Abstract
Background
Cardiovascular disease (CVD) is a major cause of morbidity and mortality in Canada. Assessment and management of CVD risk is essential in reducing disease burden. This includes both clinical risk factors and socioeconomic factors, though few studies report on socioeconomic status in relation to CVD risk and treatment. The primary objective of this study was to estimate the cardiovascular risk of patients attending primary care practices across Canada; secondly, to evaluate concordance with care indicators suggested by current clinical practice guidelines for statin prescribing according to patients’ cardiovascular risk and socioeconomic status.
Methods
This cross-sectional observational study used the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) database, which is comprised of clinical data from primary care electronic medical records. Patients aged 35-75y with at least one visit to their primary care provider between 2012 and 2016 were included. Patients were assigned to a CVD risk category (high, medium, low) and a deprivation quintile was calculated for those with full postal code available. Descriptive analyses were used to determine the proportion of patients in each risk category. Logistic regression was used to evaluate the consistency of statin prescribing according to national clinical guidelines by risk category and deprivation quintile.
Results
A total of 324,526 patients were included. Of those, 116,947 (36%) of patients were assigned to a high CVD risk category, primarily older adults, males, and those with co-morbidities. There were statistically significant differences between least (quintile 1) and most (quintile 5) deprived socioeconomic quintiles, with those at high CVD risk disproportionately in Q5 (odds ratio 1.4). Overall, 48% of high-risk patients had at least one statin prescription in their record. Patients in the lower socioeconomic groups had a higher risk of statin treatment which deviated from clinical guidelines.
Conclusions
Primary care patients who are at high CVD risk are more often male, older, have more co-morbidities and be assigned to more deprived SES quintiles, compared to those at low CVD risk. Additionally, patients who experience more challenging socioeconomic situations may be less likely to receive CVD treatment that is consistent with care guidelines.
Similar content being viewed by others
Background
Cardiovascular diseases (CVD) are significant causes of morbidity and mortality in Canada [1]. Fixed and modifiable risk factors such as age, gender, smoking, and diabetes are well known to affect individual risk of myocardial infarction and stroke [2]. There is evidence to suggest that lower socioeconomic status (SES) may contribute to a higher risk of CVD for individuals [3,4,5]. While the prevalence of CVD and its associated risk factors has been gradually increasing in Canada, the highest rates are observed among those of lower SES [6]. The importance of SES to CVD risk, including pharmacotherapy management, has been described in other countries such as the United Kingdom, [7, 8] but is not well studied in a Canadian primary care context.
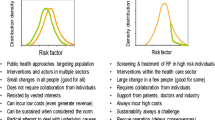
The assessment and management of cardiovascular risk by primary care providers is a key component in reducing the population burden of CVD [9]. Current Canadian clinical guidelines recommend primary health care providers use a validated cardiovascular risk calculator to inform appropriate, patient-centered, management strategies to reduce CVD incidence, morbidity and mortality [2, 9, 10]. These guidelines also recommend that patients with known CVD should be offered statins for secondary prevention unless they experience adverse effects [2]. Targeting those individuals without evidence of established cardiovascular disease is considered primary prevention, whereas secondary prevention targets individuals with prior vascular events, or with evidence of known atherosclerotic vascular disease (Appendix A).
Despite these recommendations, an observational study in Manitoba demonstrated that many individuals who were prescribed statins had no history of CVD in their medical record (suggesting their use for primary prevention), and a majority of those with CVD were not prescribed statins as a secondary prevention measure [11]. This finding indicates a potential care gap and offers an opportunity to describe the potential effect of SES on prescribing appropriateness.
The primary objective of this study was to estimate the cardiovascular risk of patients attending primary care practices across Canada. The secondary objective was to evaluate concordance of current clinical practice guidelines for statin prescribing according to patients’ cardiovascular risk and socioeconomic status.
Methods
Data source
The pan-Canadian Primary Care Sentinel Surveillance Network (CPCSSN) is a collaboration of practice-based research networks which extract and process de-identified patient data from electronic medical records (EMR) in primary care [12]. The CPCSSN database includes key cardiovascular risk factor data, such as patient age, sex, smoking status, serum lipids, blood pressure, and diagnoses. CPCSSN uses validated case definitions to identify patients with common chronic conditions, including hypertension and diabetes [13]. The CPCSSN database and processes for cleaning and standardization have been described in detail elsewhere [12,13,14,15].
