Abstract
Background
Healthcare accreditation is a widely implemented tool used to enhance the quality of care and underpin quality control. However, research is sparse on the accreditation process in general practice. The aim of this study was to explore how team-based implementation activities preceding accreditation were associated with self-perceived improvements in emergency preparedness (preparedness for urgent disease and cardiac arrest) and handling of prescription renewals in Danish general practice.
Methods
GPs (general practitioners) completed a questionnaire exploring practice-team activities conducted to implement two specific accreditation standards and the related improvements as perceived by the GPs. The following implementation activities were selected, inspired by Normalization Process Theory: Common understanding (obtaining a common understanding of the purpose of implementing changes according to the accreditation standard), key person (assigning a key person responsible for working with the standard), and easy integration (finding it easy to integrate changes into existing working procedures). Data were analysed with logistic regression, and adjusted analyses included practice type, number of GP partners, number of staff, training site for junior GPs and administrative region.
Results
The total response rate was 74% (n = 920). Around 80% of the clinics reported having conducted team-based implementation activities. Almost half of the clinics (48%) reported perceived improvements in the emergency preparedness, and 30% reported perceived improvements in the handling of prescription renewals. Obtaining a common understanding was found to have a strong, significant association with perceived improvements in the emergency preparedness (OR = 5.07 (3.06–8.40)) and handling of prescription renewals (OR = 3.66 (2.07–6.46)). Easy integration of changes was also significantly associated with improvements in both emergency preparedness (OR = 1.88 (1.24–2.85)) and handling of prescription renewals (OR = 2.34 (1.44–3.79)), whereas assigning a key person was only significantly associated with improved emergency preparedness (OR = 1.95 (1.19–3.19)).
Conclusion
Clinical quality initiatives that involve collaboration within a practice team are more likely to cause improvements if specific team-based implementation activities are conducted. It is particularly important to facilitate a common understanding of the purpose of the initiative. Therefore, external support for quality initiatives aiming at the practice level in general practice should facilitate such team-based activities.
Similar content being viewed by others
Background
Accreditation is defined as an evaluation of an organisation by an accreditation agency based on a set of predefined accreditation standards [1]. The purpose of accreditation is to improve the quality and safety of care and to underpin quality control [2, 3]. Accreditation was introduced in the primary healthcare sector in Australia in the 1990s and has been used in the secondary healthcare sector since the beginning of the 20th century [4]. Since then, a number of countries, including the USA, New Zealand and many European countries, have developed accreditation programmes for general practice [2]. Despite the widespread use of healthcare accreditation, research on its implementation and influence on clinical practice in general practice is sparse [2].
In Denmark, a mandatory accreditation programme for general practice was rolled out in 2016–2018 [5]. The Danish Institute for Quality and Accreditation in Healthcare (IKAS), which is an impartial institution, developed and managed the accreditation programme. The standards and indicators were developed by IKAS in collaboration with representatives from the Organization of General Practitioners in Denmark, the Danish College of General Practitioners, Danish Regions, Danish Patients and the Danish Association of Practicing Medical Specialists [6]. The clinics were advised one year in advance about the date of their accreditation survey and were offered support through training courses and workshops, and they were offered on-line information and access to consultants [7]. On this date, the clinic received a visit from two surveyors: a general practitioner (GP) and a practice staff. After the visit, the surveyors prepared a report based on their assessment; this report was used by the accreditation board to decide whether the clinic was eligible for accreditation [5]. The clinics were evaluated based on 16 quality standards containing indicators about professional quality, organisational quality and patient-perceived quality [5]. The standards formed a framework intended to stimulate reflection and inspire quality improvement activities [8]. However, another purpose of the programme was quality control, and many GPs were sceptical and perceived the mandatory accreditation programme as an external control tool [9]. Each clinic received 20,000 Danish kroner (approximately €2650) per GP in the clinic for their participation in the accreditation programme. The clinics received half of the amount in advance and the rest when the clinic was accredited [10].
