Abstract
Introduction
International and national guidelines highlight the need for general practitioner involvement during and after active cancer treatment and throughout long-term follow-up care. This paper aimed to evaluate patients’ acceptance of radiation oncology shared follow-up care using the Theoretical Framework of Acceptability (TFA).
Methods
This cross-sectional study was conducted at two cancer care centres in the Illawarra Shoalhaven region of Australia. A sample of patients scheduled for a radiation oncology follow-up consultation in 2021 were sent a 32-point self-complete paper-based survey. Data were analysed using descriptive, parametric and non-parametric statistical analysis. This paper followed the Checklist for Reporting of Survey Studies (CROSS).
Results
Of the 414 surveys returned (45% response rate), the acceptance for radiation oncology shared cancer follow-up care was high (80%). Patients treated with only radiotherapy were 1.7 times more likely to accept shared follow-up care than those treated with multiple modalities. Patients who preferred follow-up care for fewer than three years were 7.5 times more likely to accept shared care than those who preferred follow-up care for five years. Patients who travelled more than 20 minutes to their radiation oncologist or to the rural cancer centre were slightly more likely to accept shared care than those who travelled less than twenty minutes to the regional cancer centre. A high understanding of shared care (Intervention Coherence) and a positive feeling towards shared care (Affective Attitude) were significant predictive factors in accepting shared radiation oncology follow-up care.
Conclusion
Health services need to ensure patient preferences are considered to provide patient-centred cancer follow-up care. Shared cancer follow-up care implementation should start with patients who prefer a shorter follow-up period and understand the benefits of shared care. However, patients’ involvement needs to be considered alongside other clinical risk profiles and organisational factors. Future qualitative research using the TFA constructs is warranted to inform clinical practice change.
Similar content being viewed by others
Introduction
Once cancer patients complete active treatment, they require long-term follow-up to monitor for treatment-related side effects, recurrence, and psychosocial support [1,2,3]. The usual model of care is the hospital-based oncologist-led model [4, 5]. There is usually little formal involvement with the patient’s general practitioner in this model of care [6, 7]. While the oncologist-led model suits many patients, it may not always meet patients’ physical and psychosocial needs [8, 9]. For some patients, a shared care model might be more appropriate, tailored to their tumours, treatments, locality (metropolitan, regional or rural), access to specialists, and specific physical and emotional needs and preferences [10].
Shared care differs from the partial or whole transfer of care, where aspects of care are wholly transferred from the oncologist to another provider, such as a general practitioner. A shared cancer follow-up model of care harnesses the expertise of health professionals [11] and involves the explicit sharing of information and coordination of follow-up care [12]. Shared care is widely used in antenatal care and for managing patients with asthma, diabetes and ischaemic heart disease [13,14,15,16].
There is a growing body of evidence supporting the benefits of shared cancer follow-up models of care [17,18,19,20,21]. Randomised controlled trials have shown no difference in cancer recurrence rates or quality of life when a general practitioner is involved in follow-up care [22,23,24,25]. A shared cancer follow-up model of care offers several advantages to patients, health providers and health services. Patients generally find general practitioner appointments are more accessible than specialist appointments [26, 27]; there are fewer duplication of tests and clinical questions; reduced travel time; and more accessible parking [28, 29]. Benefits for general practitioners include increased knowledge and awareness of their patient’s overall health [30], addressing their patient’s unmet psychosocial needs [31], and improving relationships with specialists [32]. A shared care model benefits oncologists by allowing more time for newly diagnosed patients, patients on active treatment, advanced-stage and complex patients [33], and involvement in research and development activities. Additionally, the cost of shared cancer follow-up care to the health system is less than standard oncology follow-up care [34, 35].
A shared cancer follow-up model of care may vary for each medical discipline (medical oncology, radiation oncology, haematology, surgical) and tumour type (breast, prostate, head and neck, abdomen, lung, etcetera). For example, in one model for shared care for colorectal patients, the general practitioner and oncologist alternate the appointments quarterly [36]. In another model specific to radiation oncology shared follow-up care for breast, prostate and colorectal cancer patients, the radiation oncologist consultations cease entirely after three years after treatment, and patients see their general practitioner [37]. In that model the general practitioner follows a prescribed clinical follow-up assessment, and the radiation oncologist oversees and reviews the consultation results; this model is reliant on health technology and the two-way transfer of clinical information in real-time [37].
A core principle of shared cancer follow-up care is the acceptability of all parties: the oncologist, the general practitioner and the patient [38]. General practitioners are willing to accept a greater role in cancer follow-up care if there is improved information sharing and they are provided with clear clinical follow-up guidelines or protocols [39,40,41]. However, increased workload concerns remain [42,43,44]. Oncologists are more likely to prefer an oncologist-led model instead of a shared care or general practitioner-led model, as they feel they have the specialised knowledge for follow-up care [45]. However, oncologists are receptive to general practitioners taking a greater role in the more standardised aspects of follow-up care for low-risk patients [6], such as managing long-term and late side effects, blood tests and physical examinations. Several qualitative studies have found that patients appreciate their general practitioners taking a greater role in their long-term care [9, 29, 41, 46, 47].