Study design and participant selection
This was a cross-sectional study using national CPCSSN data up to December 31, 2016. Approximately 1.6 million patients of all ages are included in the database. For this study, patients aged 35–75 years with at least one visit to their primary care provider in the period January 1, 2012 to December 31, 2016 were included. Patients without a recorded birth year or gender, or without sufficient data to assign to a cardiovascular risk category, were excluded. CPCSSN data overall is considered to be reasonably representative of the Canadian base population, with slight skewing in favour of females and older adults [12, 14].
Primary outcome measurement
The primary study outcome was the proportion of patients at high, medium or low risk of developing CVD based on the 2016 Canadian Cardiovascular Society (CCS) guidelines (Fig. 1), reported by age group, sex (male or female), comorbid conditions (using validated definitions for diabetes mellitus and hypertension [13]), current smoking status and SES quintile. The Framingham Risk Score (FRS), which is recommended for use by the CCS, [2] was used to estimate 10-year CVD risk and facilitated the categorization of risk groups. Variables from the CPCSSN data used to calculate the FRS were patient age, sex, current smoking status, diagnosis of diabetes (using the validated CPCSSN definition), systolic blood pressure (BP), total cholesterol and high density lipoprotein (HDL) cholesterol. Patients with established vascular disease were not included in the FRS calculation, as this score reflects future CVD risk. SES was expressed as a deprivation quintile combining the material and social scores, as described by Pampalon et al., [16] with one (1) being the least deprived and five (5) being the most deprived.
Patients were categorized in the high risk group if any of the following criteria were met:
-
FRS ≥ 20%
-
Diabetes diagnosis and age ≥ 40 years
-
Diabetes diagnosis for ≥ 15 years and age ≥ 30 years
-
Low density lipoprotein (LDL) cholesterol ≥ 5.0 mmol/L (at initiation of statin)
-
Diagnosis indicating CVD (i.e., secondary prevention), as defined in Appendix A.
Patients deemed to be at moderate risk (that is, FRS between 10–19% and no other criteria from the high-risk group) were not included in the regression analysis because treatment decisions in this group are more nuanced and we did not have information about the clinician-patient conversations around prescribing that may have taken place.
Secondary outcome measurement
The secondary outcome focused on evaluating the concordance with guideline recommended care for statin prescribing according to CVD risk and SES quintiles. We investigated whether a patient received a statin prescription in accordance with current guidelines by observing the presence of a statin prescription for those considered at high CVD risk or the absence of a statin prescription for those at low CVD risk (FRS < 10% and no high-risk criteria) [2, 9]. Inconsistency with current guidelines was measured by identifying patients who were found to have received a statin prescription and were considered low risk or who were in a high-risk category and did not have evidence of a statin prescription.
Medication records in the EMR reflect products that have been prescribed by primary care providers, but do not necessarily contain all medications prescribed elsewhere (e.g. by a cardiologist). CPCSSN codes prescription data in a standardized way using the Anatomical Therapeutic Chemical (ATC) classification system. The ATC codes used to describe statins and combination medications were C10AA, C10AB, and C10AX. In order to exclude those who did not initiate their medication or who may have been prescribed a statin in error, statin prescription was counted for patients who had at least two refill prescriptions. This method has been used previously [11].
Analysis
Chi-square was used to determine statistically significant differences between categorical variables, such as age group and deprivation quintiles. A simple logistic regression analysis was used to evaluate the association of patient characteristics on CVD risk. The dependent variable was defined as whether the statin prescription deviated from guideline recommendations (1 = Yes, 0 = No). Independent variables were age group, sex, SES, diabetes and hypertension. A multiple logistic regression analysis was performed using backward elimination on all three independent variables together to adjust for their effects.
SQLServer2012 and Python 2.7.10 were used to retrieve data from CPCSSN and compute the FRS. Statistical analyses were performed using SPSS version 24 and 28 (IBM 2016) [17]. The protocol was reviewed and approved by the Conjoint Heath Research Ethics Board of the University of Calgary (REB17-0992).