Attaining successful implementation of complex interventions, such as accreditation, is a challenge [11, 12]. Studies on healthcare accreditation show that implementation is influenced by a variety of factors at the individual, group, structural and organizational levels [11, 13]. In the Danish accreditation programme, only 1.2% of general practice clinics failed to become accredited [14]. Still, a qualitative study shows that the implementation varied markedly; some clinics changed only very few elements, whereas other clinics made many considerable changes in response to accreditation [10]. Moreover, some studies report that the implemented changes are not always perceived to measure up to the efforts made and that the implementation process is challenging [6, 10]. Yet, interventions with external inspections, such as accreditation, have the ability to engage and involve staff, facilitate leader engagement, improve communication and enable the creation of new networks for reflection on clinical practice. Also, inspections can contribute to creating an awareness of the inspected organisation’s current practice and performance gaps, and a commitment to change and facilitate planning and implementation of change [15]. Quantitative studies of the extent of the effect are few in a general practice setting [16, 17], and results include positive, negative and mixed results [18,19,20,21]. To our knowledge, no quantitative studies investigate associations between implementation and[16] effects of general practice accreditation.
The aim of this study is to explore how team-based implementation activities preceding accreditation are associated with self-perceived improvements in the emergency preparedness (preparedness for urgent disease and cardiac arrest) and handling of prescription renewals in a general practice setting.
Methods
Setting
In Denmark, general practice is the primary entry point to the healthcare system, and general practice acts as a gatekeeper to the more specialised parts of the healthcare system [22]. GPs are self-employed, and their clinics can be organised as individual clinics with only one GP or in different types of partnership practices [23]. Most clinics employ staff members, such as practice nurses and receptionists, and approximately half of the clinics have GP trainees [23].
Study design and participants
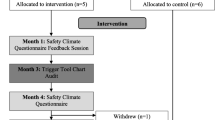
This is a cross-sectional study of the implementation of two specific standards in the Danish accreditation programme for general practice: emergency preparedness and handling of prescription renewals (Fig. 1). These specific standards were chosen as they are both concerned with patient care and therefore expected to be prioritized by the respondents. Though both standards are patient-centered, they are vastly different; the standard on emergency preparedness refers to rare incidents that the clinic must be prepared for, while the standard on handling of prescription renewals is a daily, routine task.
The paper conforms to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Standards [24].
Participants included general practice clinics conducting their accreditation survey between 27 and 2016 and 31 December 2018. After the accreditation survey, the participants received a questionnaire about their experiences with the accreditation process. The questionnaire was handed out by the visiting GP surveyor immediately after completion of the survey. The surveyor invited the GP who was most deeply involved in the accreditation to answer the questionnaire on behalf of the clinic. If the questionnaire had not been returned within two weeks, the clinics received a reminder and a new questionnaire as well as a postage-paid return envelope by regular mail.
The questionnaire consisted of 26 questions covering different aspects of the accreditation programme, including the conducted team-based implementation activities, the experience with the change process and the perceived effect of specific clinical standards included in the accreditation programme.
The questionnaire underwent a pilot test among 14 participants, including surveyors, GPs who had just completed their accreditation survey, and experienced researchers in general practice. Six of the informants gave verbal feedback to the interviewer, using cognitive interviewing techniques, during the completion of the questionnaire, whereas eight of them gave verbal feedback after completing the questionnaire [25]. In the pilot phase, the questionnaire was continually revised.
