Abstract
Background
Hypertension is one of the global public health problems. Family physician-contracted service (FPCS) is widely used in the health management of hypertension patients in China. The purpose of this study was to assess the effect of FPCS on hypertension control.
Methods
PubMed, Web of Science, the Cochrane Library, China National Knowledge Network, Chinese Scientific and Technological Journal Database (CQVIP), and Wanfang Database were searched for randomized controlled trials related to family physician-contracted service and hypertension control effect, and meta-analysis was performed on the literature meeting the inclusion criteria. The source of heterogeneity was discovered by meta-regression, and it was further investigated by subgroup analysis. The risk difference (RD) and 95% confidence interval (CI) were utilized as effect values. Evaluations of publication bias and sensitivity analysis were also conducted.
Results
A total of 46 studies were included, and the pooled RD suggested that FPCS could effectively improve the control rate by 19% (RD = 0.19; 95%CI: 0.16–0.21; P < 0.001; I2 = 59.3%). The average age (β = 0.28; P = 0.05) and the intervention mode (β = 0.36; P < 0.001) were found to be heterogeneous sources by the meta-regression. According to subgroup analysis, the hypertension control rates of the elderly and working-age population in the experimental group were 93.6% and 90.1%, respectively; the control rates of the “family physician” mode (FP), “family physician + patient” mode (FPP) and “family physician + patient + family member” mode (FPPF) in the experimental group were 90.1%, 94.4%, and 92.6%, respectively. The sensitivity analysis revealed steady results, with no discernible publication bias.
Conclusions
The FPCS is beneficial to the control of hypertension. The control effect is influenced by average age and intervention mode. The control effect of hypertension in the elderly is better than that in the working-age population, and FPP and FPPF are more beneficial to the management of hypertension than FP. The quality and continuity of FPCS should receive more focus in the future, patient self-management and family support are also essential for managing hypertension.
Similar content being viewed by others
Introduction
Hypertension is the most common risk factor for cardiovascular diseases, which is usually defined as systolic blood pressure (SBP) ≥ 140mmHg or diastolic blood pressure (DBP) ≥ 90mmHg when blood pressure is measured three times on different days without antihypertensive drugs. There isn’t a fully curative treatment for it at the moment due to its very complex pathophysiology and contributing elements [1]. An estimated 1.28 billion adults globally, aged 3–79, had a diagnosis of hypertension as of 2019, accounting for roughly 32–34% of the world’s population [2]. About 330 million people in China are thought to have cardiovascular disease (CVD), of which 245 million have hypertension [3]. With the aggravation of global aging, the disease burden caused by hypertension has become a noteworthy public health problem in China and even in the international community.
In practice, the prevention and treatment of hypertension in China have achieved remarkable results in the past 20 years [4]. To address the unbalanced distribution of medical resources, and to gradually meet the needs of continuous and comprehensive medical services for hypertension patients, China began to advocate for hypertension prevention and treatment to be placed in the community around 2000 [5]. The first standard of hypertension prevention and control in primary care was issued in 2002, which promoted hypertension management technology in primary care, emphasized community-wide prevention and control, and focused on chronic disease risk factors [6]. The standardized management of hypertension has been incorporated into the national basic public health service project since the new health care reform was implemented in 2009. This means that community health service centers, township health centers, and other primary medical institutions must strictly adhere to the “National Basic Public Health Service Standard” for the management of hypertension patients within their jurisdictions [4]. Establishing paper and electronic health records, giving at least four face-to-face follow-up services each year, testing blood pressure for patients free of charge, and providing health education and lifestyle advising services for patients free of charge are all part of the management [7]. Additionally, when updates are made to the National Basic Public Health Service Standards, the standardized management will be enhanced over time.
According to a study conducted between 2012 and 2015, China’s population now has a 15% rate of hypertension under control, which is 9% higher than it was in 2002. Effective control of hypertension has been accomplished through the National Basic Public Health Service Project. However, international experience shows that only when the control rate of high blood pressure among the population is ≥ 30%, can the incidence rate and mortality of cardiovascular disease among the population be reduced [8]. Research has indicated that the relative dearth of medical resources in the community, the low quality of treatment, and some residents’ low self-care awareness all have an impact on the effectiveness of community management of chronic diseases [9, 10]. There is still a long way to go for community management of hypertension in China.
Apart from the persistently alarming epidemic situation of chronic non-communicable diseases, China’s medical system is still beset by issues like unequal resource allocation, exorbitant medical expenses, and severe service fragmentation. A “panacea” was created in the form of the FPCS. The State Council proposed that family physician services (FPCS) be the future path of health services development in China in its “Notice on Issuing the Guidance on Promoting the Signing of Family Physician Services” [11]. The exploration of Chinese-style FPCS officially kicked off. FPCS is a personalized medical service provided by family physicians after residents sign a service agreement with grassroots medical institutions for some time. This type of full-cycle, whole-population health management service is better suited for managing hypertension over the long term. It can assist contracted residents in adopting healthy lifestyles, exploring the workings of the hierarchical medical system, and gradually achieving the goal of obtaining greater health output with less health input [12].
