Abstract
Background
Older adults are more prone to increasing comorbidities and polypharmacy. Polypharmacy is associated with inappropriate prescribing and an increased risk of adverse effects. This study examined the effect of polypharmacy in older adults on healthcare services utilization (HSU). It also explored the impact of different drug classes of polypharmacy including psychotropic, antihypertensive, and antidiabetic polypharmacy on HSU.
Methods
This is a retrospective cohort study. Community-dwelling older adults aged ≥ 65 years were selected from the primary care patient cohort database of the ambulatory clinics of the Department of Family Medicine at the American University of Beirut Medical Center. Concomitant use of 5 or more prescription medications was considered polypharmacy. Demographics, Charlson Comorbidity index (CCI), and HSU outcomes, including the rate of all-cause emergency department (ED) visits, rate of all-cause hospitalization, rate of ED visits for pneumonia, rate of hospitalization for pneumonia, and mortality were collected. Binomial logistic regression models were used to predict the rates of HSU outcomes.
Results
A total of 496 patients were analyzed. Comorbidities were present in all patients, with 22.8% (113) of patients having mild to moderate comorbidity and 77.2% (383) of patients having severe comorbidity. Patients with polypharmacy were more likely to have severe comorbidity compared to patients with no polypharmacy (72.3% vs. 27.7%, p = 0.001). Patients with polypharmacy were more likely to visit the ED for all causes as compared to patients without polypharmacy (40.6% vs. 31.4%, p = 0.05), and had a significantly higher rate of all-cause hospitalization (adjusted odds ratio aOR 1.66, 95 CI = 1.08–2.56, p = 0.022). Patients with psychotropic polypharmacy were more likely to be hospitalized due to pneumonia (crude odds ratio cOR 2.37, 95 CI = 1.03–5.46, p = 0.043), and to visit ED for Pneumonia (cOR 2.31, 95 CI = 1.00–5.31, p = 0.049). The association lost significance after adjustment.
Conclusions
The increasing prevalence of polypharmacy amongst the geriatric population with comorbidity is associated with an increase in HSU outcomes. As such, frequent medication revisions in a holistic, multi-disciplinary approach are needed.
Similar content being viewed by others
Background
The advancements in modern medicine have led to an increase in life expectancy, and have subsequently created new challenges in treating older adults, mainly comorbidity [1]. Comorbidity is defined as the coexistence of 2 or more chronic conditions [1]. As the number of chronic conditions facing older adults increases, the management complexity for both the healthcare provider and the patient also increases. As such, comorbidity will naturally necessitate an increased number of medications to manage the different conditions. This is commonly referred to as polypharmacy, another challenge in geriatric patient management.
Although there is no clear definition in the literature, polypharmacy is commonly defined as the use of 5 or more medications at the same time [2]. Alternatively, a common qualitative definition of polypharmacy is the use of multiple medications concurrently by the same patient [2].
The prevalence of polypharmacy among older adults differs across countries, but a common pattern of increased prevalence was noted. In 2010, the prevalence of polypharmacy among adults in Scotland was 22.1%, as compared to 11.4% in 1995 [3]. A similar trend was noted in Sweden with polypharmacy prevalence reaching 44%, 50% of whom were aged 65 or more [4]. In the United States, the prevalence of polypharmacy among adults 65 years or older was 65.1% between 2009 and 2016 [5]. Similar patterns were observed in the Middle East, as the prevalence of polypharmacy in Saudi Arabia among patients 60 years or older reached 51.5% [6]. Moreover, a study found that 23.9% of adults above 65 years of age in rural areas in Lebanon were exposed to polypharmacy [7].