Results
From the initial cohort of patients aged 35–75 years with at least one visit to their primary care provider between 2012–2016 (N = 511,610), 324,526 had sufficient information present in their EMR to assign to a CV risk category (Supplementary Fig. 1; Table 1). There was no postal code information for about 45% of these patients, therefore socioeconomic quintiles could only be calculated for 176,787 patients (34.6% of the initial cohort).Table 1 describes the demographic and clinical characteristics of the patients assigned to the three risk categories, by age, sex, FRS and component risk factors, overall CVD risk and SES quintile. A larger proportion of older adults were identified as being at higher CVD risk than younger adults. Males were more often categorized as high risk (48%) compared to females (26%). Individuals who were assigned to the most deprived socioeconomic quintile were more often included in the high-risk category (43%) compared to patients in the least deprived quintile (30%).
When considering statin prescribing guidelines, 7% of low-risk patients had received a statin prescription but only 48% of potentially high-risk patients had received one (Table 1). Figure 2 summarizes the proportion of patients with a statin prescription according to deprivation quintiles and risk groups (N = 42,360). Among those in the most deprived quintile, slightly more patients receiving a statin (51%) were categorized as high risk compared to the least deprived quintile (48%) (p < 0.001).
The final adjusted logistic model (Table 2) indicated that older patients were more likely to receive statin therapy in a way that was not concordant with the guidelines, relative to a reference age group of 35–44 years. In particular, older patients (aged 65–75 years) were found to have nearly four times the odds of statin prescribing that was not concordant with guidelines (adjusted OR = 3.84, 95% CI 3.66–4.02). Likewise, men have nearly twice the odds as women of receiving statins outside of guideline recommendations for their CVD risk (adjusted OR = 1.74, 95% CI 1.70–1.79). In terms of socioeconomic status, patients in the two most deprived quintiles have 1.10 to 1.21 times the odds of statin prescribing inconsistent with guidelines compared to the least deprived. Patients diagnosed with diabetes and hypertension also had higher odds of being prescribed statins that were not concordant with guidelines, with adjusted OR = 2.25 for those with diabetes and adjusted OR = 1.27 for those with hypertension.
Discussion
Among our sample of primary care patients in Canada, 36% were considered to be in a high-risk group, which included a higher proportion of males, older adults, and individuals with lower SES. Our finding that patients who lived in areas associated with high levels of deprivation had an increasingly high-risk CVD profile is not surprising and is consistent with studies in Canada and other international jurisdictions [5, 18,19,20,21,22].
Nearly half of high-risk patients were not receiving statins in accordance with the national guidelines, and few (7%) low-risk individuals were receiving statins when they potentially would not benefit (Table 1). Of concern, there was a clear gradient in the prescribing of statins in accordance with guidelines by SES, with patients in the most deprived quintile at higher odds of experiencing CVD management that deviated from clinical guidelines. Similarly inequitable statin prescribing patterns by socioeconomic status were also observed in Denmark, although only among men [23]. The reasons for this are multifaceted and often interlinked; for example, education, occupation and income are consistently associated with many cardiovascular risks, including smoking, hypertension, obesity, physical inactivity, and poor diet, among others [5]. In addition, lower SES is also correlated with poor health literacy and medication non-compliance, resulting from lower levels of education and an inability to afford prescription medications [5, 24, 25]. The effect of social determinants on health and medical care is apparent here and in many other examples worldwide [26, 27].
We anticipate this study will provide an opportunity for clinical improvement in primary care settings. As practices in Canada move toward implementing models of care focused on the patient’s "medical home", [28] strategies to ensure the consistent collection of relevant risk data, including social determinants of health, is an important first step. The subsequent use of these clinical and social risk data to improve patient outcomes is challenging, especially given limited clinician time and guidance, as well as a potential lack of available and appropriate social resources [29]. However, there are examples of ongoing efforts to promote equity-focused primary health care that exist in Canada [30,31,32], with the College of Family Physicians of Canada strongly advocating for health equity as part of their recent strategic plan [33].
