Abstract
Background
Behavioral treatments can augment the success of pharmacotherapy in smoking cessation. The aim of this study was to compare smoking quit rates between patients receiving individual counseling with their general practitioner during office visits or intensive counselling with behavioral support, both augmented by varenicline.
Methods
A nationwide retrospective cohort study conducted in a large Healthcare Maintenance Organization in Israel. We selected randomly patients who filled a prescription for varenicline and received either individual consulting by their general practitioner or intensive counselling with behavioural support, and asked them to answer a questionnaire. The outcome variables were smoking cessation 26–52 weeks following the beginning of treatment and satisfaction with the process.
Results
870 patients were contacted and 604 agreed to participate (a response rate of 69%); 301 patients in the general practitioner group, 300 in the intensive counselling group and 3 were excluded due to missing date. The quit rate was 36.5% in the general practitioner group and 42.3% in the intensive counselling group (P = 0.147). In a logistic regression analysis, controlling for age, gender, socioeconomic status, ischemic heart disease, chronic obstructive pulmonary disease, pack years and duration of varenicline consumption, the adjusted OR for quitting in the general practitioner group was 0.79 (95% CI 0.56,1.13). The adjusted OR was higher in the group with the highest socioeconomic status at 2.06 (1.39,3.07) and a longer period of varenicline consumption at 1.30 (1.15,1.47). Age, gender and cigarette pack-years were not associated with quit rate. In the general practitioner group 68% were satisfied with the process, while 19% were not. In the intensive counselling group 64% were satisfied and 14% were not (P = 0.007).
Conclusion
We did not detect a statistically significant difference in smoking quit rates, though there was a trend towards higher quit rates with intensive counselling.
Similar content being viewed by others
Background
As the leading cause of early death and preventable diseases worldwide, smoking is a global concern [1, 2]. The worldwide prevalence of daily smoking is 25%, [3] compared to a smoking rate of 20.5% in the adult population in Israel [4].
Therapeutic modalities for smoking cessation
Therapeutic modalities for smoking cessation include behavioral and pharmacological therapy. Behavioral treatment options include brief guidance by the general practitioner (GP), intensive counselling workshops (usually moderated by nurses), personal telephone consultations, and web-based programs. A Cochrane review from 2021, that assessed the effect of behavioral interventions to support smoking cessation, concluded that all forms of counselling were effective, with more pronounced effect in the absence of pharmacotherapy [5]. Drug options include varenicline, an α4β2 nicotinic acetylcholine receptor partial agonist, sustained release bupropion, a norepinephrine and dopamine reuptake inhibitor, and nicotine replacement therapy (NRT) [6]. Behavioral treatment is recommended as support therapy for people using pharmacotherapy, [7, 8] as it increases quit rates by 10–20% [9].
GP counselling vs. intensive workshops
There is a paucity of evidence regarding the effectiveness of brief counselling session provided by the patient’s personal GP, compared with intensive workshops. A randomized, controlled trial conducted in the Netherlands, compared these two modalities, both augmented with varenicline, and found similar quit rates with GP counselling, compared to nurse-moderated intensive workshops. The quit rates were 39% vs. 32.2% at 9–26 weeks following the intervention, and 28.8% vs. 25.5% at 9–52 weeks following the intervention, respectively [10]. A study from the US compared counselling by nurses with counselling by GPs and found a non-significant (NS) trend towards better quit rates with nurses (29.1% vs. 18.2%) [11]. A Cochrane review from 2017 compared individual counselling with no counselling (or brief counselling) and also more intensive counselling interventions with less intensive interventions [12]. Results showed that individual counselling is better than minimal contact control and that more intensive counseling is better than less intensive counselling. In both cases, all patients received NRT or bupropion.
