Abstract
Background
Reliable evidence on the effectiveness of interventions to prevent diabetes-related foot ulceration is essential to inform clinical practice. Well-conducted systematic reviews that synthesise evidence from all relevant trials offer the most robust evidence for decision-making. We conducted an overview to assess the comprehensiveness and utility of the available secondary evidence as a reliable source of robust estimates of effect with the aim of informing a cost-effective care pathway using an economic model. Here we report the details of the overview. [PROSPERO Database (CRD42016052324)].
Methods
Medline (Ovid), Embase (Ovid), Epistomonikos, Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effectiveness (DARE), and the Health Technology Assessment Journals Library were searched to 17th May 2021, without restrictions, for systematic reviews of randomised controlled trials (RCTs) of preventive interventions in people with diabetes. The primary outcomes of interest were new primary or recurrent foot ulcers. Two reviewers independently extracted data and assessed the risk of bias in the included reviews.
Findings
The overview identified 30 systematic reviews of patient education, footwear and off-loading, complex and other interventions. Many are poorly reported and have fundamental methodological shortcomings associated with increased risk of bias. Most concerns relate to vague inclusion criteria (60%), weak search or selection strategies (70%) and quality appraisal methods (53%) and inexpert conduct and interpretation of quantitative and narrative evidence syntheses (57%). The 30 reviews have collectively assessed 26 largely poor-quality RCTs with substantial overlap.
Interpretation
The majority of these systematic reviews of the effectiveness of interventions to prevent diabetic foot ulceration are at high risk of bias and fail to provide reliable evidence for decision-making. Adherence to the core principles of conducting and reporting systematic reviews is needed to improve the reliability of the evidence generated to inform clinical practice.
Similar content being viewed by others
Background
Diabetes mellitus is a major global public health problem. In 2019, 463 million adults around the world were living with diabetes and projections predict an increase in prevalence to 578 million by 2030 and 700 million by 2045 [1]. In the UK alone it is estimated that 5 million people will have diabetes by 2030 [2]. People with diabetes are more at risk of developing foot problems with those affected experiencing higher rates of foot ulceration, lower-limb amputation and premature death [3, 4]. The healthcare costs of diabetic foot ulcers and amputations to the NHS in England has been estimated at between £837 and £962 million, almost 1% of the NHS budget, with more than 90% of that expenditure related to ulceration [3].
Reliable evidence on the clinical effectiveness of preventive interventions is imperative to design effective care pathways that can reduce the risk of foot ulceration and its adverse consequences for people with diabetes and the associated healthcare costs. As part of a wider research project to develop an evidence-based care pathway we sought to obtain numerical estimates of effect from randomised controlled trials (RCTs) of interventions to prevent diabetic foot ulceration as RCTs have the advantage over other study designs when evaluating interventions because only a randomly allocated control group comparison can prevent systematic differences at baseline influencing the results and support reliable claims about cause and effect [5, 6].
Systematic review methods are widely used to summarise the evidence generated by multiple individual primary studies of alternative interventions to support decision-making and inform clinical practice, guidelines and health policy [6, 7]. Well-conducted systematic reviews based on explicit methods that identify, appraise and summarise the findings from all relevant primary studies of the same and alternative interventions can determine which results are sufficiently reliable to inform practice and provide more accurate estimates of effect than individual studies alone. It is however becoming increasingly common to find multiple systematic reviews in the published literature that address the same clinical questions [8, 9]. In this situation an overview can provide a comprehensive summary of the evidence base and reduce the research duplication and waste that is generated by conducting unnecessary additional reviews [10, 11]. Overviews have a similar structure and methodology to systematic reviews but include reviews rather than primary studies [12].
Several published systematic reviews of preventative interventions for foot ulceration in diabetes are known to exist, some of which reach conflicting conclusions [13, 14]. We conducted an overview to assess the comprehensiveness and utility of the available secondary evidence as a reliable source of robust estimates of effect with the aim of informing a cost-effective care pathway using an economic model, based on numerical data [5]. Although we identified 19 systematic reviews (one of which had been updated) limitations in scope, overlap and quality meant we had to undertake an additional systematic review in order to make the best possible use of the available data [14]. The purpose of this overview is to update the original searches for eligible reports and to consider the quality and reliability of systematic reviews of preventative interventions for foot ulceration in diabetes.
The overview protocol was registered on the PROSPERO Database (registration number: CRD42016052324).
Methods
The literature search, selection and appraisal methods are summarised here and reported in detail elsewhere [5].
Search strategy
A librarian (MS) developed strategies to identify systematic reviews in Medline OVID and Embase OVID (initially from inception to December 2019 then re-run to update the searches until 17th May 2021) without restrictions. The first searches were de duplicated using RefWorks. The electronic search strategies were informed by the strategies reported elsewhere [11] and include methodological search terms (see Additional file 1: supplementary files). The Cochrane Database of Systematic Reviews (CDSR), the Database of Abstracts of Reviews of Effectiveness (DARE), and the Health Technology Assessment (HTA) Journals Library and (for the update search only, Epistomonikos) were also searched. Systematic reviews in progress were identified via PROSPERO (https://www.crd.york.ac.uk/prospero/) and checked for subsequent completion or publication. Reference lists in all eligible reviews were browsed for additional relevant reviews. Additional data and clarifications about their reviews were sought from review authors.
Eligibility criteria
Systematic reviews of RCTs of interventions to prevent foot ulceration in people with type 1 or type 2 diabetes whether at high, medium, or low risk, with or without a history of foot ulceration but no existing foot ulcers at baseline were eligible for inclusion. The outcomes of interest were incident primary or recurrent foot ulcers and Lower Extremity Amputations (LEA) derived from RCTs comparing single-component or complex interventions (comprising several interacting components provided together) with standard care or alternative interventions. We excluded reviews of surgical procedures. Systematic reviews that included RCTs and other study designs were eligible for inclusion but only data from the relevant RCTs was used for the purpose of the overview.
Selection and data extraction
One reviewer (DJN or FC) screened all titles and abstracts to identify potentially relevant reviews with a second reviewer (FC or HMc) screening a 10% random sample to minimise the risk of errors of judgement. Reviewers working in pairs (DJN, AEA, FC or HMc) independently assessed the selected full text articles for eligibility and resolved disagreements in discussion with a third reviewer. Reviewers (DJN, AEA, FC or HMc) independently extracted data from the included reviews using a bespoke data extraction tool and resolved disagreements through discussion.
