Abstract
Background
Canadians are known to be frequent users of emergency department (ED) care. However, the exchange of information from ED visits to family physicians (FPs) is not well known. Our objectives were to determine whether Canadian FPs received information about their patient’s ED visit and the patient characteristics related to the receipt of ED information.
Methods
This study was a descriptive record linkage study of FP Electronic Medical Record (EMR) data linked to health administrative data. Our study cohort included patients who had at least one ED visit in 2010 or 2015 in Ontario, Canada. An ED visit could include a transfer to or from another ED. The receipt of information from an ED note was examined in relation to patient age, sex, neighbourhood income quintiles, rurality and comorbidity.
Results
There were 26,609 patients in 2010 and 50,541 patients in 2015 with at least one ED visit. In 2010, 53.3% of FPs received an ED note for patients having a single ED visit compared to 41.0% in 2015. For patients with multiple ED visits, 58.2% of FPs received an ED note in 2010 compared to 45.7% in 2015. FPs were more likely to receive an ED note for patients not living in low income neighbourhoods, older patients, patients living in small urban areas and for patients having moderate comorbidity. FPs were less likely to receive a note for patients living in rural areas.
Conclusions
Community-based FPs are more likely to get information after an ED visit for their older and sicker patients. However, FPs do not receive any information from EDs for over half their patients. Electronic health record technologies and their adoption by ED providers need to improve the seamless transfer of information about the care provided in EDs to FPs in the community.
Similar content being viewed by others
Background
Canadians are known to be frequent users of emergency department (ED) care amongst developed nations [1, 2]. Canadian ED users were ranked number one in an international comparison of 34 countries when they indicated they went to the ED because their family physician (FP) could not provide the care they needed [3]. Only 34% of Canadians said they could get evening or weekend care without going to the ED. [4] However for people who saw their FP regularly for their chronic disease management, ED use was reduced [5,6,7]. The benefits of improved access to after-hours care have been equivocal, with little difference in ED visits amongst primary care delivery models that offer better after-hours access [8]. Indeed, not having a FP or poor access to a FP may not be the reasons for frequent use of EDs by some people [9, 10]. Regardless of the reasons Canadians go to the ED, it is important to have the information gained during an ED visit provided to a patient’s FP so that acute care is followed up, complications from chronic diseases are better managed and mental health illnesses are supported.
Since the receipt of hospital discharge information by a patient’s FP has been associated with improved chronic disease management and fewer prescribing errors [11,12,13,14,15], recommendations have been made to ensure a hospital discharge note/summary is available to a FP within 48 h of a patient leaving the hospital [16]. With an increasing proportion of ED visits made by patients who are older and more medically complex, there is a need for FPs to have information from their patient’s ED visit [17]. Inadequate follow up after an ED visit is associated with disease complications [18, 19]. Furthermore, improving the coordination of care between ED and primary care could improve the duplication of treatments, opportunities to educate patients on appropriate ED use and better disease management [20]. However, little information exists on whether FPs received information from EDs.
Canadians have universal healthcare where all medically necessary physician visits are provided to residents and paid and managed by provincial government health plans [21]. In Ontario, Canada’s most populous province, FPs are the physician providers of primary care for adults and most children [22]. With the initiation of primary care reform in Ontario in 2003, an increasing proportion of patients are formally enrolled (rostered) to an individual FP for all their primary care [23,24,25]. In 2017, 88.6% of people in Ontario have a FP, with 82.9% being formally enrolled (rostered) with a FP [26].
The initial focus of Electronic Health Technology (EHT) adoption by Ontario EDs was to support ED clinicians with point-of-care access to investigations (such as laboratory and radiological test results), as concerns about information gaps on patient care existed [27]. In 2014 the provincial digital health strategy included the expansion of an integrated EHT, including improvements with communication and connectivity from EDs [28]. Prior to 2014, the standard method of communication from an ED physician to a FP was a hand-written one-page report provided directly to the patient or FAXed to their FP. Once received by the FP’s office, these ED notes would subsequently be scanned into a FP electronic medical record (EMR). The provincial digital health strategy specifically includes the expansion of a hospital medical record (HMR) system whereby FP EMRs directly receive hospital discharge summaries, notes from ED visits and the results of some radiological investigations [29]. However, there is no data which estimates whether community-based FPs actually receive this information.