Despite increasing evidence of the effectiveness of shared cancer follow-up care, data on implementation is limited. Treatment types (chemotherapy, immunotherapy, radiotherapy, surgery, etcetera) cause different short-term and long-term side effects [48], and differences in acceptance based on treatment type may help inform implementation. However, there is limited quantitative research on patients’ acceptance of a shared cancer follow-up model of care specific to radiation oncology patients, to allow generalisability to larger samples. This study aimed to evaluate patients’ acceptance of a shared cancer follow-up model of care between their general practitioner and radiation oncologist using the Theoretical Framework of Acceptability, in the Illawarra Shoalhaven Local Health District.
Methods
Study design, setting and participants
The Checklist Reporting of Survey Studies (CROSS) guided this study (Supplementary file 1). This cross-sectional study used a purpose-developed survey and was set in one regional, Illawarra Cancer Care Centre, and one rural, Shoalhaven Cancer Care Centre, Australia. This region provides health services for around 400,000 people, including radiotherapy-related services for over 6,000 distinct people for treatment and consultations annually. The study population was patients on a radiation oncology follow-up regime at one of these cancer centres in 2021.
In Australia, oncologists are guided by the American Society of Clinical Oncology, the National Comprehensive Cancer Network, and the National Institute for Clinical Excellence guidelines for follow-up care. Follow-up care is between five to 10 years, however, the actual frequency depends on the individual patient’s health, stage,treatment, and an oncologist’s individual approach.
Data sampling and data collection
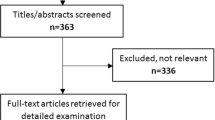
In 2021, there were 6,036 distinct patients scheduled for radiation oncology follow-up appointments in the study sites. We calculated that three-hundred and sixty-two completed surveys were required to obtain a 95% confidence interval, with a 5% margin of error. We anticipated a 40% response rate. This was assumed because paper-based surveys obtain response rates of 46% compared to online surveys of 36% [49], and we were using a mixture of the two. Therefore, we sent 950 paper-based surveys and patients could elect to return the paper survey in the prepaid envelope provided or complete the survey online using the provided Quick Response Code or weblink. A proportional stratified random sampling approach was employed based on years since treatment. Years since treatment strata were divided into < 1 year, 1–2 years, 3–4 years, 5 years, 6–10 years and > 10 years. The sample from each stratum was randomly selected using a Microsoft Excel formula to generate the participant list.
Survey
A 32-point survey was developed by the authors and comprised four sections: demographics, health and cancer-related information, access to healthcare, and acceptance of shared care. The options in the demographics, health and cancer-related information, and access to healthcare sections were adapted based on previous survey designs [50,51,52], and are described below.
Demographics: These included age, sex, postcode, country of birth, primary language spoken, ethnicity, relationship status, level of education, housing situation, employment status, and income.
Health and cancer-related information: The cancers with the highest incidence [48] (breast, prostate, lung, colorectal, pelvis and head and neck) were included, as well as an ‘Other’ option. Additional information included: the staging at diagnosis, the primary hospital where radiation oncology treatment was received, other treatments received, and years post active treatment. A five-point scale ranging from ‘Excellent’ to ‘Poor’ based on World Health Organisation recommendations [53] was used to measure self-reported health status.
Access to healthcare: Questions included whether the patient had a regular general practitioner, how often they visited their different doctors, the time required to travel to their doctors and the primary mode of transport, and how often they would like a consultation for their radiation oncology follow-up care, and how many years they would prefer follow-up care.
Acceptability of shared cancer follow-up care: Acceptance of shared care was based on the Theoretical Framework of Acceptability (TFA) [54]. The TFA is a multi-construct theoretical framework designed explicitly to assess the acceptability of healthcare interventions from the perspectives of the people who receive the intervention and those who deliver it [54]. The TFA can be applied quantitatively or qualitatively and used prior to a health intervention to form judgments about whether the participants expect the intervention to be acceptable or unacceptable. Assessment of anticipated acceptability prior to participation can highlight which aspects of the intervention could be modified to increase acceptability and thus, participation [54]. The seven constructs of the framework used to determine overall acceptability are Affective Attitude, Burden, Ethicality, Intervention Coherence, Opportunity Costs, Perceived Effectiveness and Self-efficacy. Questions were developed based on these constructs and measured using a five-point Likert scale from ‘Strongly disagree’ to ‘Strongly agree’ (see Table 1 for example).
The survey was refined with feedback from four general practitioners and two radiation oncologists. The survey included as few questions as possible to reduce the burden on patients and improve the response rate [55]. Readability was scored at Year Nine level, which is slightly higher than the Australian desired standard of Years Six to Eight [56]. The survey was piloted on ten follow-up patients and ten cancer centre staff for content validity. The average completion time was 4.5 minutes. The final version was available in printed form and online using Qualtrics XM.