Although polypharmacy may be appropriate in some older adults [8], it has potential negative effects including adverse drug events (ADEs), increased healthcare services utilization (HSU) [9], cognitive impairment, reduced adherence, falls, and mortality [10]. A retrospective study documented that 10% of emergency department (ED) visits for adults aged 65 years or older can be attributed to ADEs [11]. Another retrospective study has shown that older veterans taking more than 5 medications were 4 times more likely to be hospitalized from ADEs [12]. Moreover, the risk of drug-drug interaction increases as the number of medications increases. A patient taking 5 to 9 medications has a 50% probability of drug interactions, and a patient taking more than 20 has a 100% probability [13]. ADEs will eventually lead to more HSU since it accounts for 6.5% of hospital admissions [14].
Furthermore, polypharmacy affects cognitive ability with the number of medications shown to be a risk factor for delirium [15]. A study of cognitive impairment in older adults showed that 33% and 54% of patients taking more than 5 and 10 medications, respectively, had cognitive impairment [16]. A meta-analysis examining the association between polypharmacy and mortality showed that polypharmacy is associated with higher mortality [17].
This study aims to examine the effect of polypharmacy in older adults on HSU outcomes as defined by the rate of all-cause ED visits, rate of all-cause hospitalization, rate of ED visits for pneumonia, rate of hospitalization for pneumonia, and mortality. A second aim is to explore the impact of different drug classes of polypharmacy including psychotropic, antihypertensive, and antidiabetic polypharmacy on HSU outcomes.
Methods
Study design, participants, and setting
This retrospective cohort study involved the secondary analysis of a primary care center’s dataset. The original dataset was created using a retrospective case-control design to examine the association between polypharmacy and dementia in community-dwelling older adults who are 65 years and older with dementia, and a control group attending the ambulatory clinics of the Department of Family Medicine at the American University of Beirut Medical Center (AUBMC), Beirut, Lebanon. The sample of this study consisted of all patients (n = 496) in the original primary care cohort of community-dwelling older adults ≥ 65 years of age. All data were retrieved from the medical records at the primary healthcare clinics. In the original dataset, the reference date indicated the date of diagnosis of the cases with dementia, and the selection date referred to the date of selection of controls without dementia. Cases were matched to three controls based on age and gender, and year of dementia diagnosis. In the current study, baseline data at the reference/selection date was collected and included age, gender, history of depression, medical comorbidities, smoking status, number, and type of prescription medications. The Charlson Comorbidity Index (CCI) [18] score and the Atherosclerotic Cardiovascular Disease (ASCVD) score were calculated based on data extracted from the reference/selection date. The ASCVD score was divided into two categories; low-intermediate risk if the score is < 20%, and high risk if ≥ 20% [19]. The CCI score was used as an indicator for comorbidity and calculated as a continuous variable and then divided into three CCI categories: mild- (≤ 2), moderate- (3 to 4), and severe risk (≥ 5). CCI was further collapsed into two categories; mild-moderate risk if the score is < 5, and high risk if ≥ 5 for the analysis [20]. The chronic diseases extracted and assessed were: congestive heart failure, peripheral vascular disease, cerebrovascular stroke, hemiplegia, dementia, chronic obstructive pulmonary disease, connective tissue disorders, peptic ulcer disease, liver disease, diabetes mellitus, renal disease, tumors, leukemia, lymphoma, and HIV/AIDS.
Healthcare services utilization outcomes
HSU included 5 outcomes; the rate of all-cause ED visits, rate of all-cause hospitalization, rate of ED visits for pneumonia, rate of hospitalization for pneumonia, and mortality, all of which were collected within 3 years after the reference/selection date. ED visits and hospitalization for pneumonia were added as HSU outcomes since the prevalence of pneumonia increases with age and has a high short- and 1-year mortality rate among older adults [21]. HSU outcome rates were transformed to binary variables with ‘yes’ and ‘no’ options, and the ‘yes’ was defined as ≥ 2 episodes for all-cause ED visits and all-cause hospitalization, and ≥ 1 episode for ED visits for pneumonia, and hospitalization for pneumonia.