Limitations
While this analysis used a large, pan-Canadian sample of primary care patients, the CPCSSN dataset only includes individuals who sought care from their primary care provider. Thus, it may be more likely to contain information for patients who are more ill or visit their provider more often. Our sample was also hindered by missing data; for instance, 45% of patients were missing full postcode required to calculate the Pampalon deprivation quintiles. Some contributing CPCSSN networks do not provide full postal codes for various technical or procedural reasons. It is important to note that the Pampalon index of material and social deprivation is an ecological measure based on the postcode of residence and does not directly reflect the SES of individuals. Further, many individuals were missing data related to their FRS and therefore, the absolute number of patients at risk is likely underestimated. Missing data is a common challenge for analyses using EMR data and of the variables used in the FRS, patient smoking status is most often underreported in primary care EMR data, despite its importance as a risk factor for CVD [34,35,36,37].
The 2016 CCS guidelines used in this study were published at the end of the study time period (2012–2016) and may not have reflected previously recommended prescribing practices. However, there was little difference between the updated 2016 guidelines and its predecessor published in 2012, particular for the high-risk groups.
Lastly, there is insufficient information in the EMR to discern why these prescribing decisions were made or whether treatment was offered but declined. We did not report on the presence of chronic kidney disease (CKD) due to the absence of a validated definition for CPCSSN data at the time of this analysis, which may have been the rationale for statin prescribing when it was seemingly unwarranted. Even so, most patients with CKD experience other vascular risk factors, such as diabetes and hypertension, which would have been captured.
Conclusions
In Canada, primary care patients who are considered at high CVD risk are more often male, older, current smokers, in a lower socioeconomic quintile and with a higher prevalence of comorbid hypertension or diabetes, compared to those at low CVD risk. The odds of receiving care that was not concordant with current care guidelines were found to be greater in the most deprived group. A focus on comprehensive, systematic documentation of CVD risk factors in clinical practice, with attention to socioeconomic influences, may provide action-oriented risk assessment for patients at higher risk of CVD.
Availability of data and materials
The de-identified data that support the findings of this study are available from the national CPCSSN repository but restrictions may apply to the availability of these data, which were used under strict data security and privacy protocols, and so are not publicly available. Access to the national CPCSSN database is however available to approved researchers according to the CPCSSN data access guidelines found here: http://cpcssn.ca/dar/
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical [classification system]
- BP:
-
Blood pressure
- CCS:
-
Canadian Cardiovascular Society
- CKD:
-
Chronic kidney disease
- CPCSSN:
-
Canadian Primary Care Sentinel Surveillance Network
- CVD:
-
Cardiovascular disease
- EMR:
-
Electronic medical record
- FRS:
-
Framingham risk score
- HDL:
-
High density lipoprotein
- LDL:
-
Low density lipoprotein
- mmol/L:
-
Millimole per litre
- OR:
-
Odds ratio
- SES:
-
Socioeconomic status
References
Statistics Canada. Table 13–10–0394–01. Leading causes of death, total population, by age group. doi:https://doi.org/10.25318/1310039401-eng
Anderson TJ, Gregoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can J Cardiol. 2016;32(11):1263–82. https://doi.org/10.1016/j.cjca.2016.07.510.
Squires BP. Cardiovascular disease and socioeconomic status. Can Med Assoc J. 2000;162(9 Suppl):S3.
Najman JM, Wang W, Plotnikova M, et al. Poverty over the early life course and young adult cardio-metabolic risk. Int J Public Health. 2020;65(6):759–68. https://doi.org/10.1007/s00038-020-01423-1.
de Mestral C, Stringhini S. Socioeconomic status and cardiovascular disease: an update. Curr Cardiol Rep. 2017;19(11):1–12. https://doi.org/10.1007/s11886-017-0917-z.
Lee DS, Chiu M, Manuel DG, et al. Trends in risk factors for cardiovascular disease in Canada: Temporal, socio-demographic and geographic factors. CMAJ. 2009;181(3–4):55–66. https://doi.org/10.1503/cmaj.081629.
Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: Prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–82. https://doi.org/10.1136/bmj.39609.449676.25.
