Abstract
Background
More than 90% of antibiotics are prescribed in primary care, but 50% may be unnecessary. Reducing unnecessary antibiotic overuse is needed to limit antimicrobial resistance. We conducted a pragmatic trial of a primary care provider-focused antimicrobial stewardship intervention to reduce antibiotic prescriptions in primary care.
Methods
Primary care practitioners from six primary care clinics in Toronto, Ontario were assigned to intervention or control groups to evaluate the effectiveness of a multi-faceted intervention for reducing antibiotic prescriptions to adults with respiratory and urinary tract infections. The intervention included provider education, clinical decision aids, and audit and feedback of antibiotic prescribing. The primary outcome was total antibiotic prescriptions for these infections. Secondary outcomes were delayed prescriptions, prescriptions longer than 7 days, recommended antibiotic use, and outcomes for individual infections. Generalized estimating equations were used to estimate treatment effects, adjusting for clustering by clinic and baseline differences.
Results
There were 1682 encounters involving 54 primary care providers from January until May 31, 2019. In intervention clinics, the odds of any antibiotic prescription was reduced 22% (adjusted Odds Ratio (OR) = 0.78; 95% Confidence Interval (CI) = 0.64.0.96). The odds that a delay in filling a prescription was recommended was increased (adjusted OR=2.29; 95% CI=1.37, 3.83), while prescription durations greater than 7 days were reduced (adjusted OR=0.24; 95% CI=0.13, 0.43). Recommended antibiotic use was similar in control (85.4%) and intervention clinics (91.8%, p=0.37).
Conclusions
A community-based, primary care provider-focused antimicrobial stewardship intervention was associated with a reduced likelihood of antibiotic prescriptions for respiratory and urinary infections, an increase in delayed prescriptions, and reduced prescription durations.
Trial registration
clinicaltrials.gov (NCT03517215).
Similar content being viewed by others
Background
The need to more appropriately use antibiotics in order to limit antibiotic resistance has been widely endorsed [1, 2]. However, progress towards this goal has been slow. In Canada for example, antibiotic utilization has changed little, with 666 community antibiotic prescriptions dispensed per 1,000 persons in 2012 and 658 prescriptions in 2017 [3]. The recognition that 90% of antibiotic use occurs in the community has focused attention on primary care prescribers [4]. A 2019 U.S. study found 59% of outpatient antibiotic prescriptions are likely not needed [5]. Reducing this volume of unnecessary antibiotic use may be critical to limit antibiotic resistance. To achieve this, effective community antimicrobial stewardship (AMS) approaches are needed.
Community-based AMS programs have been tested in Scotland [6], Spain [7], the United States [8], the Netherlands [9], the United Kingdom [10], and Canada [11]. Most involved education and prescribing guidelines combined with audit-and-feedback [8,9,10,11]. Some were limited to either specific organisms [7], short durations [8], respiratory infections [9], effects were small [10], or evaluations lacked control groups, limiting conclusions about effectiveness [11, 12]. Some providers report a lack of confidence in AMS approaches, raising questions about whether community prescribers would implement programs, even where effective [13, 14]. To ensure AMS is relevant to community prescribers, programs may need to ensure they are addressing the prescribing challenges that community providers feel are most important.
One factor may be the clinical uncertainty community providers report in trying to distinguish viral from bacterial infections, owing to their similar clinical presentations [15]. There are also few point-of-care tests to aid in identifying bacterial presentations that might benefit from antibiotics. We previously developed a multi-faceted primary care provider-focused antimicrobial stewardship intervention that addressed clinical uncertainty through use of clinical decision aids, delayed prescriptions and safety netting advice [16]. A pilot evaluation identified competing clinical commitments, perceived pressure to prescribe antibiotics, and a lack of resources for stewardship activities as additional barriers for community clinicians [16]. The objective of this study was to assess the effectiveness of a community-based primary care provider-focused antimicrobial stewardship intervention addressing clinical uncertainty and other barriers on antibiotic prescription practices of primary care providers for common community infections.