Medication status
The list of prescription medications at the reference/selection date was collected. Polypharmacy is defined as the regular use of five or more medications daily [2]. All drugs recorded were coded according to the 2018 Anatomical Therapeutic Chemical (ATC) classification system developed by the WHO Collaborating Centre for Drug Statistics Methodology [22]. The dosage was not considered. Medications with different brand names and generics having the same ATC code were considered as one medicine. As-needed agents, topical agents, herbal and dietary supplements, and drugs for short-term use such as antibiotics and vaccinations were excluded.
Psychotropic, antihypertensive, and antidiabetic polypharmacy were defined as the concurrent use of two or more psychotropic, antihypertensive, and antidiabetic medications, respectively.
This definition is based on studies in the literature since there are no clear guidelines [23]. These specific classes of medications were associated with more adverse health outcomes in older adults compared to other medications [24,25,26,27]. Psychotropic medications include antidepressants, antiepileptics, antipsychotics, gabapentin, hypnotics, sedatives, anxiolytics, and mood stabilizers. The ATC codes of psychotropic medications include: N06AX21, N06AB10, N06AB03, N06AA02, N06AA14, N06AX11, N06AB05, N06AB06, N06AX16, N06AX26, N06AA09, N03AX18, N03AX14, N03AB02, N03AA03, N05AA01, N05AF01, N05AD01, N05AG02, N05AB04, N05AH04, N05AX08, N03AX12, N03AX16, N03AE01, N05CF04, N05BA06, N05CD08, N05CF02, N05BA12, N05BA08, N05BA02, N03AF01, N03AX09, N05AN01, N03AG01. The ATC code of antihypertensive medications include: C09AA02, C09AA03, C09AA04, C09AA06, C09AA05, C09AA10, C09AA09, C09AA01, C09CA06, C09CA04, C09CA01, C09CA08, C09CA07, C09CA03, C07AB03, C07AB07, C07AB09, C07AB02, C07AB12, C07AA05, C07AG02, C08CA13, C08CA05, C08DA01, C08CA01, C08EA02, C08DB01, C03DB01, C03CA02, C03DA04, C03CA01, C03AA03, C03BA, C03DA01, C03CA04, C03BA04, C01DA08, C01DA14, C01DX12, C01DX16, C01EB15. The ATC codes of the antidiabetic medications include: A10BF01, A10BA02, A10BH05, A10BH03, A10BH01, A10BH02, A10BJ02, A10AB01, A10AB05, A10AE06, A10AE05, A10AE04, A10AC04, A10BX02, A10BK01, A10BK03, A10BB01, A10BB09, A10BB12, A10BB08, A10BB01, A10BG03.
Statistical analysis
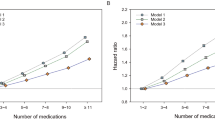
The demographic, clinical characteristics and HSU outcomes of the study population were analyzed and reported as mean and standard deviation (SD) for continuous variables, and frequency and percentage for categorical variables. Bivariate analysis was performed for the demographics, clinical characteristics, and HSU outcomes using the Chi-squared test for categorical variables, and the independent T-test for continuous variables. Binomial logistic regression models were used to predict the rates of all-cause ED visits, all-cause hospitalization; ED visits due to pneumonia, hospitalization due to pneumonia, and mortality. Two separate models for HSU outcome were performed to avoid collinearity between polypharmacy and its drug classes. Model 1 was performed to examine the association between polypharmacy and HSU outcomes. It included polypharmacy and adjusted for the patients’ demographic and clinical characteristics that include dementia, age, gender, smoking status, depression, CCI, and ASCVD scores. Model 2 was performed to examine the association between the drug classes of polypharmacy (psychotropic, antihypertensive, and antidiabetic) and HSU outcomes. Model 2 was adjusted for the same demographic and clinical characteristics. Adjusting for dementia was necessary to minimize bias since the data was originally collected as a case-control design, with the cases defined by the diagnosis of dementia.