Quality assessment
Reviewers working in pairs (DJN, AEA, FC or HMc) independently assessed the risk of bias in the included reviews using the Risk of Bias in Systematic Reviews (ROBIS) tool and reached agreement by discussion [12]. Concerns with the process of reviews are assessed using 4 domains; (i) study eligibility criteria, (ii) the identification and selection of studies, (iii) data collection and study appraisal and (iv) synthesis and findings.
Results
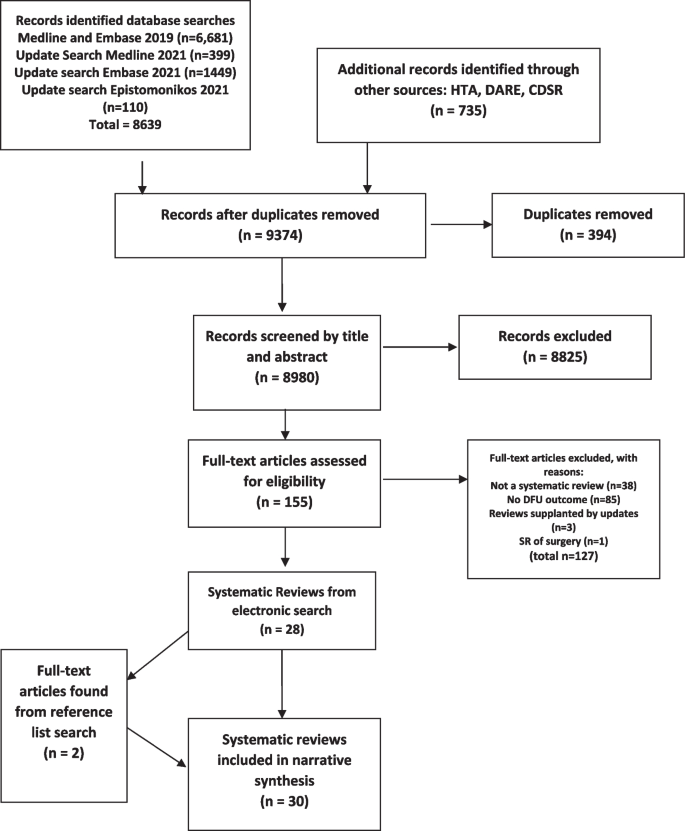
A diagram showing the flow of information through the process of identifying and selecting reviews for inclusion in the overview is presented in Fig. 1.
Included reviews
Thirty-two reviews met the criteria for inclusion in the overview [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. Two were updates of previously published reviews and the earlier versions were excluded to avoid the double-counting of data [31, 33]. Of the 30 reviews, 14 included only RCTs [13,14,15,16,17,18,19,20,21,22,23,24,25,26] and 16 included RCTs together with various other study designs [27,28,29,30, 32, 34,35,36,37,38,39,40,41,42,43,44]. The reviews were published between 1998 and 2021 in professional or scientific journals, four in the Cochrane Library, one was published in the UK National Institute of Health Research (NIHR) Health Technology Assessment (HTA) journals library and one for the Agency for Healthcare Research and Quality (AHRQ), USA [15, 16, 19, 20, 24, 41]. Other key characteristics of the included reviews are summarised in Table 1.
Overall, the 30 reviews included a total of 26 RCTs relevant to the overview (See Additional file 2: Supplementary references S1–S26). The majority of the RCTs were included in more than one review, only three being included only once (see Additional file 2: Supplementary references S16, S18, S20).
Risk of bias
The ROBIS assessment results are summarised in Table 2. Six were judged to have a low risk of bias in all four domains assessed using the ROBIS tool [15, 16, 19, 20, 23, 24]. Nineteen reviews (65%) were judged to be at high risk of bias [13, 17, 18, 21, 22, 27,28,29, 32, 34,35,36,37,38,39,40, 42,43,44]. The most common reasons for concern about bias in the reviews related to the lack of clarity in eligibility criteria specification (60%) [13, 17, 18, 21, 22, 27,28,29, 35,36,37,38,39,40,41,42,43,44] methods used to identify and select eligible studies (70%) [13, 14, 17, 18, 21, 22, 25, 26, 28, 29, 32, 34,35,36,37,38, 40,41,42,43,44] data collection and study appraisal (53%) [13, 17, 18, 21, 22, 27,28,29,30, 32, 34, 36,37,38, 42, 43] and the synthesis and findings (57%) [13, 17, 18, 21, 22, 25, 28, 29, 32, 35, 37,38,39,40, 42,43,44]. Only nine of the 26 non-Cochrane reviews reported the registration or existence of a review protocol [14, 19, 23, 24, 28, 30, 32, 39, 41]. The reviews used a variety of tools to assess the validity and risk of bias in trials with the Cochrane risk of bias tool being the most frequently used [6, 13,14,15,16,17,18, 20, 23,24,25,26, 29, 32, 41, 42]. Other assessment tools were, the JBL, [28, 39, 40, 45] reporting recommendations for trials of interventions for the foot in diabetes [27, 30, 46] PEDro [44, 47], the source of the risk of bias tool not reported [19, 22] QUADAS and other assessments for diagnostic tests [34, 37, 48, 49] Downs and Black [35, 50], McMaster Critical Review Form [38, 51]. Quality assessment not reported in two reviews [21, 43] preventative services veterans task force [36, 52].
Fifteen of the 26 non-Cochrane reviews either did not provide any information about sources of funding or declared none [17, 18, 22, 26,27,28,29,30, 32, 35, 37,38,39, 42, 43].
Evidence of effectiveness of preventive interventions
Patient education
Evidence was available from four systematic reviews of patient education interventions that included four RCTs relevant to the overview [13, 15, 17, 29]. The risk of bias in the Cochrane review was judged to be low [15] while three non-Cochrane reviews were considered to be at high risk of bias [13, 17, 29].
The Cochrane review [15] published in 2014 identified two RCTs which excluded people with foot ulcers at baseline (Additional file 2: Supplementary references S1, S2). These RCTs compared intensive foot care education programmes with brief educational interventions in people at high risk of ulceration and reported contradictory results. Clinical heterogeneity precluded meta-analysis in the review as a whole which concluded there was insufficient robust evidence that patient education was effective in preventing foot ulcers.
A review comparing intensive with routine patient education published in 2013 [17] pooled the results from the same two RCTs (Additional file 2: Supplementary references S1, S2) included in the Cochrane review with results from five other trials. The meta-analysis showed a lower incidence of foot ulceration in favour of intensive education but the pooled effect estimate is unlikely to be reliable because it combined results from trials involving people with and without existing foot ulcers [53] (Additional file 2: Supplementary references S1, S2), and the authors concede some trials did not provide details of the randomisation procedure and selection bias is possible.
