.1136/bmjopen-2022-061531.
Oecd.org. Policy responses to Coronavirus (COVID-19). The territorial impact of COVID-19: Managing the crisis and recovery across levels of government. Available from: https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/. Accessed 7 Feb 2023.
Unruh L, Allin S, Marchildon G, Burke S, Barry S, Siersbaek R, et al. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. 2022;126(5):427–37. Available from: https://doi.org/10.1016/j.healthpol.2021.06.012.
Bursens P, Popelier P, Meier P. Belgium’s response to COVID-19. In: Federalism and the Response to COVID-19. 1st ed. London: Routledge India; 2021. p. 39–48.
Bursens P, Popelier P, Verhoest K. Belgium: Cooperation Out of Necessity and Confirmation of Executive Dominance. In Governments’ Responses to the Covid-19 Pandemic in Europe 2023;387–396. Springer International Publishing. Available from: https://doi.org/10.1007/978-3-031-14145-4_32.
Luyten J, Schokkaert E. Belgium’s response to the COVID-19 pandemic. Health Econ Policy Law. 2022;17(1):37–47 (https://pubmed.ncbi.nlm.nih.gov/34219632/).
Levy M, Annemans L. Sustainability and Resilience in the Belgian Health System. 2023.
Molenberghs G. Biostatistics and the COVID-19 pandemic in Belgium, in 2020 and 2021. Statsoc. 2022;(10 | 2):31–44. Available from: https://journals.openedition.org/statsoc/482.
Jurcevic. Epidemiology of COVID-19 mortality in Belgium from wave 1 to wave 7 (March 2020–11 September 2022). sciensano.be. 2023. Available from: https://www.sciensano.be/en/biblio/epidemiology-covid-19-mortality-belgium-wave-1-wave-7-march-2020-11-september-2022.
Peeters I, Vermeulen M, Bustos N, Renard F, Van Der Heyden J, Scohy A, et al. Couverture vaccinale et impact épidémiologique de la campagne de vaccination Covid-19 en Belgique. Sciensano.be. Available from: https://covid-19.sciensano.be/sites/default/files/Covid19/COVID-19_THEMATIC_REPORT_VaccineCoverageAndImpactReport_FR.pdf. Accessed 20 Jan 2024.
Van Poel E, Vanden Bussche P, Klemenc-Ketis Z, Willems S. How did general practices organize care during the COVID-19 pandemic: the protocol of the cross-sectional PRICOV-19 study in 38 countries. BMC Prim Care. 2022;23(1). Available from: https://doi.org/10.1186/s12875-021-01587-6.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95(103208):103208. Available from: https://doi.org/10.1016/j.jbi.2019.103208.
Dyrbye LN, Satele D, Shanafelt T. Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. J Occup Environ Med. 2016;58(8):810–7. Available from: https://www.jstor.org/stable/48500991.
RIZIV - zoeken. Fgov.be. Available from: https://webappsa.riziv-inami.fgov.be/silverpages/. Accessed 20 Jan 2024.
Brigham T, Accreditations Council for Graduate Medical Education, Barden C, Legreid Dopp A, Hengerer A, Kaplan J, et al. A journey to construct an all-encompassing conceptual model of factors affecting clinician well-being and resilience. NAM Perspect. 2018;8(1). Available from: https://doi.org/10.31478/201801b.
Collins C, Clays E, Van Poel E, Cholewa J, Tripkovic K, Nessler K, et al. Distress and wellbeing among general practitioners in 33 countries during COVID-19: Results from the cross-sectional PRICOV-19 study to inform health system interventions. Int J Environ Res Public Health. 2022;19(9):5675. Available from: https://doi.org/10.3390/ijerph19095675.
Baromètre Inclusion Numérique 2022. Koning Boudewijnstichting. Available from: https://kbs-frb.be/fr/barometre-inclusion-numerique-2022. Accessed 24 Jan 2024.
Homeniuk R, Collins C. How COVID-19 has affected general practice consultations and income: general practitioner cross-sectional population survey evidence from Ireland. BMJ Open. 2021;11(4):e044685. Available from: https://doi.org/10.1136/bmjopen-2020-044685.
Carde E. When social inequalities produce “difficult patients”: A qualitative exploration of physicians’ views. SAGE Open. 2019;9(4):215824401989428. Available from: https://doi.org/10.1177/2158244019894280.
Flye Sainte Marie C, Querrioux I, Baumann C, Di Patrizio P. Difficultés des médecins généralistes dans la prise en charge de leurs patients précaires. Sante Publique. 2015;27(5):679–90. Available from: https://doi.org/10.3917/spub.155.0679.
Pedersen AF, Vedsted P. Understanding the inverse care law: a register and survey-based study of patient deprivation and burnout in general practice. Int J Equity Health. 2014;13(1). Available from: https://doi.org/10.1186/s12939-014-0121-3.
Vaes B, Vos B, Foidart M, De Schreye R, Schrans D, Philips H, et al. Burden of COVID-19 on primary care in Belgium: a prospective nationwide observational study from March to August 2020. Arch Public Health. 2022;80(1). Available from: https://doi.org/10.1186/s13690-022-01003-0.
COVID-19 pandemic analyses. Who.int. Available from: https://eurohealthobservatory.who.int/monitors/hsrm/analyses/hsrm/compensating-healthcare-professionals-for-income-losses-and-extra-expenses-during-covid-19. Accessed 23 Jan 2024.