Reliability and validity
Internal consistency reliability estimates how much total test scores would vary if slightly different items were used [57]. The reliability across the seven constructs was assessed by computing Cronbach’s α, with the minimum acceptable value of α = 0.70. The coefficients for the constructs totalled α = 0.78, indicating an acceptable level of internal consistency [58, 59]. Table 2 shows that the reliability would slightly improve if the Opportunity Costs construct were removed; however, the research team deemed the improvement small and did not delete it. The construct validity of the TFA constructs (that is, how accurately the constructs measure what they say they do) [60] was calculated with Pearson’s correlation coefficient of the patient’s responses to an item with their total scores. A validity coefficient above 0.35 is strongly valid [61], and all constructs were positively associated.
Statistical analysis
Data were analysed using the statistical software package SPSS version 29 [62]. Frequencies and percentages were calculated for categorical variables and reviewed for normality. Two forms of acceptance scores were generated. For the first, an average score across all TFA constructs, with opportunity scores reversed to align from a negative to a positive scale. A patient’s summated score was divided by the number of constructs constituting the scale, thereby creating a mean that falls within the range of the values for the response continuum options. All items comprising the construct’s scale were assumed to have equal weight when calculating a summated score. The second form of acceptance score was achieved by dichotomising the data into ‘Accept’ and ‘Not Accept’. The Accept score was generated from the ‘Strongly agree’ and ‘Agree’ response categories, and the Not accept score was generated from ‘Neither agree/disagree’, ‘Disagree’ and ‘Strongly disagree’. The dichotomised data were used to understand whether acceptance could be predicted based on any of the TFA categorical constructs (logistic regression).
Parametric tests included multinomial and ordinal logistic regression. If requirements for parametric test procedures were not met, non-parametric tests were used: Chi-Square, Kruskal Wallace Test and posthoc analysis. All tests were 2-sided; statistical significance was defined as p ≤ 0.05. Weighted adjustments were used to compensate for missing data.
Ethical consideration
Ethical approval for this study was obtained from the Joint University of Wollongong and Illawarra Shoalhaven Local Health District Human Research Ethics Committee. Patients were provided with a participant information sheet about the study’s aim and procedures and informed that consent was tacit upon completing the survey and that responses would be anonymised. Patients did not receive payment or an honorarium.
Results
Of the 950 surveys sent, 414 were returned (response rate of 45%); 371 had no missing data. Twenty-eight surveys were returned to sender (26 were no longer at that address, and two stated that the patient was deceased). Most (383 of 414) surveys were returned via post (92%). Patient demographics, health characteristics and healthcare access are presented in Table 3. Age and sex did not significantly influence a patient’s preference regarding their choice of follow-up care, and there were no significant socio-demographic variables on the acceptance for shared care.
One-third of the patients (n = 141, 34%) were treated with only radiotherapy, and two-thirds (n = 273, 66%) were treated with radiotherapy and chemotherapy and/or surgery. More patients reported their health as either ‘Excellent’ or ‘Very good’ (43.5%), followed by ‘Good’ (36.6%) and ‘Fair’ or ‘Poor health’ (19.9%). Almost all patients had a regular general practitioner (98%); 90% lived within a 20-minute drive of their general practitioner, and 40% lived within a 20-minute drive of their radiation oncologist.
Table 4 shows a high acceptance of radiation oncology shared care across the different tumour types. However, no statistically significant results were found with patient acceptance of shared care between the tumour group, cancer staging, or years since treatment.
Theoretical Framework of Acceptability Constructs
Table 5 shows patients’ acceptance for shared follow-up care across each construct in the Theoretical Framework of Acceptability. For Affective Attitude 85% agreed that they would be satisfied for their follow-up care to be shared with their general practitioner as long as the radiation oncologist was still involved. Ethicality: 88% agreed a shared cancer follow-up model fits with their values. Intervention Coherence: 88% agreed that they understood the benefits of shared cancer follow-up care for themselves, their doctors and the health care system. Perceived Effectiveness: 87% agreed that shared care was likely to achieve its purpose. Self-Efficacy: 75% elected to have shared follow-up care; sub-analysis showed 97% had confidence in their choice (p = < 0.001).
Acceptance and preferences for follow-up care
Patients treated with only radiotherapy were associated with an increase odds of accepting shared care, odds ratio 1.707 (95% CI 1.051–2.773), Wald χ2(1) = 4.668, p < 0.031. Additionally, patients who self-reported ‘Very good’ health had a statistically significant higher acceptance of shared care than those who self-reported their health as ‘Good’ (p = 0.008). However, health status was not a strong predictor of accepting shared care (χ2(4), 7.951, p = 0.093).
The majority of patients preferred to have their radiation oncology follow-up for five years (44%). Patients who preferred follow-up care for one year were 2.9 times more likely to accept shared care (p = 0.025), than those who wanted follow-up care beyond five years; and those who preferred follow-up care for three years were 7.5 times more likely to accept shared care (p = 0.012) than those who preferred care beyond five years.