A subsequent review and meta-analysis [13] included six RCTs of which three met the criteria for the overview: one (Additional file 2: Supplementary reference S24) included in the Cochrane review, one (Additional file 2: Supplementary reference S3) published after completion of the Cochrane review, and interim findings from a trial (Additional file 2: Supplementary reference S4) that the Cochrane review classified as awaiting final results. One of the RCTs (Additional file 2: Supplementary reference S1) included in the previous reviews was omitted. This review was rated high for risk of bias with particular concerns about the synthesis of findings casting doubt on the reliability of the results. Meta-analysis of ulcer incidence data pooled results from trials in people with and without existing foot ulcers and failed to take account of the risk of bias in the primary studies and inconsistency in their results (I2 = 92%). The review’s positive conclusion, that intensive educational intervention reduced the incidence of foot ulcers compared with brief educational intervention, was based on a single meta-analysis which was interpreted as being statistically significant (p = 0.05). This review also pooled LEA data from dissimilar trials as reported in the earlier review by He et al. [17].
A review that intended to include only RCTs to assess the effectiveness of health education programmes to improve foot self-care and reduce foot problems in older people with diabetes expanded its scope to include non-randomised studies due to ‘the dearth of information’ identified [29]. The review method raised concerns about its ability to identify relevant studies. Ultimately it included 14 studies of various types and the only RCT (Additional file 2: Supplementary reference S2) was included in the earlier reviews we identified.
Systematic reviews that addressed the question of the effectiveness of a broad range of preventive interventions provided no additional evidence on the effectiveness of patient education from RCTs relevant to the overview. The most recent of these, an update of a previous review, undertaken to inform International Working Group on the Diabetic Foot (IWGDF) guidance on the prevention of foot ulcers in at-risk patients [30, 31] considered evidence from four RCTs (Additional file 2: Supplementary references S2, S3, S4, S14) alongside results from non-controlled studies. Conclusions were informed by a system for grading evidence-based guidelines [46] and reached by consensus. The reviews of assorted preventative interventions which included RCTs of patient education either included or pre-dated the patient education RCTs already described and identified no others [14, 18, 19, 21, 22, 25, 30, 41].
Overall these systematic reviews all found that there is inadequate evidence upon which to base recommendations about patient education to prevent foot ulceration in diabetes, [13, 15, 17, 29] except one which concluded that patient education is effective in preventing foot ulcers [13].
Reviews of psychosocial interventions
Three reviews assessed the evidence for psychosocial interventions to prevent foot ulcers [23, 24, 27], two of which were judged to be at low risk of bias [23, 24].
One published in the Cochrane library [24] and included a single RCT of home monitoring of foot skin temperature which included theory-based counselling for people whose foot skin temperature was raised (Additional file 2: Supplementary reference S25). A second review of psychosocial interventions included six RCTs relevant to our overview, all of which had previously been reviewed by others mostly within reviews of educational interventions [23].
A review of the effect of motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration was judged to be at high risk of bias [27]. The only RCT data included were the interim findings from the trial (Additional file 2: Supplementary reference S4) previously included in the review of educational interventions by Adiewere et al. [13].
These reviews all concluded there was a lack of evidence of effectiveness for psychosocial interventions or motivational interviewing and the authors of one suggested randomised controlled trials of theoretically informed interventions to assess clinical outcomes are required [23].
Footwear and off-loading
Eight reviews [20, 28, 32, 34,35,36, 38, 40] aimed to evaluate footwear and/or offloading interventions and a further eight reviews of assorted interventions included footwear and offloading [14, 18, 19, 21, 22, 25, 30, 41], collectively identified nine RCTs relevant to the overview (Additional file 2: Supplementary references S5–S10, S16, S18, S19). Only two reviews were judged to be at low risk of bias [19, 20] and ten others were considered to be at high risk [18, 21, 22, 28, 32, 34,35,36, 38, 40].
A Cochrane review published in 2000 [20] identified one quasi-randomised trial, in which patients were allocated alternately, not randomly, showed a significant reduction in recurrent ulceration with therapeutic shoes compared with standard footwear (Additional file 2: Supplementary reference S5).
Two subsequent reviews of the effectiveness of therapeutic footwear for preventing re-ulceration [34, 36] restricted inclusion of studies to those published in English, included one additional RCT (Additional file 2: Supplementary reference S6) and other study designs. The authors concluded that the evidence to support footwear interventions to prevent re-ulceration is conflicting because non-randomised and observational studies reported positive results while the RCT showed no benefit.
The quasi-randomised trial (Additional file 2: Supplementary reference S5) was the only study with an outcome relevant to the overview that was included in a review of the effectiveness of insoles for the prevention of ulcer recurrence [35]. This review considered evidence from mixed study designs which did not support its overly positive conclusions.
A review that focussed on the effectiveness of off-loading interventions to prevent primary (first) diabetic foot ulcers was restricted to studies published in English and failed to identify any relevant RCTs with ulceration as an outcome [28].
A review [32] (updating a previous version [33]) to inform IWGDF guidance on footwear and off-loading interventions to prevent and heal diabetic foot ulcers included five additional RCTs (Additional file 2: Supplementary references S7–S11). This review considered the findings from the RCTs (including the quasi-randomised trial) alongside results from cohort studies. The authors conclude that the evidence supporting the use of specific footwear interventions to prevent recurrent plantar ulcers is quite strong and that sufficient good quality evidence supports the use of therapeutic footwear with demonstrated pressure relief to prevent plantar ulcer recurrence [32]. This finding appeared to be based on the results from a subgroup analysis within a single RCT (Additional file 2: Supplementary reference S7).
A review of the effects of footwear and insoles published in 2020 [38] identified five RCTs, only one of which had not been included in a review previously (Additional file 2: Supplementary reference S19). The RCT (n = 51) compared ridged with semi ridged rocker soles in people at high risk of foot ulceration and found a statistically significantly reduction in ulcers in those allocated to the ridged rocker sole. The review concluded there was limited evidence to inform the use of footwear and insoles to prevent foot ulceration. A more recent review [40] included one RCT evaluating the use of a mobile phone to alert patients of increased foot pressures which was out with the search dates of all other systematic reviews (Additional file 2: Supplementary reference S18). The proof of concept trial allocated 90 patients who were at high risk of foot ulceration to an insole system where either audio-visual alerts via a smartwatch and offloading instructions were sent to the patients’ phones when increased pressures were detected or, in the control group, no alerts were sent. The trial had a large loss to follow up (36%) and no statistically significant difference in the number of ulcerations was observed but time to event analyses found the intervention group were ulcer-free for longer. The review concludes there was difficulty in singling out the most effective weight-redistributing preventative features in shoes and insoles but concluded that this type of intervention appears to be effective.