Based on continuous practice and reference to international chronic disease management, China has gradually formed several representative FPCS models, as follows: (1) The “integrated Medical treatment and nursing care system” contracted service model in Hangzhou. The primary goals are to provide health management services that integrate medical treatment, pensions, and rehabilitation for insured people, as well as to integrate basic medical resources within the community [13]. (2) “1 + 1 + 1” contracted service model in Shanghai. Residents voluntarily select a family doctor from the community health service center, district, and municipal medical institutions to sign a contract, so that the above three levels of medical institutions can form an alliance and effectively manage patients in terms of medical treatment, referral, and medical insurance [14]. (3) The “co-management of three types of doctors” contracted service model in Xiamen. It refers to a management team comprised of a general practitioner, a health manager, and a specialty doctor who collaborate to complete the entire process of chronic disease management for patients [15]. These models do, however, still have certain common issues, such as a lack of family doctors, a shortage of resident service utilization, and inadequate information construction [16].
In light of the severe prevalence of hypertension, assessing FPCS’s efficacy is practically significant. Furthermore, the majority of studies on the impact of FPCS on the management of hypertension use experimental research using community members as case studies. These studies lack a systematic theoretical analysis framework and a thorough understanding of the variables impacting the efficiency of the services. Thus, the goal of this study is to ascertain the present state of hypertension management under FPCS and methodically assess its influencing factors.
Methods
Theoretical model
Dr. Anderson of the University of Chicago School of Public Health originally introduced the Behavioral Model of Health Services Use (BMHSU) in 1968, and this study is primarily based on it [17]. After five iterations and additions, the model—which was first used to examine the variables influencing family medical services utilization—has progressively grown to be regarded as a reliable framework for medical and health services research [18]. By incorporating multi-level elements impacting the rate of hypertension control into a relatively mature analysis framework, BMHSU can provide a more thorough explanation of the key traits of patients with hypertension and prevent the selection of influencing factors at random.
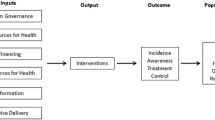
As seen in Fig. 1, this paper’s theoretical framework is divided into four Sect. (1) External environment. That is, the policy environment of FPCS is confronted by a rising number of chronic patients’ objective desire for long-term health treatment. (2) Individual characteristics. This may represent the effect of specific factors on the rate at which hypertension in patients is controlled. The following three aspects are mostly examined and discussed in this article: (a) Predisposing factors. They are defined as a tendency to use health services, which reflects people’s potential to use health services. Two factors, age, and region, were included in this study; (b)Enabling factors. They correspond to the availability of FPCS, which in this study is referred to as the experimental period, representing the length of time individuals have access to FPCS; (c) Need factors. People use medical services for a variety of reasons, the most common of which are personal health requirements. In this study, hypertension is the need factor. (3) Health behaviors. Primarily consist of the health service providers’ intervention strategies and the health service demanders’ use of FPCS. Intervention mode refers to different family physician contract service models, including the “Family physician” model (FP), the “Family physician + Patient” model (FPP), and the “Family physician + Patient + Family member” model (FPPF). (4) Outcome. The hypertension control rate is the most direct manifestation of the effectiveness of FPCS.
Search strategy
This report was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Supplementary Material 1). Literature on hypertension control rate under contracted family physician services published from the establishment of the database to January 14, 2023, were systematically searched. The search databases included PubMed, Web of Science, the Cochrane Library, China National Knowledge Infrastructure (CNKI), the Database of Chinese sci-tech periodicals (CQVIP), and the Wanfang Database. Terms and keywords used in the searches included the following: (“family physician” OR “family physician” OR “General practitioners”) AND (“hypertension” OR “high blood pressure”) AND (“control rate” OR “control ratio” OR “effective rate”) AND (“China” OR “Chinese”), the full search strategy was provided in Supplementary Material 2.
Criteria for included and excluded studies
Inclusion criteria
(a) Study subjects: hypertensive patients, and basic information such as sample size, age, and place of residence are explained; (b) Intervention measures: FPCS; (c) Study type: randomized controlled trial (RCT); (d) Outcome measures: hypertension control rate.
Excluded criteria
(a) Study subjects: non-hypertensive patients; (b) Intervention measures are not FPCS; (c) Study type: non-randomized controlled trial; (d) There is no clear definition of outcome indicators or lack of outcome indicators; (e) The sample size, age and other basic information of the study subjects are not stated; (f) Low-quality literature.
Literature screening and study data extraction
The pertinent information from the included literature was extracted based on the inclusion and exclusion criteria. This included the title, author, publication time, sample size, hypertension control rate, average age, gender ratio, region, experimental cycle, intervention measures, and other key information. The control rate of hypertension includes three definitions: First, \(control\ rate=(valid+average)/total\times 100\%\) (valid: blood pressure was maintained at a normal level (SBP/DBP≤140/90 mmHg) for 75% or 80% of the year; average: blood pressure was maintained at a normal level (SBP/DBP ≤ 140/90 mmHg) for more than half a year; invalid: blood pressure was maintained at an abnormal level for more than half a year). Second, \(control\ rate=(valid+average)/total\times 100\%\) (valid: after treatment, the patient’s blood pressure level decreased to a normal level, and the clinical symptoms of headache and dizziness disappeared; average: after treatment, the patient’s blood pressure level decreased but did not reach the normal level, the patient was accompanied by mild headache, dizziness, and other clinical symptoms; invalid: after treatment, the patient’s blood pressure level did not change significantly, and the patient’s clinical symptoms did not relieve). Third, the control rate represents blood pressure measured at the last follow-up visit at the normal level. Two reviewers conducted it independently and cross-checked it to complete the literature screening and data extraction. Disparities were reconciled through dialogue or by consulting a third party. To guarantee the accuracy of the information gathered, double entry was performed using Excel.