In 2019, 86% of Canadian FP practices use EMRs for their clinical care [30]. FP EMRs contain a wealth of information describing care provided to their patients and this data has increasingly been used for research and quality improvement [31, 32], including how well the healthcare system coordinates care across different health care sectors [33].
Therefore, the objectives of this study were to determine whether information from a patient’s ED visit is received by their FP, to examine patient factors related to the receipt of ED information and to see if changes in the receipt of ED information by FPs has occurred between 2010 and 2015.
Methods
Study design
We conducted a descriptive analysis on a cohort of patients enrolled with FPs in Ontario, Canada who went to the ED in 2010 and 2015.
Sources of data
We used information gathered from the Electronic Medical Records Primary Care (EMRPC) database held at ICES, which is comprised of EMRs from a network of community-based FPs across Ontario [34]. EMRPC contains the entire clinical record of FP patients, including their cumulative patient profile, progress notes, consultant notes, radiological and laboratory tests, hospital and emergency discharge notes and referrals. ICES is a ‘prescribed entity’ under Ontario privacy legislation which provides the legal authority to collect individual level health information, as ICES has the policies and procedures in place to protect patient privacy and confidentiality [35]. The health administrative data for this study included ED visits from the Canadian Institute for Health Information National Ambulatory Record System (NACRS) database, physician encounter claims from the Ontario Health Insurance Plan (OHIP) database and patient age and sex held in the Registered Persons Database (RPDB). These datasets were linked using unique encoded identifiers and analyzed at ICES.
ED study cohort
Our study cohort include EMRPC patients who had at least one NACRS ED visit in 2010 or 2015. EMRPC patients were excluded if they did not have a valid health card number or date of birth, they were not formally enrolled (rostered) to the EMRPC FP or if their ED visit resulted in an admission to hospital.
We used previously standardized methods to define an ED visit from ED health service research in Ontario [36]. An ED visit may include multiple NACRS ED visit claims or records. For example, an ED visit could include an ED visit that involves a transfer to another ED or facility and an ED visit which is a transfer from another ED or facility or a revisit within 28 days. An ED revisit within 28 days with no indication of an ED transfer is not considered the same ED visit and would be considered a separate ED visit. For our ED study cohort, we separated patients having one ED visit versus patients having multiple ED visits.
ED information in FP EMR notes
All EMRPC specialist consultant notes for each patient were examined starting after the ED visit dates up to 6 months after the end each study cohort. We used a hieratical method to identify ED notes/information in the EMR. First, we identified the EMR ED note using a date which was the same as the ED visit date. For the remaining ED visits, we identified any type of specialist consultant note with the same date as the ED visit date. Finally, for the remaining ED visits we identified any notations in the EMR with terms “Emerg”, “ER”, “Urgent Care” and their misspellings and combinations. These notations included non-note formats such as laboratory and radiological test results.
Covariates
The covariates in our study included patient age, sex, rurality, neighbourhood income quintiles and comorbidity. Statistics Canada’s postal code conversion files and census data were used to calculate neighbourhood income quintiles [37] and the location of residence as defined by the rurality index of Ontario [38]. The Johns Hopkins ACG® System Aggregated Diagnosis Groups (ADGs) were used to measure patient comorbidity from all health care encounters in the year prior to their ED visit [39]. Validated chronic disease administrative data algorithms were used to identify comorbidities such as a previous history of an acute myocardial infarction (post-AMI), asthma, chronic obstructive pulmonary disorder (COPD), congestive heart failure (CHF), diabetes, hypertension or mental health conditions [40,41,42,43,44,45,46,47].
Statistical analysis
For 2010 and 2015, we calculated the proportion of ED notes received by FPs for both patients with a single ED visit and those with multiple ED visits. Single ED visit patients were counted as having an ED note if at least one note was received. Multiple ED visit patients were counted as having an ED note if a note from any ED visit was received. We conducted bivariate analyses of patient characteristics between patients having single or multiple ED visits in 2010 and 2015. For 2015, we compared patient characteristics when their FP received and or did not receiving an ED note. A p < 0.001 indicated statistical significance. Logistic regression was undertaken to examine the association of patient characteristics on their independent role with the receipt of any ED notes. All analyses were performed using SAS Enterprise Guide version 7.1 (Cary, NC) [48].