Patients treated at the regional hospital were 1.8 times more likely to want follow-up care to continue for over 10 years (p = 0.027), and five times more likely to want follow-up for life (p = < 0.001), compared to patients treated at the rural hospital. These results align with travel time. Patients who travelled less than 20 minutes one-way to their radiation oncologist had a slightly lower acceptance for shared care (mean rank = 186.08, p = 0.025) than those who travelled more than 20 minutes (mean rank = 207.15, p = 0.025). Although not significant, patients treated at the rural hospital had a slightly higher average acceptability score of shared care (3.94/5 compared to 3.86/5 from the regional hospital).
Logistic regression predicted patients’ acceptance of shared care (see Table 6). Patients with a high understanding of shared care (Intervention Coherence) were predicted to be seven times more likely to accept a shared cancer follow-up model of care; those with a high Affective Attitude were predicted to be three times more likely; those with a high Ethicality were two and half times more likely; and those with high Self-Efficacy were three times more likely. Other constructs were not significant in predicting acceptance of shared care.
Discussion
This multi-centre cross-sectional study evaluated patients’ acceptance of a shared cancer follow-up model of care between their general practitioner and radiation oncologist using the Theoretical Framework of Acceptability (TFA). We found that 80% of patients accepted a radiation oncology shared follow-up model of care, and 75% would choose shared care compared to the oncologist-led model if given a choice. Patients treated only with radiotherapy were more likely to accept shared follow-up care, and patients who preferred follow-up care for fewer than three years were more likely to accept shared follow-up care. The TFA constructs of Intervention Coherence, Affective Attitude and Self Efficacy were significant predictors of acceptance for shared cancer follow-up care.
Previous qualitative research has found that patients are willing to accept shared cancer follow-up care if their oncologist remained remains involved and can oversee their care [6]. Although previous research does not distinguish between patients treated with only radiation therapy or other modalities, this study confirms that most radiation oncology patients would accept shared cancer follow-up care provided their radiation oncologist was still involved. However, the extent to how the oncologist was to remain involved was not explicitly addressed. It has been suggested that for the oncologist to remain involved and oversee the patient’s care, there is a need for improved two-communication and linkage of medical records between health professionals [6, 63].
Some patients require follow-up appointments with multiple specialists: radiation oncologist, medical oncologist, surgeon (for example, urologist, breast surgeon), and shared care has been highlighted as beneficial in reducing the number of appointments and duplication of assessments [6, 64]. However our results found that patients who only received radiotherapy treatment were more likely to accept shared follow-up care, and no significant difference with years since treatment was found. This is an interesting result, as patients treated with only one modality have fewer follow-up consultations than those treated with multiple modalities (who would be more likely to benefit from having fewer appointments). The higher acceptance for patients treated with only radiotherapy may be due to other unknown factors, such as long-term toxicity and treatment side effects and warrants further investigation.
To our knowledge, this is the first quantitative study to apply the TFA, which helped determine factors that may predict a patient’s acceptance of a radiation oncology shared follow-up model of care. Patients with good Intervention Coherence, Affective Attitude and Self-Efficacy were significantly more likely to accept a shared care model. Additionally, these constructs were also useful in predicting acceptance and could be useful for health services to undertake readiness assessments. This finding is also supported by the Social Cognitive Theory that goes beyond the individual behaviour (Health Belief Model and Theory of Reasoned Action/Planned Behaviour) and considers interactions with social and environmental influences. According to Bandura [65], if people lack awareness of how their lifestyle habits affect their health, they have little reason to change; conversely, knowledge creates the precondition for change [65]. Therefore, the knowledge and understanding (Intervention Coherence) regarding the benefits of shared cancer follow-up care is important to consider before transferring the care of patients to their general practitioner in a shared care model. This finding is also supported by a recent study that found women need to be provided with the evidence that shared follow-up care is effective, so they can form a thorough understanding (Intervention Coherence) of what shared is, who is responsible for what and to understand that shared care will not negatively impact their health outcomes [66]. The TFA allows researchers and health services to determine which constructs require further attention to increase acceptance before implementing health interventions.
Although there are several system barriers to implementing shared cancer follow-up care (such as the need for defined health professional roles [6], protocols, evidence-based guidelines [40, 46, 67], and communication tools [28]), acceptability to patients is fundamental. Our results support that shared cancer follow-up care needs to be individualised based on the patient’s cancer type, treatment type, current health, and personal preferences [50]. The American Society of Clinical Oncology suggested that “models of risk are needed to stratify survivors into different levels of intensity and setting for follow-up care. Components needed in such a model include risk recurrence, the persistence of moderate to severe toxicity or therapy, risk of serious physical late effects and psychosocial status" [68 p.634]. Another form of stratification to select appropriate patients for a shared care model beyond the clinical paradigm is to evaluate the patient’s acceptability toward shared care.