Theoretical framework
Normalization Process Theory (NPT) provides a useful framework to gain insight into the mechanisms governing the implementation of changes in small organizations, such as general practice clinics. It was developed to describe how new interventions are introduced in various settings, and how they become routines in everyday practice [26, 27]. NPT mainly focuses on how people work together in the implementation process and is less concerned with individual intentions or attitudes [28]. The theory describes four mechanisms, which are driven by different types of team-based implementation activities that motivate and shape implementation processes [28]. [22][29]. Coherence describes the ways participants make sense of the intervention. Cognitive participation focuses on the ways participants engage in the initial implementation activities. Collective action relates to the way participants support the initial implementation by investing skills and resources in the intervention. Finally, reflexive monitoring refers to the individual and collective assessment of the implementation and how it affects the participants [29]. Each of the four constructs contain multiple sub-constructs exploring different aspects of the main construct.
The Normalisation MeAsure Development (NoMAD) instrument derives from NPT and can be used to quantitatively measure team-based implementation activities and their outcomes [28, 30]. It consists of 25 questions covering all NPT sub-constructs which assess the team-based implementation activities from the perspective of the professionals who are directly involved in the activities [28, 30].
Team-based implementation activities
In this study, we explored three specific NPT sub-constructs within implementation: Communal specification (coherence), interactional workability (collective action), and initiation (cognitive participation). To operationalize the sub-constructs, three NoMAD questions were included in the questionnaire. A professional interpreter translated the questions and, together with the researchers, made a culturally adaptation to fit a GP setting and the context of the study (Table 1).
Coherence and collective action were assessed on a five-point Likert scale comprising ‘mainly agree’, ‘partly agree’, ‘neither agree nor disagree’, ‘partly disagree’ or ‘mainly disagree’. In the analyses, they were dichotomised and ‘occurrence of implementation activity’ included the first two response options. Cognitive participation was assessed through a Yes/No question, with the option to report the professional background of potential key person(s).
Self-perceived improvements
To investigate whether the emergency preparedness had improved after the accreditation process, the respondents were asked, “How is the emergency preparedness in your clinic today compared to the time before the work with the standard?” Similarly, to evaluate if the handling of prescription renewals had improved after the accreditation process, the respondents were asked, “How is the handling of prescription renewal in your clinic today compared to the time before the work with the standard?” For both questions, the respondents could select ‘better’, ‘just as good’ or ‘worse’. In the analysis, ‘better’ indicated improvements, whereas ‘worse’ and ‘just as good’ indicated no improvements.
Practice characteristics
Practice characteristics such as practice type, number of GP partners, number of staff, training site for junior GPs and administrative region were included as potential predictors, as they were considered to be potentially influencing the team-based implementation activities [7, 31]. Since GPs were asked to answer the questionnaire on behalf of the clinic, no individual data was collected. Practice type was categorised as single-handed or group practice, where group practice was defined as clinics with more than one GP partner and/or formalised cooperation with other clinics. Number of GP partners, and number of staff were included as continuous variables. Training site for junior GPs was categorised as a dichotomous variable indicating whether the clinic had GP trainees (Yes/No). Geographical location was based on the five Danish administrative regions: North Denmark Region, Capital Region of Denmark, Region Zealand, Region of Southern Denmark and Central Denmark Region.
Statistical analysis
Descriptive statistics were performed to characterize the dataset and assess the frequency of implementation activities and self-perceived improvements.
Logistic regression analyses tested associations between team-based implementation activities and perceived improvements in the emergency preparedness and handling of prescription renewals. The hypothesis is that clinics who engage in team-based implementation activities preceding accreditation are more likely to experience improvements in their emergency preparedness as well their handling of prescription renewals.
Associations were calculated as unadjusted as well as adjusted odds ratios (ORs). The adjusted statistical model included the crude improvement rate adjusting for implementation activities, practice type, number of GP partners, number of staff, GP trainees in clinic and administrative region. All variables in the adjusted model were entered in one step. The analyses were restricted to respondents with complete data on all variables in the models. Spearman’s correlation coefficients were used to test for multicollinearity. No strong collinearity was found between independent variables.
The 95% confidence intervals (CIs) were calculated, and P values of ≤ 5% were considered statistically significant. Data were analysed using Stata (version 16.1).