Methods
Study setting and design
The University of Toronto Practice-based Research Network (UTOPIAN) consists of 14 family medicine clinics in south central Ontario affiliated with the Department of Family and Community Medicine of the University of Toronto. Two clinics had participated in a pilot study of the intervention and were excluded [16]. Of the remaining 12 clinics invited to participate, family physicians and nurse practitioners from six clinics agreed to participate in a pragmatic controlled trial of a primary care provider-focused stewardship intervention. The intervention was delivered between September 2018 and December 2018, followed by a 5 month evaluation period from January 1st 2019 until May 31st 2019. Baseline prescribing rates for each clinic were calculated from prescribing data for the previous winter. Ethics approval was obtained from research ethics boards of the University of Toronto, Mount Sinai Hospital, Women’s College Hospital and North York General Hospital. The study was registered with clinicaltrials.gov on 08/05/2018 (registration number NCT03517215).
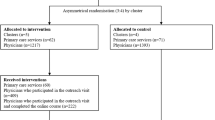
Randomization by minimization was conducted due to the small number of clinics [17]. Using prescribing data collected for the winter before the intervention, prescribing rates, number of providers and the presence of trainees were selected as minimizing factors. Clinics were assigned a number (by SV) and randomly assigned (by WM) without awareness of clinic identities. However, delays in securing participation from all clinics led to five being initially randomized, and a sixth clinic was later allocated to balance provider numbers. As a result, imbalances in factors associated with antibiotic use at baseline persisted. Statistical methods were therefore utilized to adjust for these factors in estimating the effect of the intervention.
Intervention
The intervention was a multi-faceted program of clinician education, clinical decision aids for prescribing decisions, patient information leaflets, audit and feedback of clinic prescription practices, local clinic support, and incentives. An initial one hour on-site education session was delivered by study staff at each clinic regarding antimicrobial resistance, stewardship, and interventions for reducing antibiotic prescribing. The clinic’s prescribing practices the previous winter were reviewed, and providers set prescribing goals. Providers were then sent electronic modules to complete over four months explaining the use of the decision aids for a given condition and optimal prescription practices. Additional on-site sessions were held during the winter to review antibiotic utilization and revise prescribing goals.
The modules addressed five infections: acute sinusitis, acute uncomplicated upper respiratory infections (URI), sore throat presentations (pharyngitis, tonsillitis), acute bronchitis and acute uncomplicated cystitis. These conditions account for approximately 50% of community antibiotic prescriptions in Canada [18]. Modules took approximately 15 minutes to complete and were sent each month by email to intervention clinics.
Module topics included prescribing issues for each infection and a 1-page clinical prescribing decision aid. The aid addressed criteria for diagnosis, indications for antibiotics, recommended first line antibiotic choices, treatment durations, and ‘red flags’ for serious presentations. Validated clinical decision rules were incorporated into prescribing aides where available [19, 20]. Modules also included ‘communication’ scripts to engage patients in prescribing decisions [21], patient handouts, delayed prescription options, [22] and advice to give patients about when to seek medical care where antibiotics were not prescribed (‘safety-netting’) [23].
Clinicians at intervention sites received $200 compensation, pro-rated for the number of completed modules and education sessions. Continuing medical education credits and a free antibiotic prescribing formulary [24] were also provided. Control arm participants provided usual care but received the free antibiotic formulary upon trial completion.
Data collection
Data from eligible visit encounters were abstracted from electronic medical record (EMR) systems at each clinic. Eligible visits were defined as those involving adults 18 years of age or older, seen by a consenting physician between January 1st 2018 and February 28th 2018 (baseline period) or between January 1st 2019 and May 31st 2019 (evaluation period), and with an eligible ICD-9 diagnosis code (International Classification of Diseases, Ninth Revision (ICD 9) identified from billing records. Urinary infections involving males or pregnant females were excluded, as were follow-up visits of previously treated infections.
