Abstract
Background
Musculoskeletal pain is one of the leading complaints in the ambulatory setting. There are many ways to treat it, including pharmacologic and non-pharmacologic approaches. Dry needling (DN) is an option that is easy to learn, cheap and has a good safety profile. The aim of this study was to assess the association between DN performed by GPs for acute myofascial pain syndrome (MPS) and pain relief and to evaluate factors associated with treatment success.
Methods
In this prospective cohort study, two GPs performed DN in their clinics. Patients were asked to rank their pain using the Short-Form McGill Pain Questionnaire (SF-MPQ) before, 10-min and 1-week after the procedure. The SF-MPQ index consists of 3 parts; visual analog scale (VAS), pain rating index (PRI) and present pain intensity (PPI).
Logistic regressions were performed to assess the variables associated with short- and medium- term success.
Results
Fifty two patients were recruited from September 2019 until August 2020. VAS was 6.0 ± 2.3 (before), 4.1 ± 2.5 (10-min after) and 2.6 ± 2.71 (1-week after), P < 0.05. PRI was 17 ± 9.1 (before), 10.8 ± 8.5 (10-min after) and 5.1 ± 6.5 (1-week after), P < 0.05. PPI was 2.6 ± 1.0 (before), 1.7 ± 1.0 (10-min after) and 1.1 ± 1.2 (1-week after), P < 0.05.
Short-term success was associated with the physician who performed the procedure (OR 10.08, 95% CI 1.15,88.4) and with the use of a single needle (vs. multiple needles inserted) (OR 4.55, 95% CI 1.03,20.11). Medium-term success was associated with being a native born (non-immigrant), OR 8.59, 95% CI 1.11,66.28 and with high level of initial pain, OR 11.22, 95% CI 1.82,69.27.
Conclusion
Our study demonstrated improvement in acute pain 10-min and 1-week after DN performed by a GP, in all parts of the SF-MPQ. Therefore, we believe DN is a good therapeutic option for GPs to aid patients suffering from MPS.
Similar content being viewed by others
Background
Pain is one of the leading complaints in the ambulatory setting. The Global Burden of Diseases, Injuries, and Risk Factors Study 2019 demonstrated that low back pain, neck pain and other musculoskeletal pain complaints are the leading causes of morbidity globally in terms of years lived with disease [1]. Musculoskeletal pain is one of the most frequent complaints in general practitioners’ (GPs) clinics [2].
Myofascial pain syndrome (MPS) is a potential cause of musculoskeletal pain [3]. MPS is defined as a regional pain characterized by the presence of myofascial trigger points (MTrPs) [4, 5, 3]. MtrPs is a hyperirritable palpable nodule in the skeletal muscle fibers that can produce local or referred pain. There are many ways to treat MPS, including pharmacologic and non-pharmacologic approaches [6]. Dry needling (DN) is an option that is easy to learn, cheap and has a good safety profile [7]. DN is performed by inserting a needle into MtrPs located in skeletal muscles. It is a simple method to deal with pain in the physician’s office.
The effectiveness of DN was examined in many studies. Most systemic reviews and meta-analysis recommended DN for treating acute and chronic pain in patients with temporomandibular joint dysfunction [8], upper-quarter myofascial pain [9], upper trapezius pain [10], neck and shoulder pain [11,12,13,14,15], elbow pain [16], low back pain [17,18,19], knee pain [20], and plantar fasciitis [21]. On the other hand, some studies have shown no efficacy for DN treatment in MPS [22], specifically in the neck [23] and upper extremities [24].
Side effects of dry needling include minor adverse events such as mild bleeding (16%), bruising (7.7%) and pain during DN (5.9%). Major adverse events such as pneumothorax or hemothorax are rare (< 0.1%) [7].
In 2015, the Israeli society of Musculoskeletal Medicine released a position paper concerning intra-muscular stimulation (IMS), written by six experts, using the Delphi procedure [25]. The general statement agreed upon was “IMS is one of the preferred treatments for MPS. The treatment is evidence-based, effective, safe, and inexpensive. The position of the Israeli Society of Musculoskeletal Medicine is that the treatment should be taught and used by all GPs and those physicians in other areas of medicine who deal with pain in their work.”