Eight other reviews of assorted preventative interventions were identified and again either included or pre-dated RCTs of footwear and/or offloading already described and identified no others [14, 18, 19, 21, 22, 25, 30, 41]. Meta-analyses of RCT data were presented in two of the more recent reviews [14, 25]. These suggest that footwear and insoles can reduce foot ulceration but further research to examine the most effective features of footwear and insoles and their effect in people with different risk profiles is merited.
Complex interventions
We classified three systematic reviews of the effectiveness of interventions as complex [16, 37, 39]. One review was judged to be at low risk of bias [16], two others being judged to be at high risk. There were eight reviews of assorted interventions [14, 18, 19, 21, 22, 25, 30, 41] which included integrated foot care or complex interventions, and collectively all reviews included six RCTs relevant to the overview (Additional file 2: Supplementary references S1, S13–S16, S24).
A Cochrane review published in 2015 which assessed complex interventions defined as combinations of preventive strategies identified three RCTs relevant to the overview [16]. One RCT of an education-focused intervention in low to medium-risk patients (Additional file 2: Supplementary reference S12) reported a reduction in the incidence of foot ulceration compared with usual care but may not be reliable because the cluster-randomisation design was reportedly not accounted for in the analysis. One of two RCTs that compared more intensive and comprehensive complex interventions with usual care in high-risk patients showed no difference in the incidence of foot ulceration but a significant reduction in LEA (Additional file 2: Supplementary reference S13) whereas the other trial reported the opposite (Additional file 2: Supplementary reference S14). This review judged all three RCTs at high risk of bias and the pooling of data in a meta-analysis inappropriate due to marked heterogeneity. Overall, it concluded there was insufficient evidence to support the effectiveness of complex interventions.
A review of monofilament and other threshold tests for preventing foot ulceration was judged at high risk of bias across all 4 ROBIS domains and included only one RCT evaluating the prevention of foot ulceration and amputation in people with diabetes which was also included in the Cochrane review (Additional file 2: Supplementary reference S13) [37]. The review produced overly positive conclusions about the value of screening in preventing of foot ulcers and amputations given the trial found no statistically significant difference in the incidence of foot ulcers in the two groups [37].
The same trial was excluded from a review to inform IWGDF guidance on the prevention of foot ulcers in at-risk patients because of concerns about the comparability of the intervention and control groups [30].
The review undertaken to inform IWGDF guidance included studies of integrated foot care, defined as care given by one or multiple collaborating professionals treating patients on multiple occasions with multiple interventions [30]. It excluded the trial by McCabe et al. (Additional file 2: Supplementary reference S13) but included an RCT of chiropodist care (Additional file 2: Supplementary reference S15), (which was classified in other reviews as patient education) as well as unpublished data from an additional RCT of podiatric care (Additional file 2: Supplementary reference S16) which contributed to the assessment alongside data from non-controlled studies. No conclusion could be drawn about first ulcer prevention, and the suggestion that integrated foot care may be beneficial in preventing recurrent ulceration was largely based on the results from uncontrolled studies.
A systematic review of the effect of contact with a podiatrist, working within a team, on the incidence of foot ulceration did not identify any RCTs which met its own eligibility criteria [39].
The eight reviews of assorted interventions, details of which are presented below, identified no additional trials of complex interventions [14, 18, 19, 21, 22, 25, 31, 41].
Reviews of telehealth interventions and foot temperature monitoring
The overview identified two systematic reviews evaluating telehealth interventions to prevent foot ulceration [42, 43]. Both reviews were judged to be at high risk of bias across all 4 ROBIS domains but only one included any RCTs. The review by Hazenberg et al. [42] analysed data from 4 RCTs of home-monitoring of foot skin temperature and presented a meta-analysis showing a reduction in the number of foot ulcers when abnormal temperatures were recorded and patients’ avoided weight-bearing until their foot temperature lowered (Additional file 2: Supplementary references S21–S23, S25). These same 4 RCTs were pooled by Ena et al. [26] in a review of temperature monitoring and were also included in three systematic reviews of assorted interventions [14, 25, 30].
The two reviews conclude that further research is required, [42, 43] one also acknowledge the limitations in the studies and that a larger evidence base is required before this technology could be widely implemented in practice [42]. However, the review by Ena et al. concludes that daily measurement of skin temperature when measured using a handheld infrared thermometer reduces the appearance of new foot ulcers and notes the risk of bias in the same 4 RCTs is low (Additional file 2: Supplementary references S21–S23, S25) [26]. The three reviews of assorted interventions all concluded that the available data suggest this intervention may prevent foot ulcers developing [14, 25, 30] but two noted the need for further evaluation and the possibility that the intervention might not be feasible in real world settings [14, 25].
Reviews of physical activity
We found one systematic review of physical activity which we judged to be at high risk of bias in its evaluation of the effect of exercise of the prevention of foot ulceration [44]. It included one RCT in which foot ulceration was an outcome (Additional file 2: Supplementary reference S24). The reviewers’ conclusion that exercise can delay the development of foot ulcers is not supported by the trial results (Additional file 2: Supplementary reference S24). The RCT was also included in three separate systematic reviews of assorted interventions [14, 30, 41].
Reviews of assorted preventative interventions
Eight systematic reviews included a variety of interventions to prevent foot ulcers [14, 18, 19, 21, 22, 25, 30, 41] only one was judged to be at low risk of bias [19]. Four were judged to have an unclear risk of bias because of approaches they took to the selection of studies or the analysis [14, 25, 30, 41] and three were judged at high risk of bias [18, 21, 22].
Collectively they assessed the evidence from 26 RCTs, 2 of which were not included in intervention-specific reviews presented above. Two reviews included a trial of elastic compression stockings as a preventive intervention [14, 19]. The incidence of foot ulcers in people randomised to elastic compression stockings compared with those who did not receive hosiery was not found to be statistically significantly different. The trial population was at high risk of foot ulceration (Additional file 2: Supplementary reference S26).
Three reviews [14, 31, 41] included one RCT of patient instruction to apply antifungal nail lacquer as a way to increase the frequency of foot self-inspection but found no difference in the incidence of first or recurrent ulcers when compared with standard care (Additional file 2: Supplementary reference S17).