To identify most eligible visits, a number of ICD-9 billing codes were selected. These included 460 (URI), 462 (pharyngitis), 463 (tonsillitis), 461(acute sinusitis), 466 (acute bronchitis), and (595) acute uncomplicated cystitis. In addition, visits coded 464 (laryngitis), 599 (other urinary-eg. hematuria, incontinence), 486 (pneumonia), and 487(influenza) were included to ensure other respiratory and urinary symptom visits had not been mislabeled. This was assessed by comparing a provider’s written diagnosis and the billing code. Two independent raters reviewed all visits using standardized coding rules developed for the study (Available upon request). The final visit diagnosis was adjusted if the written diagnosis indicated an eligible infection presentation. Non-infection diagnoses (e.g.’new patient visit’) and non-eligible infections (eg. pyleonephritis, chronic sinusitis) were excluded, as were presentations involving asthma or chronic lung disease. Raters agreed on the final diagnosis for 94% of visits. Disagreements were resolved through case review and agreement by both raters.
Data abstracted from each visit included patient age, sex, antibiotic allergies, clinic site, visit date, clinician type, billing ICD-9 code, clinician written diagnosis, selected vital signs, tests ordered, and antibiotic prescriptions. Prescription information included the antibiotic name, prescription duration, and if a patient was advised to delay filling the prescription (‘delayed prescription’).
Study outcomes
The primary study outcome was total antibiotic prescriptions for the five selected conditions combined (URI, sore throat presentations, acute sinusitis, acute bronchitis, acute uncomplicated cystitis) in each arm. Secondary outcomes were the proportion of prescriptions issued as delayed antibiotic prescriptions, prescriptions for longer than 7 days duration, and total, delayed and long duration prescriptions for each infection individually. A post-hoc decision was made to also assess test utilization.
Statistical analysis
A 25% relative reduction in the total prescriptions was selected as the minimum important effect size, consistent with previously reported national goals [25]. To detect a 25% relative difference with 90% power, assuming a similar 30% antibiotic prescribing rate as in the pilot study [26], a sample size of 834 cases in each study arm was estimated, unadjusted for clustering. Visit and clinic characteristics of each group were compared using unadjusted chi-square, Fisher’s exact test or t-tests as appropriate. The intervention effects were expressed as odds ratios, estimated from unadjusted and adjusted logistic generalized estimation equation (GEE) models that accounted for clustering by clinics in each study arm. Models were adjusted for differing baseline characteristics between control and intervention groups associated with antibiotic prescriptions, as well as baseline prescribing rates. All analyses were performed using R statistical software [27].
Results
There were 1,904 eligible visits from January 1, 2019 until May 31, 2019. After exclusions, 1682 (88.3%) visits were available for analysis; 943(56.1%) in control clinics and 739 (43.9%) from intervention clinics (Fig. 1). The average meeting attendance at intervention clinics was 81% with a 77% average education module completion rate. Overall, 16/34 (47.1%) of these providers completed all intervention elements.
Table 1 compares characteristics of intervention and control clinic visits in the prior winter and during the evaluation period. In both time periods, groups differed in the number of providers, total visits, and visits outside of regular clinic hours (after hours). Patients seen at intervention clinics during the evaluation tended to be older (mean 53.4 years) than at control clinics (47.1 years, p<0.001), more likely to be female (76.9% versus 70.6%, p=0.005), and have an antibiotic allergy (24.0% versus 16.1%, p<0.001). The distribution of infections differed between the groups in both time periods (p<0.001). While there were fewer cases of acute bronchitis at intervention clinics during the evaluation period (6.6%) compared to the baseline period (11.0%), there was no increase in pneumonia diagnoses to suggest diagnostic shifting (8.9% evaluation period vs 10.4% baseline).
