Abstract
Objective
To examine the unique contribution of patient reported experiences of compassion to overall patient quality care ratings. Additionally, we assess whether patients’ reported experiences of compassion in the emergency department differed between sociodemographic groups.
Methods
Provincial data for this cross-sectional study were collected from 03/01/2022 to 09/05/2022 from 14 emergency departments in Alberta, Canada. Data from 4501 emergency department patients (53.6% women, 77.1% White/European) were analyzed. The primary outcome was patients’ overall quality care ratings during their most recent ED visit. Measures included in the hierarchical stepwise regression included demographics, and those drawn from the Emergency Department Patient Experience of Care (EDPEC) questionnaire: single and multi-item measures of patient information (e.g., patient perceptions health) and patient experience (e.g., physician communication), and compassion (e.g., Sinclair Compassion Questionnaire; SCQ-ED).
Results
Data from 4501 ED patients were analysed. Stepwise hierarchical linear multiple regression indicated that of 21 included variables, compassion most strongly predicted overall quality care ratings (b=1.61, 95% CI 1.53-1.69, p<.001, f2=.23), explaining 19% unique variance beyond all other measures. One-way ANOVAs indicated significant demographic differences in mean compassion scores, such that women (vs. men) reported lower compassion (MD=-.15, 95% CI=-.21, -.09, p<.001), and Indigenous (vs. White) patients reported lower compassion (MD=-.17, 95% CI =-.34, -.01, p=.03).
Conclusions
Compassion was identified as a key contributor to ED overall quality care ratings, and experiences of compassion varied as a function of demographics. Patient-reported compassion is an indicator of quality care that needs to be formally integrated into clinical care and quality care assessments.
Similar content being viewed by others
Introduction
In comparison to other healthcare environments, emergency care is relatively unmatched when it comes to utilization, pace, and acuity. In light of these factors, and the increasing demand of patients seeking care in emergency departments (EDs), there have been urgent calls [1,2,3,4] to ensure that patients receive care that is both safe and high-quality. Increasingly, a recognized critical component of quality care is compassion [5,6,7]. In this study, we examine how compassion contributes to a primary outcome of the patient experience, overall quality care rating, and whether there are demographic differences in patients’ experiences of compassion. We measure compassion using a validated patient reported measure adapted for use in the ED.
Compassion is operationalized as “a virtuous response that seeks to address the suffering and needs of a person through relational understanding and action.”[5 p.195] Compassion has potential to alleviate patient suffering and contribute to improved quality care [5, 7,8,9]. Likewise, less compassionate care may promote negative perceptions of care, patient complaints, and worse patient outcomes [1,2,3,4,5, 7,8,9,10,11]. Unfortunately, patients in various healthcare settings have indicated that compassion is one of their greatest unmet needs, and there are indications that this is increasing [2, 3, 7, 9, 10]. The implications of health systems that are lacking compassion on patients and healthcare provider well-being are well-documented [2, 3, 11]. In the ED specifically, a lack of compassion was identified as a primary factor in system wide increased patient safety issues, adverse medical events, and in some cases mortality [4].
A mixed-methodological study examining the role of compassion in emergency medicine settings found that UK National Health Service consultants who reported higher levels of compassion fatigue and/or lower levels of compassion satisfaction reported a greater propensity to treat both colleagues and patients with irritability, and with a reduced standard of care [1]. Although these findings are important steps to understanding the consequences of deficiencies in compassion, more research examining patient experiences of compassion in the ED is needed.
Recently, a valid and reliable patient reported compassion measure was developed, providing the opportunity to investigate the impact of compassion in the ED setting. The Sinclair Compassion Questionnaire’s (SCQ) validity has been established in long term care, hospice, and acute care settings [12] and was recently identified as the standard for evaluating compassion in research and clinical care [6]. In the current study, we verify its validity in the ED, and explore two principal goals. First, we examine whether the SCQ-ED explains variance in overall quality care ratings. Specifically, whether compassion predicts unique variance in overall quality care ratings, over and above other commonly collected measures of patient information, demographics, and patient experience. Second, we explore whether ED patients’ experiences of compassion varied based on demographics, with the aim of determining whether any specific groups of patients indicated differences in the compassion they received in the ED.