Quality evaluation
Two reviewers independently evaluated the quality of the included studies through the risk-of-bias tool recommended by the Revised Cochrane risk-of-bias tool for randomized trials (RoB2). If there was no consensus, the decision was made after discussion with the third reviewer. This tool includes the following domains: (a) risk of bias arising from randomization and allocation concealment; (b) risk of bias due to participants, investigators, and outcome assessors being aware of the intervention-group assignments; (c) risk of bias due to missing data; (d) risk of bias from the measurement of the outcome; (e) risk of bias due to selective reporting. The risk of bias can be classified into three levels: “low risk of bias,” “some concerns,” and “high risk of bias” [19].
Statistical analysis
For the meta-analysis, Review Manager (version 5.3) and STATA (version 16.0) were utilized. A forest plot was created and the effect estimate was calculated using the risk difference (RD) and the 95% confidence interval (CI). I2 and P-value are applied to describe the heterogeneity among the studies. If there is no statistical heterogeneity among the results of the studies (I2 < 50%, P > 0.05), the fixed effect model is used. If there is statistical heterogeneity (I2 > 50%, P < 0.05), the random effects model is used [20]. Meta-regression was utilized to examine heterogeneity sources, which were further investigated as subgroup variables. Egger test [21] and inverted funnel plot were used to evaluate the publication bias of studies and test the stability and reliability of the results through sensitivity analysis.
Result
Study screening process and results
According to the above literature retrieval formula, a total of 1195 relevant studies were retrieved, and then each study was excluded and confirmed one by one according to the literature inclusion and exclusion criteria. Finally, 46 studies were included, with a total sample size of 8424 people, including 4223 people in the experimental group and 4201 people in the control group (Fig. 2).
Characteristics of studies
Basic information
The literature was published between 2015 and 2022, and the survey area included 17 provinces, cities, and autonomous regions in China’s east, middle, and west. There were 11 studies with an experimental cycle of less than 12 months, 21 studies with a 12-month experimental cycle, and 14 studies with a period of more than 12 months. Table 1 summarizes the basic characteristics of the included studies.
Characteristics of intervention mode
Intervention models were classified according to the three roles involved in hypertension management. The FP denotes that the family physician is primarily responsible for patients’ health status. The intervention measures primarily consist of (1) signing a family physician service agreement; (2) establishing and maintaining health records; (3) developing personalized health intervention plans; (4) conducting follow-ups every three months or one month, including blood pressure monitoring, medication, diet, and exercise guidance; and (5) group health education, the key contents include frequent health education lectures, the distribution of hypertension prevention and control pamphlets, the formation of mutual aid groups for hypertension prevention and control. The FPP indicates that the patients will also be managed by themselves under the guidance of the family physician based on the FP. During the follow-up, family physicians used cognitive behavioral therapy, Motivational Interviewing (MI), or the Knowledge-Attitude-Practice (KAP) model to strengthen patients’ self-management abilities. The MI explores the inner contradictions of patients in the process of changing their bad behavior and finding personalized solutions through observation and interview, which is a communication method that guides patients in changing bad behavior [22]. The KAP is a knowledge, belief, and behavior intervention in which patients attain the goal of modifying behavior through three continuous processes: learning knowledge, changing attitude, and forming behavior [23]. The FPPF symbolizes the three roles involved in hypertension management. The creation of a family health worker is a feature of this model, to assist the family doctor in monitoring blood pressure, supervising medication administration, educating patients about health issues, and checking in with the patient once a week.
Quality assessment
According to the results of the quality assessment in Figs. 3 and 23.9% of studies were assessed as “low-risk bias” (11 of 46 studies), 65.2% of studies were assessed as “some concerns” (30 of 46 studies), and 10.9% of studies were assessed as “high-risk bias” (5 of 46 studies).To be clear, all the studies had the subjects sign the informed consent form, so none of the studies were double-blinded, but the literature quality evaluators judged that the outcomes would not be affected by the lack of blinding, and selected “low-risk of bias”. No missing outcome data were identified and appropriate measurements of the outcome were used in all studies. Prior protocols were not found in all studies which were judged as “some concerns”.
The control rate of hypertension
According to the results of the meta-analysis, the FPCS can increase the control rate of hypertension by 19% (RD = 0.19, 95%CI: 0.16–0.21), and the difference was statistically significant (χ2 = 110.56, P < 0.001). As shown in Fig. 4, the 46 studies included have moderate heterogeneity ( I2 = 59.3%, P < 0.001), so the random effect model was used for the pooled analysis of effect size.
Meta-regression
A meta-regression analysis was conducted to examine the effects of average age, experimental cycle, region, and intervention mode on the control rate of hypertension (Table 2). Average age (β = 0.28, P = 0.05) and intervention mode (β = 0.36, P < 0.001) have significant effects on the control rate.
Subgroup analysis
The average age and the mode of intervention are the sources of heterogeneity that impact the control rate of hypertension, as indicated by the meta-regression analysis results. To further investigate variations by age and by intervention model, subgroup analyses were carried out. The outcomes (Table 3) were as follows:
The control rate of hypertension for different ages
The population under 65 is categorized as working-age, and the population 65 and older is classed as elderly, according to the National Bureau of Statistics of China’s age classification guidelines. There are 22 research that focus on the elderly population and 24 that deal with the working-age population. Table 2 illustrates that the elderly population has a greater control rate than people of working age (Supplementary Material 3).