In addition to the risk stratification for cancer patients, essential elements for shared care include improved communication between the general practitioner and oncologist [32, 69, 70]. It is equally important to provide patient-centred care, including engaging with patients and understanding their needs and preferences [71]. We show that patients with a strong understanding (Intervention coherence) of the benefits of shared care are seven times more likely to accept a shared care follow-up model.
Study limitations
To our knowledge, this was the first study that used the Theoretical Framework of Acceptability quantitatively, and there is limited guidance on applying the framework in survey format. The study was specific to radiation oncology follow-up; some patients may have confused this with their medical oncology or surgical oncology follow-up. Although this study had a good response rate, there is no information about the 55% who declined to participate. It is possible that those who did not respond were less likely to accept shared cancer follow-up care, and response bias may be present. The authors were unable to conduct a non-report analysis. Additionally, there were few responses from colorectal cancer patients; this may be due to fewer colorectal cancer patients being treated with radiotherapy compared to breast and prostate patients. Finally, this study was conducted across a regional and rural population and may not be generalisable to the metropolitan population. However, based on our results, patients who travel less than 20 minutes to their oncologist were slightly less likely to accept shared care and may produce similar results in a metropolitan area where people live closer to cancer centres. The lead author is a critical realist researcher and acknowledges that many unobservable structures and events may influence the results.
Conclusion
There is a need to normalise shared cancer follow-up care into practice. However, normalising shared cancer care requires a multifaceted approach and support from specialists, general practitioners and patients. Based on the findings of this study, informing patients about the concept and benefits of shared care is important to foster acceptance. Follow-up care should be based on individual clinical risk and patient preference for follow-up care. Further investigation is needed to establish how the oncologist is to remain involved and oversee care in a shared care model, and to qualitatively research the acceptance among radiation oncologists, general practitioners and patients using the TFA constructs to inform clinical practice change.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Bernat J, Wittman D, Hawley S, Hamstra D, Helfand A, Haggstrom DA, et al. Symptom burden and information needs in prostate cancer survivors: a case for tailored long-term survivorship care. BJU Int. 2016;118:372–8. https://doi.org/10.1111/bju.13329.
Madarnas Y, Joy A, Verma S, Sehdev S, Lam W, Sideris L. Models of care for early-stage breast cancer in Canada. Curr Oncol. 2011;18:10.
McCabe M, Partridge A, Grunfeld E, Hudson M. Risk-based Health Care, the Cancer Survivor, the oncologist, and the primary care physician. Semin Oncol. 2013;40:804–12. https://doi.org/10.1053/j.seminoncol.2013.09.004.
Lewis R, Neal R, Williams N, France B, Hendry M, Russell D, et al. Follow-up of cancer in primary care versus secondary care: systematic review. Br J Gen Pract. 2009;59:e234–247. https://doi.org/10.3399/bjgp09X453567.
Gosain R, Miller K. Symptoms and symptom management in long-term cancer survivors. Cancer J. 2013;19:405–9. https://doi.org/10.1097/01.PPO.0000434391.11187.c3.
Schütze H, Chin M, Weller D, Harris MF. Patient, general practitioner and oncologist views regarding long-term cancer shared care. Fam Pract. 2018;35:323–9. https://doi.org/10.1093/fampra/cmx105.
Chan RJ, Emery J, Cuff K, Teleni L, Simonsen C, Turner J, et al. Implementing a nurse-enabled, integrated, shared-care model involving specialists and general practitioners in breast cancer post-treatment follow-up: a study protocol for a phase II randomised controlled trial (the EMINENT trial). Trials. 2020;21:855. https://doi.org/10.1186/s13063-020-04740-1.
Berendsen AJ, Roorda C, Jansen L, de Bock GH. Patients’ beliefs about the aims of breast cancer follow-up: a qualitative study. Maturitas. 2016;91:140–4. https://doi.org/10.1016/j.maturitas.2016.06.014.
Roorda C, de Bock GH, Scholing C, van der Meer K, Berger MY, de Fouw M, et al. Patients’ preferences for post-treatment breast cancer follow-up in primary care vs. secondary care: a qualitative study. Health Expect. 2015;18:2192–201. https://doi.org/10.1111/hex.12189.
Cancer Council Victoria and Department of Health Victoria. Optimal cancer care pathways 2021.
Cohen HJ. A model for the Shared Care of Elderly Patients with Cancer. J Am Geriatr Soc. 2009;57:300–2.
Rubin G, Berendsen A, Crawford SM, Dommett R, Earle C, Emery J, et al. The expanding role of primary care in cancer control. Lancet Oncol. 2015;16:1231–72.
Lucas C, Charlton K, Brown L, Brock E, Cummins L. Review of patient satisfaction with services provided by general practitioners in an antenatal shared care program. Aust Fam Physician. 2015;44:317–21. https://doi.org/10.3316/informit.139602351082165.
Drummond N, Abdalla M, Buckingham JK, Beattie J, a. G, Lindsay T, Osman LM, et al. Integrated care for asthma: a clinical, social, and economic evaluation. BMJ. 1994;308:559–64. https://doi.org/10.1136/bmj.308.6928.559.