In 2017, Maccabi Healthcare Services, the second largest health maintenance organization (HMO) in Israel, launched DN courses for GPs. The basic course consists of 3 sessions of 10 academic hours each. Every GP who attends the course is afterwards certified to treat their patients with DN. Since, there has been an increase in the number of certified physicians, from 107 in 2017 to 199 in 2020 as well as an additional increase in the number of DN procedures, from 7,644 in 2017 to 10,647 in 2020 (a slight decrease compared to 2019, during which 12,088 DN procedures were done; this decrease might be due to the COVID-19 effect).
The aim of this study was to assess the association between DN performed by GPs for acute MPS and short- and medium-term pain relief. Secondary aim was to evaluate factors that are associated with treatment success.
Methods
Study design
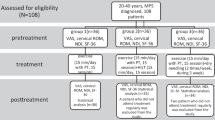
This is a prospective cohort study. Two GPs who regularly treat patients with DN in their clinics invited eligible patients to participate in the study. Participation was voluntary and patients who refused to take part were still treated with DN. Patients who agreed to take part in the study were given full explanation on the procedure of DN and possible side effects and signed a written informed consent statement. Patients were asked to rank their pain using the Short-Form McGill Pain Questionnaire (SF-MPQ) before, 10 min after and 1 week after the procedure. The study was approved by the ethical committee of Bait Balev (the institutional review board), ID 0017–19-BBL. All data was saved anonymously.
Setting
DN was performed by two GPs, one is a specialist with 3 years of experience with DN and 8 years working in the same clinic and the other a resident, with 4 years of experience with DN but only 1 year working in the clinic. The GPs who performed DN chose the muscles to be treated based on the patient's complaints and findings of the physical examination. The length of the needle used for DN varies according to the muscle location, from 30 to 120 mm, and the diameter was 0.3 mm. Insertion of the needle was deep and perpendicular except for the back area, where it was oblique to the skin.
Study population
Inclusion criteria were age > 18 years old, Hebrew speakers, acute MPS (less than a week from onset) and consent to take part in the study. Exclusion criteria were pregnancy, local infection, hemophilia, anti-coagulants use, local mass in the site of insertion, a contagious disease (hepatitis B, hepatitis C, HIV), having orthopedic implants or having undergone lymph node dissection. Follow-up of patients was done via telephone by the lead researcher.
The diagnosis of MPS in this study relies on specific finding in the physical examination and clinical judgment of the physicians. The findings relevant for MPS in the physical examination include identification of a taut band and intentionally producing the pain by application of pressure to a point of tenderness within the band [26, 27].
Variables
The outcome variables were the SF-MPQ which consists of three distinct parts; First, pain rating index – which includes 15 words describing pain (in 2 subscales – sensory and affective), each rated on intensity scale of 0 (none) to 3 (severe). Total scores range from 0 to 45. Second, present pain intensity which represents the amplitude of pain from 0 (no pain) to 5 (excruciating pain) and third, a 10 cm visual analog scale (VAS) for average pain [28, 29]. The SF-MPQ is considered a reliable tool to indicate clinically valuable difference in musculoskeletal pain [30].
Independent variables included were sociodemographic and DN related variables; sociodemographic data were collected for all participants including gender, age, marital status, country of birth (native born vs. other), socioeconomic status (SES, rated from 1 (lowest) to 10, (highest)). Smoking status and DN related variables were also collected, including exact site of DN, single vs. multiple needles inserted, the physician who performed the procedure and the baseline VAS (low [1,2,3,4,5] and high [3,6,7,8,9]).
Statistical analysis
Sample size was calculated based on assumptions of pain rating index of 30 before DN and 25 after DN (with SD of 7) and VAS of 6 before DN and 4 after DN with a power of 90%, p value < 0.001 and a correlation of 0.4 assumed between both tests. These assumptions yield a sample size of 50 patients.
For each part of the SF-MPQ a mean and standard deviation were produced (pain rating index, present pain intensity and VAS; before DN, 10-min and 1-week after DN). Change was estimated using ANOVA with Bonferroni correction;10 min after compared to the baseline (short-term effect), 1-week after compared to the baseline (medium-term effect) and 1-week after compared to 10 min after. A success was defined has having at least 2 measures that have improved (out of the three parts of the SF-MPQ). A continuous success was considered success in both short- and medium-term indices. A logistic regression was performed to assess what variables are associated with short-term, medium-term, and continuous success, using the Forward approach. Analyses were performed using SPSS Statistics, version 27.