The control rate of hypertension by different intervention models
The three intervention modes were separated into FP, FPP, and FPPF. 25 of them employed the FP, 13 the FPP, and 8 the FPPF. According to the meta-analysis findings, FP, FPP, and FPPF had hypertension control rates of 90.1%, 94.4%, and 92.6%, respectively. Compared to the FP, the control rates of the FPP and FPPF were greater (Supplementary Material 3).
Publication bias
The funnel plot demonstrated that there was no evident publication bias and that the distribution of studies was fairly symmetrical. Additionally, there was no evident publication bias, as shown by the Egger test (p = 0.382 > 0.05) (Fig. 5).
Sensitivity analysis
Sensitivity analysis was performed using the one-by-one exclusion method to compare the pooled effect value with the results before the exclusion, and Fig. 6 shows that the conclusion was relatively stable.
Discussion
Summary of evidence
This study aims to evaluate the effect of family doctor signing services on the rate of hypertension control. A meta-analysis and systematic review revealed that FPCS could raise the rate of hypertension control by 19%. The average age and the intervention mode were found to be the sources of heterogeneity, according to the meta-regression results. Subgroup analysis was used to further explore the difference in average age and intervention mode. The results suggested that self-management and family support were key factors in the management of hypertension, that the elderly population had a better effect on hypertension control than the working-age population, and that the FPP and FPPF intervention had a better effect than FP.
The influence of FPCS on the control rate of hypertension
Patients in the control group were intervened by routine community management or self-medication. The two key components of routine management in the community are phone follow-up and outpatient review. During the review, medical personnel will administer medicine, provide recommendations on diet and exercise, and provide health education based on the patient’s condition. The purpose of the phone follow-up is to check the blood pressure and schedule the review session. Self-medication intervention refers to hypertensive patients taking calcium antagonists, diuretics, and other antihypertensive drugs according to the doctor’s advice, and carrying out outpatient review after the treatment [70]. These two intervention models require excellent self-management skills, primarily relying on patients’ autonomy to seek care from grassroots medical institutions, concentrating on managing a particular disease condition rather than managing the patient [71]. However, in practice, patients’ capacity to self-manage their conditions is hampered by competing life circumstances. They frequently struggle to take their medications on time, have low self-management awareness, and are ignorant of the causes and treatments of hypertension, all of which contribute to inadequate illness control.
FPCS is a contractual cooperation between residents and nearby grassroots medical institutions. They are focused on enhancing patients’ quality of life, guaranteeing management continuity through routine patient health status monitoring, and offering advice on medication, diet, exercise, and other topics. It can effectively strengthen communication between doctors and patients, and improve the trust and compliance of patients. Furthermore, it will compensate for the shortcomings of traditional medical services, and solve the problem of poor effectiveness in patient self-management due to a lack of attention and supervision [72]. Nevertheless, the majority of current FPCS might overlook the effects of anxiety, depression, and other psychological issues on patients’ general health and drug compliance. It is urgent to provide targeted mental health services. Fortunately, there has been a progressive increase in awareness of the mental health issues that individuals with chronic illnesses face [73]. In short, the awareness, treatment, and control rates of hypertension in China have significantly improved recently, but they are still relatively low when compared to wealthy nations, and there is still much space for development in the management of hypertension [74].
The influence of individual characteristics on the control rate of hypertension
The area has no discernible impact on the hypertension control effect, due to the study’s findings. According to a study, the eastern region’s contracted family doctors had a better effect on hypertension control than other regions [75]. This is because FPCS has a wealth of practical expertise and the eastern region has very accessible high-quality medical resources [76]. Yet, FPCS is implemented later in other places, and issues including a lack of family physicians and their caliber as well as an unscientific management system exist [77], which partially impedes the prevention and management of hypertension.
Compared with the working-age population, older people had a higher control rate for their hypertension, which is consistent with those of other studies [78, 79]. In addition to posing a longer medical history and a higher risk of complications like stroke, older patients also have higher levels of disease cognition [80], and their declining physical function means they will interact with the healthcare system more frequently and have more experience managing their condition, all of which are beneficial for blood pressure control [79]. Due to hectic work schedules, individuals of working age may not have the time to engage in health promotion activities like health education, which may result in a lack of initiative and compliance as well as a lack of information regarding the management of hypertension [81].
There is no obvious effect of the experimental cycle on the rate of hypertension control. The family physician’s contract service offers continuity features in theory. The beneficial influence on health-related behavior increases with the length of the contract [82]. A meta-analysis demonstrated that family physicians with contracts ranging from one to three years had a greater rate of hypertension control than those with contracts less than a year [75]. Nonetheless, Liang’s research revealed that, during the first three years of the intervention, the rate of hypertension management under general practitioners’ care rose, but in the fifth year, it fell in comparison to the third year [83]. It’s evident that the FPCS can, to a certain extent, improve the contracted objects’ health status, but this improvement may not last forever. Most studies have shown that the FPCS will continue to improve the patient’s compliance [84, 85], so this study speculates that the family doctor’s job burnout may be the reason for the drop in intervention intensity and service quality.
According to a systematic review on the topic, general practitioners experience moderate to high levels of job burnout globally [86]. This can have a detrimental effect on family physicians’ productivity, the quality of their services, and their patients’ health outcomes. The family practice system in China is currently improving gradually, but it also brings a work environment that increases pressure on family physicians with unreasonable workloads, arduous documentation burdens, etc. [68]. Family physicians may experience occupational burnout as a result of these reasons. As a result, it’s important to monitor job burnout to ensure the smooth development of family physician contracts.