Results
For our primary care patient cohort, there were 26,609 patients in 2010 and 50,541 patients in 2015 with at least one ED visit. In both years, most patients had a single ED visit. Table 1 provides the demographic and comorbidity characteristics of the ED study cohort with column percentages provided for each characteristic. In both 2010 and 2015, a higher proportion of patients with multiple ED visits were adults aged 18 to 24 years and 65 years and older, living in areas with lower income, living in rural locations, and having higher ADG comorbidities compared with those with a single ED visit. The 2015 ED cohort was older and had a higher proportion of comorbidities compared to the 2010 ED cohort.
Table 2 describes the receipt of an ED note (and type of note) by a patient’s FP. FPs received an ED note from 10,471 (53.3%) patients and from 15,257 (41.0%) patients having a single ED visit in 2010 and in 2015, respectively. For patients with multiple ED visits, the patient’s FP received an ED note from 4044 (58.2%) patients in 2010 and from 6106 (45.7%) patients in 2015. In 2010, a higher proportion of ED notes received by FPs were ED consultation notes in comparison to 2015.
Table 3 compares the characteristics of single and multiple ED visit patients whose FPs received or did not receive an ED note in 2015. For patients with either a single ED visit or multiple ED visits, FPs received an ED note from a higher proportion of patients who were older, were living in urban areas, and had moderate to high comorbidity compared to patients whose FP did not receive an ED note. A lower proportion of patient’s FP received an ED note were living in the lowest neighbourhood income quintile for single ED visits, but not for multiple ED visits. For patients with CHF, COPD, diabetes, hypertension and mental health conditions having a single ED visit only, a higher proportion of their FPs received an ED note.
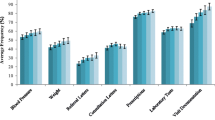
An examination of patient factors associated with the receipt of an ED note by FPs are presented in Table 4. After adjusting for all other covariates, FPs were more likely to receive an ED note for patients not living in low income neighbourhoods. Compared to patients living in major urban areas, FPs were more likely to receive an ED note for patients living in small urban areas but less likely to receive them for patients living in rural areas. FPs were more likely to receive an ED note for patients having moderate comorbidity compared to the people with no or low comorbidity. Similar findings were found between patients having single versus multiple ED visits.
Discussion
In contrast to the receipt of a discharge note after a hospital admission, there are no established benchmarks for FPs receiving information about their patients’ ED visits. In our study, not quite half of patients visiting the ED had information provided to their FP. We used a broad definition of an ED note in this study. An ED note could include an encounter or consultation note, a notification that a patient was seen and/or discharged from the ED or the results of laboratory or radiological tests. We also credited multiple ED visits as having provided the FP a note if anyone of the ED visits had an associated note found in the FP’s EMR.
While EMR use for clinical care is similar between FPs and specialist physicians in Ontario [49], the proportion of Ontario ED physicians documenting their clinical encounters using EMRs is unknown. The implementation of EHRs in EDs continues to evolve in Ontario. EHR/EMR implementation and adoption poses unique challenges as an ED cannot shut down while testing a system and the impact of ED physician allocation and efficiencies are different than office-based practices [50]. A recent Ontario study found a reduction in ED physician efficiencies over time that did not recover to baseline after the implementation of an ED EHR [51]. However an important objective of the digital health strategy is to improved communications with providers across healthcare sectors. In our study we found a lower rate of communication from EDs to community FPs in 2015 compared to 2010. Benchmarks for communication with community providers need to be established and regularly measured as EDs adopt EHRs to ensure that information is truly received by community providers in a timely manner.
Whether a written note is FAXed to a community FP or an electronic note is directly sent into the FPs EMR, it is a necessary first step that the patient’s FP be identified when coming to the ED. One reason that FPs do not receive information is because the FP’s contact information held in EDs may be inaccurate or unknown. Similar to our study, a recent survey found over half of Canadian FPs (59% in Ontario) say they receive notification of an ED visit [30]. Indeed only 22% of Canadian FPs said they could communicate patient clinical summaries across health care sectors [16]. EHR technology is already imbedded in ED and primary care practices. However, improvements are needed with the integration of technologies that interface across different healthcare settings to improve communication between EDs and community FPs in a seamless manner, without increasing the workload on either busy provider.
Rural patients were less likely to have their FPs received an ED note. However, FPs practicing in rural areas may see their own patients in the ED and therefore may not send themselves an ED note [52]. These ED visits may be related to chronic disease management, rather than an acute condition. We found moderate comorbidity was associated with the receipt of ED notes, yet having a chronic condition did not. Our measure of comorbidity (ADGs) are case mix measures that combine health conditions to determine a person’s need for health services [39]. Patients having more health care services may be a trigger to send information to the FP. However, patients with a defined chronic condition may be stable with respect to that condition, or see the ED for another reason, and this does not prompt ED providers to send information to the community FP.