Methods
Study design, procedure, and sample
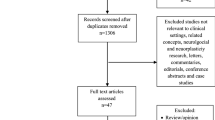
Employing a cross-sectional survey design, data were collected from ED patients between 03/01/2022 to 09/05/2022 in Alberta, Canada. Data were collected from the fourteen busiest urban and regional hospital EDs. Every two weeks, 160 patients were sampled from each ED (50% of which were discharged from the ED, and 50% who were admitted to the hospital after their ED visit). The survey vendor called respondents up to 9 times, at various times and days in an attempt to reach them. Surveying continued until at least 20 discharged and 20 admitted patients from each of the 14 EDs have responded, on each bi-weekly wave. Data from a total of 4501 ED patients were available for analysis.
Exclusion criteria were patients who: were under 16; left the ED without being seen or treated; died in the context of their ED visit or inpatient admission; were without contact information (i.e., phone number), had privacy-sensitive cases (e.g., domestic abuse, attempted suicide, etc.), or had been surveyed in the past year. The patient response rate during the study period was 23%.
This study is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies. This study was approved the Research Ethics Board (CHREB) at the University of Calgary (REB21-1938). In accordance with our REB approval, we were granted a waiver of consent for all participants, as gaining the contact information for these individuals through this administrative data was deemed not feasible. The dataset was obtained from the data custodians, the Health Quality Council of Alberta.
Measures
Demographic and patient information
Demographics including age, gender, education, ethnicity, household income, self-reported overall health, self-perceived financial situation, and reason for visit were included (See Appendix A for full demographic questions).
Emergency department patient experience of care
Seventeen items from the Emergency Department Patient Experience of Care (EDPEC) survey, which has been extensively used and validated [13,14,15], was used to assess patients’ experiences during their most recent ED visit; referred hereafter as patient experience measures. Domains of patient experience included (See Appendix A): multi-item composites such as communication with patients by ED physicians (current sample Cronbach’s α = .83; Q17-20), communication with patients by ED nurses (current sample Cronbach’s α = .82; Q13-16), and single item measures covering: whether the patient arrived by ambulance (Q3), timeliness of care (Q4), new medication received (Q5), whether the side effects of new medications were described in a clear way (Q6), whether patient had pain (Q7), whether doctors and nurses attempted to reduce patient pain (Q8), pain medication received (Q9), whether the possible side effects of pain meds were clearly described (Q10), whether common tests were conducted (Q11), whether doctors and nurses provided sufficient info on the results of tests (Q12).
Finally, our primary outcome measure queried patients’ overall perceptions of care (i.e., 0 corresponding to the worst care possible, and 10 to the best care) during their most recent ED visit (Q21), referred to hereafter as overall quality care ratings.
Sinclair compassion questionnaire
The SCQ [12] measures a single latent construct of compassion and demonstrates strong internal consistency (original study Cronbach’s α = .96). The development of the SCQ rigorously adhered to measure development guidelines [16, 17] and heavily featured patient perspectives throughout its development. The full 15-item SCQ (current sample Cronbach’s α = .98) was included in this study, querying patients’ experiences of compassion by their healthcare providers (HCP) during their most recent ED visit on a 5-point Likert scale. The SCQ-ED, along with a variety of adapted versions (e.g., SCQ-Short Form, SCQ-Primary Care, etc.) are freely available to researchers and clinicians at www.compassionmeasure.com.
EQ-5D
The EQ-5D is a 5-item measure extensively used and validated non-disease specific tool aimed at measuring patients’ quality of life (current sample Cronbach’s α = .77) [18]. Full wording of the EQ-5D can be found in Appendix A.
Data analysis
After preparing the dataset for analyses (e.g., data cleaning), the following analyses were conducted to address the study objectives. First, validity of the SCQ-ED in this population was verified (see Appendix B). Next, we assessed correlations (Pearson and point-biserial) between compassion and demographics, patient information, and patience experience variables. This served as a preliminary exploration of the zero-order relationships before moving on to the regression analysis addressing our primary objective. To explore whether and how much compassion uniquely predicted the variance explained for patients’ overall quality care ratings beyond patient demographics and information as well as patience experience measures contained in the EDPEC, we conducted a stepwise hierarchical linear multiple regression. It is important to note that throughout this study we will use terminology such as “predict” or “predictive”, as it normatively used in regression-based analyses. However, such language should not be conflated with etiological or causal claims, rather it refers to multiple factors that in together predict an outcome of interest, regardless of causality [19]. This regression analysis provided an opportunity to directly compare the explanatory power of all variables for quality care ratings simultaneously through the standardization of the beta weights. Finally, we sought to address whether any specific groups of patients reported lower levels of compassion during their recent ED visits by conducting analysis of variance (ANOVAs) with patient demographics.