The influence of health behaviors on the control rate of hypertension
The effectiveness of two health behaviors, self-management and family support, in hypertension management was demonstrated in the current study. FPP emphasizes the importance of self-management in the prevention and control of hypertension, which is the lack of FP mode. Compared with group health education in FP, the advantage of MI is that it does not provide the same health education to all patients. Instead, according to the condition and self-management status of each patient, appropriate publicity and education methods are developed through discussion and consultation with patients, which pay more attention to the patient’s feelings and communication skills [87]. The relationship between knowledge, beliefs, and behavior is strengthened by the KAP model. Knowledge acquisition can help patients understand disease and treatment knowledge, which is the basis for correcting their thinking concepts; physicians play a vital role in changing patients’ attitudes and can help them overcome obstacles and build confidence; and finally, the formation of target behaviors based on knowledge and attitude can help patients adjust their physical and mental state, give play to their subjective initiative, and correct inappropriate behavior [88, 89]. A randomized controlled trial has shown that cognitive behavioral therapies increased patients’ self-efficacy levels and assisted them in improving metabolic control and health behaviors [90]. Additionally, a review found that cognitive behavioral therapy is an effective approach to enhancing medication adherence [91].
FPPF highlights the vital role of health workers in blood pressure control, which is neglected by FP. Many research outcomes have demonstrated that the support of family members was conducive to the improvement of the disease to a large extent, patients with stable families have a better state of health compared with patients from disrupted or isolated social circumstances [92]. The primary reasons are as follows: First, family health workers can provide health education and lifestyle guidance to patients as relatives, which makes it easier to gain the trust of patients and has higher compliance [93]; second, the participation of family members is a facilitator of positive self-management in patients, which can allow patients to feel more support and encouragement, and promote the improvement of self-efficacy [94]; third, timely family member care and communication can assist patients in lowering psychological stress, enhancing their self-confidence in their ability to fend off illness, maintaining a healthy mental state, and ultimately helping to normalize blood pressure [95].
Suggestion
Based on the aforementioned findings and discussion, the present research makes the following recommendations:
First, it is suggested to further promote the application of FPCS in hypertension management, and at the same time, it is also necessary to pay more attention to the psychological state of patients with hypertension and provide personalized mental health services, to maximize the role of family doctors.
Additionally, other regions of China should learn from the experience of hypertension management in the eastern region to improve the service quality, and increasing research output should be emphasized to provide high-quality evidence to inform hypertension management.
Third, family physicians ought to tailor their medical care to each patient’s age-specific needs. For the working-age population who have less opportunity to participate in face-to-face services, it is suggested to use the blood pressure remote monitoring platform for real-time and whole process management of blood pressure.
Fourth, facilitate the performance appraisal system of family doctors, determine the remuneration through the actual workload and service output, and ensure the rationality of their income, to strengthen the service motivation of family physicians and reduce job burnout.
Limitation
First, the majority of the studies included in this systematic review are from eastern China, while the studies in the central and western regions are fewer, and the representativeness of the results is limited. Second, in the included studies, scholars have several definitions of outcome indicators, which to some extent affected the heterogeneity between studies. Third, this study only included RCTs, and excluded Randomized self-control clinical studies, without verifying the difference in results caused by different experimental types.
Conclusion
In conclusion, the family physician-contracted service has a high application value in the health management of hypertensive patients. The prevention and control of hypertension will depend on several elements, including average age, region, and intervention mode. To improve the quality of care provided by family physicians, efforts should be made to address the problems of uneven regional development, inadequate management of hypertension in the working-age population, and family physician job burnout. Patients and their families are encouraged to actively cooperate and work together to provide systematic, comprehensive, and targeted treatment services for patients, to promote the prognosis and quality of life of patients.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- FPCS:
-
Family physician-contracted service
- RD:
-
Risk difference
- CI:
-
Confidence interval
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- CVD:
-
Cardiovascular disease
- CNKI:
-
China National Knowledge Infrastructure
- CQVIP:
-
Chinese Scientific and Technological Journal Database
- FP:
-
“Family physician” model
- FPP:
-
“Family physician + Patient” model
- FPPF:
-
“Family physician + Patient + Family member” model
- MI:
-
Motivational Interviewing
- KAP:
-
“Knowledge – Attitude - Practice” model
References
Chinese Medical Association, Chinese Medical Journals Publishing House., Chinese Society of General Practice, Editorial Committee of Chinese Journal of General Practitioners, Expert Group for the Development of guidelines for Primary Care Cardiovascular diseases: Guideline for primary care of hypertension(2019). Chin J Gen Pract 2019(8):723–31.
(NCD-RisC) NRFC. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–80.
Writing committee of the report on cardiovascular health and diseases in China. Report on Cardiovascular Health and diseases in China 2021: an updated Summary. Biomed Environ Sci. 2022;35(7):573–603.
Wang J. Hypertension research in China has entered a new era. Chin J Cardiol. 2019;9:718–21.
Zhang L, Chen Z, Sun J, He Q. The necessity and significance of strengthening community management of hypertension. China J Mod Med 2001(12):70–1.
Practical guidelines for the. Prevention and treatment of hypertension in primary care. Chin J Gen Practitioners 2003(04):2–7.
Zhang M, Li L. Effect of standardized management of hypertension in primary public health services. Chin J Prev Control Chronic Dis. 2013;21(04):443–4.
Wu Y. Further expanding human resources for management of hypertension to cover all patients. Chin J Health Manage. 2022;05:289–91.