Results
Demographic and clinical characteristics of the study population
Table 1 summarizes the baseline characteristics of our sample of 496 patients. The mean age of our sample was 78.6 years old, of which 195 (39.3%) were females and 301 (60.7%) were males. Sixty-two (24.9%) patients had a low-intermediate risk ASCVD score and 187 (75.1%) had a high-risk ASCVD score. Comorbidities were present in all patients, with 22.8% (113) of patients having mild to moderate comorbidity (CCI < 5) and 77.2% (383) of patients having severe comorbidity (CCI ≥ 5).
One hundred and twenty-four (25%) patients had dementia. Overall, the prevalence of polypharmacy was 68.5%, 8.5% for psychotropic polypharmacy, 72.8% for antihypertensive polypharmacy, and 95.6% for antidiabetic polypharmacy (Fig. 1). The number of comorbid chronic conditions in our patient population is illustrated in Fig. 2.
Bivariate analysis
Patients with polypharmacy had considerably more severe comorbidity (CCI ≥ 5) compared to the non-polypharmacy group (72.3% vs. 27.7%, p = 0.001), were more likely to visit the ED for all causes (40.6% vs. 31.4%, p = 0.05), and were more likely to be hospitalized (37.9% vs. 25.6%, p = 0.007). When mortality, ED visits for pneumonia, and hospitalization for pneumonia were compared between the polypharmacy and no polypharmacy groups, no statistically significant differences were found (Table 2).
Association between polypharmacy, drug classes of polypharmacy, and healthcare services utilization outcomes
In model 1, logistic regression was performed to examine the association between polypharmacy and HSU outcomes. Model 1 was adjusted for age, gender, smoking status, depression, dementia, CCI, and ASCVD scores. Patients with polypharmacy had a significantly higher rate of all-cause hospitalization (aOR 1.66, 95 CI = 1.08–2.56, P = 0.022) (Table 3). In model 2, logistic regression was performed to examine the association between drug classes of polypharmacy and HSU outcomes. Model 2 was adjusted for the same covariates as model 1. Patients with psychotropic polypharmacy were more likely to visit the ED (cOR 2.31, 95 CI = 1.00–5.31, P = 0.049) and to be hospitalized for pneumonia (cOR 2.37, 95 CI = 1.03–5.46, P = 0.043), however, this association lost significance when the model was adjusted. No significant association between antidiabetic and antihypertensive polypharmacy and HSU outcomes was found (Table 4).
Discussion
The present study examined the effect of polypharmacy on HSU outcomes in older adults with comorbidities. It also shed light on the impact of different drug classes of polypharmacy, including psychotropic, antihypertensive, and antidiabetic polypharmacy on HSU outcomes.
We report a high prevalence of polypharmacy (68.5%) in our study sample, which is consistent with prior studies that found comparable rates [7,8,9]. Our findings revealed a lower prevalence rate of psychotropic polypharmacy (8.5%) compared to previous research (18% and 44.9%) [29, 30]. These disparities could be attributed to variations in study design and settings. To the best of our knowledge, there have been no studies that describe the prevalence of antidiabetic and antihypertensive polypharmacy. Patients with polypharmacy had higher comorbidity scores, which is in line with previous research indicating that people with multiple chronic conditions are more likely to have polypharmacy [28, 29].
We found a significant association between polypharmacy and all-cause hospitalization, consistent with previous studies [30,31,32]. The increase in hospital admissions can be attributed to the adverse effects of medications. This is further supported by evidence suggesting that as the number of prescribed medications increases, so does the likelihood of prescribing error, high-risk prescribing, and ADEs [33]. Despite controlling for comorbidities, it is important to note that comorbidity indices quantify the burden of coexisting medical conditions and often do not reflect the clinical complexity of the older patient or the severity of chronic diseases, which may partially explain the observed association between polypharmacy and hospitalization [34]. We did not find an association between polypharmacy and mortality. Although some studies [17, 32] demonstrated an association between polypharmacy and increased mortality in older adults, others have been inconsistent and failed to find these associations [35]. The causality of the relationship remains unclear and must be carefully considered [32].
