Abstract
Background
The latest Surviving Sepsis Campaign 2021 recommends early antibiotics administration. However, Emergency Department (ED) overcrowding can delay sepsis management. This study aimed to determine the effect of ED overcrowding towards the management and outcome of sepsis patients presented to ED.
Methods
This was an observational study conducted among sepsis patients presented to ED of a tertiary university hospital from 18th January 2021 until 28th February 2021. ED overcrowding status was determined using the National Emergency Department Overcrowding Score (NEDOCS) scoring system. Sepsis patients were identified using Sequential Organ Failure Assessment (SOFA) scores and their door-to-antibiotic time (DTA) were recorded. Patient outcomes were hospital length of stay (LOS) and in-hospital mortality. Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 26. P-value of less than 0.05 for a two-sided test was considered statistically significant.
Results
Total of 170 patients were recruited. Among them, 33 patients presented with septic shock and only 15% (n = 5) received antibiotics within one hour. Of 137 sepsis patients without shock, 58.4% (n = 80) received antibiotics within three hours. We found no significant association between ED overcrowding with DTA time (p = 0.989) and LOS (p = 0.403). However, in-hospital mortality increased two times during overcrowded ED (95% CI 1–4; p = 0.041).
Conclusion
ED overcrowding has no significant impact on DTA and LOS which are crucial indicators of sepsis care quality but it increases overall mortality outcome. Further research is needed to explore other factors such as lack of resources, delay in initiating fluid resuscitation or vasopressor so as to improve sepsis patient care during ED overcrowding.
Similar content being viewed by others
Background
Emergency Department (ED) as the first patient encounter, plays a crucial role in the initial management of sepsis patients. To increase the rate of sepsis survival, emergency physicians aimed for early sepsis recognition, early fluid resuscitation, early appropriate antibiotics and source control [1]. The latest Surviving Sepsis Campaign guideline 2021 recommended antibiotic time within 1 h for patients with possible septic shock or high likelihood for sepsis. In cases where sepsis is possible but without hypotension or shock, rapid assessment of an etiology should be determined within 3 h. If concern for infection persists, antibiotics should be given within 3 h of sepsis recognition [2].
However, most EDs had failed to achieve the targeted time for antibiotics initiation. Studies show that ED overcrowding delays antibiotics initiation in sepsis patients with an increase of DTA time by 4 min for each 10% increase in ED occupancy [3,4,5,6].
ED overcrowding is defined as a situation where the demand for ED services exceeds the ability to provide service [7]. In Malaysia, there are 223 hospitals that provide ED service, but the number of patient visits has been increasing [8]. The escalating demand for ED services had surpassed the rate of ED expansion, hence causing ED overcrowding.
Research on ED overcrowding and DTA time in Malaysia is lacking, despite the extensive publications available from other regions [3, 4, 6, 9,10,11]. Hence, in this study, we aimed to determine the impact of ED overcrowding towards the DTA time in sepsis patients with LOS and in-hospital mortality as secondary outcomes in a tertiary hospital in Malaysia.
Method
Study design & setting
We conducted an observational study, from 18th January 2021 until 28th February 2021 in an 880-bed tertiary academic hospital, Hospital Canselor Tuanku Muhriz (HTCM), Universiti Kebangsaan Malaysia (UKM) in Kuala Lumpur, Malaysia. The annual ED attendance is around 70,000 visits with admission rate of 13% [12]. Sepsis patients account for about 10% of the hospital admissions according to our unpublished internal ED census.
This study was approved by the Medical Research Ethics Committee (MREC) Universiti Kebangsaan Malaysia (JEP-2020-634).
Selection of participant
The inclusion criteria were all patients above 18 years old who presented to the ED, diagnosed with sepsis and had received antibiotics in ED. The diagnosis of sepsis and septic shock were based on the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) [1]. Patients with sepsis were defined as patients presented with a source of infection and sustained organ dysfunction. Organ dysfunction is present when two or more criteria in Sequential Organ Failure Assessment (SOFA) were met. SOFA is a scoring system which requires laboratory testing to calculate the dysfunction level in six systems, namely respiratory, cardiovascular, coagulation, liver, renal and neurological systems [1, 13]. Meanwhile, septic shock was defined as patients with persistent hypotension despite adequate fluid resuscitation and requiring vasopressors to maintain MAP ≥ 65mmHg.