Factors associated with receiving an antibiotic prescription (Supplementary Table 1) included the type of infection (p<0.01,), being assessed after hours (p=0.02), female gender (p<0.01), and age (p=0.07). These factors were adjusted for in comparisons of prescribing outcomes. Table 2 indicates the intervention effects on prescribing outcomes for the five selected infections combined (n=1,372 visits). There was an observed increase in the crude odds of receiving any antibiotic prescription at intervention clinics (crude odds ratio (OR)=1.72; 95% CI =1.00, 2.98). However, after adjustment for characteristics associated with antibiotic prescriptions, there was a 22% reduction in the odds of receiving an antibiotic prescription (adjusted OR = 0.78; 95% CI = 0.64, 0.96) at intervention clinics.
More prescriptions at intervention clinics were issued as delayed prescriptions (22.1%) than in control clinics (11.7%; adjusted OR = 2.29; 95% CI=1.37, 3.83). The odds that intervention physicians advised patients to start antibiotics immediately were reduced 37% compared to control clinics (adjusted OR= 0.63; 95% CI=0.45, 0.89). Antibiotic prescriptions for longer than 7 days duration were also decreased at interventions clinic (21.3%) compared to control clinics (29.3%; adjusted OR = 0.24; 95% CI = 0.13, 0.43). Use of recommended antibiotics were high in both control (84.9%) and intervention (92.2%) clinics (adjusted p=0.37).
There were no reductions in total antibiotic prescriptions for individual infections (Table 3). Prescriptions for URI cases were increased in intervention clinics (13.0% vs 7.7% control clinics, p<0.01), although most (56.5%) were delayed prescriptions. The odds of a delayed prescription was increased for acute sinusitis in unadjusted comparisons, and for acute cystitis in adjusted comparisons. The odds of a prescription for longer than 7 days was reduced for acute bronchitis only (adjusted OR = 0.46; 95% CI = 0.29, 0.73).
A post-hoc analysis of the effect of testing recommendations included in clinical decision aids found a throat swab or rapid strep test was ordered more frequently at intervention clinics (56/81, 69.1%) than control clinics (28/91, 30.8%) for sore throat presentations (adjusted OR = 4.63, 95% CI=2.81, 7.63). Chest x-rays were ordered more often at intervention clinics (19/49, 38.8%) than control clinics (13/126, 10.3%) for cases of acute bronchitis (adjusted OR = 3.85, 95% CI = 2.58, 5.76). Urinalysis and urine culture utilization was similar in both control (93.3%) and intervention (90.7%) clinics.
Discussion
This community-based, primary care provider-focused antimicrobial stewardship intervention reduced total antibiotic prescriptions to adults with a respiratory or urinary tract infection, increased the proportion issued as delayed prescriptions, and reduced prescription durations for longer than 7 days.
Although the observed crude rates of total antibiotic prescriptions were not different between intervention and control clinics, there were a number of differences in baseline characteristics between the two groups of clinics that persisted after randomization. When clinic difference were adjusted for, there was a 22% reduction in the odds of prescribing an antibiotic at intervention clinics. In addition, these prescriptions were twice as likely to be issued as delayed prescriptions. This is relevant as only 33% of prescriptions with instructions to delay starting may ultimately be filled [28]. As a result, patients seen at intervention clinics were less likely to be advised to begin antibiotics immediately. Prolonged antibiotic treatment durations are also an issue in primary care [29]. Long duration prescriptions were substantially reduced at intervention clinics. In addition, the change in test utilization at intervention clinics suggests the decision aids were important in affecting clinical change, as testing recommendations were only included in these aids.
Other multi-faceted ASP intervention studies have varied in the intervention focus, types of infections, and measures of antibiotic use [10, 30, 31]. A Quebec-based trial of shared decision making reported a 50% reduction in patient-reported intent to start antibiotics after a respiratory infection [30]. However, delayed prescriptions were allowed, which may have been later filled, and changes in total or dispensed antibiotics was not reported. A British trial of physician education, decision support and audit and feedback reported a 12% relative reduction in antibiotic prescriptions, but for respiratory infections only [31]. An evaluation of a national AMS program (TARGET) where practices were unaware they were part of a trial found a small 2.7% relative reduction in dispensed antibiotics [10]. These studies highlight the challenges of multi-faceted primary care AMS interventions, and the need to consider broader prescribing characteristics other than total prescriptions to fully understand the potential impact of primary care stewardship on antimicrobial resistance.