Our study included a large cohort of FPs from rural and urban regions in Ontario and practicing in academic and community settings. We used EMR and health administrative data, as opposed to survey data which is susceptible to recall bias. While our study cohort of FPs and their patients are similar to FPs practicing in Ontario, it does over represent rural FPs and Canadian trained FPs [34]. We did not examine the quality of the ED information received, nor the receipt of ED notes by any specific acute or chronic disease conditions. We did not examine telephone or other direct communication between ED providers and FPs and therefore may be underestimating communication about ED visits. Finally, we did not examine the influence of ED provider or ED characteristics (such as their level of EHR adoption) on the receipt of ED information by community FPs.
Conclusions
FPs are more likely to get information after an ED visit for their older and sicker patients. However, FPs do not receive information from EDs for over half their patients. Electronic health record technologies, alongside the adoption of their use by ED providers need to improve the seamless transfer of information about the care provided in ED to FPs in the community.
Availability of data and materials
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
References
Osborn R, Squires D, Doty MM, Sarnak DO, Schneider EC. New Survey of 11 Countries, U.S. Adults Still Struggle with Access to and Affordability of Health Care. Health Affairs Web First. 2016;35:2327–36.
Gunja MZ, Tikkanen R, Seervai S, Collins SR. What Is the Status of Women’s Health and Health Care in the U.S. Compared to Ten Other Countries? Commonwealth Fund. 2018. https://www.commonwealthfund.org/publications/issue-briefs/2018/dec/womens-health-us-compared-ten-other-countries (accessed 20 Oct 2020).
Doty MM, Tikkanen R, Shah A, Schneider EC. Primary care physicians’ role in coordinating medical and health-related social needs in eleven countries. Health Affairs. 2019; https://www.commonwealthfund.org/sites/default/files/2019-12/PDF_2019_intl_hlt_policy_survey_primary_care_phys_CHARTPACK_12-10-2019.pdf (accessed 20 Oct 2020).
Moineddin R, Meaney C, Agha M, Zagorski B, Glazier RH. Modeling factors influencing the demand for emergency department services in Ontario: a comparison of methods. BMC Emerg Med. 2011;11:13. Published 2011 Aug 19. https://doi.org/10.1186/1471-227X-11-13.
Mian O, Pong R. Does better access to FPs decrease the likelihood of emergency department use? Results from the primary care access survey. Can Fam Physician. 2012;58(11):e658–66.
van den Berg MJ, van Loenen T, Westert GP. Accessible and continuous primary care may help reduce rates of emergency department use. An international survey in 34 countries. Fam Pract. 2016;33(1):42–50.
Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract J R Coll Gen Pract. 2013;63:e813–20. https://doi.org/10.3399/bjgp13X675395.
Kiran T, Moineddin R, Kopp A, Frymire E, Glazier RH. Emergency department use and enrollment in a medical home providing after-hours care. Ann Fam Med. 2018;16(5):419–27.
Palmer E, Leblanc-Duchin D, Murray J, Atkinson P. Emergency department use. Is frequent use associated with a lack of primary care provider? Can Fam Physician. 2014;60:e223–9.
Chan BT, Ovens HJ. Frequent users of emergency departments. Do they also use family physicians' services? Can Fam Physician. 2002;48:1654–60.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–41.
Uppal NK, Eisen D, Weissberger J, Wyman RJ, Urbach DR, Bell CM. Transfer of care of postsurgical patients from hospital to the community setting: cross-sectional survey of primary care physicians. Am J Surg. 2015;210(4):778–82. https://doi.org/10.1016/j.amjsurg.2015.03.006 Epub 2015 May 14.
Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–51.
van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–92.
Hoyer EH, Odonkor CA, Bhatia SN, Leung C, Deutschendorf A, Brotman DJ. Association between days to complete inpatient discharge summaries with all-payer hospital readmissions in Maryland. J Hosp Med. 2016;11(6):393–400. https://doi.org/10.1002/jhm.2556 Epub 2016 Feb 23.
Health Quality Ontario. Transitions Between Hospital and Home. 2016. https://www.hqontario.ca/Portals/0/documents/qi/health-links/ensure-discharge-summary-available-within-hours-en.pdf (accessed 20 Oct 2020).