Smith SM, O’Leary M, Bury G, Shannon W, Tynan A, Staines A, et al. A qualitative investigation of the views and health beliefs of patients with type 2 diabetes following the introduction of a diabetes shared care service. Diabet Med. 2003;20:853–7. https://doi.org/10.1046/j.1464-5491.2003.01071.x.
Sebern MD, Woda A. Shared Care Dyadic intervention: outcome patterns for heart failure Care Partners. West J Nurs Res. 2012;34:289–316. https://doi.org/10.1177/0193945911399088.
Grunfeld E. Cancer survivorship: a challenge for primary care physicians. Br J Gen Pract. 2005;55:741–2.
Grunfeld E, Levine MN, Julian JA, Coyle D, Szechtman B, Mirsky D, et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol. 2006;24:848–55. https://doi.org/10.1200/JCO.2005.03.2235.
Lund AS, Lund L, Jønler M, Graversen P, Bro F, Borre M. Shared care in prostate cancer: a three-year follow-up. Scand J Urol. 2016;50:346–51. https://doi.org/10.1080/21681805.2016.1206618.
Rychetnik L, Morton RL, McCaffery K, Thompson JF, Menzies SW, Irwig L. Shared care in the follow-up of early-stage melanoma: a qualitative study of australian melanoma clinicians’ perspectives and models of care. BMC Health Serv Res. 2012;12:468–76.
Bro F, Lund L, Morten J, Peter G, Michael B. To be followed up in general practice” - developing and implementing a shared care model for prostate cancer. Int J Integ Care. 2017;17:71–2.
Johnson CE, Saunders CM, Phillips M, Emery JD, Nowak AK, Overheu K, et al. Randomized Controlled Trial of Shared Care for patients with Cancer Involving General Practitioners and Cancer specialists. J Oncol Pract. 2015;11:349–55. https://doi.org/10.1200/JOP.2014.001569.
Ghezzi P, Magnanini S, Rinaldini M, Berardi F, Biagio GD, Testare F, et al. Impact of follow-up testing on Survival and Health-Related quality of life in breast Cancer patients: a Multicenter Randomized Controlled Trial. JAMA. 1994;271:1587–92. https://doi.org/10.1001/jama.1994.03510440047031.
Grunfeld E, Mant D, Yudkin P, Adewuyi-Dalton R, Cole D, Stewart J, et al. Routine follow up of breast cancer in primary care: randomised trial. BMJ. 1996;313:665–9.
Grunfeld E, Fitzpatrick R, Mant D, Yudkin P, Adewuyi-Dalton R, Stewart J, et al. Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: results from a randomized controlled trial. Br J Gen Pract. 1999;49:705–10.
Tan L, Gallego G, Nguyen TTC, Bokey L, Reath J. Perceptions of shared care among survivors of colorectal cancer from non-english-speaking and english-speaking backgrounds: a qualitative study. BMC Fam Pract. 2018;19. https://doi.org/10.1186/s12875-018-0822-6.
Brennan M, Butow P, Spillane AJ, Marven M, Boyle FM. Follow up after breast cancer - views of australian women. Aust Fam Physician. 2011;40:311–6.
Lisy K, Kent J, Piper A, Jefford M. Facilitators and barriers to shared primary and specialist cancer care: a systematic review. Support Care Cancer. 2021;29:85–96. https://doi.org/10.1007/s00520-020-05624-5.
Hall SJ, Samuel LM, Murchie P. Toward shared care for people with cancer: developing the model with patients and GPs. J Fam Pract. 2011;28:554–64. https://doi.org/10.1093/fampra/cmr012.
Dahlhaus A, Vanneman N, Guethlin C, Behrend J, Siebenhofer A. German general practitioners’ views on their involvement and role in cancer care: a qualitative study. J Fam Pract. 2014;31:209–14. https://doi.org/10.1093/fampra/cmt088.
Fok RW-Y, Low LL, Quah HMJ, Vasanwala F, Low SG, Soh LL, et al. Roles and recommendations from primary care physicians towards managing low-risk breast cancer survivors in a shared-care model with specialists in Singapore—a qualitative study. J Fam Pract. 2020;37:547–53. https://doi.org/10.1093/fampra/cmaa009.
Lizama N, Johnson CE, Ghosh M, Garg N, Emery JD, Saunders C. Keeping primary care “in the loop”: general practitioners want better communication with specialists and hospitals when caring for people diagnosed with cancer. Asia Pac J Clin Oncol. 2015;11:152–9. https://doi.org/10.1111/ajco.12327.
Vanhuyse M, Bedard PL, Sheiner J, Fitzgerald B, Clemons M. Transfer of follow-up care to family physicians for early-stage breast cancer. J Clin Oncol. 2007;19:172–6. https://doi.org/10.1016/j.clon.2007.01.115.
Emery JD, Jefford M, King M, Hayne D, Martin A, Doorey J, et al. ProCare Trial: a phase II randomized controlled trial of shared care for follow-up of men with prostate cancer. BJU Int. 2017;119:381–9. https://doi.org/10.1111/bju.13593.