Providers were compensated for participating in the current study. An American study similarly provided compensation to participants with a 70% participation rate [32]. Incentives have also been implemented outside of studies to promote optimal antimicrobial use. In Britain, a financial Quality Premium introduced in 2015 for reductions in antibiotic use was associated with an 8% absolute decline in antibiotic prescriptions [33]. The current study also provided logistical support for AMS activities in intervention clinics. Other jurisdictions have similarly utilized direct supports to clinics [34, 35]. A Scottish national AMS program utilized Antimicrobial Management Teams to support local prescribing leadership [34]. In Britain, Medicine Management Teams play a role in education of community providers [35]. The current study and this research suggest the provision of incentives and logistical support at the clinic level may be important in facilitating community AMS efforts.
A limitation of the study was not all clinicians at each clinic participated. Participating clinicians may have been more receptive to the AMS intervention than might be seen in the broader primary care community. Another limitation was the short study duration over one winter season. Whether the impact on prescriptions would be sustained is unclear. AMS effects have declined when interventions are removed [36, 37]. The study also relied on written prescriptions as an outcome rather than dispensed antibiotics. While reducing initial prescriptions and their durations are important to reducing dispensed antibiotics, patients may have sought out other providers and received antibiotics. However, as more providers are exposed to AMS practices, patients may receive consistent antibiotic recommendations from all prescribers. Finally, the safety of this program was not assessed. Other studies have found adverse events associated with reduced antibiotic use in primary care are uncommon and require large samples to detect [38]. However, the elderly may be one group where caution is needed [39]. Clear ‘safety-netting advice’ where antibiotics are not prescribed, appropriate use of delayed prescriptions and clinical follow up can help mitigate such risks and prevent a loss of provider confidence in stewardship efforts.
Conclusion
This study has demonstrated that clinically important changes in antibiotic utilization in primary care clinics are possible with local stewardship efforts involving provider-focused education, clinical decision aids, clinic support, ongoing audit and feedback, and compensation for ASP activities. Structured and supported community-based antimicrobial stewardship efforts, similar to those in hospital settings, warrant further study.
Availability of data and materials
The data is available by contacting the principal author on reasonable request. Appropriate data transfer agreements with the participating institutions may be required.
References
The White House (US). National action plan for combating antibiotic-resistant bacteria. 2015 [Cited 2015 Mar 27]. Available from: https://www.cdc.gov/drugresistance/pdf/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf
Department of Health. Government Response to the Review on Antimicrobial Resistance. Department of Health: United Kingdom; 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/553471/Gov_response_AMR_Review.pdf
Public Health Agency of Canada. Canadian antimicrobial resistance surveillance system: Update 2018. Ottawa: Publications Canada; 2018.
Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core elements of outpatient antibiotic stewardship. MMWR. 2016;65(6):1–2. https://doi.org/10.2307/24904408.
Chua KP, Fischer MA, Linder JA. Appropriateness of outpatient antibiotic prescribing among privately insured US patients: ICD-10-CM cross-sectional study. BMJ. 2019;364:k5092.
Nathwani D, Sneddon J, Malcolm W, Wiuff C, Patton A, Hurding S, et al. Scottish antimicrobial prescribing group (SAPG): development of the Scottish national antimicrobial stewardship programme. Int J Antimicrob Agents. 2011;38(1):16–26.
Penalva G, Fernandez-Urrusuno R, Turmo JM, Hernandez-Soto R, Pajares I, Carrion L, et al. Long-term impact of an educational antimicrobial stewardship programme in primary care on infections caused by extended-spectrum β-lactamase-producing Escherichia coli in the community: an interrupted time series analysis. Lancet Infect Dis. 2020;20(2):199–207.