Psychotropic polypharmacy was found to increase the likelihood of ED visits for pneumonia, and hospitalization for pneumonia. However, after adjustment, the association lost significance. No association was found between antihypertensive and antidiabetic polypharmacy and HSU outcomes. Our findings are supported by recent evidence indicating that the use of psychotropic drugs (antipsychotics, benzodiazepine [BZD], and benzodiazepine-related drugs) is associated with an increased risk of pneumonia in older adults aged ≥ 65 years [36, 37]. This relationship increased in strength as age increased, which also supports our explanation in the setting of older adults [36]. First, the extrapyramidal side effects of antipsychotics, in particular tardive dyskinesia, increase the likelihood of aspiration because of involuntary buccolingual movements and oropharyngeal dysphagia [38]. Second, the histamine receptor-blocking ability of antipsychotics, coupled with the age-related changes of the airway, causes patients to inadequately handle secretions, which can lead to aspiration [39].
Moreover, a recent systematic review and meta-analysis found that older adults aged ≥ 65 years who were exposed to BZD had an increased risk of pneumonia [40]. The sedative effect induced by BZDs in older adults may lead to an increased risk of aspiration pneumonia [41, 42]. In addition, BZD exposure has been associated with an increased risk of gastroesophageal reflux disease (GERD) in older adults, which may be related to the relaxation of the esophageal sphincter, possibly leading to aspiration [41, 42]. Animal studies showed that BZDs increase vulnerability to infection by activating specific Gamma-aminobutyric acid (GABA) receptors on immune cells [43].
Studies on the association between antidepressant use and the development of pneumonia yielded mixed results. When controlling for confounders, it was found that antidepressants were not associated with an increased risk of pneumonia [44]. However, a strong body of evidence suggests that antidepressants increase the risk of pneumonia through anticholinergic properties [45] and its sedative effects [46].
The association between psychotropic polypharmacy and pneumonia should be explored in light of the indications and diagnoses associated with this class of medications. This was evident in our results, as the association between psychotropic polypharmacy and pneumonia, both ED visits and admission lost significance after adjusting for potential confounders. One explanation can stem from the well-documented association between dementia and the increased risk of pneumonia-related healthcare utilization [47]. Moreover, psychiatric disorders like depression, schizophrenia, and bipolar disorder, are associated with a higher risk of having pneumonia compared to the general population [48, 49]. Thus the association of psychotropic polypharmacy and pneumonia-related healthcare utilization should be considered with the different cofounders in mind.
Despite the lack of evidence on the association between regular medication review and prevention of adverse clinical outcomes, such as hospitalization and mortality [50], our findings encourage regular medication review as part of clinical encounters to reduce polypharmacy and inappropriate prescribing and to identify potential drug-drug interactions. It is crucial to focus on “high-risk” medication classes, their indications, and their risk-benefit ratios. One solution is adopting a multidisciplinary approach when caring for older adults, which involves the input of physicians, clinical pharmacists, and other healthcare personnel. This collaborative approach improves medication appropriateness by alerting the healthcare provider about polypharmacy and informing the patient about potential side effects and warning signs [51]. Another solution would be to use the American Geriatrics Society Beers Criteria® (AGS Beers Criteria®) for Potentially Inappropriate Medication (PIM) use in older adults as a screening tool to taper down or discontinue inappropriate medications [52].