Results
Between 27 and 2016 and 31 December 2018, 1,230 clinics conducted their accreditation survey. A total of 920 clinics returned the questionnaire (74%). Of these, 721 clinics filled out the questionnaire which was handed out at the survey, and 199 clinics answered the reminder questionnaire. Table 2 shows the characteristics of the responding clinics.
Self-perceived improvements
In almost half of the clinics (48%), the respondents perceived to have obtained a better emergency preparedness compared to before. In the remaining clinics, no changes were perceived, except for one clinic in which the respondents reported to do worse (Table 3). In around a third (31%) of the clinics, the respondents reported that prescription renewals were handled better after compared to before the accreditation process. In only one clinic, the handling of prescription renewals was reported to be worse while the remaining respondents reported to experience no difference (Table 3).
Team-based implementation activities
Obtaining a common understanding of the purpose of preparing the guidelines was frequently reported (85% and 79%). The most commonly reported team-based implementation activity was the assignment of a key person responsible for working with the standards (88% and 86%) (Fig. 2). Finding it easy to integrate changes into existing working procedures was reported by 83% and 78% of the clinics (Fig. 2).
Most often, the role as key person was held by one or more GPs (56% and 63%). In some clinics, the role was shared by GPs and staff (30% and 63%), whereas the key person was one or more of the staff members in few clinics (6% and 7%).
Associations between implementation activities and improvements
The univariate logistic regression analysis showed that all team-based implementation activities were significantly associated with perceived improvements, except for the association between assigning a key person and improvements in prescription renewals (Table 4). The associations were still significant after adjusting for practice characteristics.
Obtaining a common understanding of the purpose of implementing changes according to the accreditation standard was found to have the strongest association with perceived improvements (OR = 5.07 (3.06–8.40) regarding the emergency preparedness and OR = 3.66 (2.07–6.46) regarding handling of prescription renewals). Easy integration of changes was also significantly associated with improvements in both emergency preparedness (OR = 1.88 (1.24–2.85)) and handling of prescription renewals (OR = 2.34 (1.44–3.79)). Assigning a key person responsible for working with the standard was only significantly associated with improved emergency preparedness (OR = 1.95 (1.19–3.19)) (Table 4). Additional file 1 shows the full adjusted model with all covariates.
Discussion
Main findings
Around 80% of the clinics had performed several specific, team-based implementation activities to fulfil the criteria for accreditation. Almost half of the clinics (48%) reported perceived improvements in the emergency preparedness, and 30% reported perceived improvements in the handling of prescription renewals. Very few respondents experienced impairment of their work procedures.
For both emergency preparedness and handling of prescription renewals, around 80% of the clinics reported to have obtained a common understanding of the purpose of preparing the guidelines, and that the preparation of the guidelines could be easily integrated into their way of working. The team-based implementation activities also included assignment of a key person which was reported by 86-88%. This role was seldomly delegated exclusively to a staff member.
The results revealed significant associations between the three types of team-based implementation activities and perceived improvements in the emergency preparedness and handling of prescription renewals. Obtaining a common understanding of the purpose of implementing changes according to the accreditation standard was found to have the strongest, significant association with perceived improvements. Finding it easy to integrate changes into existing working procedures was also significantly associated with improvements, whereas assigning a key person responsible for working with the standard was only significantly associated with improved emergency preparedness.
Strengths and limitations
An important strength of this study includes the high response rate compared to other questionnaire studies in this setting [32, 33]. Another strength includes hand distribution of the questionnaire by GP surveyors to all general practices in the study period immediately after their survey visit. In general, GP surveyors in Denmark succeeded at establishing a trust-based relation to GPs and GP staff [34] and are therefore valid distributers of the questionnaire. An important limitation of the study is the study design since cross-sectional studies do not allow us to draw firm causal conclusions. Another limitation is the embedded risk of recall bias as the experiences with both the team-based implementation activities and the perceived improvements were measured some time after the actual implementation processes. To address the risk of recall bias, we asked the GP most involved in the accreditation process to complete the questionnaire.