Pearson and point-biserial correlations
Pearson or point-biserial correlation analyses were conducted between all continuous and dichotomous variables. These analyses provide information about the extent to which two variables are related to each other linearly, ranging between -1 and 1.A common rule of thumb for interpreting the strength of correlations states that coefficients of .10 indicate small associations, .30 indicate moderate associations, and those .50 or greater indicate large associations [20].
Multiple linear regression
A three-step hierarchical linear regression was conducted with overall quality care ratings as the outcome measure. Variables were added in a stepwise manner to assess the unique contribution of demographics and patient information (i.e., EQ-5D) [Step 1], patient experience measures (i.e., EDPEC) [Step 2], and compassion (i.e., SCQ-ED) [Step 3] on overall quality care ratings. This strategy also allowed for the direct comparison of the contribution of each of these variables through the standardization of the beta-weights (i.e., B in Table 4).
We utilized Cohen’s f2 as an indicator of local effect size for our multiple regressions. The common rule of thumb of interpreting f2 indicates that .02 = small, .15 = medium, and .35 = a large effect [20].
Analysis of variance
Analysis of variance (ANOVA) was used to explore whether SCQ-ED scores differed based on categorical demographic variables. We have used η2 as an indicator of effect size (.01 = small, .06 = medium, and .14 = large effects [21]. Post-hoc analyses using Tukey’s HSD [22] were used to assess pairwise comparisons.
Results
A total of 4501 patients completed the survey, gender characteristics consisted of 53.6% women (45.3% men). Ethnicity of the sample was predominantly White/European (77.1%). The sample age was well distributed across all groups, with 16–24-year-olds representing the smallest proportion of the sample (9.3%), and 65-74-year-olds representing the largest proportion (16.2%). Full sample characteristics can be found in Table 1. All analyses were conducted using IBM SPSS 27.
Preliminary analyses
Listwise deletion was employed for missing data (n = 304, see Appendix B for missing value analysis). The SCQ-ED demonstrated excellent validity [6, 12] and internal consistency/reliability, with a Cronbach’s alpha of .98 (N = 4197). Descriptive statistics for the SCQ-ED can be found in Table 2, along with SCQ-ED item intercorrelations in Appendix C.
Exploring the zero-order relationships
Pearson and point-biserial correlational analyses revealed a large number of statistically significant relationships. Mean SCQ-ED scores were strongly associated with overall quality care ratings (r = .76, p <.001), nursing communication (r = .61, p = <.001), and doctor communication (r = .56, p <.001). Moderate relationships were revealed between the SCQ-ED and whether doctors and nurses provided sufficient information about the results of tests conducted (r = .38, p <.001), and whether doctors and nurses attempted to reduce patients’ pain (r = .33, p <.001). Small to moderate relationships also existed between the SCQ-ED and whether patients received care within 30 minutes (r = .26, p <.001), whether doctors or nurses clearly described the potential side effects of new medications (r = .26, p <.001), and whether the potential side effects of pain medications were discussed (r = .22, p <.001). Additional correlational relationships between the SCQ-ED, EDPEC items, and the EQ5D can be found in Table 3, and full correlational relationships, including demographics can be found in Appendix D.
Assessing the unique contribution of compassion to quality care ratings
A three-step hierarchical multiple regression was conducted to predict overall quality care ratings from applicable continuous, ordinal, and dichotomously coded variables (N = 2998 Table 4).
In step one, demographic and patient information variables statistically significantly contributed to the model, F(14, 2984) = 22.05, p < .001, R2 = .09. In step 2, patient experience variables statistically significantly added to the model, F(20, 2978) = 125.59, p < .001, R2 = .45 (R2 Δ = .36, p < .001). In step 3, the SCQ statistically significantly added to the model, F(21, 2977) = 259.80, p < .001, R2 = .65 (R2 Δ = .19, p < .001).