Discussion
Systematic reviews are widely regarded as the cornerstone of evidence-based healthcare. Harnessing that evidence has become increasingly challenging as the prevalence of systematic reviews in the biomedical literature continues to increase with one recent estimate suggesting a publication rate of more than 8000 per year [9]. It is therefore unsurprising that we identified 30 systematic reviews of interventions to prevent diabetic foot ulceration that met the criteria for inclusion in our overview, with one-third having been published in the last 5 years. Yet, this surfeit of systematic reviews does not provide a wholly reliable source of evidence for decision-making.
The ability of an overview to provide useful decision-support is reliant on the quality of the conduct and reporting of the systematic reviews available. As stated, our original purpose was to conduct an overview of reviews to obtain numerical summaries of the effects of preventative interventions for foot ulcers in diabetes to populate an economic model, but two-thirds of the reviews we included had methodological shortcomings associated with a high risk of bias and reliable meta-analyses of trial data were first published in 2020 [14, 25].
Those reviews without protocols made it difficult to ascertain whether the reviews’ methods were pre-defined, adhered to or decided or modified during the review process. The absence of pre specified primary study inclusion criteria in a third of the reviews also made it hard to judge whether reviewers’ decisions about including studies during the conduct of the reviews could have introduced bias. The evident inadequate development of search strategies may suggest a lack of familiarity with the principles of searching electronic databases and working with an information specialist who possesses the skills to construct and implement robust search strategies. Searches were frequently compromised by involving few sources, limited search terms and unjustified restrictions. Only around half of the reviews searched without language restrictions and few searched sources of unpublished data. More than half of the reviews included various study designs as well as RCTs but few considered the influence that study design could have on the results.
The conduct of evidence synthesis was another common cause for concern about bias in most of the reviews we identified. Quantitative synthesis of RCT data was performed in only five of the reviews but we found problems with meta-analyses that included data from patients who did not meet predefined eligibility criteria, errors in the interpretation of meta-analytical statistics and failure to explore reasons for heterogeneity. Narrative approaches largely entailed study-by-study narrative summaries which may indicate a lack of awareness or expertise in methods for the conduct of narrative synthesis in systematic reviews. Whatever the approach used, interpretation of the findings often ignored or glossed over the potential for bias in the included studies and other important between-study differences. The upshot of this is seen in overly positive conclusions that are not supported by the evidence reviewed.
Guidance for conducting overviews is accumulating but challenges remain [54] and some limitations to our overview warrant consideration. We could have missed some relevant systematic reviews by not searching a wider range of sources but, finding more reviews is unlikely to have altered our concern about the reliability of the evidence base as a whole. We may also have failed to find reviews including RCTs of other relevant interventions. We used ROBIS [12] to appraise the quality of the included systematic reviews but found that using this validated tool often relied on subjective judgment, especially in the absence of review protocols, resulting in lengthy deliberations to resolve disagreements. Research published by others has shown inadequate inter-rater reliability among professional reviewers using ROBIS [55] and we concur that the tool and guidance need revision to improve its reliability and utility. We suggest that reviewers who intend to use ROBIS to assess the risk of bias in systematic reviews clarify and agree the reasons for allocating specific ratings during the development of the protocol and again periodically during the conduct of the overview.
In any overview of multiple systematic reviews evaluating alternative intervention options some overlap in the included primary studies is to be expected and has to be assessed to avoid introducing bias [56, 57]. This overview revealed how substantial the overlapping nature of the evidence from systematic reviews of RCTs addressing diabetic foot ulcer prevention is and crucially, the same (largely poor-quality) trials being reviewed over and over again without our understanding about what works to improve patient outcomes becoming any clearer [14].
The predominance of low-quality trials that are subsequently included in systematic reviews without due consideration is a concern for journal editors as it undermines confidence in systematic reviews to reliably inform clinical practice [58]. From the overview it appears some editors do not share those concerns and may not even be aware of the methodological flaws in the systematic reviews their journals have published. This is at odds with the endorsement of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [59] by most of those journals in their instructions to authors and is also hard to reconcile with a robust peer review process. These systematic reviews were published over two decades, but we saw little improvement in the quality of conduct and reporting over time. This mirrors the pattern observed more widely in the biomedical literature by researchers who have recommended certified training for journal editors in how to implement PRISMA and facilitate its use by peer reviewers as one way to improve the value of systematic reviews [9]. The same challenges might also exist for the recent reporting guidelines for literature searches in systematic reviews, PRISMA-S, despite the clear intention to improve the reproducibility of searches in reviews [60].
Practitioners involved in developing international guidelines on the prevention of diabetic foot ulcers recognise the need to improve the quality of the intervention studies that are conducted and submitted for publication [46]. They have drawn attention to the omission of core details from many trial reports that hinders appraisal of study quality and clinical relevance in systematic reviews. This has implications for relying on overviews to understand the evidence base if it is not possible to tell from systematic review reports whether missing details were absent from the included trial reports or overlooked by the reviewers. The proposed reporting standards checklist for studies on the management and prevention of foot ulcers in diabetes should inform the conduct of systematic reviews as well primary studies alongside PRISMA and CONSORT (Consolidated Standards of Reporting Trials) [59, 61] to improve the quality of published research in this area. Other researchers engaged in synthesizing evidence of health technologies for clinical conditions other than the foot in diabetes may also find condition-specific reporting standards helpful when undertaking an assessment of relevant literature.
Using evidence from unreliable systematic reviews to inform clinical practice has obvious negative consequences including invalid clinical guidelines recommendations which could result in the provision of suboptimal care that will not lead to improved outcomes for patients. There is already evidence that the number of overviews of systematic reviews of healthcare interventions is rising and their quality is variable [62]. Given the abundance of systematic reviews summarising poor-quality trials of interventions to prevent diabetic foot ulcers, it may only be a matter of time before uncritical overviews also start to proliferate. Those who conduct, fund, peer review and publish research in this area have a joint responsibility to ensure that the evidence base does not serve the interests of researchers and publishers rather than improving outcomes for people living with diabetes.
Availability of data and materials
All data generated or analysed during the current study are included in this published article and its supplementary information files.
References
International Diabetes Federation. IDF diabetes atlas. 9th ed. Brussels; 2019. Available from: https://www.diabetesatlas.org. Cited 2020 Nov 1
Diabetes UK. Facts and figures. Available from: https://www.diabetes.org.uk/professionals/position-statements-reports/statistics. Cited 2020 Nov 1.
Kerr M, Barron E, Chadwick P, Evans T, Kong WM, Rayman G, et al. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet Med. 2019;36(8):995–1002.