Health Quality Ontario. Under Pressure: Emergency department performance in Ontario. Toronto: Queen’s Printer for Ontario; 2016. https://www.hqontario.ca/portals/0/Documents/system-performance/under-pressure-report-en.pdf (accessed 20 Oct 2020)
Schull MJ. Making aftercare more than an afterthought: patient follow-up after emergency department discharge in Ontario. Healthcare Q. 2014;17(2):11–3.
McCusker J, Roberge D, Vadeboncoeur A, Verdon J. Safety of discharge of seniors from the emergency department to the community. Healthcare Quarterly. 2009;12(Special Issue):24–32.
Carrier E, Yee T, Holzwart RA. Coordination between emergency and primary care physicians. Adv Health Policy Res. 2011;3. https://www.nihcr.org/analysis/improving-care-delivery/prevention-improving-health/ed-coordination/.
Tiedemann M. Legal and Social Affairs Division. Parliament and Information Research Services. The Canada Health Act-An Overview (Background Paper). Publication No. 2019–54-E. Ottawa: Library of Parliament, Canada ©; 2020.
Jaakkimainen L, Schultz SE, Klein-Geltink JE, Thiruchelvam D, Kopp A. Ambulatory physician Care for Adults and Guttman a, Schultz SE, Jaakkimainen L. primary Care for Children. In: Jaakkimainen L, Upshur R, Klein-Geltink JE, Leong a, Maaten S, Schultz SE, Wang L, editors. Primary Care in Ontario: ICES atlas. Toronto: Institute for Clinical Evaluative Sciences; 2006.
Glazier RH, Hutchison B, Kopp A. Comparison of Family Health Teams to Other Ontario Primary Care Models, 2004/05 to 2011/12. Toronto: Institute for Clinical Evaluative Sciences; 2015. ISBN: 978–1–926850-56-6 (Online)
McLeod L, Buckley G, Sweetman A. Ontario primary care models: a descriptive study. CMAJ Open. 2016;4(4):E679–88. https://doi.org/10.9778/cmajo.20160069.
Schultz SE, Glazier RH. Identification of physicians providing comprehensive primary care in Ontario: a retrospective analysis using linked administrative data. CMAJ Open. 2017;5(4):E856–63. https://doi.org/10.9778/cmajo.20170083.
Jaakkimainen L, Bayoumi I, Glazier R, Premji K, Kiran T, Khan S, et al. Development and validation of an algorithm using health administrative data to define patient attachment to primary care providers. J Health Organ Manag. 2021;35(6):733–43. https://doi.org/10.1108/JHOM-05-2020-0171.
Stiell A, Forster AJ, Stiell IG, van Walraven C. Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ. 2003;169(10):1023–8.
Ontario Ministry of Health and Long-Term Care. Patients First: Action Plan for Health Care. 2015.
OntarioMD Inc. About HRM®: increase the clinical value of your EMR. 2021. https://www.ontariomd.ca/products-and-services/health-report-manager/about-hrm (accessed 21 Jun 2021).
Canadian Institute for Health Information. How Canada compares: results from the commonwealth Fun’s 2019 international health policy survey of primary care physicians – accessible report. Ottawa: CIHI; 2020.
Jaakkimainen RL, Bronskill SE, Tierney MC, Herrmann N, Green D, Young J, et al. Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J Alzheimers Dis. 2016;54:337–49.
Zhang H, Candido E, Wilton AS, Duchen R, Jaakkimainen L, Wodchis W, et al. Identifying transitional high cost users from unstructured patient profile written by primary care physicians. Pac Symp Biocomput. 2020;25:127–38 Epub 2020 Jan 1.
Jaakkimainen RL, Glazier R, Barnsley J, Salkeld E, Lu H, Tu K. Waiting to see the specialist: patient and provider characteristics of wait times from primary to specialty care. BMC Family Pract. 2014;15:16.
Tu K, Widdifield J, Young J, Oud W, Ivers N, Butt D, et al. Are family physicians comprehensively using electronic medical records such that the data can be used for secondary purposes? A Canadian perspective. BMC Med Inform Decis Mak. 2015;15:67 PMID 26268511.
ICES. Privacy at ICES. https://www.ices.on.ca/Data-and-Privacy/Privacy-at-ICES (accessed 20 Oct 2020).
Li G, Lau JT, McCarthy ML, Schull MJ, Vermeulen M, Kelen GD. Emergency department utilization in the United States and Ontario. Canada Acad Emerg Med. 2007;14(6):582–4 Epub 2007 Apr 30.