Adding the SCQ-ED to the regression model in step 3 explained an additional 19% variance in overall quality care ratings, p < .001. Overall, with the inclusion of the SCQ, we were able to explain 65% (versus 46%) of the variance in ED patients’ overall quality care ratings.
The full model significantly predicted overall quality care ratings, A total of 4 variables statistically predicted care ratings with effect sizes f2 ≥ .01. In order of effect size, these significant variables were the SCQ-ED (f2=.23), nurse communication (f2=.01), whether patients received care within 30 minutes (f2=.01), and age (f2=.01); see Table 4.
Investigating demographic group differences in compassion
To assess whether patients reported experiences of compassion differed by demographic grouping, one-way ANOVAs were conducted. If statistically significant ANOVAs were identified, post-hoc analyses were utilized to better understand these differences. To supplement these analyses, a multivariate regression predicting SCQ-ED mean scores can be found in Appendix B.
Ethnicity and compassion
A one-way ANOVA was conducted, indicating a statistically significant difference between ethnic groups was found, F(7, 4040) = 2.83, η2 = .01, p = .006. Tukey’s post-hoc pairwise comparisons revealed that compassion scores belonging to those that identified as Indigenous People of Canada were statistically significantly lower than those that identified as white (Mean Difference = -.17, SE = .05, 95% CI = [-.34, -.01], p = .033).
Gender and compassion
A statistically significant difference between groups was found, F(4, 4455) = 11.58, η2 = .01, p <.001. Tukey’s post-hoc pairwise comparisons revealed that those that identified as women reported statistically significantly lower levels of compassion than those that identified as men (Mean Difference = -.15, SE = .02, 95% CI = [-.21, -.09], p <.001).
Other variables and compassion
No statistically significant differences were found between groups by language spoken (p = .797), regional health zone (p = .059), education (p = .941), or reason for their ED visit (p = .345)
Exploratory demographic group differences in overall care ratings
Given that mean compassion scores differed by ethnicity and gender, we opted exploratorily assess whether similar differences existed for these demographic groups by overall care ratings. As such, we conducted additional one-way ANOVAs for care ratings by ethnicity and gender.
Ethnicity and care ratings
A statistically significant difference between ethnicity groups was found, F(7, 4032) = 5.49, η2 = .01, p <.001. Tukey’s post-hoc pairwise comparisons revealed that those that identified as Indigenous peoples of Canada reported statistically significantly lower overall care ratings (Mean Difference = -.47, SE = .14, 95% CI = [-.91, -.03], p = .027). They also reported statistically significantly lower care ratings than Southeast Asian patients (Mean Difference = -.71, SE = .21, 95% CI = [-1.35, -.07], p = .017) and Latin American/South American/Hispanic patients, (Mean Difference = -.84, SE = .25, 95% CI = [-1.61, -.07], p = .020). Additionally, other pairwise differences indicated that such that South Asian participants reported statistically significantly lower care ratings than white patients (Mean Difference = .53, SE = .15, 95% CI = [.09, -.97], p = .006.), Southeast Asian patients (Mean Difference = -.78, SE = .21, 95% CI = [-1.42, -.13], p = .006), and Latin American/South American/Hispanic patients, (Mean Difference = -.91, SE = .25, 95% CI = [-1.67, -.14], p = .008). Finally, Latin American/South American/Hispanic patients reported statistically significantly higher care ratings than patients with mixed ethnicities (Mean Difference = .97, SE = .31, 95% CI = [.02, 1.92], p = .042).
Gender and care ratings
A statistically significant difference between gender groups was found, F(4, 4042) = 5.74, η2 = .01, p <.001. Tukey’s post-hoc pairwise comparisons revealed that women statistically significantly reported lower care ratings than men (Mean Difference = -.28, SE = .06, 95% CI = [-.45, -.11], p < .001.)
Demographic group differences in overall care ratings controlling for compassion
Results of the above ANOVAs indicated that the group in overall care ratings for Indigenous (vs white) patients, and women (vs. men) operated in the same direction as the differences found in compassion scores. To further explore whether patients’ reported compassion played a role in these discrepancies patients’ overall care ratings two Analyses of Covariance (ANCOVA) with mean SCQ-ED scores included as the covariate were explored and detailed below.