Saluja S, Anderson SG, Hambleton I, Shoo H, Livingston M, Jude EB, et al. Foot ulceration and its association with mortality in diabetes mellitus: a meta-analysis. Diabet Med. 2020;37(2):211–8.
Crawford F, Chappell FM, Lewsey J, Riley R, Hawkins N, Nicolson DJ, et al. Risk assessments and structured care interventions for prevention of foot ulceration in diabetes: development and validation of a prognostic model. Health Technol Assess. 2020;24(62):1.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester: Wiley; 2019.
Systematic Reviews. CRD’s guidance for undertaking reviews in health care: Centre for Reviews and Dissemmination, University of York; 2009. Available from: https://www.york.ac.uk/crd/guidance/
Moher D. The problem of duplicate systematic reviews. BMJ. 2013;347:f5040.
Page MJ, Shamseer L, Altman DG, Tetzlaff J, Sampson M, Tricco AC, et al. Epidemiology and reporting characteristics of systematic reviews of biomedical research: a cross-sectional study. PLoS Med. 2016;13(5):e1002028.
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15.
Wu L, Norman G, Dumville JC, O’Meara S, Bell-Syer SE. Dressings for treating foot ulcers in people with diabetes: an overview of systematic reviews. Cochrane Database Syst Rev. 2015;(7) Available from: http://doi.wiley.com/10.1002/14651858.CD010471.pub2.
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Adiewere P, Gillis R, Imran Jiwani S, Meal A, Shaw L, Adams GG. A systematic review and meta-analysis of patient education in preventing and reducing the incidence or recurrence of adult diabetes foot ulcers (DFU). Heliyon. 2018;4(5):e00614.
Crawford F, Nicolson DJ, Amanna AE, Martin A, Gupta S, Leese GP, et al. Preventing foot ulceration in diabetes: systematic review and meta-analyses of RCT data. Diabetologia. 2020;63(1):49–64.
Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2014;(12) Available from: http://doi.wiley.com/10.1002/14651858.CD001488.pub5.
Hoogeveen RC, Dorresteijn JA, Kriegsman DM, Valk GD. Complex interventions for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2015;(8) Available from: http://doi.wiley.com/10.1002/14651858.CD007610.pub3.
He J, Zhang L, Liu L, Zhu Y. Intensive versus routine education on diabetes mellitus for prevention of diabetic foot ulcer: a systematic review [Chinese]. Chinese J Evidence-Based Med. 2013;13(12):1470–4.
Arad Y, Fonseca V, Peters A, Vinik A. Beyond the monofilament for the insensate diabetic foot. A systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes. Diabetes Care. 2011;34(4):1041–6.
O’Meara S, Cullum N, Majid M, Sheldon T. Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration. Health Technol Assess. 2000;4(21):1–237.
Spencer SA. Pressure relieving interventions for preventing and treating diabetic foot ulcers. Cochrane Database Syst Rev. 2000;(3) Available from: http://doi.wiley.com/10.1002/14651858.CD002302.
Mason J, O’Keeffe C, McIntosh A, Hutchinson A, Booth A, Young RJ. A systematic review of foot ulcer in patients with type 2 diabetes mellitus. I: prevention. Diabet Med. 1999;16(10):801–12.
Kaltenthaler E, Morrell CJ, Booth A, Akehurst RL. The prevention and treatment of diabetic foot ulcers: a review of clinical effectiveness studies. J Clin Eff. 1998;3(3):99–104.
Norman G, Westby MJ, Vedhara K, Game F, Cullum NA. Effectiveness of psychosocial interventions for the prevention and treatment of foot ulcers in people with diabetes: a systematic review. Diabet Med. 2020;37:1256–65.
McGloin H, Devane D, McIntosh CD, Winkley K, Gethin G. Psychological interventions for treating foot ulcers, and preventing their recurrence, in people with diabetes. Cochrane Database Syst Rev. 2021;(2):CD012835. https://doi.org/10.1002/14651858.CD012835.pub2.
Alkahoon C, Fernando M, Galappaththy C, Matthews EO, Lazzarini P, Moxon JV, et al. Meta-analysis of randomised controlled trials reporting the effect of home foot temperature monitoring, patient education or off-loading footwear on the incidence of diabetes related foot ulcers. Diabet Med. 2020;37(8):1266–79.
Ena J, Carretero-Gomez J, Arevalo-Lorido C, SanchezaArdila C, Zapatero-Gaviria A, Gomez-Huelgas G. The association between elevated foot skin temperature and the incidence of diabetic foot ulcers: a meta-analysis. Int J Low Extrem Wounds. 2020:1–8. https://doi.org/10.1177/1534734619897501.
Binning J, Woodburn J, Bus SA, Barn R. Motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration. Diabetes Metab Res Rev. 2019;35(2):e3105.
Heuch L, Gomersall JS. Effectiveness of offloading methods in preventing primary diabetic foot ulcers in adults with diabetes: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14(7):236–65.
Ahmad Sharoni S, Minhat H, Mohd Zulkefli N, Baharom A. Health education programmes to improve foot self-care practices and foot problems among older people with diabetes: a systematic review. Int J Older People Nursing. 2016;11(3):214–39.
van Netten JJ, Raspovic A, Lavery LA, Moneiro-Soares, Rasmussen A, Sacco ICN, et al. Patient prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(S1):e3270. https://doi.org/10.1002/dmrr.3270.
van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):84–98.
Bus SA, van Deursen RW, Armstrong DG, Lewis JEA, Caravaggi CF, Cavanagh PR. Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review. Diabetes Metab Res Rev. 2015;32(Suppl 1):99–118.
Bus SA, Valk GD, van Deursen RW, Armstrong DG, Caravaggi C, Hlavácek P, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev. 2008;24(Suppl 1):S162–80.
Healy A, Naemi R, Chockalingam N. The effectiveness of footwear as an intervention to prevent or to reduce biomechanical risk factors associated with diabetic foot ulceration: a systematic review. J Diabetes Complicat. 2013;27(4):391–400.
Paton J, Bruce G, Jones R, Stenhouse E. Effectiveness of insoles used for the prevention of ulceration in the neuropathic diabetic foot: a systematic review. J Diabetes Complicat. 2011;25(1):52–62.
Maciejewski M, Reiber G, Smith D, Wallace C, Hayes S, Boyko EJ. Effectiveness of diabetic therapeutic footwear in preventing reulceration. Diabetes Care. 2004;27(7):1774–82.