Europe: Compensating healthcare professionals for income losses and extra expenses. Issa.int. Available from: https://iskm.issa.int/node/14065. Cited 2024 Jan 20.
plancad_medecin_2004–2016_fr_1.pdfz. Santé Publique. Available from: https://organesdeconcertation.sante.belgique.be/fr/file/plancadmedecin2004-2016fr1pdf. Accessed 20 Jan 2024.
Goroll AH. Addressing burnout—focus on systems, not resilience. JAMA Netw Open. 2020;3(7):e209514. Available from: https://doi.org/10.1001/jamanetworkopen.2020.9514.
Karam M, Macq J, Duchesnes C, Crismer A, Belche J-L. Interprofessional collaboration between general practitioners and primary care nurses in Belgium: a participatory action research. J Interprof Care. 2022;36(3):380–9. Available fromhttps://doi.org/10.1080/13561820.2021.1929878.
Pignault A, Houssemand C. What factors contribute to the meaning of work? A validation of Morin’s Meaning of Work Questionnaire. Psicologia. 2021;34(1). Available from: https://doi.org/10.1186/s41155-020-00167-4.
Shanafelt TD. Enhancing meaning in work: a prescription for preventing physician burnout and promoting patient-centered care: A prescription for preventing physician burnout and promoting patient-centered care. JAMA. 2009;302(12):1338–40. Available from: https://doi.org/10.1001/jama.2009.1.
Shanafelt TD, West CP, Sloan JA, Novotny PJ, Poland GA, Menaker R, et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990. Available from: https://doi.org/10.1001/archinternmed.2009.70.
Lepièce B, Lenoir A-L, de Rouffignac S. Vécu des internes en médecine générale lors de la crise sanitaire du COVID-19: répercussions sur l’anxiété et la motivation pour la médecine générale. Sante Publique. 2022;34(5):675–82. Available from: https://doi.org/10.3917/spub.225.0675.
Patel R, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A review. Behav Sci (Basel). 2018;8(11):98. Available from: https://doi.org/10.3390/bs8110098.
Keeton K, Fenner DE, Johnson TRB, Hayward RA. Predictors of physician career satisfaction, work–life balance, and burnout. Obstet Gynecol. 2007;109(4):949–55. Available from: https://doi.org/10.1097/01.aog.0000258299.45979.37.
Jamart H, Van Maele L, Ferguson M, Drielsma P, Macq J, Van Durme T. La première vague de Covid-19 en Belgique et les soins primaires. Rev Med Suisse. 2020;16(713):2119–22. Available from: https://www.revmed.ch/revue-medicale-suisse/2020/revue-medicale-suisse-713/la-premiere-vague-de-covid-19-en-belgique-et-les-soins-primaires). Cited 2023 Mar 3
Werdecker L, Esch T. Burnout, satisfaction and happiness among German general practitioners (GPs): A cross-sectional survey on health resources and stressors. PLoS One. 2021;16(6):e0253447. Available from: https://doi.org/10.1371/journal.pone.0253447.
Kacenelenbogen N, Offermans AM, Roland M. Burnout of general practitioners in Belgium: societal consequences and paths to solutions. Rev Med Brux. 2011;32(4):413–23. Available from: (https://pubmed.ncbi.nlm.nih.gov/22034774/). Cited 2023 Mar 3.
Atlas AIM. AIM-IMA. Available from: https://www.aim-ima.be/Atlas-AIM. Accessed 07 Nov 2022.
Acknowledgements
The authors wish to express their sincere gratitude to all the participating GP practices.
About this supplement
This article has been published as part of BMC Primary Care Volume 24 Supplement 1, 2023: COVID-19 and beyond – lessons for the future of primary care. The full contents of the supplement are available online at https://bmcprimcare.biomedcentral.com/articles/supplements/volume-24-supplement-1.
Funding
The PRICOV-19 study was set up in close collaboration with the 'European Society of Quality and Safety in Family Practice (EQuiP) and implemented without external funding except for a small grant from the 'European General Practice Research Network' (EGPRN). The funding received did not exert any influence over the study's design, nor did it impact the collection, analysis, and interpretation of data, the decision to publish, or the writing of the manuscript. This publication was funded by a grant from the Academic Center of General Medicine, UCLouvain, Brussels, Belgium.
Author information
Authors and Affiliations
Contributions
Study conception and design: E.V.P and S.W; Focus of the article and analysis approach: C.P, J.C., S.D.R., and M.D.J.; Data collection: C.P., E.V.P., and B.P; Analysis and interpretation: C.P, J.C., S.D.R., and M.D.J.; Writing draft manuscript: J.C. and C.P.; Review and approval: C.P., S.D.R., B.P., E.V.P., S.W., and M.D.J.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki. The Research Ethics Committee of Ghent University Hospital approved the protocol of the PRICOV-19 study and Belgian data collection (BC-07617). Research Ethics Committees in the different partner countries gave additional approval if needed.
Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cholewa, J., Ponsar, C., de Rouffignac, S. et al. General practitioners’ well-being in Belgium: results from the cross-sectional PRICOV-19 study. BMC Prim. Care 24 (Suppl 1), 284 (2023). https://doi.org/10.1186/s12875-024-02341-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02341-4