Results
From September 2019 to August 2020, 55 patients were recruited (all data are available in the supplementary file). Three patients were excluded due to loss of follow-up at 1 week. 52% of patients were women with a mean age of 37.8 ± 12.6 (Table 1). Most of the DN procedures were done on the Trapezius muscle (40%), Iliocostalis Lumborum (27.3%) and Latissimus Dorsi (12.7). In each procedure one or more needles were inserted (76.9% single needle vs. 23.1% multiple needles).
Univariate analysis
VAS was 6.0 ± 2.3 before DN was performed, 4.1 ± 2.5 10-min after and 2.6 ± 2.71-week after. Pain rating index was 17 ± 9.1 before DN was performed, 10.8 ± 8.5 10-min after and 5.1 ± 6.5 1-week after. Present pain intensity was 2.6 ± 1.0 before DN was performed, 1.7 ± 1.0 10-min after (P < 0.001) and 1.1 ± 1.2 1-week after (Table 2, Fig. 1). All comparisons were significant with a P < 0.05.
Multivariate analysis
A logistic regression for short-term success (improvement after 10-min) showed that 2 factors were associated with it; the physician who performed the procedure (OR 10.08, 95% CI 1.15,88.4) and single needle inserted (vs. multiple needles) (OR 4.55, 95% CI 1.03,20.11). Medium-term success (improvement after 1-week, compared to baseline) was associated with being a native born (i.e., not having immigrated to Israel) (OR 8.59, 95% CI 1.11,66.28) and high level of initial pain (OR 11.22, 95% CI 1.82,69.27). Continuous success was associated with insertion of one needle, compared to multiple needles (OR 5.00, 95% CI 0.97,25.77).
Discussion
Main results
Our study demonstrated improvement in acute MPS 10-min after and 1-week after DN. Improvement was demonstrated in all parts of the SF-MPQ (pain rating index, present pain intensity and VAS). Short-term success was associated with the physician who performed the procedure and the insertion of a single needle (vs. multiple needles). Medium-term success was associated with being a native born and with higher levels of baseline pain (as evident by a VAS level higher than 5). Continuous success was associated with insertion of one needle (vs. multiple needles).
Interpretation
In this study we explored the effectiveness of DN when performed by GPs in their clinics. Most research conducted on DN focuses on other health care providers who perform this intervention (physiotherapists and consultant physicians). The only data we found about DN in family practice is a review published by the Journal of the American Board of Family Medicine in 2010 [31]. In this review, Kalichman & Vulfsons recommended that DN can be used as part of the complex treatment of musculoskeletal pain by GPs.
Our findings on the effectiveness of DN support the body of knowledge that DN can be considered as a good treatment for acute pain [32]. The success of DN in improving pain levels was reported immediately after and also had a delayed effect with better results reported 1-week later. This suggests that the effect is continuous. Previous studies have shown both short-term and medium-term positive effect on pain intensity when comparing DN to sham needling [33,34,35], and to no intervention [36]. We demonstrated a mean VAS decrease of 1.9 10-min after DN and 3.4 1-week after. These findings are in line with other studies on the effect of DN, which showed a mean VAS decrease larger than 1.5 [37]; this decrease is larger than 1.2, the minimum clinically important difference in VAS [38].
High intensity of pain before the procedure, as indicated by a VAS of 6 or more, was associated with medium-term success. This might suggest that DN is more effective in alleviating pain when it is severe in the first place.
We believe that certain aspects of DN performed specifically by GPs should be addressed. Firstly, continuity of care, which is a fundamental aspect of primary care can augment the success of the procedure [39]. In our study, two GPs, a specialist and a resident, performed DN on their patients. Both had 3–4 years of experience with DN, but the specialist had worked in the same clinics for 8 years while the resident only worked in the clinic for 1 year. When DN was performed by the specialist, better results were observed with higher rates of immediate and continuous success. Although a meta-analysis indicated that experience of acupuncturist does not modify outcomes of DN [40], this might not be true to GPs. The impact of DN performed by a familiar physician might add to the success of the treatment, giving GPs a leverage on other health care providers providing this procedure. Secondly, access to care is essential to management of acute pain, which is another advantage of GPs over consultant physicians.