Mayfield J, Sugarman J. The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract. 2000;49(11):S17–29.
Ahmed S, Barwick A, Butterworth P, Nancarrow S. Footwear and insole design features that reduce neuropathic plantar foot ulcer risk in people with diabetes: a systematic literature review. J Foot Ankle Res. 2020;13:30. https://doi.org/10.1186/s13047-020-00400-4.
Blanchette V, Brousseau-Foley M, Cloutier L. Effect of contact with podiatry in a team approach context on diabetic foot ulcer and lower extremity amputation: systematic review and meta analysis. J Foot Ankle Res. 2020;13(15). https://doi.org/10.1186/s13047-020-0380-8.
Collings R, Freeman J, Latour JM, Paton J. Footwear and insole design features for offloading the diabetic at risk foot-a systematic review and meta analysis. Endocrinol Diabetes Metab. 2020. https://doi.org/10.1002/edm2.132.
Dy SM, Bennett WL, Sharma R, Zhang A, Waldfogel JM, Nebit SA, Yeh H-C, Chelladurai Y, Feldman D, Wilson LM, Robinson KA. Preventing complications and treating symptoms of diabetic peripheral neuropathy. AHRQ publication no. 17-EHC005-EF. 2017.
Hazenberg CEVB, aan de Stegge WB, Van Baal SG, Moll FL, Bus SA. Telehealth and telemedicine applications for the diabetic foot: a systematic review. Diabetes Metab Res Rev. 2019;36(3). https://doi.org/10.1002/dmrr.3247.
Da Silva AFR, de Carvalho FJ, Guimaraes MR, Bernardes RA, Brito VRR, da Silva ARV. Tecnologia movel no cuidado com os pes em pessoas com diabetes mellitus: revisao integrativa. Cienc Cuid Saude. 2020;19:e5036.
Matos M, Mendes R, Silva AB, Sousa N. Physical activity and exercise on diabetic foot related outcomes: a systematic review. Diabetes Res Clin Pract. 2018;139:81–90.
JBI checklist for randomised controlled trials.Checklist_for_RCTs.docx (live.com). Accessed 11 May 2022.
Jeffcoate WJ, Bus SA, Game FL, Hinchliffe RJ, Price PE, Schaper NC. Reporting standards of studies and papers on the prevention and management of foot ulcers in diabetes: required details and markers of good quality. Lancet Diabetes Endocrinol. 2016;4(9):781–8.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. https://doi.org/10.1093/ptj/83.8.713.
Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic test accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Jaeschke R, Guyatt G, Sackett DL, the Evidence-Based Medicine Working Group. Users’ guides to the medical literature: III. How to use an article about a diagnostic test: are the results of the study validity. JAMA. 1994;271:389–91.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Letts L, Wilkins S, Law MC, Stewart DA, Bosch J, Westmorland MG. Guidelines for critical review form - qualitative studies (version 2.0): McMaster University Occupational Therapy Evidence-Based Practice Research Group; 2007.
Harris RP, Helfland M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the U. S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(Suppl 3):21–35.
Malone J, Snyder M, Anderson G, Bernard VM, Holloway GA, Bunt TJ. Prevention of amputation by diabetic education. Am J Surg. 1989;158:520–4.
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254.
Gates M, Gates A, Duarte G, Cary M, Becker M, Prediger B, et al. Quality and risk of bias appraisals of systematic reviews are inconsistent across reviewers and centers. J Clin Epidemiol. 2020;125:9–15.
Pollock M, Fernandes R, Newton A, Scott S, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18.
Ballard M, Montgomery P. Risk of bias in overviews of reviews: a scoping review of methodological guidance and four-item checklist. Res Synth Methods. 2017;8(1):92–108.
Horton R. Offline: the gravy train of systematic reviews. Lancet. 2019;394(10211):1790.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89.
Rethlefsen, M.L., Kirtley, S., Waffenschmidt, S. et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev 2021;10: 39. https://doi.org/https://doi.org/10.1186/s13643-020-01542-.
Schulz K, Altman D, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
Pieper D, Buechter R, Jerinic P, Eikermann M. Overviews of reviews often have limited rigor: a systematic review. J Clin Epidemiol. 2012;65(12):1267–73.
Acknowledgments
We thank our public partner Mr. William Morrison for his help and enthusiasm during the project and Xin Wang, PhD candidate at the University of Edinburgh for her English translation of the review published in Chinese [17]. We also thank the following for their kind replies to our requests for clarification and additional information about their reviews; Dr. Susan O’Meara, the University of Leeds; Professor Dirk Stengel Unfallkrankenhaus, Berlin. Thanks are also due to Dr. Heather M McIntosh (independent researcher) for her assistance with risk of bias assessments and study selection and data extraction of the reviews identified in the update searches and Angela Martin (Podiatry Principal, NHS Fife) for her clinical advice.
Funding
This overview was funded as part of a wider project by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme (HTA project: 15/171/01). The views expressed are those of the authors and not necessarily those of the NIHR or UK Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
M.S. developed and implemented the search strategies. D.J.N. screened titles and abstracts to identify relevant reviews, assessed full text articles for eligibility, assessed risk of bias and extracted data from the included reviews. A.E.A. assessed full text articles for eligibility. F.C. designed the study, screened titles and abstracts, assessed risk of bias, and extracted data from the included reviews. H.Mc. participated in the data extraction and risk of bias assessments. F.C. interpreted the data and wrote the manuscript. M.S., D.J.N., A.E.A., read and approved the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Appendix
Appendix
Medline strategy
-
1.
exp foot orthoses/
-
2.
exp shoes/
-
3.
exp health education/
-
4.
exp primary health care/
-
5.
exp emollients/
-
6.
insole*.mp.
-
7.
footwear.mp.
-
8.
educat*.mp.
-
9.
specialist car*.mp.
-
10.
multi disciplinary team*.mp.
-
11.
multidisciplinary team*.mp.
-
12.
routine podiatry car*.mp.
-
13.
exp general practice/
-
14.
exp community health services/
-
15.
off load*.mp.
-
16.
offload*.mp.
-
17.
emollient*.mp.
-
18.
shoe*.mp.
-
19.
or/1–18
-
20.
exp foot/
-
21.
exp foot diseases/
-
22.
exp diabetic foot/
-
23.
exp diabetic neuropathies/
-
24.
exp diabetes mellitus/
-
25.
exp diabetic angiopathies/
-
26.
exp diabetes complications/
-
27.
exp podiatry/
-
28.
exp foot ulcer/
-
29.
exp skin ulcer/
-
30.
exp ischemia/
-
31.
exp bacterial infections/
-
32.