In the interpretation of the findings, it should also be borne in mind that the study explored the first round of accreditation in Danish general practice. The implementation activities and the perceived effects might have been different if the clinics were familiar with the concept of accreditation [18].
Furthermore, only two of the 16 accreditation standards were explored in this study. Both standards are about patient care and were chosen based on perceived clinical relevance. The findings might reflect this, and the effects of team-based implementation could be different for accreditation standards focusing on organization and management. Though most results showed associations between team-based implementation activities and self-perceived improvements, assigning a key person responsible for working with the standard was only significantly associated with improved emergency preparedness and not with prescription renewals. A possible explanation might relate to the fact that emergency preparedness refers to rare incidents, whereas prescription renewals is a daily, routine task where GPs and staff already must be expected to have more well-defined roles. Thus, a study from general practice found that implementation processes might be different for daily routine work compared to infrequent processes [35]. Assigning a key person to take care of prescription renewals might therefore be less important.
Accreditation is a highly complex process, which takes place in a complex clinical reality. Although accreditation has been studied in multiple settings [1, 18, 36], a link between accreditation and improvements in the quality of care has not been fully established [21, 37]. Also, it is difficult to ensure that measured effects can be attributed to accreditation. In this study, we sought to increase the content validity of the questions regarding perceived effects by asking questions on two specific accreditation standards.
The NoMAD instrument was chosen as a means for measuring implementation activities. In the current study, only three NoMAD questions were included as proxy measures for team-based implementation of accreditation in general practice; therefore, they should be seen as a simplification of the highly complex concept of implementation activities. The relevance of the NoMAD instrument is supported by its use in other recent studies, also in general practice [38, 39]. Furthermore, the instrument has been translated to a range of other languages, including a Danish version launched after the initiation of our data collection. Only minor differences exist between the translated version of the questions in our questionnaire, which was used in this study, and the official Danish version of the NoMAD instrument [40].
Comparison with literature
Studies of Danish GPs’ experiences with accreditation have found large variations in the use of external implementation support during the accreditation process [7], as well as their in-clinic implementation activities and the impact of accreditation [10]. In our study, the large majority of the clinics had been engaged in specific, team-based implementation activities. However, it is not possible to assess the thoroughness of these activities.
In our study, we found that improvements in work procedures were significantly more likely to appear if any of the specific, team-based implementation activities were conducted. This is in line with other studies, finding that a shared understanding among staff [35, 41] and assigning a key person for the implementation activities [41, 42] were important factors for successful implementation of accreditation standards or other quality interventions in general practice. However, other factors may also influence the implementation activities and the effect of the accreditation programme, e.g. that the Danish programme is mandatory [13].
Implementation and effectiveness can be influenced by the pre-existing motivation to comply with a top-down mandatory intervention [43] such as an accreditation programme, which can be criticized for causing a focus on bureaucratic exercises rather than improving healthcare [44]. Thus, a favourable perception of accreditation has been identified as an enabling factor for implementation [13]. A previous study found widespread scepticism prior to the implementation of accreditation standards in general practice in Denmark [9]. This individual scepticism might influence implementation activities as well as perceived effects of accreditation. Perhaps scepticism is mostly related to the accreditation standards that are perceived as bureaucratic (e.g. standards concerning management) and less related to the more directly clinically relevant standards which are included in our study.
Implications
We found that the percentage of clinics engaging in specific, team-based implementation activities was similar for both emergency preparedness and handling of prescription renewals. Moreover, the association between team-based implementation activities and perceived effects was to a large degree similar for both procedures. This suggests that our findings might also apply to the implementation of other accreditation standards dealing with clinical behaviour, and most likely also in other quality development initiatives aiming at improving clinical behaviour in general practice. Therefore, facilitating team-based implementation activities such as those explored can increase the likelihood of improvements in working procedures and quality of care.