Smoking cessation in Israel
In 2010 smoking cessation workshops became available, free of charge, to all smokers in Israel, through all Israeli health maintenance organizations (HMOs) [13]. Varenicline and bupropion were offered at reduced cost to smokers who attended smoking-cessation workshops. Starting in 2015, NRT was also offered at a reduced cost as a second line treatment for smokers who attended the workshops. Starting in 2019, varenicline and bupropion were also available at reduced cost to smokers who were counselled by their GPs [14].
Over the past 10 years the number of patients attending intensive counseling workshops in Israel has increased by 230% from 11,844 persons in 2010 to 27,342 persons in 2017.
Maccabi Healthcare Services (MHS), the second largest HMO in Israel, offers different smoking cessation programs including eight 90-minute meetings in an intensive workshop, usually led by a nurse, personal telephone counselling delivered through six 30-minutes calls, and per-request GP smoking cessation counselling. GPs were invited to a short smoking cessation counselling training, in which they were advised to provide three smoking counselling sessions for each patient; however, it was not mandatory to provide all three. GPs were paid for smoking cessation counselling by the HMO once for each patient, regardless of the number of consultations that were actually done. We therefore assumed that each patient received between 1 to 3 sessions (the estimated duration of a session was 10–15 minutes). All these options can be augmented by pharmacotherapy, often with varenicline, which is the drug of choice because of its good efficacy and safety profiles [15, 16].
In light of the health policy change made in 2019, the aim of this study was to compare the effectiveness of smoking cessation by GP office visits (GP group) with intensive counselling (behavioral support; workshops or personal telephone support) (IC group), in both cases augmented by varenicline. The secondary aim was to compare patients’ satisfaction with the different programs.
Methods
Study design and setting
We designed a nation-wide retrospective cohort study using the MHS database. We identified patients who filled a prescription for varenicline from October 2019 to September 2020, and divided them to two groups according to the smoking cessation program they used: patients who participated in group workshops or received personal telephone sessions were included in the IC group, while patients who received smoking cessation counselling from their GP were included in the GP group.
Patients in both groups were selected randomly. We sent text messages to all patients 26 to 52 weeks after they first purchased varenicline, with a request to complete an online questionnaire to assess their smoking status. Text messages were sent in October 2020 and again in March 2021. Patients who did not respond were contacted by telephone between November 2020 and April 2021.
Variables
The outcome variables were (a) quit rate, using an ordinal scale of 0–3 (0 – does not smoke, 1 – smokes rarely, 2 – smokes every day, but less than before, and 3 – smokes as much as before) and (b) satisfaction with the smoking cessation process using a 5-point Likert scale (1 = very dissatisfied, 5 = very satisfied). The quit rate was later reduced to a binary variable with patients who said they did not smoke at all categorized as non-smokers and the others categorized as smokers. Smoking status variable described the patient’s abstinence status from the pharmacological treatment until the time that the questionnaire was answered. Data for both variables were collected by patient self-report; no biochemical confirmation was obtained.
Behavioural support for smoking cessation, either intensive counselling or GP counselling, served as the exposure variable. Data were extracted from the electronic records and verified using patient self-report.
Confounder variables included sociodemographic data such as gender, age and socioeconomic status (SES); medical data including comorbid diseases such as diabetes mellitus type 2 (DMt2), hypertension, ischemic heart disease (IHD), chronic obstructive pulmonary disease (COPD), a history of malignancy; and smoking-related variables including cigarettes per day, duration of smoking in years and duration of treatment with varenicline in months. All sociodemographic and medical variables were obtained from the electronic medical records. All smoking related variables were obtained by patient self-report.
Sample size
MHS proactively follows workshop participants with an 80% quit rate at the end of the workshop, and a 45% quit rate 1 year after the workshop. Accordingly, we assumed a quit rate of 45% in the IC group and considered a difference of 5% or less as non-inferior. 301 patients for each group were required for a significance level of 5% with a power of 80% in a 2-sided test. The sample size was calculated using the WinPepi software, v11.65.