Shively NR, Buehrle DJ, Wagener MM, Clancy CJ, Decker BK. Improved antibiotic prescribing within a Veterans Affairs primary care system through a multifaceted intervention centered on peer comparison of overall antibiotic prescribing rates. Antimicrob Agents Chemother. 2020;64(1):e000928–19.
Van der Velden AW, Kuyvenhoven MM, Verheij TJM. Improving antibiotic prescribing quality by an intervention embedded in the primary care practice accreditation: the ARTI4 randomized trial. J Antimicrob Chemother. 2016;71(1):257–63.
McNulty C, Hawking M, Lecky D, Jones L, Owens R, Charlett A, et al. Effects of primary care antimicrobial stewardship outreach on antibiotic use by general practice staff: pragmatic randomized controlled trial of the TARGET antibiotics workshop. J Antimicrob Chemother. 2018;73(5):1423–32.
details.McKay RM, Vrbova L, Fuertes E, Chong M, David S, Dreher K, et al. Evaluation of the Do Bugs Need Drugs? program in British Columbia: can we curb antibiotic prescribing? Can J Infect Dis Med Microbiol. 2011;22(1):19–24.
Mamun A, Zhao B, McCabe M, Dreher K, Otterstatter M, Smith N, et al. Cost-benefit analysis of a population-based education program on the wise use of antibiotics. Can J Public Health. 2019;110(6):732–40.
Mauffrey V, Kivits J, Pulcini C, Boivin JM. Perceptions of acceptable antimicrobial stewardship strategies in outpatient settings. Medicine et maladies infectieuses. 2016;46:285–93.
Szymcsak JE, Feemster KA, Zaoutis TE, Gerber JS. Pediatrician perceptions of an outpatient antimicrobial stewardship intervention. Infect Control Hosp Epidemiol. 2014;35(S3):S69–78.
Hansen MP, Hoffman TC, McCullough AR, van Driel ML, Del Mar CB. Antibiotic resistance: what are the opportunities for primary care in alleviating the crisis? Front Public Health. 2015;3:35.
Jeffs L, McIsaac W, Zahradnik M, Senthinathan A, Dresser L, McIntyre M, et al. Barriers and facilitators to the uptake of an antimicrobial stewardship program in primary care: A qualitative study. PLoS One. 2020;15(3):e0223822.
Han B, Enas NH, McEntegart D. Randomization by minimization for unbalanced treatment allocation. Stat Med. 2009;28(27):3329–46.
Government of Canada. Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS) - Human Antimicrobial Use Report, 2012-2013. Guelph: Public Health Agency of Canada; 2014.
McIsaac WJ, Goel V, To T, Low DE. The validity of a sore throat score in family practice. CMAJ. 2000;163(7):811–5.
McIsaac WJ, Moineddin R, Gágyor I, Mazzulli T. External validation study of a clinical decision aid to reduce unnecessary antibiotic prescriptions in women with acute cystitis. BMC Fam Pract. 2017;18(1):89.
Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for C reactive protein and training in communication skills on antibiotic use in lower respiratory tract infections: cluster randomised trial. BMJ. 2009;338:b1374.
de la Poza AM, Dalmau GM, Bakedano MM, González AI, Criado YC, Anadón SH, et al. Prescription strategies in acute uncomplicated respiratory infections: a randomized clinical trial. JAMA Intern Med. 2016;176(1):21–9.
Jones D, Dunn L, Watt I, Macleod U. Safety netting for primary care: evidence from a literature review. BMJ. 2019;69(678):e70–9.
Anti-Infective Review Panel. Anti-infective guidelines for community-acquired infections. Toronto: MUMS Guideline Clearinghouse; 2013.
Health Canada. Controlling antimicrobial resistance. An integrated action plan for Canadians. Can Commun Dis Rep. 1997;23(Suppl 7):i–iv 1-32.