Ethnicity, compassion, and care ratings
A statistically significant relationship was found for mean SCQ-ED scores F(1, 4020) = 5535.01, <.001, and ethnicity F(7, 4020) = 3.36, p = .001. The model had a R2 = .58. This can be interpreted such that compassion explained a very large additional proportion of variance in overall care ratings, consistent with the multiple regression results above. Ethnicity remained a statistically significant predictor of overall care ratings however, but had a reduced F value, indicating that compassion may have explained some (but not all) of these differences in overall care ratings.
Gender, compassion, and care ratings
A statistically significant relationship was found for mean SCQ-ED scores F(1, 4028) = 6112.27, <.001 and overall care ratings. However, gender did not have a statistically significant relationship with overall care ratings F(4, 4028) = .20, p = .940. The model had a R2 = .58. This can be interpreted such that compassion explained a very large additional proportion of variance in overall care ratings, consistent with the multiple regression results above. Gender however became non-significant in the presence of mean SCQ-ED scores, indicating that the lower care ratings reported by women (vs men) were likely due to differences in perceived compassion in the ED.
Discussion
To accomplish our main objective of understanding how compassion contributes to overall quality care ratings when considered within the broader landscape of existing patient experience measures, we used stepwise hierarchical linear multiple regression. We discovered that compassion, as measured by the SCQ-ED, was by far, the variable with the strongest prediction of overall quality care ratings, with a moderate-to-large effect size. Additionally, our analyses indicated that the inclusion of the SCQ-ED uniquely explained sizable (nearly 20%) additional variance in overall quality care ratings - the main outcome variable in the EDPEC, and other patient experience surveys including the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys [23]. When one considers the salience of compassion to overall quality care ratings, above and beyond the existing domains of patient experience embedded within these questionnaires; the integration of compassion within these surveys and learning health systems [24] warrants serious consideration [25].
In addition to demonstrating that compassion was a key predictor of patients’ quality care ratings, another novel finding of this study was that receiving compassionate care varied according to patient demographic group (i.e., ethnicity and gender). First, we noted that women reported statistically significant lower levels of compassion and overall care ratings in the ED when compared to men. Indeed, follow-up analyses indicated that these differences in compassion, as measured by the SCQ-ED were very likely responsible for effects such that reported women lower overall care ratings than men. These quantifiable differences in compassion, as measured by the SCQ-ED are consistent with findings of discrimination in healthcare delivery for women versus men, which have found that personal experiences of prejudice are associated with reduced adherence to healthcare screening guidelines and pre-emptive health behaviours such as going to see a doctor when seriously ill [26]. Our findings that women experienced both less compassion and reported reduced overall care rating in ED settings merits further investigation within the context of experiences of prejudice and discrimination.
Additionally, we found statistically significant differences in the responses on the SCQ-ED between Indigenous and white/European patients. Specifically, we found that Indigenous patients reporting lower levels of compassion, as well as lower overall care ratings. This is consistent with findings that Indigenous peoples experience significant health disparities when compared to non-indigenous groups [21, 27]. Exploratory follow-up analyses (i.e., ANCOVA) examined group differences on overall care ratings, and indicated that the differences in patient-reported compassion may have played a role in the differences in overall care ratings reported by Indigenous patients. Our findings also echo recent work which found that First Nations individuals in Alberta were almost twice as likely to leave EDs without receiving care than non-First Nations patients, at least in part due to prejudice and discrimination. Follow-up interviews described First Nations’ patients facing anti-Indigenous stereotypes in diagnostic questions and case management, overhearing prejudicial attitudes being expressed by their providers, and discriminatory behaviours surrounding their quality of care [28]. We recommend future research, in partnership with Indigenous and diverse gender communities, and the deployment of improved EDI training in healthcare settings. Such approaches would help explore whether understandings and experiences of compassion differ, along with the development of studies investigating the role of how institutional racism, sexism, unconscious bias, and stigma operate in the inequitable access to and provision of compassion to different social groups [29, 30]. Further, we encourage that future research explore potentially interactive effects between patient and HCP sociodemographic features on patient-perceived compassion (e.g., do patients that receive care from providers with similar demographic identities, or cultural backgrounds feel they received more compassionate care?).