Strengths and limitations
To the best of our knowledge, this is the first study in a primary care setting that explored the association between polypharmacy and drug classes of polypharmacy and HSU outcomes. Nevertheless, we acknowledge that there are limitations to our study. First, cases and controls were both selected from the same clinic and hospital, which increases selection bias, and make the data less generalizable to the population. Second, this study was conducted in a tertiary medical center, which makes it susceptible to referral bias. The results can be prone to assessor bias in making the diagnosis of dementia. Since the cohort was not randomized but selected as cases and controls, differences in the character of each group can introduce confounders in the results. The cohort was taken from a dataset originally collected as a case-control study assessing the effect of polypharmacy on dementia; however, adjusting for dementia and other potential confounders in the models decreased the chance of bias. Given that our study was retrospective chart review research, incomplete or missing documentation may have occurred. Our study did not investigate the impact of medication interactions, either within the same class or across different classes, or medication adherence on healthcare-associated outcomes. Other outcomes could be explored in future studies, such as falls and related ED visits or hospitalization to further our understanding of the prognostic impact of polypharmacy. Future studies are also needed to examine the effect of drug interactions and medication adherence on healthcare utilization and outcomes.
Conclusion
The advancements in modern medicine have brought about an ever-growing aging population, which presents a unique set of challenges. Comorbidity and consequently polypharmacy warrants particular attention due to potential inappropriate prescribing and consequent adverse events in this age group. This study demonstrated an association between polypharmacy and all-cause hospitalization in older adults. It further highlighted the effect of psychotropic polypharmacy on ED visits for pneumonia, and hospitalization for pneumonia. These findings indicate the need for frequent medication revisions among older adults, in a holistic, multi-disciplinary approach.
Data Availability
The datasets generated and analyzed during the current study are not publicly available to protect patients’ confidentiality but are available from the corresponding author upon reasonable request.
Abbreviations
- AUBMC:
-
American University of Beirut Medical Center
- HSU:
-
Healthcare Services Utilization
- ED:
-
Emergency Department
- CCI:
-
Charlson Comorbidity Index
- ASCVD:
-
Atherosclerotic Cardiovascular Disease
- ADEs:
-
Adverse Drug Events
- ATC:
-
Anatomical Therapeutic Chemical
- SD:
-
Standard deviation
- BZD:
-
benzodiazepine
- GERD:
-
Gastroesophageal reflux disease
- GABA:
-
Gamma-aminobutyric acid
- AGS:
-
American Geriatrics Society
- PIM:
-
Potentially Inappropriate Medication.
References
Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74.
Morin L, Johnell K, Laroche ML, Fastbom J, Wastesson JW. The epidemiology of polypharmacy in older adults: register-based prospective cohort study. Clin Epidemiol. 2018;10:289–98.
Young EH, Pan S, Yap AG, Reveles KR, Bhakta K. Polypharmacy prevalence in older adults seen in United States physician offices from 2009 to 2016. PLoS ONE. 2021;16(8):e0255642.
Aljawadi MH, Khoja AT, Alaboud NM, AlEnazi ME, Al-Shammari SA, Khoja TA, et al. Prevalence of polypharmacy and factors Associated with it among saudi older adults - results from the Saudi National Survey for Elderly Health (SNSEH). Saudi Pharm J. 2022;30(3):230–6.
Zgheib E, Ramia E, Hallit S, Boulos C, Salameh P. Factors Associated with Functional Disability among Lebanese Elderly Living in Rural Areas: Role of Polypharmacy, Alcohol Consumption, and Nutrition-based on the aging and malnutrition in Elderly Lebanese (AMEL) Study. J Epidemiol Glob Health. 2018;8(1–2):82–90.
Duerden M, Avery T, Payne R. Polypharmacy and medicines optimisation making it safe and sound. The King’s Fund; 2013.
Lin RK, Hsu HS, Chang JW, Chen CY, Chen JT, Wang YC. Alteration of DNA methyltransferases contributes to 5’CpG methylation and poor prognosis in lung cancer. Lung cancer (Amsterdam Netherlands). 2007;55(2):205–13.
Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57–65.
Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38(6):666–71.
Marcum ZA, Amuan ME, Hanlon JT, Aspinall SL, Handler SM, Ruby CM, et al. Prevalence of unplanned hospitalizations caused by adverse drug reactions in older veterans. J Am Geriatr Soc. 2012;60(1):34–41.