Preferences of patients might also be different when GPs perform DN compared to other health care workers; our study demonstrated that insertion of 1 needle (vs. multiple needles) was associated with short-term and continuous success, contrary to a meta-analysis that found the effect of acupuncture increased when more needles were inserted [40]. This may represent patients’ preferences for a shorter and more precise intervention during a GP visit compared to a physiotherapist consultation or a consultant physician, like an orthopedic specialist.
Strengths
This study examines the effect of DN performed by GPs in their clinics. This is unlike most studies, which examine DN use by physiotherapists or physicians that are not necessarily GPs. As this procedure is widely and increasingly used by GPs, this is an important aspect of the research on the effectiveness of DN. The use of a validated scale for pain, the SF-MPQ, increases the validity of this study. Measuring the effect of DN both in short- and medium-term is another strength of this study.
Limitations of the data
This study did not include a control group, and thus the treatment cannot be compared to other treatment options or to sham-therapy. Additionally, patients were treated by two GPs in the southern district of Israel; the population of patients does not represent the whole Israeli population, which may affect the results found. Both physicians who performed the DN also treat patients for other medical problems. This may influence patients’ satisfaction and pain. The specialty status of the GPs (one was a specialist and the other a resident) might also have impacted the results. Another limitation is the lack of follow-up with patients who declined to participate; thus, a possible selection bias might exist.
Conclusion
DN is a good therapeutic option for GPs to aid patients suffering from acute pain. All SF-MPQ parameters of pain improved significantly, both in short- and medium-term. The physician who performed the procedure was associated with short-term and continuous success rates. Initial high intensity pain (VAS > 5) was associated with medium-term success. Considering it is a low-cost method and relatively easy skill to impart, it should be encouraged by policy makers to increase its availability to patients. This can be done by exposing students, residents and specialists to this skill. Further research should explore the effectiveness of DN shortly after having learned the method and by a larger group of GP participants in different settings. Future studies may prefer to choose algometry as a method to assess pain rather than questionnaires as we had chosen.
Availability of data and materials
All data generated and analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- DN:
-
Dry needling
- GPs:
-
General practitioners
- IMS:
-
Intra-muscular stimulation
- MPS:
-
Myofascial pain syndrome
- MTrPs:
-
Myofascial trigger points
- SES:
-
Socioeconomic status
- SF-MPQ:
-
Short-Form McGill Pain Questionnaire
- VAS:
-
Visual analog scale
References
Abbafati C, Machado DB, Cislaghi B, Salman OM, Karanikolos M, McKee M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832–40.
Barbero M, Schneebeli A, Koetsier E, Maino P. Myofascial pain syndrome and trigger points: evaluation and treatment in patients with musculoskeletal pain. Curr Opin Support Palliat Care. 2019;13(3):270–6.
Kuan TS. Current studies on myofascial pain syndrome. Curr Pain Headache Rep. 2009;13:365–9.
Hong CZ, Simons DG. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil. 1998;79:863–72 W.B. Saunders.
Urits I, Charipova K, Gress K, Schaaf AL, Gupta S, Kiernan HC, et al. Treatment and management of myofascial pain syndrome. Best Pract Res Clin Anaesthesiol. 2020;34:427–48 Bailliere Tindall Ltd.
Boyce D, Wempe H, Campbell C, Fuehne S, Zylstra E, Smith G, et al. Adverse events associated with therapeutic dry needling. Int J Sports Phys Ther. 2020;15(1):103–13.
Vier C, de Almeida MB, Neves ML, dos Santos ARS, Bracht MA. The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: a systematic review and meta-analysis. Braz J Phys Ther. 2019;23:3–11 Revista Brasileira de Fisioterapia.
Kietrys DM, Palombaro KM, Azzaretto E, Hubler R, Schaller B, Schlussel JM, et al. Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2013;43(9):620–34.