Conclusion
Clinical quality initiatives that involve collaboration within a practice team are more likely to cause improvements if specific team-based implementation activities are conducted. It is particularly important to facilitate a common understanding of the purpose of the initiative, but also assigning a key person responsible for the quality work and finding it easy to integrate changes into existing working procedures is important. Therefore, external support for quality initiatives aiming at the practice level in general practice should facilitate such team-based activities.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due to the lack of consent of participants but are available from the corresponding author on reasonable request.
Abbreviations
- GP:
-
General practitioner
- IKAS:
-
(Danish) Institute for Quality and Accreditation in Healthcare
- NoMAD:
-
Normalisation MeAsure Development
- NPT:
-
Normalisation Process Theory
References
Hinchcliff R, Greenfield D, Moldovan M, Westbrook JI, Pawsey M, Mumford V, Braithwaite J. Narrative synthesis of health service accreditation literature. BMJ Qual Saf. 2012;21(12):979–91.
O’Beirne M, Zwicker K, Sterling PD, Lait J, Lee Robertson H, Oelke ND. The status of accreditation in primary care. Qual Prim Care. 2013;21(1):23–31.
Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008;20(3):172–83.
Mainz J. Basal kvalitetsudvikling [Basic quality improvement] Kbh. Munksgaard; 2017.
Danish Institute for Quality and Accreditation in Healthcare (IKAS). Den Danske Kvalitetsmodel, Akkrediteringsstandarder for almen praksis [Danish Healthcare Quality Programme, Accreditation standards for general practice]. 2018.
Due TD, Thorsen T, Kousgaard MB. Understanding accreditation standards in general practice – a qualitative study. BMC Fam Pract. 2019;20(1):1–12.
Jensen MLO, Bro F, Mygind A. Implementation of healthcare accreditation in Danish general practice: a questionnaire study exploring general practitioners’ perspectives on external support. Scand J Prim Health Care. 2021;39:85–91.
IKAS. Accreditation standards. https://www.ikas.dk/den-danske-kvalitetsmodel/ddkm-in-english/accreditation-standards. Accessed 13 February 2020.
Waldorff FB, Nicolaisdottir DR, Kousgaard MB, Reventlow S, Sondergaard J, Thorsen T, Andersen MK, Pedersen LB, Bisgaard L, Hutters CL, et al. Almost half of the Danish general practitioners have negative a priori attitudes towards a mandatory accreditation programme. Dan Med J. 2016;63:9.
Kousgaard MB, Thorsen T, Due TD. Experiences of accreditation impact in general practice – a qualitative study among general practitioners and their staff. BMC Fam Pract. 2019;20:1.
Dogherty EJ, Estabrooks CA. Why do barriers and facilitators matter? In: Complex interventions in health. Edited by Richards DA, Hallberg IR. New York: Routledge; 2015. 273–281.
Skolarus TA, Sales AE. Implementation issues. In: Complex interventions in health. Edited by Richards DA, Hallberg IR. New York: Routledge; 2015. 265–272.
Hinchcliff R, Greenfield D, Westbrook JI, Pawsey M, Mumford V, Braithwaite J. Stakeholder perspectives on implementing accreditation programs: a qualitative study of enabling factors. BMC Health Serv Res. 2013;13(1):437.
IKAS. Akkreditering af almen praksis - status pr. 11.09.2019 [Accreditation in general practice - status as of 11 September 2019]. Aarhus; 2019.
Hovlid E, Braut GS, Hannisdal E, Walshe K, Bukve O, Flottorp S, Stensland P, Frich JC. Mediators of change in healthcare organisations subject to external assessment: a systematic review with narrative synthesis. BMJ open. 2020;10(8):e038850.
O’Beirne M, Zwicker K, Sterling PD, Lait J, Lee Robertson H, Oelke ND. The status of accreditation in primary care. Qual Prim Care. 2013;21:23–31.
Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care. 2008;20:172–83.