Ward PR, Noyce PR, St Leger AS. How equitable are GP practice prescribing rates for statins?: An ecological study in four primary care trusts in north west England. Int J Equity Health. 2007;6:1–14. https://doi.org/10.1186/1475-9276-6-2.
Allan GM, Lindblad AJ, Comeau A, et al. Simplified lipid guidelines: Prevention and management of cardiovascular disease in primary care. Can Fam Physician. 2015;61(10):857–67.
National Institute for Health and Care Excellence (NICE) Guideline Development Group. Cardiovascular disease: risk assessment and reduction, including lipid modification (CG181). https://www.nice.org.uk/guidance/cg181/resources/cardiovascular-disease-risk-assessment-and-reduction-including-lipid-modification-pdf-35109807660997. Published 2016. Accessed September 20, 2021.
Brown F, Singer A, Katz A, Konrad G. Statin-prescribing trends for primary and secondary prevention of cardiovascular disease. Can Fam Physician. 2017;63:495–503.
CPCSSN. Canadian Primary Care Sentinel Surveillance Network (CPCSSN). http://cpcssn.ca. Published 2021. Accessed March 12, 2021.
Williamson T, Green ME, Birtwhistle R, et al. Validating the 8 CPCSSN case definitions for chronic disease surveillance in a primary care database of electronic health records. Ann Fam Med. 2014;12(4):367–72. https://doi.org/10.1370/afm.1644.
Garies S, Birtwhistle R, Drummond N, Queenan J, Williamson T. Data Resource Profile: National electronic medical record data from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). Int J Epidemiol. 2017;46(4):1091–1092f. https://doi.org/10.1093/ije/dyw248.
Garies S, Cummings M, Forst B, et al. Achieving quality primary care data: a description of the Canadian Primary Care Sentinel Surveillance Network data capture, extraction, and processing in Alberta. Int J Popul Data Sci. 2019;4(2).
Pampalon R, Hamel D, Gamache P, Philibert MD, Raymond G, Simpson A. An area-based material and social deprivation index for public health in Québec and Canada. Can J Public Health. 2012;103(SUPPL.2):17–22. doi:https://doi.org/10.17269/cjph.103.3156
IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. 2016.
Dai H, Younis A, Kong JD, Bragazzi NL, Wu J. Trends and Regional Variation in Prevalence of Cardiovascular Risk Factors and Association with Socioeconomic Status in Canada, 2005–2016. JAMA Netw Open. 2021;4(8):2005–16. https://doi.org/10.1001/jamanetworkopen.2021.21443.
Valero-Elizondo J, Hong JC, Spatz ES, et al. Persistent socioeconomic disparities in cardiovascular risk factors and health in the United States: Medical Expenditure Panel Survey 2002–2013. Atherosclerosis. 2018;269:301–5. https://doi.org/10.1016/j.atherosclerosis.2017.12.014.
Alter D., Brandes S, Irvine J, Iron K. Impact of socioeconomic status on cardiovascular outcomes in Canada. Expert Rev Pharmacoeconomics Outcomes Res. 2003;3.
Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation. 2018;137(20):2166–78. https://doi.org/10.1161/CIRCULATIONAHA.117.029652.
Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: Risks and implications for care. Nat Rev Cardiol. 2009;6(11):712–22. https://doi.org/10.1038/nrcardio.2009.163.
Thomsen RW, Johnsen SP, Olesen AV, et al. Socioeconomic gradient in use of statins among Danish patients: Population-based cross-sectional study. Br J Clin Pharmacol. 2005;60(5):534–42. https://doi.org/10.1111/j.1365-2125.2005.02494.x.
Stormacq C, Van Den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review Health Promot Int. 2019;34(5):E1–17. https://doi.org/10.1093/heapro/day062.
Law MR, Cheng L, Dhalla IA, Heard D, Morgan SG. The effect of cost on adherence to prescription medications in Canada. CMAJ. 2012;184(3):297–302. https://doi.org/10.1503/cmaj.111270.
Marmot M, Bell R. Fair society, healthy lives. Public Health. 2012;126(SUPPL.1):S4. doi:https://doi.org/10.1016/j.puhe.2012.05.014
Braveman P, Gottlieb L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014;129(SUPPL. 2):19–31. https://doi.org/10.1177/00333549141291s206.