All patients presented to ED with probable infection and were prescribed and received antibiotics during this study period were identified and screened for eligibility. Patients who fulfilled the inclusion and exclusion criteria were recruited. A total of three patients who were discharged at their own risk, and four patients who did not receive antibiotics despite antibiotics being prescribed in ED had been excluded from our study.
Data collection and processing
The study included two parts of data collection, which ran concurrently. The first part involved determination of ED status, using the National ED Overcrowding Study (NEDOCS) scoring system. NEDOCS scoring system measured ED overcrowding using seven variables recorded at one point, which includes total number of patients in ED, number of ED beds, total number of admitted patients in the ED, number of hospital beds, waiting time from triage to ED bed placement for patients placed in ED beds, longest boarding time of patients waiting for admission and number of ventilators in use in ED [14]. Data were collected daily from three shifts at their peak time which were 11am, 6pm, and 11pm daily. Our rationale for this decision was based on the variability in patient acuity and staffing patterns that occur throughout the day, which may impact the delivery of care. By collecting data from three shifts, we aimed to capture a more comprehensive representation of the clinical environment. All data required for NEDOCS scoring were collected from ED bed manager’s census, patient’s case notes and direct observations by the researcher during the designated data collection times. These data were then entered into MedCalc for windows, version 5.2.5 to calculate the NEDOCS scoring of each respective shift.
The severity of ED overcrowding was graded into 6 levels, with level 1 (0–20) being not busy, level 2 (20–60) busy, level 3 (60–100) extremely busy but not overcrowded, level 4 (100–140) overcrowded, level 5 (140–180) severely overcrowded and level 6 (190–200) dangerously crowded. Level 1 to level 3 is grouped as non-overcrowded ED whereas level 4 to level 6 is grouped as overcrowded ED. A pilot study was performed from 30th November 2020 to 6th December 2020 to ensure the feasibility of utilizing NEDOCS in our setting. Throughout the seven days; consisting of 21 shifts; the NEDOCS score ranged from 2 to 6 (median score = 4).
The second part involved data collection of sepsis patients who received antibiotics in ED. During the study period, all patients presented to the ED with probable infection were identified. The treating team provided care to these patients according to standard protocols, and the management instituted were documented in their case notes. Relevant clinical and demographic data like age, gender, race, arrival time, DTA time, and SOFA score were collected during this process. Patients with SOFA score ≥ 2 and who had received antibiotics were recruited in the study. Following the admission of the patients, they were followed up and their LOS and in-hospital mortality were retrieved from the patient’s case note and hospital electronic system database. The NEDOCS score of the ED shifts during which the patients presented were compared and analysed.
The DTA time was measured as the difference between time of patient’s registration to first eligible antibiotic administered. The time was taken as per that recorded in the patient’s drug chart. Hospital LOS were counted from the first day of patient presentation to ED till discharge, where the data were collected from the hospital electronic system databases. In-hospital mortality was defined as patients who died during admission in hospital, in which data were collected from hospital electronic system database and patient’s medical records. The patient’s identifiers were coded and treated with the utmost discretion to maintain the patient’s confidentiality. All treatment and management of patients were under the discretion of the treating physicians as per department protocol.
Data analysis
The continuous variables were presented as mean ± SD (standard deviation), or median (Interquartile range (IQR)) for duration and clinical parameters, while categorical variables were expressed as frequencies and percentages. To compare sepsis patient presented during ED overcrowded and not overcrowded period, Pearson chi-square test was used for categorical variables like gender, race, ED triage zone, and in-hospital mortality. The Student T test was used for continuous variables with equal distribution like age, diastolic blood pressure, respiratory rate, temperature, GCS, SpO2 and SOFA score. To analyse continuous data variables with unequal distribution, like systolic blood pressure, heart rate, DTA time and length of stay, the Mann-Whitney U test was employed.