The validation of the SCQ-ED in this study also provides health leaders, researchers, and clinicians a valid and reliable measure to routinely assess patients experiences of compassion, and in doing so, an important, but previously hidden ingredient of quality care. We would like to highlight that the findings in this study are strengthened by our large sample size (N = 4501), and that our sample was derived from 14 EDs. Such a tool has potential utility for monitoring ED quality care, assessing interventions aimed at improving compassion, and providing patients with the ability to provide feedback on a central, but previously unmeasurable, aspect of the patient experience. We also note that a short 5-item SCQ measure is available (Sinclair et al, 2021), which has maintained the excellent reliability and validity of the full SCQ-ED. This short measure reduces patient burden and allows for greater flexibility where survey length is a concern. At a health systems level, the SCQ-ED could be considered a factor in hospital rating scores, while providing opportunities for health organizations to potentially establish and monitor benchmarks of compassion at a unit, institutional, regional or national level, and among various patient groups. Such benchmarking would allow for clear and tenable research connections between patient-reported compassion and a host of important clinical outcomes (e.g., patient recovery times, symptom severity, survival, etc.).
Study limitations
This study is limited in its recall period, such that patients were asked to recall their most recent ED visit. As such, there is a level of variability in time from healthcare experienced to completion of the questionnaire, potentially limiting some specificity in recall. Additionally, we recognize several ethnic groups were not represented in our sample, specifically individuals identifying as Black or African American, and Middle Eastern, North African, and West African patients. We recognize this lack of full representation in the respondents and note that it is possible that such limited responding may have biased our results in an unknown direction. We therefore strongly recommend that future research include these populations. We also believe it is important to note that, our response rate may have been limited (i.e., 23%). Due to the data being collected as part of the provincial health authority’s standardized patient experience survey, we were limited to data they were authorized to collect and share. This did not include the demographic data of the initial population sampled.
It is important to acknowledge that although this study was conducted among a large sample of patients from a variety of regional and metropolitan EDs, our data was exclusively collected from the Canadian province of Alberta. We recommend the replication of these results in other jurisdictions, both nationally and internationally. While the initial results from ongoing studies (i.e., Spain, Italy, Portugal) validating the SCQ indicate that the SCQ functions well across cultures, future studies are required to assess the transferability of the SCQ-ED across cultures [31, 32]. Our very large sample provides us with an excellent opportunity to conduct analyses that can detect small and complex effects, without worrying about insufficient statistical power. While large sample sizes allow for the detection small and complex effects, it also comes with important caveats, including interpreting our findings in conjunction with our provided effect sizes and confidence intervals. Finally, data collection occurred during the COVID-19 pandemic and as such future studies outside the context of a pandemic are needed to verify and extend our results [33].
We acknowledge the limitations of cross-sectional studies, as such designs are insufficient for confirming etiological relationships between compassion and important outcome measures, such as overall patient experience. We recommend future studies employ both experimental and longitudinal designs to better establish causal relationships between perceptions of compassion in ED settings, quality care ratings and other important outcomes (e.g., recovery time, patient complaints, etc.).
In summary, this cross-sectional study of patient experience measures in EDs, we identified compassion as strongly associated with patients overall quality care ratings, presenting researchers with compelling evidence to consider the inclusion of compassion as a core domain of the patient experience. Finally, this study provided healthcare leaders, policy makers, and providers evidence that improving compassion is an essential and potent means for improving quality care, that can no longer be dismissed.
Availability of data and materials
The data that support the findings of this study are not publicly available due to privacy restrictions. However, anonymized data may be available from the Health Quality Council of Alberta upon reasonable request. Please contact Dr. Markus Lahtinen (Markus.Lahtinen@hqca.ca) with requests.
Abbreviations
- ANOVA:
-
Analysis of Variance
- CAHPS:
-
Consumer Assessment of Healthcare Providers and Systems
- CFREB:
-
Conjoint Faculties Research Ethics Board
- ED:
-
Emergency Department
- EDPEC:
-
Emergency Department Patient Experience of Care
- HQCA:
-
Health Quality Council of Alberta
- MD:
-
Mean difference
- SCQ-ED:
-
Sinclair Compassion Questionnaire – Emergency Department
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
References
Dasan S, Gohil P, Cornelius V, Taylor C. Prevalence, causes and consequences of compassion satisfaction and compassion fatigue in emergency care: a mixed-methods study of UK NHS Consultants. Emerg Med J. 2015;32(8):588–94.