Ren X, Bai W. Management and nursing intervention of chronic disease patients in community. Chin Nurs Res. 2012;26(29):2775–7.
Wu H, Liu Y, Yang D, Chen Y. Exploration and practice of the four-way linkage prevention and treatment model for chronic diseases in Karamay community. Chin J Prev Control Chronic Dis. 2015;23(03):219–21.
Health and Family Planning Commission., Development and Reform Commission, Ministry of Civil Affairs, Ministry of Finance, Ministry of Human Resources and Social Security Bureau of Traditional Chinese Medicine, Circular on issuing Guidance on promoting family doctor contracted service. Gaz State Council People’s Repub China 2016(30):67–71.
Zhang L, Huang W, Lin S. Application of family doctor contracted service mode in comprehensive nursing care for residents’ health. Int Med Health Guidance News 2017(13):2119–22.
Hu X, Hou L, Shao P, Meng F. Studying onThe Utilization of Community Health Services and the influence from promoting contractual services sampled with Main Urban Area of Hangzhou. Chin Health Service Manage. 2020;37(07):489–93.
Cai L, Hou J. Implementation effect of the 1 + 1 + 1 type of contract on the development of Family Doctor services. Chin Gen Pract. 2018;21(31):3814–7.
Liu R, Yang D, Wu H, Li G. Contracted Family Doctor Service models leading to Healthy China:a comparative study. Chin Gen Pract. 2020;23(25):3139–45.
Wang H, Shi L, Han X, Zhang J, Ma Y, Yang X, Liu M, Fan L, Lou F. Factors associated with contracted services of Chinese family doctors from the perspective of medical staff and consumers: a cross-sectional study. BMC Health Serv Res. 2019;19(1):986.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1–10.
Lederle M, Tempes J, Bitzer EM. Application of Andersen’s behavioural model of health services use: a scoping review with a focus on qualitative health services research. BMJ Open. 2021;11(5):e045018.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Palacio A, Garay D, Langer B, Taylor J, Wood BA, Tamariz L. Motivational interviewing improves Medication Adherence: a systematic review and Meta-analysis. J Gen Intern Med. 2016;31(8):929–40.
Wang J, Chen L, Yu M, He J. Impact of knowledge, attitude, and practice (KAP)-based rehabilitation education on the KAP of patients with intervertebral disc herniation. Ann Palliat Med. 2020;9(2):388–93.
Liu C, Huang P. Analysis of Family Doctor service of empty Nester Hypertension Management. Med Inform. 2016;29(4):52–253.
Liu C. Application of family doctor contract service in community nursing management of elderly patients with hypertension. Diet Health-Care. 2018;5(23):129.
Liu D, Zheng B, Luo L, Shi M. Evaluation of the intervention effect of family doctor team service on community hypertension patients. Electron J Clin Med Literature. 2020;7(88):79–80.
Zhang D. The effectiveness of family doctor contract services in the management of chronic hypertension in communities. Diet Health-Care 2020(46):289.
Wang F, Qiu X. The method and effect of family doctor contract management mode in the comprehensive management of hypertension community. Healthmust-Readmagzine 2020(2):289.
Li G, Wang Y. Analysis of changes in awareness, treatment, and control rates of hypertension among newly diagnosed hypertension patients in the community before and after signing up for family doctor services. Chin Community Doctors. 2019;35(16):148–9.
Yang H. Chronic disease management and implementation effect evaluation under family doctor service mode. Health Literature. 2022;23(8):83–4.
Zhu H. Observation of intervention effect on hypertension patients in community by the Family Doctor System Service Model. Chin Prim Health Care. 2015;29(1):40–3.
Mo H, Chen S, Luo Z, Ou W, Wang J, Wang J. Evaluation on effect of community family doctor service intervention on community chronic disease management in Guangzhou. Practical Prev Med. 2017;24(04):468–71.
Jiang H. Effect of general treatment and standardized management of essential hypertension in community. Diabetes New World. 2018;15(11):137.
Dou H. Analysis of chronic disease management under the mode of family doctor service. Health Horizon 2020(1):287.
Wang H. Clinical effect of community family doctor contract service on elderly hypertension patients with type 2 diabetes. Healthmust-Readmagzine. 2021;18:288–9.
Wang J, Le X, Li D. Related exploration on family doctor contract service in the management of chronic diseases in communities. China Med Pharm. 2019;9(16):245–8.
Cheng J. The effect of family doctor signed intervention on blood pressure control in community hypertensive patients. Diet Health-Care. 2019;6(23):291.
Dong J. Application of family doctor contract service in the implementation of community nursing management for elderly patients with hypertension. Nurs Garden. 2022;12:28–30.
Sun J. Application of family doctor contract service in community nursing management of Elderly Hypertensive patients. Chin Community Doctors. 2022;38(11):111–3.
Shi L. Evaluation of the effectiveness of family doctor contract services in elderly chronic disease health management. J Clin Med. 2018;5(77):8092.
Zhang L. Effect of family doctor service on treatment compliance and control rate in community patients with essential hypertension. China Med Pharm. 2017;7(14):248–50.
Zhang L, Han S. Analysis of the Effect of the Family Doctor Contracted Service Model on the management of hypertension patients in the community. Cuide of China Medicine. 2020;18(12):15–7.
Tao L. Application effect of family doctor contract service in community nursing management of elderly patients with hypertension. Care Health 2022(10):158–60.
Xue L. Application value of family doctor contract service in community nursing management of elderly patients with hypertension. Health Horizon 2021(10):261.