Grunfeld E, Gray A, Mant D, Yudkin P, Adewuyi-Dalton R, Coyle D, et al. Follow up of breast cancer in primary care vs specialist care: results of an economic evaluation. Br J Cancer. 1999;79:1227–33.
Jefford M, Emery J, Grunfeld E, Martin A, Rodger P, Murray AM et al. SCORE: Shared care of Colorectal cancer survivors: protocol for a randomised controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-2245-4.
Sandell T, Schütze H, Miller A. A Shared cancer follow-up model of care between general practitioners and radiation oncologists for patients with breast, prostate, and colorectal cancer: protocol for a mixed methods implementation study. JMIR Res Protoc. 2021, 10(1): e21752. doi: 10.2196/21752
Koczwara B, White K, Emery J, Mitchell G, Mazza D, Yates P et al. Principles Statement: Shared Care. PC4 Cancer Research in Primary Care, Victoria, Australia; 2016.
Walter FM, Usher-Smith JA, Yadlapalli S, Watson E. Caring for people living with, and beyond, cancer: an online survey of GPs in England. Br J Gen Pract. 2015;65:e761–8. https://doi.org/10.3399/bjgp15X687409.
DiCicco-Bloom B, Cunningham RS. The experience of information sharing among primary care clinicians with cancer survivors and their oncologists. J Cancer Surviv. 2013;7:124–30. https://doi.org/10.1007/s11764-012-0253-7.
Laporte C, Vaure J, Bottet A, Eschalier B, Raineau C, Pezet D, et al. French women’s representations and experiences of the post-treatment management of breast cancer and their perception of the general practitioner’s role in follow-up care: a qualitative study. Health Expect. 2017;20:788–96. https://doi.org/10.1111/hex.12518.
Johnson CE, Lizama N, Garg N, Ghosh M, Emery J, Saunders C. Australian general practitioners’ preferences for managing the care of people diagnosed with cancer. Asia Pac J Clin Oncol. 2014;10:e90–98. https://doi.org/10.1111/ajco.12047.
Roorda C, Berendsen AJ, Haverkamp M, van der Meer K, de Bock GH. Discharge of breast cancer patients to primary care at the end of hospital follow-up: a cross-sectional survey. Eur J Cancer. 2013;49:1836–44. https://doi.org/10.1016/j.ejca.2013.01.016.
Greenfield DM, Absolom K, Eiser C, Walters SJ, Michel G, Hancock BW, et al. Follow-up care for cancer survivors: the views of clinicians. Br J Cancer. 2009;101:568–74. https://doi.org/10.1038/sj.bjc.6605160.
Cheung WY, Aziz N, Noone A-M, Rowland JH, Potosky AL, Ayanian JZ, et al. Physician preferences and attitudes regarding different models of cancer survivorship care: a comparison of primary care providers and oncologists. J Cancer Surviv. 2013;7:343–54. https://doi.org/10.1007/s11764-013-0281-y.
Anvik T, Holtedahl KA, Mikalsen H. When patients have cancer, they stop seeing me” -- the role of the general practitioner in early follow-up of patients with cancer -- a qualitative study. BMC J Fam Pract. 2006;7:1–9.
Hudson SV, Miller SM, Hemler J, Ferrante JM, Lyle J, Oeffinger KC, et al. Adult Cancer Survivors discuss follow-up in primary care: “Not what I want, but maybe what I need. Ann Fam Med. 2012;10:418–27. https://doi.org/10.1370/afm.1379.
Australian Institute of Health and Welfare. Cancer in Australia 2021 2021. https://doi.org/10.25816/YE05-NM50.
Ebert JF, Huibers L, Christensen B, Christensen MB. Paper- or web-based Questionnaire Invitations as a Method for Data Collection: cross-sectional comparative study of differences in response rate, completeness of data, and Financial cost. J Med Internet Res. 2018;20. https://doi.org/10.2196/jmir.8353.
Brennan ME, Butow P, Spillane AJ, Boyle FM. Survivorship care after breast cancer: follow-up practices of australian health professionals and attitudes to a survivorship care plan: breast cancer survivorship care survey. Asia Pac J Clin Oncol. 2010;6:116–25. https://doi.org/10.1111/j.1743-7563.2010.01286.x.
Kwan JYY, Croke J, Panzarella T, Ubhi K, Fyles A, Koch A, et al. Personalizing post-treatment cancer care: a cross-sectional survey of the needs and preferences of well survivors of breast cancer. Curr Oncol. 2019;26.
Young JM, Durcinoska I, DeLoyde K, Solomon MJ. Patterns of follow up and survivorship care for people with colorectal cancer in new South Wales, Australia: a population-based survey. BMC Cancer. 2018;18.
de Bruin A, Picavet HSJ, Nossikov A, editors. Health interview surveys: towards international harmonization of methods and instruments. Copenhagen: World Health Organization, Regional Office for Europe; 1996.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17. https://doi.org/10.1186/s12913-017-2031-8.