Lown BA, Rosen J, Marttila J. An agenda for improving compassionate care: a survey shows about half of patients say such care is missing. Health Aff. 2011;30(9):1772–8.
Francis R. Report of the Mid Staffordshire NHS Foundation Trust public inquiry: executive summary. London: The Stationery Office; 2013.
Parliamentary and Health Service Ombudsman. Care and compassion? Report of the Health Service Ombudsman on ten investigations into NHS care of older people. 2011. Cited 2023 Aug 3. Available from: https://www.ombudsman.org.uk/sites/default/files/2016-10/Care%20and%20Compassion.pdf.
Sinclair S, McClement S, Raffin-Bouchal S, Hack TF, Hagen NA, McConnell S, Chochinov HM. Compassion in health care: an empirical model. J Pain Sympt Manag. 2016;51(2):193–203.
Sinclair S, Kondejewski J, Hack TF, Boss HC, MacInnis CC. What is the most valid and reliable compassion measure in healthcare? An updated comprehensive and critical review. Patient-Patient-Centered Outcomes Res. 2022;15(4):399–421.
Trzeciak S, Mazzarelli A, Booker C. Compassionomics: The revolutionary scientific evidence that caring makes a difference. Pensacola: Studer Group; 2019.
Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229–39.
Sinclair S, Norris JM, McConnell SJ, Chochinov HM, Hack TF, Hagen NA, McClement S, Bouchal SR. Compassion: a scoping review of the healthcare literature. BMC Palliat Care. 2016;15(1):1–6.
Lown BA, Dunne H, Muncer SJ, Chadwick R. How important is compassionate healthcare to you? A comparison of the perceptions of people in the United States and Ireland. J Res Nurs. 2017;22(1–2):60–9.
Pavlova A, Paine SJ, Sinclair S, O’Callaghan A, Consedine NS. Working in value-discrepant environments inhibits clinicians’ ability to provide compassion and reduces well-being: a cross-sectional study. J Intern Med. 2023;293(6):704–23.
Sinclair S, Hack TF, MacInnis CC, Jaggi P, Boss H, McClement S, Sinnarajah A, Thompson G, The COMPASS Research Team. Development and validation of a patient-reported measure of compassion in healthcare: the Sinclair Compassion Questionnaire (SCQ). Open. 2021;11:e045988.
Weinick RM, Becker K, Parast L, Stucky BD, Elliott MN, Mathews M, Chan C, Kotzias V. Emergency department patient experience of care survey: development and field test. Rand Health Quarterly. 2014;4(3). PMC5396202.
Health Quality Council of Alberta. Emergency Department Patient Experience of Care Survey Methodology. HQCA Focus; 2017. Cited 2023 Aug 3. Available from: https://focus.hqca.ca/wp-content/uploads/2018/03/EDPEC_survey_methods_FINAL.pdf.
Ye F, Parast L, Hays RD, Elliott MN, Becker K, Lehrman WG, Stark D, Martino S. Development and validation of a patient experience of care survey for emergency departments. Health Serv Res. 2022;57(1):102–12.
Hinkin TR. A brief tutorial on the development of measures for use in survey questionnaires. Organ Res Methods. 1998;1(1):104–21.
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. USA: Oxford University Press; 2015.
Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Ramspek, et al. Prediction or causality? A scoping review of their conflation within current observational research. Eur J Epidemiol. 2021;36:889–98.
Cohen J. Statistical power analysis for the behavioral sciences. New York: Routledge; 1988.
Wylie L, McConkey S, Corrado AM. Colonial legacies and collaborative action: improving indigenous Peoples’ Health Care in Canada. Int Indig Policy J. 2019;10(5):1–27. https://doi.org/10.18584/iipj.2019.10.5.9340.
Abdi H, Williams LJ. Tukey’s honestly significant difference (HSD) test. In: Salkind NJ, editor. Encyclopedia of research design. Thousand Oaks: Sage Publications; 2010. p. 1–5.
Agency for Healthcare Research and Quality. CAHPS Emergency Department Survey. Rockville: Agency for Healthcare Research and Quality; 2023. Cited 2023 Nov 10. Available from: https://www.ahrq.gov/cahps/surveys-guidance/ed-cahps/index.html.