Statistical analysis
Descriptive statistics were used for all variables, with absolute numbers and percentages for categorical variables and mean and standard deviation for continuous variables. The chi-square test was used for univariate analyses of categorical variables. Student’s t-test was used for normally distributed continuous variables and the Mann-Whitney test for continuous variables which did not distribute normally. We performed a multivariate logistic regression analysis including variables with statistically significant associations with the outcome variables in univariate analyses, with the addition of smoking cessation group, age and gender regardless of the results of the univariate analysis. For null findings, we used the Bayes Factor to demonstrate that no association is a real finding and that the evidence supports the null hypothesis [17]. A Bayes Factor of less than 0.3 is considered substantial evidence to support the null hypothesis. We calculated a non-inferiority margin of 0.815, based on an assumption of 5% delta and a quit rate of 45% in the IC group. We used the Statistical Package for Social Sciences (SPSS) software version 27 for data analysis, and BayesFactor package in the R statistical programming environment to calculate the Bayes factor.
Ethical considerations.
All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was given via the online questionnaire or orally during telephone calls. The local ethics committee (IRB) of MHS approved this study (ID 0062–20-MHS).
Results
Study population
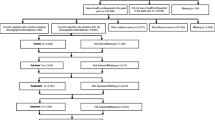
From October 2019 to September 2020, 3817 patients fulfilled prescriptions for varenicline in MHS, 3066 (80.3%) received intensive behavioural support (by workshop or telephone), and 751 (19.7%) received GP counselling. We randomly sampled 435 patients from each group to participate in our survey. We sent the study questionnaire via text message and later conducted phone interviews with those who did not respond to the text messages. 604 patients (69%) agreed to participate in the study. Three patients were excluded due to missing data on behavioural counselling. Of the 601 patients who were included in the study, 300 were in the IC group and 301 in the GP group. The two groups were similar in gender and SES distribution, but patients in the IC group were older (47.4 vs. 44.7 years, P = 0.007) and smoked more (26.1 vs. 22.6 years, P < 0.001) (Table 1).
Quit rates
The quit rate for the GP group was 36.5% and for the IC group 42.3% (P = 0.147). The crude odds ratio (OR) for success in the GP group was 0.78 (0.56, 1.09) (Table 2). A test of association yielded a Bayes factor of 0.117 in support of the conclusion that there is no relationship between study group and outcome.
In a logistic regression analysis, controlling for age, gender, SES, IHD, COPD, number of cigarettes per day and duration of varenicline consumption, no significant difference in quitting odds was found between the IC group and the GP group. The adjusted OR (aOR) for GP group quitting was 0.79 (0.56, 1.13) with a Bayes Factor of 0.1 (Table 2). Non-inferiority could not be proven and the result is inconclusive.
For the entire study population, significantly higher aORs for quitting were found in the highest SES group with an aOR of 2.06, (1.39,3.07) and with a longer duration of varenicline consumption with an aOR of 1.30 (CI 1.15,1.47). Patients with COPD had an insignificantly higher aOR of 2.46 (0.96,6.30). Age, gender, and number of cigarettes per day were not associated with quit rate.
Satisfaction
In the entire study population, satisfaction was significantly higher for patients who stopped smoking (82%) compared with those who continued smoking (35%) (P < 0.001). In the GP group, 68% of the participants were satisfied (57% very satisfied and 11% satisfied), while only 19% were not satisfied or not satisfied at all. In the IC group 64% were satisfied (51% very satisfied and 13% satisfied) and 14% were not satisfied or not satisfied at all. The proportion of participants who were neither satisfied nor dissatisfied was higher in the IC group (23% vs 14%) (P = 0.007).