Doan J, Zakrzewski-Jakubiak H, Roy J, Turgeon J, Tannenbaum C. Prevalence and risk of potential cytochrome P450-mediated drug-drug interactions in older hospitalized patients with polypharmacy. Ann Pharmacother. 2013;47(3):324–32.
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329(7456):15–9.
Martin NJ, Stones MJ, Young JE, Bedard M. Development of delirium: a prospective cohort study in a community hospital. Int Psychogeriatr. 2000;12(1):117–27.
Jyrkka J, Enlund H, Lavikainen P, Sulkava R, Hartikainen S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol Drug Saf. 2011;20(5):514–22.
Leelakanok N, Holcombe AL, Lund BC, Gu X, Schweizer ML. Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharm Assoc (2003). 2017;57(6):729–38e10.
Gravina GL, Marampon F, Di Staso M, Bonfili P, Vitturini A, Jannini EA, et al. 5-Azacitidine restores and amplifies the bicalutamide response on preclinical models of androgen receptor expressing or deficient prostate tumors. Prostate. 2010;70(11):1166–78.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):49–73.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Henig O, Kaye KS. Bacterial pneumonia in older adults. Infect Dis Clin North Am. 2017;31(4):689–713.
WHO WHO. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses [Available from: https://www.who.int/tools/atc-ddd-toolkit/atc-classification.
Davis DW, Lohr WD, Feygin Y, Creel L, Jawad K, Jones VF, et al. High-level psychotropic polypharmacy: a retrospective comparison of children in foster care to their peers on Medicaid. BMC Psychiatry. 2021;21(1):303.
DeCarlo K, Wallia A, Kang RH, Cooper A, Cherupally M, Harris SA, et al. Initiating second-line antidiabetic medication among older adults with type 2 diabetes on Metformin. BMC Geriatr. 2022;22(1):97.
Harrison SL, Bradley C, Milte R, Liu E, Kouladjian O’Donnell L, Hilmer SN, et al. Psychotropic medications in older people in residential care facilities and associations with quality of life: a cross-sectional study. BMC Geriatr. 2018;18(1):60.
Anderson TS, Jing B, Auerbach A, Wray CM, Lee S, Boscardin WJ, et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at Hospital Discharge. JAMA Intern Med. 2019;179(11):1528–36.
Varghese D. Ishida. C, Koya. HH. Polypharmacy: StatPearls; 2022.
Aggarwal P, Woolford SJ, Patel HP. Multi-Morbidity and Polypharmacy in Older People: Challenges and Opportunities for clinical practice. Geriatr (Basel). 2020;5(4).
Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:2042098620933741.
Abe T, Tamiya N, Kitahara T, Tokuda Y. Polypharmacy as a risk factor for hospital admission among ambulance-transported old-old patients. Acute Med Surg. 2016;3(2):107–13.
Chang TI, Park H, Kim DW, Jeon EK, Rhee CM, Kalantar-Zadeh K, et al. Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci Rep. 2020;10(1):18964.
Li Y, Zhang X, Yang L, Yang Y, Qiao G, Lu C, et al. Association between polypharmacy and mortality in the older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2022;100:104630.
Fialova D, Topinkova E, Gambassi G, Finne-Soveri H, Jonsson PV, Carpenter I, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293(11):1348–58.
Canaslan K, Ates Bulut E, Kocyigit SE, Aydin AE, Isik AT. Predictivity of the comorbidity indices for geriatric syndromes. BMC Geriatr. 2022;22(1):440.
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62(12):2261–72.
Herzig SJ, LaSalvia MT, Naidus E, Rothberg MB, Zhou W, Gurwitz JH, et al. Antipsychotics and the risk of Aspiration Pneumonia in individuals hospitalized for nonpsychiatric conditions: a Cohort Study. J Am Geriatr Soc. 2017;65(12):2580–6.