Li L. Effect and compliance evaluation of family doctor contracted service in community nursing management of elderly patients with hypertension. Chin Community Doctors. 2021;37(29):129–30.
Yuan L. Analysis of intervention effect of family doctor contract management on elderly patients with hypertension and type 2 diabetes living alone. In: Proceedings of 2021 South China Forum on Integrated Traditional Chinese and Western Medicine Health Management and Rehabilitation Medicine Guangzhou; 2021: 32–34.
Zou L. Effect of family doctor service model on chronic disease health management in community. J Imaging Res Med Appl. 2017;1(08):232–3.
He M. Intervention effect of family doctor contract service mode in community high-risk groups of chronic diseases. Health Guide 2019(34):1.
Yang M, Jia W. Exploration Theintervention practical effect of family doctor’s on refractory hypertension under the whole-specialized combined mode in community hospital. Chin Community Doctors. 2020;36(27):74–5.
Huang P. Family doctor service on blood pressure control in hypertensive patients in community. Chin Community Doctors. 2018;34(29):175–6.
Zhang R. Effects of community family doctor service model on patients with diabetes and hypertension. Diabetes New World. 2019;22(11):194–5.
Wang S, Li Y, Huang S. The impact of community family doctor contract services on standardized medication, blood pressure values, compliance rates, and awareness of hypertension prevention and control knowledge among community hypertensive patients. Jilin Med J. 2019;40(11):2637–40.
Wang W. Evaluation of the management effect of the contracted service of smart home doctors on the management of hypertension patients in the community. Chin Community Doctors. 2021;37(36):171–2.
Zuo W. Evaluation on the management effect of family doctors for patients with hypertension in community. Diet Science 2018(24).
Chen X, Lyu W. The effect of applying Family Doctor’s Contract Service to Community Hypertension patients and its influence on their quality of life. Chin Foreign Med Res. 2020;18(14):175–7.
Zhang X, Zhang J. Analysis of the application effect of family doctor contract services in elderly chronic disease health management. China Health Care & Nutrition. 2020;30(2):382–3.
Zhang X. Analysis of the effect of family doctor comprehensive intervention on blood pressure control in community hypertension patients. Chin Community Doctors. 2018;34(27):156–7.
Dong X. Evaluation of the effect of the information-based family doctor team appointment follow-up mode in the management of hypertension. Shanghai Med Pharm J. 2019;40(12):33–5.
Huang X. The impact of pharmaceutical services provided by family doctor teams on the management of chronic diseases. China Pharmaceuticals 2020, 29(S02).
Luan Y, Zhan H, Zhang Y, Miao H. The application effect of family doctor in the control of hypertension in community. J Taishan Med Coll. 2020;41(4):272–4.
Zheng Y. Chronic disease management under the family doctor service model. Home Med. 2020;7:211–2.
Su Y, Qian Z. Effect of Comprehensive Medical intervention on Hypertension Management in Community. Practical J Cardiac Cereb Pneumal Vascular Disease. 2017;25(S1):35–7.
Bai Y. Application of family doctor service model in health management of community patients with chronic diseases. Women’s Health Research 2021(15):194–5.
Li W. Application of community nurse-led family medical team in patients with hypertension. Healthful Friend. 2020;4:154.
Chen Y, Chen T, Chen Y, Wu W. Impact of 1 + 1 + 1 combination contract on management effect and drug payment in hypertensive patients. Guangxi Med J. 2020;42(1):95–8.
Peng Z. Evaluation of the Effect of Family Doctor Contract Management intervention on Community Hypertension patients. J Qiqihar Univ Med. 2016;37(29):3687–8.
Liu Z. The Effect of Family Doctor Team Service Model on Hypertension Community Management. Healthmust-Readmagzine. 2021;32:213–4.
Lin Z. A study on the management effect of family doctor contract management model on elderly hypertensive patients with poor compliance. Capital Med. 2020;27(15):20–1.
Shi Z. Analysis of the effectiveness of community general practitioner contract signing model in preventing and treating chronic diseases in elderly patients in the community. Renowned Doctor 2022(12):51–3.
Gu M, Qin T, Qiao K, Bai X, Wang Y, Yang Y, Li X. A network meta-analysis of primary hypertension management patterns in China. Chin Gen Pract:1–22.
Allegrante JP, Wells MT, Peterson JC. Interventions to support behavioral self-management of Chronic diseases. Annu Rev Public Health. 2019;40:127–46.
Jafar TH, Gandhi M, de Silva HA, Jehan I, Naheed A, Finkelstein EA, Turner EL, Morisky D, Kasturiratne A, Khan AH, et al. A community-based intervention for managing hypertension in Rural South Asia. N Engl J Med. 2020;382(8):717–26.
Yu K, Wang J, Zhou Z, Chen X, Wang S. Chronic Disease Management in Primary Care in China: recent advances and Hotspot Analysis using VOSviewer. Chin Gen Pract. 2022;25(28):3493–501.
Zhu L, Xu J. Community management of hypertension based on contracted services of general practitioner: thoughts on clinical practice of guideline for primary care of hypertension. Chin J Gen Practitioners 2023(03):245–9.
Chen D, Xu P, Yao X, Li Y. Meta-analysis of Chronic Disease Control Rate under the model of family doctors in China. Chin J Social Med. 2022;39(02):200–4.
Wang L, Yu Q, Wang X, Shi P, Shen Q, Chen Z, Pu C, Xu L, Hu Z, Ma A, et al. Strengths, shortcomings and key control points of capacity-building in hypertension prevention and control: a comparative analysis among provincial-level administrative divisions in China. Chin J Public Health. 2023;39(09):1089–95.