Discussion
Summary
We conducted a retrospective nation-wide cohort study to assess the difference in quit rates using two counselling styles, brief GP counselling during an office visit or intensive counselling, in both cases augmented by varenicline. We report a non-significant lower quit rate in the GP group compared with the IC group (36.5% vs. 42.3% respectively), with an aOR of 0.79 (0.56,1.13). Non-inferiority could not be proven, and the result was inconclusive. In the entire study group, we found a higher satisfaction rate for quitters compared with patients who continued smoking (82% vs. 35%) and for the GP group compared with the IC (68% vs. 64%).
Strengths and limitations
The strengths of this study are its relatively large sample size, the high response rate (69%) and the heterogeneity of the participants and the large number of health providers personnel (GPs and nurses). Another strength is the observational design that provided real-world results, as the smoking cessation counsellors and the patients were not aware of being observed, they behaved as they usually do. This design eliminated a possible Hawthorne effect.
This study has several limitations. Being an observational study, compared with a randomised controlled trial study, exposes the study to selection bias. Patients who chose to attend an intensive counselling group might have had different characteristics from those who chose GP counselling. In order to overcome this bias, we compared the groups and checked for differences that might have impacted the outcomes, including comorbidities (Table 1). We also compared basic differences between patients who chose to attend the study and those who refused to take part (Table 3). In addition, we did not enquire regarding baseline psychological factors that might have influenced the outcomes. Another limitation is lack of uniformity of GP counselling, which could vary between merely providing a prescription to repeated counselling sessions. Although the study had a relatively large sample size, it was inadequate to prove a significant association (or lack of it) in quitting rates between the two groups. Last, as a retrospective study, the information which was provided in the questionnaire, including self-reported quitting status might have been biased.
Comparison with existing literature
GP group vs. IC group
A similar study, from the Netherlands compared nurses-led intensive counselling to GP brief counselling. The nurses-led group included 3 face-to-face and 7 telephone sessions, mostly done by the first 13 weeks of the quitting attempt. In the GP group, patients had at least one visit for smoking cessation with their GP and received a prescription for varenicline. This study found a non-significant trend in favor of the GP group compared with a nurses-led group, with a quit rate of 39% vs. 32.2% respectively [10]. There are two differences between the Dutch study and the present one that might explain the opposite trends that were found: (a) the Dutch study was a randomized controlled trial, while the current study was a retrospective cohort, and (b) the Dutch study used chemical validation to check smoking abstinence while the current study relied on self-report. The lack of a significant difference in both the Dutch study and the present one suggests that these types of behavioral therapy support have a similar effect when augmented with varenicline.
A Cochrane review of eight RCTs (2048 patients), that compared more intensive to less intensive counselling, found a relative effect of 1.26 [95% CI 1.04–1.52] in favor of the more intensive counselling, however the patients in seven of these studies were treated with NRT, and with a combination of NRT and bupropion in one study, none were treated with varenicline [12]. The different result of the present study may result from the different pharmacological treatment.
MHS offers its patients intensive counselling groups free of charge, but they had to actively register for the workshop. On the other hand, GP counselling starts during a regular office visit with the patient’s personal GP, often initiated by the physician during an appointment set for other purposes. This may result in a selection bias where patients in the intensive counselling group are more likely to be at a more advanced Prochaska’s stage [18]. According to Prochaska’s model there are five stages in the change process: pre-contemplation, contemplation, and preparation for people who currently smoke; and action and maintenance for those who have quit. Interventions which require action, are more effective in the advanced stages [19,20,21]. On the other hand, in MHS the patients had long relationship with their personal GP, who usually knew them well, and had the opportunity to offer assisted quitting in good timing, and was also available for further counselling and support.
Another possible explanation for the differences in quit rates between the two groups is differences in patients’ characteristics in each group; the patients in the intensive counselling group were older and smoked more. In a recent cohort study, smoking cessation success was significantly associated with older age and fewer years of smoking [22]. No association was found with the number of cigarettes that were smoked per week. In our multivariate analysis, age and pack-years, which may be equivalent to years of smoking, were not associated with successful quitting.