Denny K, Davidson MJ. Area-based socio-economic measures as tools for health disparities research, policy and planning. Can J Public Health. 2012;103(8):S4–6.
Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Toronto: Ontario Medical Review; 2000.
The Johns Hopkins ACG® System Version 10.
Austin PC, Daly PA, Tu JV. A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J. 2002;144:290–6.
Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying patients with physician-diagnosed asthma in health administrative databases. Can Respir J. 2009;16:183–8.
Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physician diagnosed COPD in health administrative databases. COPD. 2009;6(5):388–94.
Schultz SE, Rothwell DM, Chen Z, Tu K. Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis Inj Can. 2013;33(3):160–6.
Lipscombe LL, Hwee J, Webster L, Shah BR, Booth GL, Tu K. Identifying diabetes cases from administrative data: a population-based validation study. BMC Health Serv Res. 2018;18:316.
Tu K, Lipscombe LL, Chen ZL. For the CHEP outcomes research taskforce. Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ. 2008;178(11):1429–35.
Steele L, Glazier R, Lin E, Evans M. Using administrative data to measure ambulatory mental health service provision in primary care. Med Care. 2004;42:960–5.
Kurdyak P, Lin E, Green D, Vigod S. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry. 2015;60:362–8.
SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC).
Canada Health Infoway Inc. 2018 Canadian physician survey. Physicians’ Use of Digital Health and Information Technologies in Practice. 2018. https://infoway-inforoute.ca/en/component/edocman/resources/reports/benefits-evaluation/3643-2018-canadian-physician-survey (accessed 20 Oct 2020).
Rosenfield D, Harvey G, Jessa K. Implementing electronic medical records in Canadian emergency departments. CJEM. 2019;21(1):15–7.
Calder-Sprackman S, Clapham G, Kandiah T, Choo-Foo J, Aggarwal S, Sweet J, et al. The impact of adoption of an electronic health record on emergency physician work: a time motion study. JACEP Open. 2021;2:e12362. https://doi.org/10.1002/emp2.12362.
Bhimani M, Dickie G, McLeod S, Kim D. Emergency medicine training demographics of physicians working in rural and regional southwestern Ontario emergency departments. CJEM. 2007;9(6):449–52. https://doi.org/10.1017/s1481803500015487.
Acknowledgements
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Funding
This study was funded by a Canadian Institutes for Health Research (CIHR) Operating Grant (FRN:1304180).
Author information
Authors and Affiliations
Contributions
Liisa Jaakkimainen was responsible for the study design, analysis framework and she wrote the first draft of the paper. Hannah Chung worked on the analytic plan and the interpretation of results. Hong Lu conducted all the analyses using health administrative data. Bogdan Pinzaru is a health informatician and conducted all the electronic medical record cuts and EMR data analyses. Elisa Candido contributed to the analytic plan and interpretation of results. All authors read the paper and contributed to the editing of paper.
Authors’ information
In 2018, the institute formerly known as the Institute for Clinical Evaluative Sciences formally adopted the initialism ICES as its official name. This change acknowledges the growth and evolution of the organization’s research since its inception in 1992, while retaining the familiarity of the former acronym within the scientific community and beyond. Liisa Jaakkimainen is a senior scientist and program lead of the Primary Care and Health Systems program at ICES. She is an Associate Professor in the Department of Family and Community Medicine and the Institute of Health Policy, Management and Evaluation at the University of Toronto and a staff family physician at the Department of Family and Community Medicine at Sunnybrook Health Sciences Centre. Hannah Chung is a senior epidemiologist at ICES. Hong Lu is a senior analyst at ICES. Bogdan Pinzaru is a health informatician analyst at ICES. Elisa Candido is a staff scientist at ICES.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
ICES is a prescribed entity under Ontario’s Personal Health Information Protection Act (PHIPA). Section 45 of PHIPA authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects that use data collected by ICES under section 45 of PHIPA, and use no other data, are exempt from REB review. The use of the data in this project is authorized under section 45 and approved by ICES’ Privacy and Legal Office.
Consent for publication
Not Applicable.
Competing interests
The authors have no competing interests or conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jaakkimainen, L., Chung, H., Lu, H. et al. The receipt of information by family physicians about their patient’s emergency department visits: a record linkage study of electronic medical records to health administrative data. BMC Fam Pract 22, 235 (2021). https://doi.org/10.1186/s12875-021-01582-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-021-01582-x