Cagnie B, Castelein B, Pollie F, Steelant L, Verhoeyen H, Cools A. Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: a systematic review. Am J Phys Med Rehabil. 2015;94:573–83 Lippincott Williams and Wilkins.
Liu L, Huang QM, Liu QG, Ye G, Bo CZ, Chen MJ, et al. Effectiveness of dry needling for myofascial trigger points associated with neck and shoulder pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96:944–55.
Navarro-Santana MJ, Sanchez-Infante J, Fernández-de-las-Peñas C, Cleland JA, Martín-Casas P, Plaza-Manzano G. Effectiveness of dry needling for myofascial trigger points associated with neck pain symptoms: an updated systematic review and meta-analysis. J Clin Med. 2020;9(10):3300.
Navarro-Santana MJ, Gómez-Chiguano GF, Cleland JA, Arias-Buría JL, Fernández-De-Las-Peñas C, Plaza-Manzano G. Effects of trigger point dry needling for nontraumatic shoulder pain of musculoskeletal origin: a systematic review and meta-analysis. Phys Ther. 2021;101(2):216.
Lew J, Kim J, Nair P. Comparison of dry needling and trigger point manual therapy in patients with neck and upper back myofascial pain syndrome: a systematic review and meta-analysis. J Man Manip Ther. 2021;29(3):136–46.
Fernández-De-Las-Peñas C, Plaza-Manzano G, Sanchez-Infante J, Gómez-Chiguano GF, Cleland JA, Arias-Buría JL, et al. Is dry needling effective when combined with other therapies for myofascial trigger points associated with neck pain symptoms? A systematic review and meta-analysis. Pain Res Manag. 2021;2021:8836427 Hindawi Limited.
Navarro-Santana MJ, Sanchez-Infante J, Gómez-Chiguano GF, Cleland JA, López-de-Uralde-Villanueva I, Fernández-de-las-Peñas C, et al. Effects of trigger point dry needling on lateral epicondylalgia of musculoskeletal origin: a systematic review and meta-analysis. Clin Rehabil. 2020;34(11):1327–40.
Liu L, Huang QM, Liu QG, Thitham N, Li LH, Ma YT, et al. Evidence for dry needling in the management of myofascial trigger points associated with low back pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(1):144-152. e2 W.B. Saunders.
Tüzün EH, Gıldır S, Angın E, Tecer BH, Dana KÖ, Malkoç M. Effectiveness of dry needling versus a classical physiotherapy program in patients with chronic low-back pain: a single-blind, randomized, controlled trial. J Phys Ther Sci. 2017;29(9):1502–9.
Furlan AD, van Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry Furlan AD, van Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 2005;(1):CD001351.
Rahou-El-Bachiri Y, Navarro-Santana MJ, Gómez-Chiguano GF, Cleland JA, López-de-Uralde-Villanueva I, Fernández-de-las-Peñas C, et al. Effects of trigger point dry needling for the management of knee pain syndromes: a systematic review and meta-analysis. J Clin Med. 2020;9(7):2044.
Rastegar S, BaradaranMahdavi S, Hoseinzadeh B, Badiei S. Comparison of dry needling and steroid injection in the treatment of plantar fasciitis: a single-blind randomized clinical trial. Int Orthop. 2018;42(1):109–16.
Charles D, Hudgins T, MacNaughton J, Newman E, Tan J, Wigger M. A systematic review of manual therapy techniques, dry cupping and dry needling in the reduction of myofascial pain and myofascial trigger points. J Bodyw Mov Ther. 2019;23(3):539–46.
Gattie E, Cleland JA, Pandya J, Snodgrass S. Dry needling adds no benefit to the treatment of neck pain: a sham- controlled randomized clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. 2021;51(1):37–45.
Hall ML, Mackie AC, Ribeiro DC. Effects of dry needling trigger point therapy in the shoulder region on patients with upper extremity pain and dysfunction: a systematic review with meta-analysis. Physiotherapy. 2018;104(2):167–77 Elsevier Ltd.
Ratmansky M, Minerbi A, Kalichman L, Kent J, Wende O, Finestone AS, et al. Position statement of the Israeli society for musculoskeletal medicine on intramuscular stimulation for myofascial pain syndrome—a delphi process. Pain Pract. 2017;17(4):438–46.