Agency for Healthcare Research and Quality. About Learning Health Systems. Rockville: Agency for Healthcare Research and Quality; Cited 2024 Jan 25. Available from: https://www.ahrq.gov/learning-health-systems/about.html.
Agency for Healthcare Research and Quality. What Is Patient Experience?. Cited 2023 Aug 3. Available from: https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html.
Facione NC, Facione PA. Perceived prejudice in healthcare and women’s health protective behavior. Nurs Res. 2007;56(3):175–84.
Health and inequity in Australia. Lancet Public Health. 2023;8(8):e575. Available from: https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(23)00157-3/fulltext.
McLane P, Bill L, Healy B, Barnabe C, Big Plume T, Bird A, Colquhoun A, Holroyd BR, Janvier K, Louis E, Rittenbach K, Curtin KD, Fitzpatrick KM, Mackey L, MacLean D, Rosychuk RJ. Leaving emergency departments without completing treatment among First Nations and non–First Nations patients in Alberta: a mixed-methods study. CMAJ. 2024;196(15):E510–23. https://doi.org/10.1503/cmaj.231019.
Tang SY, Browne AJ. ‘Race’ matters: racialization and egalitarian discourses involving Aboriginal people in the Canadian health care context. Ethnic Health. 2008;13(2):109–27.
McLane P, Mackey L, Holroyd BR, Fitzpatrick K, Healy C, Rittenbach K, Plume TB, Bill L, Bird A, Healy B, Janvier K. Impacts of racism on First Nations patients’ emergency care: results of a thematic analysis of healthcare provider interviews in Alberta Canada. BMC Health Serv Res. 2022;22(1):1–8.
Chu XR, Jaggi P, Louis JS, Sinclair S. Initial Validation of a Patient-Reported Compassion Measure in a Mandarin-Speaking Long-Term Care Patient Population. J Nurs Meas. 2024;32(2):300–11.
Soto-Rubio A, Andreu Y, Gil-Juliá B, et al. Adaptation and validation of a patient-reported compassion measure in the Spanish population: The Spanish version of the Sinclair Compassion Questionnaire (SCQesp). Res Nurs Health. 2024;47(3):344–55. https://doi.org/10.1002/nur.22373.
Lluch C, Galiana L, Doménech P, Sansó N. The impact of the COVID-19 pandemic on burnout, compassion fatigue, and compassion satisfaction in healthcare personnel: a systematic review of the literature published during the first year of the pandemic. Healthcare. 2022;10(2):364.
Acknowledgements
Harrison Boss, Dr. Cara MacInnis, and Dr. Shane Sinclair had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Use of the Sinclair Compassion Questionnaire (SCQ), authored by Dr. Shane Sinclair, Dr. Tom Hack, Dr. Cara MacInnis, Harrison Boss, Priya Jaggi, Dr. Susan McClement, Dr. Aynharan Sinnarajah and Dr. Genevieve Thompson was made under license from UTI Limited Partnership. The Sinclair Compassion Questionnaire (SCQ) and other adaptions are available at www.compassionmeasure.com; by emailing the contact author directly (sinclair@ucalgary.ca), or by emailing ipm@innovatecalgary.com.
Funding
Funding was provided by the Health Quality Council of Alberta to Dr. Shane Sinclair, and Mr. Harrison Boss for the purposes of graduate training. The Health Quality Council of Alberta was responsible for the collection and management of data, review and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
H.B., C.M., and S.S. wrote the main manuscript text. R.S., J.J., and M.L. were responsible for the acquisition of the data. Data analysis was conducted by H.B. and C.M. Project funding was acquired by M.L., and S.S.. All authors were involved in the design of the work, interpretation of the data, and review of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved the Research Ethics Board (CHREB) at the University of Calgary (REB21-1938). In accordance with our REB approval, we were granted a waiver of consent for all participants, as gaining the contact information for these individuals through this administrative data was deemed not feasible. The dataset was obtained from the data custodians, the Health Quality Council of Alberta.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boss, H., MacInnis, C., Simon, R. et al. What role does compassion have on quality care ratings? A regression analysis and validation of the SCQ in emergency department patients. BMC Emerg Med 24, 124 (2024). https://doi.org/10.1186/s12873-024-01040-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-01040-8