Our study demonstrated a relatively higher quit rate for both groups, compared with previous publications on the effectiveness of varenicline [15, 16]. This could be related to self-reported quit status, without chemical validation of abstinence; however, it has been shown that self-reported smoking status was a reliable measure [23,24,25,26,27,28].
The multivariate analysis, demonstrated that patients with higher SES had a higher odds ratio for quitting, which is consistent with the results of previous studies [29,30,31].
Satisfaction with the process
We found greater satisfaction in the GP group, in contrast to the findings of the Dutch study, where a higher degree of satisfaction was seen in the nurses-led group. This difference may result from the different study designs, i.e., a retrospective cohort vs. a randomized control trial. Patients in the current study chose whether to actively attend a workshop, or to rely solely on the counselling of their GP, a possible source of selection bias that could have affected satisfaction from the process as well. The lower proportion of participants, who were neither satisfied nor dissatisfied in the GP group (14% vs 23%), might indicate a higher level of emotional engagement with their personal GP compared with a smoking cessation counselor, with whom they had no prior familiarity.
Conclusion
This study did not find that office-visit smoking cessation counselling was significantly different from intensive behavioral therapy when augmented by varenicline. However, the results of non-inferiority were inconclusive. This finding should encourage GPs to deepen their knowledge regarding smoking cessation counselling and to offer this counselling during regular visits. Randomized controlled trials are required in order to further validate the results of this study in a controlled environment.
Availability of data and materials
The data that support the findings of this study are available from Limor Adler (the corresponding author) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the local ethics committee of MHS.
Abbreviations
- GP:
-
General practitioner
- IC:
-
Intensive counselling
- NRT:
-
Nicotine replacement therapy
- NS:
-
Non-significant
- HMOs:
-
Health maintenance organizations
- MHS:
-
Maccabi Healthcare Services
- SES:
-
Socioeconomic status
- DMt2:
-
Diabetes mellitus type 2
- IHD:
-
Ischemic heart disease
- COPD:
-
Chronic obstructive pulmonary disease
- OR:
-
Crude odds ratio
- aOR:
-
Adjusted odds ratio
References
Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013 23(2):103–12.
WHO global report: mortality attributable to tobacco. https://www.who.int/publications/i/item/9789241564434. Accessed Oct 2021.
GBD 2015 Tobacco Collaborators, Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885–906.
Smoking status in Israel, 2017 [internet]. The Israeli ministry of Health. 2018 [cited 2021 May 23]. Available from: https://www.health.gov.il/PublicationsFiles/smoking_2017.pdf
Hartmann-Boyce J, Livingstone-Banks J, Ordóñez-Mena JM, Fanshawe TR, Lindson N, Freeman SC, et al. Behavioural interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev. 2021;1:CD013229.
Lindson N, Klemperer E, Hong B, Ordóñez-Mena JM, Aveyard P. Smoking reduction interventions for smoking cessation. Cochrane Database Syst Rev. 2019 ;30(9):CD013183.
West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Thorax. 2000 ;55:987–99.
Clinical practice guideline treating tobacco use and dependence 2008 update panel, liaisons, and staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008 ;35(2):158–76.
Hartmann-Boyce J, Hong B, Livingstone-Banks J, Wheat H, Fanshawe TR. Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database Syst Rev. 2019;6:CD009670.
van Rossem C, Spigt M, Viechtbauer W, Lucas AEM, van Schayck OCP, Kotz D. Effectiveness of intensive practice nurse counselling versus brief general practitioner advice, both combined with varenicline, for smoking cessation: a randomized pragmatic trial in primary care. Addiction. 2017 ;112:2237–47.
Byers MA, Wright P, Tilford JM, Nemeth LS, Matthews E, Mitchell A. Comparing smoking cessation outcomes in nurse-led and physician-led primary care visits. J Nurs Care Qual. 2018;33(3):272–8.
Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2017 ;31(3):CD001292.