Mann-Whitney U test was also used to compare LOS between septic patients and sepsis patient without shock. To analyse in-hospital mortality, Pearson chi-square test was used; while Fisher’s Exact test was used when the data count was below five. Kruskal-Wallis Test was used to compare in-hospital mortality with hour upon hour DTA time among the sepsis patients.
All the tests were two-sided and p-values below 0.05 were regarded as statistically significant. Binary logistic regression is used to estimate the effect of ED overcrowding towards in-hospital mortality. Statistical analysis was carried out using Statistical Package for Social Science (SPSS Statistics 26.0, IBM Corp, Armonk, NY).
Results
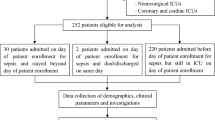
Data from 126 ED shifts were collected whereby 62 shifts (49.2%) were overcrowded (NEDOCS level 4–6) and 64 shifts (50.8%) were not overcrowded (NEDOCS level 1–3). The most crowded shifts occurred during night shifts (n = 65, 51.6%). Weekdays were more crowded compared to weekends (n = 109, 87.1%). In these 126 shifts, a total of 432 patients with probable infection had presented to ED, in which only 40% (N = 177) fulfilled SOFA criteria ≥ 2. The final recruitment were 170 patients with seven being excluded (Fig. 1).
Generally, the patients who presented with sepsis had a mean SOFA of 3 and were mostly elderly male. A total of 78 patients (45.9%) had presented during overcrowded ED and 92 patients (54.1%) had presented in a not overcrowded ED. There is no statistical difference in the clinical parameters of the patients between each group. The patients’ demographic and clinical parameters were as shown in Table 1.
DTA time and patient’s outcome according to ED overcrowding status
A total of 170 sepsis patients were recruited. Among them, 19.4% (n = 33) sepsis patients presented with shock and 80.6% (n = 137) patients presented without shock. Only 15.2% (n = 5) septic shock patients received antibiotics within 1 h and 58.4% (n = 80) sepsis patients without shock received antibiotics within 3 h (Fig. 1). The overall median DTA time was 144 min (IQR 27–677 min). There was no significant difference between DTA in overcrowded ED compared to not overcrowded ED [(median 143 min, IQR 32–677 min) vs. (median 150 min, IQR 27–553 min); p-= 0.989]. There was also no significant difference in DTA time when comparing NEDOCS across categories 1–6 as shown in Fig. 2 (p = 0.284). The LOS between these two groups were also not significantly different (p = 0.403) as described in Table 2.
The overall in-hospital mortality was 27% (n = 46) with a higher mortality during overcrowded ED compared to non-overcrowded ED (34.6% vs. 20.7%) as described in Table 2. Logistic regression analysis showed that overcrowded ED increased the in-hospital mortality by 2 times (95% CI 1–4; p = 0.041). There was no significant association between ED overcrowding and hospital LOS [(median 5 days, IQR 0–47 days) vs. (median 6 days, IQR 0–25 days); p = 0.403] as described in Table 2.
Further analysis of the 46 mortalities revealed septic shock group was associated with higher mortality compared to the sepsis without shock group (22.6%, n = 31 vs. 45.5%, n = 15; p = 0.008). There was no significant difference in the hospital LOS between these two groups (p = 0.152) as described in Table 3.
In the septic shock group, there was no significant difference seen between DTA time ≤ 1 h vs. > 1 h and patient’s outcome [in-hospital mortality (p = 0.591) and LOS (p = 0.673)]. Similarly, the in-hospital mortality (p = 0.230) or LOS (p = 0.380) in sepsis patient without shock also did not differ statistically between DTA time ≤ 3 h vs. DTA time > 3 h (Table 4).
The impact of hour-to-hour DTA time to in-hospital mortality
Figure 3 summarizes the total number of patients that survived or died according to hour upon hour DTA time. The mortality rate of sepsis patients who received antibiotics ≤ 1 h, > 1–2 h, > 2–3 h, >3 h are 21.1%, 29.8%, 30.6% and 25.0% respectively. In general, the mortality rate increased when DTA time was more than one hour, however it was not statistically significant (p = 0.827) as shown in Fig. 3.