(diabet* adj3 ulcer*).mp.
-
33.
(diabet* adj3 (foot or feet)).mp.
-
34.
(diabet* adj3 wound*).mp.
-
35.
(diabet* adj3 amputat*).mp.
-
36.
or/20–35
-
37.
systematic* review*.mp.
-
38.
meta-analysis as topic/
-
39.
(meta-analytic* or meta-analysis or metanalysis or metaanalysis or meta analysis or meta synthesis or meta-synthesis or metasynthesis or meta-regression or metaregression or meta regression).mp.
-
40.
(synthes* adj3 literature).mp.
-
41.
(synthes* adj3 evidence).mp.
-
42.
(integrative review or data synthesis).mp.
-
43.
(research synthesis or narrative synthesis).mp.
-
44.
(systematic study or systematic studies).mp.
-
45.
(systematic comparison* or systematic overview*).mp.
-
46.
((evidence based or comprehensive or critical or quantitative or structured) adj review).mp.
-
47.
(realist adj (review or synthesis)).mp.
-
48.
or/37–47
-
49.
review.pt.
-
50.
(medline or pubmed or embase or cinahl or psyc?lit or psyc?info).mp.
-
51.
((literature or database* or bibliographic or electronic or computeri?ed. or internet) adj3 search*).mp.
-
52.
(electronic adj3 database*).mp.
-
53.
included studies.mp.
-
54.
(inclusion adj3 studies).mp.
-
55.
((inclusion or selection or predefined or predetermined) adj criteria).mp.
-
56.
(assess* adj3 (quality or validity)).mp.
-
57.
(select* adj3 (study or studies)).mp.
-
58.
(data adj3 extract*).mp.
-
59.
extracted data.mp.
-
60.
(data adj3 abstraction).mp.
-
61.
published intervention*.mp.
-
62.
((study or studies) adj2 evaluat*).mp.
-
63.
(intervention* adj2 evaluat*).mp.
-
64.
(confidence interval* or heterogeneity or pooled or pooling or odds ratio*).mp.
-
65.
(Jadad or coding).mp.
-
66.
or/50–65
-
67.
49 and 66
-
68.
review.ti.
-
69.
66 and 68
-
70.
(review* adj4 (papers or trials or studies or evidence or intervention* or evaluation*)).mp.
-
71.
48 or 67 or 69 or 70
-
72.
letter.pt.
-
73.
editorial.pt.
-
74.
comment.pt.
-
75.
72 or 73 or 74
-
76.
71 not 75
-
77.
19 and 36 and 76
Embase search strategy
-
1.
exp foot orthosis/
-
2.
shoe/
-
3.
exp health education/
-
4.
exp primary health care/
-
5.
emollient agent/
-
6.
insole*.mp.
-
7.
footwear*.mp.
-
8.
educat*.mp.
-
9.
specialist car*.mp.
-
10.
multi disciplinary team*.mp.
-
11.
multidisciplinary team*.mp.
-
12.
routine podiatry car*.mp.
-
13.
general practice/
-
14.
exp community care/
-
15.
off load*.mp.
-
16.
offload*.mp.
-
17.
emollient*.mp.
-
18.
shoe*.mp.
-
19.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
20.
exp foot/
-
21.
exp foot disease/
-
22.
diabetic foot/
-
23.
diabetic neuropathy/
-
24.
exp diabetes mellitus/
-
25.
exp diabetic angiopathy/
-
26.
(diabet* adj3 complicat*).mp.
-
27.
podiatry/
-
28.
foot ulcer/
-
29.
exp skin ulcer/
-
30.
exp ischemia/
-
31.
exp bacterial infection/
-
32.
(diabet* adj3 ulcer*).mp.
-
33.
(diabet* adj3 (foot or feet)).mp.
-
34.
(diabet* adj 3 wound*).mp.
-
35.
(diabet* adj3 amputat*).mp.
-
36.
20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35
-
37.
systematic* review*.mp.
-
38.
meta analysis/
-
39.
(meta-analytic* or meta-analysis or metanalysis or metaanalysis or meta analysis or meta synthesis or meta-synthesis or metasynthesis or meta-regression or metaregression or meta regression).mp.
-
40.
(synthes* adj3 literature).mp.
-
41.
(synthes* adj3 evidence).mp.
-
42.
(integrative review or data synthesis).mp.
-
43.
(research synthesis or narrative synthesis).mp.
-
44.
(systematic study or systematic studies).mp.
-
45.
(systematic comparison* or systematic overview*).mp.
-
46.
((evidence based or comprehensive or critical or quantitative or structured) adj review).mp.
-
47.
(realist adj (review or synthesis)).mp.
-
48.
or/37–47
-
49.
review.pt.
-
50.
(medline or pubmed or embase or cinahl or psyc?lit or psyc?info).mp.
-
51.
((literature or database* or bibliographic or electronic or computer?ed. or internet) adj3 search*).mp.
-
52.
(electronic adj3 database*).mp.
-
53.
included studies.mp.
-
54.
(inclusion adj3 studies).mp.
-
55.
((inclusion or selection or predefined or predetermined) adj criteria).mp.
-
56.
(assess* adj3 (quality or validity)).mp.
-
57.
(select* adj3 (study or studies)).mp.
-
58.
(data adj3 extract*).mp.
-
59.
extracted data.mp.
-
60.
(data adj3 abstraction).mp.
-
61.
published intervention*.mp.
-
62.
((study or studies) adj2 evaluat*).mp.
-
63.
(intervention* adj2 evaluat*).mp.
-
64.
(confidence interval* or heterogeneity or pooled or pooling or odds ratio*).mp.
-
65.
(jadad or coding).mp.
-
66.
or/50–65
-
67.
49 and 66
-
68.
review.ti.
-
69.
66 and 68
-
70.
(review* adj4 (papers or trials or studies or evidence or intervention* or evaluation*)).mp.
-
71.
48 or 67 or 69 or 70
-
72.
letter.pt.
-
73.
editorial.pt.
-
74.
comment.pt.
-
75.
72 or 73 or 74
-
76.
71 not 75
-
77.
exp. animals/not humans/
-
78.
78.76 not 77
-
79.
19 and 36 and 76
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Crawford, F., Nicolson, D.J., Amanna, A.E. et al. Reliability of the evidence to guide decision-making in foot ulcer prevention in diabetes: an overview of systematic reviews. BMC Med Res Methodol 22, 274 (2022). https://doi.org/10.1186/s12874-022-01738-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12874-022-01738-y