Rosen LJ, Peled-Raz M. Tobacco policy in Israel: 1948-2014 and beyond. Isr J Health Policy Res. 2015 ;1(4):12.
Expansion of the National Basket of Health Services, 2019 [Internet]. The Israeli Ministry of Health. [cited 2021 Available from: https://www.health.gov.il/hozer/mk01_2019.pdf
Jorenby DE, Hays JT, Rigotti NA, Azoulay S, Watsky EJ, Williams KE, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):56–63.
Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):47–55.
Dienes Z. Using Bayes to get the most out of non-significant results. Front Psychol. 2014 ;29(5):781.
Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychother: Theory, Research & Pract. 1982;19(3):276–88.
Prochaska JO. Flaws in the theory or flaws in the study: a commentary on “the effect of Transtheoretical model based interventions on smoking cessation”. Soc Sci Med. 2009 ;68(3):404–6.
DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991 ;59(2):295–304.
Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983 ;51(3):390–5.
Holm M, Schiöler L, Andersson E, Forsberg B, Gislason T, Janson C, et al. Predictors of smoking cessation: a longitudinal study in a large cohort of smokers. Respir Med. 2017 ;132:164–9.
Rebagliato M. Validation of self reported smoking. J Epidemiol Community Health. 2002 ;56(3):163–4.
Wells AJ, English PB, Posner SF, Wagenknecht LE, Perez-Stable EJ. Misclassification rates for current smokers misclassified as nonsmokers. Am J Public Health. 1998 ;88:1503–9.
Pérez-Stable EJ, Marín G, Marín BV, Benowitz NL. Misclassification of smoking status by self-reported cigarette consumption. Am Rev Respir Dis. 1992 ;145(1):53–7.
Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994 ;84(7):1086–93.
Noonan D, Jiang Y, Duffy SA. Utility of biochemical verification of tobacco cessation in the Department of Veterans Affairs. Addict Behav. 2013 ;38(3):1792–5.
Maclaren DJ, Conigrave KM, Robertson JA, Ivers RG, Eades S, Clough AR. Using breath carbon monoxide to validate self-reported tobacco smoking in remote Australian indigenous communities. Popul Health Metrics. 2010 ;8(1):2.
Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M, ITC Collaboration. Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the international tobacco control four country survey. Nicotine Tob Res. 2010 ;12(Suppl):S20–33.
Cambron C, Lam CY, Cinciripini P, Li L, Wetter DW. Socioeconomic status, social context, and smoking lapse during a quit attempt: an ecological momentary assessment study. Ann Behav Med. 2020;54(3):141–50 Feb.
Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012 ;1248:107–23.
Acknowledgments
none.
Funding
Pfizer has provided LA an independent grant for this study, # 65254759.
Author information
Authors and Affiliations
Contributions
IY conceptualized the work, was a major contributor to data collection and reviewed and revised the manuscript. LA conceptualized the work, analyzed and interpreted the data and wrote the initial manuscript. SAH conceptualized the work and reviewed and revised the manuscript. MMR helped with the changes asked by the reviewers and reviewed and revised the manuscript. AB analyzed and interpreted the data and reviewed and revised the manuscript. KO was responsible for data collection and reviewed and revised the manuscript. GZ analyzed and interpreted the data and wrote the initial manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local ethics committee (IRB) of Maccabi Healthcare Services approved this study (ID 0062–20-MHS). Informed consent was given via the online questionnaire or orally during telephone calls. These methods of obtaining informed consent were approved by the ethical committee of Maccabi Healthcare Services. When the interviews were made using telephone calls, and since no personal details were documented, a verbal consent was sufficient. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yehoshua, I., Adler, L., Hermoni, S.A. et al. Smoking quit rates among patients receiving pharmacotherapy who received general practitioner counselling versus intensive counselling: a retrospective cohort study. BMC Prim. Care 23, 340 (2022). https://doi.org/10.1186/s12875-022-01953-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01953-y