Nouwens E, van Lieshout J, Bouma M, Braspenning J, Wensing M. Effectiveness of Improvement Plans in Primary Care Practice Accreditation: A Clustered Randomized Trial. PLoS ONE. 2014;9(12):14.
Szecsenyi J, Campbell S, Broge B, Laux G, Willms S, Wensing M, Goetz K. Effectiveness of a quality-improvement program in improving management of primary care practices. CMAJ. 2011;183(18):E1326–33.
Riisgaard H, Waldorff FB, Kirstine Andersen M, Pedersen LB. Does accreditation of general practice promote patient-reported quality of care? A natural cluster randomised experiment. BMJ open. 2020;10(6):e034465.
van Doorn-Klomberg AL, Braspenning JCC, Wolters RJ, Bouma M, Wensing M. Effect of accreditation on the quality of chronic disease management: a comparative observational study. Bmc Family Practice 2014:15:8.
Pedersen KM, Andersen JS, Sondergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(Suppl 1):34–8.
The Danish Health Data Authority. Beskrivelse af almen praksissektoren i Danmark [Description of the primary care sector in Denmark]. 2016.
Elm Ev, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational Studies. Ann Intern Med. 2007;147(8):573–7.
Beatty PC, Gordon WB. Research synthesis. Pract Cogn interviewing Public Opin Q. 2007;71:287–311.
May C. Applying normalization process theory to the implementation of complex interventions. In: Complex interventions in health. edn. Edited by Richards DA, Hallberg IR. New York: Routledge; 2015: 293–299.
Rapley T, Girling M, Mair FS, Murray E, Treweek S, McColl E, Steen IN, May CR, Finch TL. Improving the normalization of complex interventions: part 1 - development of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med Res Methodol. 2018;18(1):133.
May C, Finch T, Rapley T. Normalization Process Theory In: Handbook on implementation science. edn. Edited by Nilsen P, Birken SA. Cheltenham Edward Elgar Publishing Limited; 2020: 144–167.
May C, Finch T. Implementing, Embedding, and Integrating Practices: An Outline of Normalization Process Theory. Sociology. 2009;43(3):535–54.
Finch TL, Girling M, May CR, Mair FS, Murray E, Treweek S, McColl E, Steen IN, Cook C, Vernazza CR, et al. Improving the normalization of complex interventions: part 2 - validation of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med Res Methodol. 2018;18(1):135.
Mygind A, Munksgaard PP, BF. Regional støtte til implementering af akkreditering i almen praksis: Udbud og anvendelighed [Regional support for implementation of accreditation in general practice: Supply and applicability]. Danish. Aarhus: The Research Unit for General Practice; 2019.
Ahnfeldt-Mollerup P, dePont Christensen R, Halling A, Kristensen T, Lykkegaard J, Nexoe J, Barwell F, Spurgeon P, Sondergaard J. Medical engagement and organizational characteristics in general practice. Fam Pract. 2016;33(1):69–74.
Le JV, Pedersen LB, Riisgaard H, Lykkegaard J, Nexøe J, Lemmergaard J, Søndergaard J. Variation in general practitioners’ information-seeking behaviour - a cross-sectional study on the influence of gender, age and practice form. Scand J Prim Health Care. 2016;34:327–35.
Due TD, Thorsen T, Kousgaard MB. The survey visit as a key evaluative event in accreditation–a qualitative study of survey visit experiences among surveyors and general practice professionals. BMC Fam Pract. 2021;22(1):163.
Høj K, Mygind A, Bro F. Exploring implementation processes in general practice in a feedback intervention aiming to reduce potentially inappropriate prescribing: a qualitative study among general practitioners. Implement Sci Commun. 2021;2(1):4.
Bogh SB, Falstie-Jensen AM, Bartels P, Hollnagel E, Johnsen SP. Accreditation and improvement in process quality of care: a nationwide study. Int J Qual Health Care. 2015;27(5):336–43.