Rajamaki B, Hartikainen S, Tolppanen AM. Psychotropic Drug-Associated Pneumonia in older adults. Drugs Aging. 2020;37(4):241–61.
Miarons Font M, Rofes Salsench L. Antipsychotic medication and oropharyngeal dysphagia: systematic review. Eur J Gastroenterol Hepatol. 2017;29(12):1332–9.
Trifiro G, Gambassi G, Sen EF, Caputi AP, Bagnardi V, Brea J, et al. Association of community-acquired pneumonia with antipsychotic drug use in elderly patients: a nested case-control study. Ann Intern Med. 2010;152(7):418–25. W139-40.
Sun GQ, Zhang L, Zhang LN, Wu Z, Hu DF. Benzodiazepines or related drugs and risk of pneumonia: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2019;34(4):513–21.
Schindler JS, Kelly JH. Swallowing disorders in the elderly. Laryngoscope. 2002;112(4):589–602.
Juergens SM. Problems with Benzodiazepines in Elderly Patients. Mayo Clin Proc. 1993;68(8):818–20.
Obiora E, Hubbard R, Sanders RD, Myles PR. The impact of benzodiazepines on occurrence of pneumonia and mortality from pneumonia: a nested case-control and survival analysis in a population-based cohort. Thorax. 2013;68(2):163–70.
Hennessy S, Bilker WB, Leonard CE, Chittams J, Palumbo CM, Karlawish JH, et al. Observed association between antidepressant use and pneumonia risk was confounded by comorbidity measures. J Clin Epidemiol. 2007;60(9):911–8.
Chatterjee S, Carnahan RM, Chen H, Holmes HM, Johnson ML, Aparasu RR. Anticholinergic medication use and risk of Pneumonia in Elderly adults: a nested case-control study. J Am Geriatr Soc. 2016;64(2):394–400.
Comaty JE. Geriatric pharmacotherapy. The Tablet. 2015.
Knox S. Pneumonia Readmissions in older adults with dementia. Med Care. 2019;57(10):766–72.
Han J, Shen M, Wan Q, Lv Z, Xiao L, Wang G. Risk factors for community-acquired pneumonia among inpatients with mental disorders in a tertiary general hospital. Front Psychiatry. 2022;13:941198.
Haga T, Ito K, Sakashita K, Iguchi M, Ono M, Tatsumi K. Risk factors for pneumonia in patients with schizophrenia. Neuropsychopharmacol Rep. 2018;38(4):204–9.
Patterson SM, Cadogan CA, Kerse N, Cardwell CR, Bradley MC, Ryan C et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2014(10):CD008165.
Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, et al. An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing. 2004;33(6):612–7.
AGS AGS. American Geriatrics Society 2019 updated AGS Beers Criteria(R) for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–94.
Acknowledgements
The authors thank Dr. Samar Noureddine for peer-reviewing and proofreading the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
GA and KEA conceived and planned the experiment. MI collected the data. GD and KEA analyzed the data. GD created the result tables. GD and DD wrote the manuscript. GA and LA revised and amended the manuscript. LA prepared the figures and tables. GA supervised the project. All authors reviewed and approved the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the Code of Ethics of The World Medical Association (Declaration of Helsinki) and was approved by the Institutional Review Board at the American University of Beirut (Approval ID: BIO-2018-0094). The study was a retrospective record review after extracting de-identified data from the electronic healthcare records at the American University of Beirut Medical Center (AUBMC), so there were no identifiers collected that would enable the investigators to identify the participant, and informed consent was waived by the Institutional Review Board at the American University of Beirut.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Doumat, G., Daher, D., Itani, M. et al. The effect of polypharmacy on healthcare services utilization in older adults with comorbidities: a retrospective cohort study. BMC Prim. Care 24, 120 (2023). https://doi.org/10.1186/s12875-023-02070-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-023-02070-0