Urits I, Charipova K, Gress K, Schaaf AL, Gupta S, Kiernan HC, et al. Treatment and management of myofascial pain syndrome. Best Pract Res Clin Anaesthesiol. 2020;34(3):427–48.
Cummings M, Baldry P. Regional myofascial pain: diagnosis and management. Best Pract Res Clin Rheumatol. 2007;21(2):367–87.
Grafton KV, Foster NE, Wright CC. Test-retest reliability of the Short-Form McGill Pain Questionnaire: Assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. Clinical J Pain. 2005;21(1):73–82. Available from: https://pubmed.ncbi.nlm.nih.gov/15599134/. [cited 2021 Mar 15].
Chaffee A, Yakuboff M, Tanabe T. Responsiveness of the VAS and McGill Pain Questionnaire in measuring changes in musculoskeletal pain. J Sport Rehabil. 2011;20(2):250–5. Available from: https://pubmed.ncbi.nlm.nih.gov/21576715/. [cited 2021 Mar 15]
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(SUPPL. 11):S240-52.
Kalichman L, Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board Fam Med. 2010;23:640–6. Availble from: https://pubmed.ncbi.nlm.nih.gov/20823359/. [cited 2021 Mar 11].
Kelly R, Willis J. Acupuncture for Pain. Am Fam Physician. 2019;100(2):89–96.
Tekin L, Akarsu S, Durmuş O, Çakar E, Dinçer Ü, Kiralp MZ. The effect of dry needling in the treatment of myofascial pain syndrome: A randomized double-blinded placebo-controlled trial. Clin Rheumatol. 2013;32(3):309–15.
Mayoral O, Salvat I, Martín MT, Martín S, Santiago J, Cotarelo J, et al. Efficacy of myofascial trigger point dry needling in the prevention of pain after total knee arthroplasty: A randomized, double-blinded, placebo-controlled trial. Evid Based Complement Alternat Med. 2013;2013:694941.
Tsai CT, Hsieh LF, Kuan TS, Kao MJ, Chou LW, Hong CZ. Remote effects of dry needling on the irritability of the myofascial trigger point in the upper trapezius muscle. Am J Phys Med Rehabil. 2010;89(2):133–40.
Mejuto-Vázquez MJ, Salom-Moreno J, Ortega-Santiago R, Truyols-Domínguez S, Fernández-De-Las-peñas C. Short- term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44(4):252–60.
Espejo-Antúnez L, Tejeda JFH, Albornoz-Cabello M, Rodríguez-Mansilla J, de la Cruz-Torres B, Ribeiro F, et al. Dry needling in the management of myofascial trigger points: a systematic review of randomized controlled trials. Complement Ther Med. 2017;33:46–57 Churchill Livingstone.
Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18(3):205–7.
Tammes P, Salisbury C. Continuity of primary care matters and should be protected. BMJ. 2017;356. Available from: https://pubmed.ncbi.nlm.nih.gov/28148480/ [cited 2022 Nov 29].
MacPherson H, Maschino AC, Lewith G, Foster NE, Witt C, Vickers AJ. Characteristics of acupuncture treatment associated with outcome: an individual patient meta-analysis of 17,922 patients with chronic pain in randomised controlled trials. PLoS One. 2013;8(10):e77438.
Acknowledgements
None.
Funding
This work was supported by Marom, a research program for physicians and residents in Maccabi Healthcare Services.
Author information
Authors and Affiliations
Contributions
IY and OR performed DN on their patients. LA analyzed and interpreted the data and wrote the initial draft of the manuscript. RP and MMR supervised the study. IY, OR, RP, MMR revised the manuscript critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethical committee of Bait Balev (the institutional review board), ID 0017–19-BBL. Patients who agreed to take part in the study were given full explanation on the procedure of DN and possible side effects and signed a written informed consent. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Dataset - IMS.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yehoshua, I., Rimon, O., Mizrahi Reuveni, M. et al. Dry needling for the treatment of acute myofascial pain syndrome in general practitioners’ clinics: a cohort study. BMC Prim. Care 23, 339 (2022). https://doi.org/10.1186/s12875-022-01951-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01951-0