Brubakk K, Vist GE, Bukholm G, Barach P, Tjomsland O. A systematic review of hospital accreditation: the challenges of measuring complex intervention effects. BMC Health Serv Res. 2015;15:280.
Mills K, Griffin SJ, Sutton S, Usher-Smith JA. Development and usability testing of a very brief intervention for personalised cancer risk assessment to promote behaviour change in primary care using normalisation process theory. Prim Health Care Res Dev. 2020;21:e1.
Sturgiss EA, Elmitt N, Haesler E, van Weel C, Douglas K. Feasibility and acceptability of a physician-delivered weight management programme. Fam Pract. 2017;34(1):43–8.
ImpleMentAll. Normalization Measure Development Questionnaire (short NoMAD). 2018. https://www.implementall.eu/NoMAD_Danish.pdf. Accessed 5 September 2022.
Shea CM, Turner K, Albritton J, Reiter KL. Contextual factors that influence quality improvement implementation in primary care: The role of organizations, teams, and individuals. Health Care Manage Rev. 2018;43(3):261–9.
Nouwens E, van Lieshout J, Wensing M. Determinants of impact of a practice accreditation program in primary care: a qualitative study. BMC Fam Pract. 2015;16:8.
Weske U, Boselie P, van Rensen ELJ, Schneider MME. Using regulatory enforcement theory to explain compliance with quality and patient safety regulations: the case of internal audits. BMC Health Serv Res. 2018;18(1):62.
Pomey MP, François P, Contandriopoulos AP, Tosh A, Bertrand D. Paradoxes of French accreditation. Qual Saf Health Care. 2005;14(1):51–5.
World Medical Association. WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects. Helsinki; 2013.
The European Parliament and the Council of the European Union: The protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) In.: https://gdpr-info.eu/; 2016.
National Committee on Health Research Ethics. Act on Research Ethics Review of Health Research Projects. 2018. https://en.nvk.dk/rules-and-guidelines/act-on-research-ethics-review-of-health-research-projects.
Acknowledgements
We would like to thank all GPs who completed the questionnaire, the surveyors for engaging in the project and handing over all the questionnaires, Pia Pinholt Munksgaard for project coordination and Henrik Schou Pedersen for statistical support.
Funding
This study was supported by an unrestricted grant from the Danish Institute for Quality and Accreditation in Healthcare (IKAS) and the Danish Research Foundation for General Practice (Fonden for Almen Praksis).
Author information
Authors and Affiliations
Contributions
AM and FB generated the idea for and designed the study. AM managed the data collection. CM conducted the analysis and led the drafting of the manuscript. All authors contributed to the drafting of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the general ethical principles of good clinical research practice drawn up by the World Medical Association in the Helsinki Declaration [45]. The respondents were informed by a written formal cover letter about the study, including purpose, confidentiality, voluntariness, and anonymity. Returning the completed questionnaire was interpreted as informed consent to participate in the study. The study was approved by the Danish Data Protection Agency (record number 2016-41-4579), and data storage and access comply with the General Data Protection Regulation guidelines. The project is registered in the Record of Processing Activities at the Research Unit for General Practice, Aarhus, in accordance with the Danish Data Protection Act (Act No. 502 of 23 May 2018) and the General Data Protection Regulation (GDPR) by the EU [46]. In Denmark, approval by the Committee on Health Research Ethics is not required for questionnaire and registry studies [47].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding author:
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
File name: Additional file 1.
File format: Microsoft Word Document (.docx).
Title of data: Association between team-based implementation activities and perceived improvements (full model with all predictors).
Description of data: Adjusted model including all predictors in the logistic regression analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mølgaard, C., Bro, F. & Mygind, A. What GPs do to meet accreditation standards – implementation activities and perceived improvements attributed to general practice accreditation. BMC Prim. Care 23, 265 (2022). https://doi.org/10.1186/s12875-022-01864-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01864-y