Hu X. Bibliometric analysis of the current Status and trends of Research on Family Doctor contracting services. Chin Prim Health Care. 2022;36(09):39–43.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE million persons project). Lancet. 2017;390(10112):2549–58.
Yin M, Augustin B, Fu Z, Yan M, Fu A, Yin P. Geographic distributions in Hypertension diagnosis, measurement, prevalence, awareness, treatment and control rates among middle-aged and older adults in China. Sci Rep. 2016;6:37020.
Hu L, Liao J, Tang Z, Jike C, Zhu T, Cao Y, Yu J, Zhu W, Zhang H, Liao Q, Zhang T. Analysis of current situation and influencing factors of blood pressure control in patients with hypertension. Mod Prev Med. 2023;50(11):2101–6.
Feng G, Ji Y, Yuan H, Xie Z, Chen Y. Home Blood Pressure Monitoring and Health Education Analysis in Hypertensive patients of different ages. Chin Gen Pract. 2019;22(34):4246–50.
Meng W, Liu S, Jiang X, Peng H, Li Z, Yu Q, Yin W, Sun K, Chen Z, Guo H. Mechanisms affecting the effectiveness of contracted family doctor services:a grounded theory analysis. Chin Gen Pract. 2023;26(10):1192–7.
Liang X, Zhong H, Xiao L. The effect of community hypertension management on blood pressure control and its determinants in southwest China. Int Health. 2020;12(3):203–12.
Huang J, Liu S, He R, Fang S, Lu W, Wu J, Liang H, Zhang Y. Factors associated with residents’ contract behavior with family doctors in community health service centers: a longitudinal survey from China. PLoS ONE. 2018;13(11):e0208200.
Shang X, Huang Y, Li B, Yang Q, Zhao Y, Wang W, Liu Y, Lin J, Hu C, Qiu Y. Residents’ Awareness of Family Doctor Contract Services, Status of Contract with a Family Doctor, and Contract Service Needs in Zhejiang Province, China: A Cross-Sectional Study. Int J Environ Res Public Health 2019, 16(18).
Karuna C, Palmer V, Scott A, Gunn J. Prevalence of burnout among GPs: a systematic review and meta-analysis. Br J Gen Pract. 2022;72(718):e316–24.
Steffen PLS, Mendonça CS, Meyer E, Faustino-Silva DD. Motivational interviewing in the management of type 2 diabetes Mellitus and arterial hypertension in Primary Health Care: an RCT. Am J Prev Med. 2021;60(5):e203–12.
Ghannadi S, Amouzegar A, Amiri P, Karbalaeifar R, Tahmasebinejad Z, Kazempour-Ardebili S. Evaluating the Effect of Knowledge, Attitude, and Practice on Self-Management in Type 2 Diabetic Patients on Dialysis. J Diabetes Res 2016, 2016:3730875.
Yang M, Fu Y, Wang L. Effects of 3H nursing based on knowledge, belief and practice model combined with family follow-up intervention on blood pressure, self-management behavior and self-perceived burden of elderly patients with primary hypertension. Clin Res Pract. 2022;7(34):167–70.
Selçuk-Tosun A, Zincir H. The effect of a transtheoretical model-based motivational interview on self-efficacy, metabolic control, and health behaviour in adults with type 2 diabetes mellitus: a randomized controlled trial. Int J Nurs Pract. 2019;25(4):e12742.
Kini V, Ho PM. Interventions to improve Medication Adherence: a review. JAMA. 2018;320(23):2461–73.
Osamor PE. Social support and management of hypertension in South-West Nigeria. Cardiovasc J Afr. 2015;26(1):29–33.
Fort MP, Steiner JF, Santos C, Moore KR, Villaverde M, Nease DE, Ortega D, Manson SM. Opportunities, challenges, and strategies for Engaging Family in Diabetes and Hypertension Management: a qualitative study. J Health Care Poor Underserved. 2020;31(2):827–44.
Shi J, Ferretti L, McCallion P. Attending with family members, completion rate and benefits accrued from chronic disease self-management program. Chronic Illn. 2022;18(4):784–95.
Li Y, Zhao N, Zhao P. Relationship between family support and hope of elderly pations with hypertension: China mediating effect of anxiety and depression. China J Health Psychol. 2022;30(06):839–43.
Funding
Establish a new mechanism for the operation of the grassroots medical service system, Grant Number: 2022B2033.
Author information
Authors and Affiliations
Contributions
Yiping Zheng, Yuqing Liu, Dongyu Xue, Zhao Shang, Baoquan Zhang, and Yue Dai contributed to the conception and design of this study. Yiping Zheng, Yuqing Liu, and Dongyu Xue were involved in literature screening, data collection, and quality evaluation. Yiping Zheng, Zhao Shang, Baoquan Zhang, and Yue Dai analyzed and interpreted the data. The manuscript was drafted by Yiping Zheng and Yue Dai. Baoquan Zhang provided financial support. The final version was reviewed and approved by all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
PRISMA 2020 Checklist
Supplementary Material 2:
Search Strategies
Supplementary Material 3:
Effect Sizes Forest Plots
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, Y., Liu, Y., Xue, D. et al. Research on the control rate of hypertension under family physician-contracted service. BMC Prim. Care 25, 47 (2024). https://doi.org/10.1186/s12875-024-02280-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-024-02280-0