College of Family Physicians of Canada. Summary of a New Vision for Canada: Family Practice - the Patient’s Medical Home 2019. Mississauga, ON; 2019. https://patientsmedicalhome.ca/files/uploads/PMH2019Summary_ENG.pdf.
Andermann A. Taking action on the social determinants of health in clinical practice: A framework for health professionals. CMAJ. 2016;188(17–18):E474–83. https://doi.org/10.1503/cmaj.160177.
O’Neill B, Ferrer R, O’Brien P, et al. Improving equity through primary care: Proceedings of the 2019 Toronto international conference on quality in primary care. Ann Fam Med. 2020;18(4):364–369. doi:https://doi.org/10.1370/afm.2560
Browne AJ, Varcoe C, Ford-Gilboe M, Wathen CN. EQUIP Healthcare: An overview of a multi-component intervention to enhance equity-oriented care in primary health care settings. Int J Equity Health. 2015;14(1):1–11. https://doi.org/10.1186/s12939-015-0271-y.
Pinto AD, Bloch G. Framework for building primary care capacity to address the social determinants of health. Can Fam Physician. 2017;63(11):e476–82.
College of Family Physicians of Canada. CFPC Strategic Plan 2017–2022. Mississauga, ON; 2018.
Greiver M, Aliarzadeh B, Meaney C, et al. Are we asking patients if they smoke?: Missing information on tobacco use in Canadian electronic medical records. Am J Prev Med. 2015;49(2):264–8. https://doi.org/10.1016/j.amepre.2015.01.005.
Garies S, Cummings M, Quan H, et al. Methods to improve the quality of smoking records in a primary care EMR database: Exploring multiple imputation and pattern-matching algorithms. BMC Med Inform Decis Mak. 2020;20(1):1–10. https://doi.org/10.1186/s12911-020-1068-5.
Taggar JS, Coleman T, Lewis S, Szatkowski L. The impact of the Quality and Outcomes Framework (QOF) on the recording of smoking targets in primary care medical records: Cross-sectional analyses from The Health Improvement Network (THIN) database. BMC Public Health. 2012;12:329. https://doi.org/10.1186/1471-2458-12-329.
Aref-Eshghi E, Leung J, Godwin M, et al. Low density lipoprotein cholesterol control status among Canadians at risk for cardiovascular disease: Findings from the Canadian Primary Care Sentinel Surveillance Network Database. Lipids Health Dis. 2015;14(1):1–6. https://doi.org/10.1186/s12944-015-0056-8.
Acknowledgements
The authors would like to acknowledge the invaluable help offered by Ken Martin and numerous individuals within the CPCSSN network, not forgetting the primary care providers and their patients whose data this study reviewed.
Funding
This study was part of a family medicine residency research project and received no funding.
Author information
Authors and Affiliations
Contributions
ISJ and BM conceptualized the study. ISJ, BS and GP conducted the analysis. All authors contributed to the development of the methods, interpretation of findings, and the drafting and revision of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Calgary’s Conjoint Health Research Ethics Board (CHREB) (REB17-0992) and adheres to all relevant guidelines and regulations for research involving de-identified health data (e.g. CHREB, Tri-Council Policy Statement on the Ethical Conduct for Research Involving Humans [TCPS2]). A waiver of individual patient consent was granted by Research Ethics Boards at universities affiliated with each participating CPCSSN practice-based research network for the collection and use of de-identified EMR data, including the CHREB at the University of Calgary.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Appendix A: ICD-9 codes used to identify patients in the secondary prevention group
Additional file 2:
The RECORD statement – checklist of items, extended from the STROBE statement, that should be reported in observational studies using routinely collected health data
Additional file 3:
Patient flow diagram
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Johnston, I.S., Miles, B., Soos, B. et al. A cross-sectional study evaluating cardiovascular risk and statin prescribing in the Canadian Primary Care Sentinel Surveillance Network database. BMC Prim. Care 23, 128 (2022). https://doi.org/10.1186/s12875-022-01735-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-022-01735-6