Kost RG, Correa da Rosa J. Impact of survey length and compensation on validity, reliability, and sample characteristics for Ultrashort-, Short-, and long-research participant perception surveys. J Clin Transl Sci. 2018;2:31–7. https://doi.org/10.1017/cts.2018.18.
Clinical Excellence Commission. NSW Health literacy Framework – 2019–2024. Sydney: Clinical Excellence Commission; 2019.
Salkind N. Encyclopedia of Research Design 2022. https://doi.org/10.4135/9781412961288.
Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess. 1995;7:309–19. https://doi.org/10.1037/1040-3590.7.3.309.
Henson RK. Understanding internal consistency reliability estimates: a conceptual primer on coefficient alpha. Meas Evaluation Couns Dev. 2001;34:177.
Odom LR, Morrow JR Jr. What’s this r? A Correlational Approach to explaining validity, reliability and objectivity coefficients. Meas Phys Educ Exerc Sci. 2006;10:137–45. https://doi.org/10.1207/s15327841mpee1002_5.
Oktavia R, Irwandi, Rajibussalim, Mentari M, Mulia IS. Assessing the validity and reliability of questionnaires on the implementation of indonesian curriculum K-13 in STEM education. J Phys: Conf Ser. 2018;1088:012014. https://doi.org/10.1088/1742-6596/1088/1/012014.
IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 29.0. Armonk, NY: IBM Corp.
Vuong K, Uebel K, Agaliotis M, Jun S, Taggart J, Suchy S, et al. Assessing suitability for long-term colorectal cancer shared care: a scenario-based qualitative study. Fam Pract. BioMed Central; 2020;21:1–8.
Baena-Cañada JM, Ramírez-Daffós P, Cortés-Carmona C, Rosado-Varela P, Nieto-Vera J, Benítez-Rodríguez E. Follow-up of long-term survivors of breast cancer in primary care versus specialist attention. J Fam Pract. 2013;30:525–32. https://doi.org/10.1093/fampra/cmt030.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13:623–49. https://doi.org/10.1080/08870449808407422.
White V, Der Vartanian C, Tansley F, Ugalde A. Understanding women’s perspectives and information needs about shared follow-up care for early breast cancer: a qualitative study. J Fam Pract. 2021;cmab048. https://doi.org/10.1093/fampra/cmab048.
Haq R, Heus L, Baker NA, Dastur D, Leung F-H, Leung E, et al. Designing a multifaceted survivorship care plan to meet the information and communication needs of breast cancer patients and their family physicians: results of a qualitative pilot study. BMC Med Inf Decis Mak. 2013;13. https://doi.org/10.1186/1472-6947-13-76.
McCabe MS, Bhatia S, Oeffinger KC, Reaman GH, Tyne C, Wollins DS, et al. American Society of Clinical Oncology Statement: Achieving High-Quality Cancer Survivorship Care. J Clin Oncol. 2013;31:631–40. https://doi.org/10.1200/JCO.2012.46.6854.
Aubin M, Vézina L, Verreault R, Fillion L, Hudon É, Lehmann F, et al. Family physician involvement in cancer care and lung cancer patient emotional distress and quality of life. Support Care Cancer. 2011;19:1719.
Hanks H, Harris M, Veitch C. Managing Colorectal Cancer: the General Practitioner’s roles. Aust J Prim Health. 2008;14:78–84.
Van Haitsma K, Abbott KM, Arbogast A, Bangerter LR, Heid AR, Behrens LL, et al. A preference-based model of care: an integrative theoretical model of the role of preferences in person-centered care. J Gerontol. 2020;60:376–84. https://doi.org/10.1093/geront/gnz075.
Acknowledgements
The authors thank the Radiation Oncology Service and Research Central at the Illawarra Shoalhaven Local Health District and thank Tiana-Lee Elphick} for their assistance with the data analysis.
Funding
TS is a recipient of an Australian Government Research Training Program scholarship and a top-up scholarship by the Radiation Oncology Service from the Illawarra Shoalhaven Local Health District. Award/Grant number is not applicable.
Author information
Authors and Affiliations
Contributions
TS, HS and AM contributed to the study conception and design. Ethics was prepared and submitted by TS and HS. Material preparation, data collection were performed by TS. Research Central supported TS with the statistical analysis. TS prepared the first draft of the manuscript and all authors (HS, AM and RI) contributed to subsequent revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Joint University of Wollongong and the Illawarra Shoalhaven Local Health District Human Research Ethics Committee, 2020ETH00301. The respondents were informed by a written formal cover letter about the study, including purpose, confidentiality, voluntariness, and anonymity. Returning the completed survey was interpreted as informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sandell, T., Schütze, H., Miller, A. et al. Patients’ acceptance of a shared cancer follow-up model of care between general practitioners and radiation oncologists: A population-based survey using the theoretical Framework of Acceptability. BMC Prim. Care 24, 86 (2023). https://doi.org/10.1186/s12875-023-02032-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-023-02032-6