McIsaac WJ, Senthinathan A, Moineddin R, Nakamachi Y, Dresser L, McIntyre M, et al. Development and evaluation of a primary care antimicrobial stewardship program (PC-ASP) in Toronto, Ontario, Canada. JAMMI. 2021;6(1):32–48.
R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013.
Spurling GK, Del Mar CB, Dooley L, Foxlee R, Farley R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev. 2013;4:CD004417.
Pouwels KB, Hopkins S, Llewelyn MJ, Walker AS, McNulty CAM, Tobotham JV. Duration of antibiotic treatment duration for common infections in English primary care: cross-sectional and comparison with guidelines. BMJ. 2019;364:l440.
Légaré F, Labrecque M, Cauchon M, Castel J, Turcotte S, Grimshaw J. Training family physicians in shared decision-making to reduce the overuse of antibiotics in acute respiratory infections: a cluster randomized trial. CMAJ. 2012;184(13):E726–34.
Guillford MC, Prevost AT, Charlton J, Juszczyk SJ, McDermott L, et al. Effectiveness and safety of electronically delivered prescribing feedback and decision support on antibiotic use for respiratory illness in primary care: REDUCE cluster randomized trial. BMJ. 2019;364:l236.
Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA. 2016;315(6):562–70.
Balinskaite V, Johnson AP, Holmes A, Aylin P. The impact of a national antimicrobial stewardship program on antibiotic prescribing in primary care: an interrupted time series analysis. Clin Infect Dis. 2019;69(2):227–32.
Nathwani D, Sneddon J, Patton A, Malcolm W. Antimicrobial stewardship in Scotland: impact of a national programme. Antimicrob Resist Infect Control. 2012;1(1):1–3.
Allison R, Lecky DM, Beech E, Ashiru-Oredope D, Costelloe C, Owens R, et al. What resources do NHS Commissioning Organizations use to support antimicrobial stewardship in primary care in England? Antibiotics. 2020;9(4):158.
Little P, Stuart B, Francis N, Douglas E, Tonkin-Crine S, Anthierens S, et al. Antibiotic prescribing for acute respiratory infections 12 months after communication and CRP training: a randomized trial. Ann Fam Med. 2019;17(2):125–32.
Linder JA, Meeker D, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effects of behavioral interventions on inappropriate prescribing in primary care 12 months after stopping interventions. JAMA. 2017;318(14):1391–2.
Gulliford MC, Moore MV, Little P, Hay AD, Fox R, Prevost AT, et al. Safety of reduced antibiotic prescribing for self-limiting respiratory tract infections in primary care: cohort study using electronic health records. BMJ. 2016;354:i3410.
Gharbi M, Drysdale JH, Lishman H, Goudie R, Molokhia M, Johnson AP, et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: population based cohort study. BMJ. 2019;364:I525.
Acknowledgements
None additional
Funding
This work was supported by the Innovation Fund of the Alternative Funding Plan for the Academic Health Sciences Centres of Ontario. The funding body had no role in the design, data collection, analysis or interpretation.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by WM, with support from AM, NI, and YN. The intervention and study materials were designed by WM, SW. SK, SV, AB conducted data collection and entry, with contributions from BO, NI, RL, NT, MS, and RA. WM, SK, EH, LS participated in the formal analyses. WM, SK prepared the first draft of the manuscript. All authors participated in editing the final draft and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the research ethics boards of the University of Toronto, Mount Sinai Hospital, Women’s College Hospital and North York General Hospital. Written informed consent was obtained from all study participants as approved by the ethics committees. This research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1
. Associations between visit, patient, and condition characteristics, and having received an antibiotic prescription.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McIsaac, W., Kukan, S., Huszti, E. et al. A pragmatic randomized trial of a primary care antimicrobial stewardship intervention in Ontario, Canada. BMC Fam Pract 22, 185 (2021). https://doi.org/10.1186/s12875-021-01536-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12875-021-01536-3