The mortality rate of septic shock patients who received antibiotics ≤ 1 h, > 1–2 h, > 2–3 h, >3 h were 40.0%, 28.6%, 66.7% and 63.6% respectively. While the mortality rate for patient with sepsis without shock who received antibiotics ≤ 1 h, > 1–2 h, > 2–3 h, 3 h Were 14.3%, 30.3%, 27.3% and 17.5% respectively (Fig. 4).
Discussion
ED are designed to deliver time-sensitive interventions for critical illnesses, including sepsis which carries a significant mortality risk [15]. Hence, our study aimed to determine the impact of ED overcrowding towards the DTA time in sepsis patients with LOS and in-hospital mortality as secondary outcomes in a tertiary hospital in Malaysia. In our study, 15% septic shock patients received antibiotics within 1 h and 58.4% sepsis patients without shock received antibiotics within 3 h upon arrival in ED. These timings are notably longer in comparison to other advanced nations such as Korea, Japan and the UK where DTA time within 1 h was achieved in 28.6%, 30.5%, and 48.1% of cases, respectively [16,17,18]. As a teaching hospital, our ED patients were managed by different levels of doctors; junior doctors, emergency residents and emergency physicians therefore affecting the timings of antibiotics administration [19,20,21]. Additionally, lack of a standardized sepsis clinical pathway also contributed to the inconsistency in sepsis management, including antibiotics delivery [22,23,24,25,26].
Similar to previous studies done in Thailand and Korea, our study found that the delay in DTA time was not increased further despite ED overcrowding [27, 28]. This might be the result of our ED patient process flow. A systematic approach to all new patients has been enforced in our ED despite the patient occupancy level. In fact, the first doctor to patient contact time is one of the key performance indicators (KPI) of the department. Hence, regardless of the ED condition, all newly arrived sepsis patients will be assessed, investigated, and given the appropriate management such as administration of antibiotics.
The in-hospital mortality rate of 27% found in this study is comparable to other countries such as Korea 28% [29] and China 30% [30]. There was a higher mortality burden in patients with septic shock compared to those without shock and this finding was consistent with previous meta-analysis done [29, 31, 32]. Nonetheless, despite the delay in DTA time, we found no mortality benefit nor reduced hospital LOS in patients who received timely antibiotics. This finding is consistent with meta-analyses done previously, where no significant mortality benefit was found in DTA time within 1 h as compared to 3 h in patients with severe sepsis and septic shock [33, 34]. It is crucial to emphasize that extended delivery times for antibiotics do not necessarily result in poorer outcomes [34,35,36,37]. But this does not imply that timely administration of antibiotics is unnecessary. It’s important to approach the implementation of strict time frames with caution. Decisions regarding antibiotic administration should be guided by a comprehensive assessment of each patient’s clinical condition, the susceptibility patterns of the infecting microbes, and the institution’s antimicrobial stewardship policies [3, 38, 39]. Other aspects, such as the duration and volume of fluids administered, the collection of cultures, the types and timing of vasopressors treatments, can also potentially affect sepsis outcomes [37, 39, 40]. However, these factors were not explored in this study.
Although the overcrowded condition in our ED did not result in a significant delay in DTA time, there was two times increase in in-hospital mortality during periods of ED overcrowding. This finding highlights the importance of prompt sepsis management, which includes timely identification of sepsis, hemodynamic support, cultures acquisition, and appropriate antibiotics administration. Continuous monitoring of patients and dynamic reassessment of fluid responsiveness are crucial to prevent complications of fluid overload and reduce risk of mortality [41]. However, during times of ED overcrowding, this critical aspect of sepsis management tends to be overlooked, leading to increased mortality among sepsis patients [3, 42, 43].
Limitations and recommendations
This study was done in a tertiary teaching hospital with limited sample size. These results were generated from only one hospital and may not be generalizable to all hospitals. The sample size is relatively small especially in the septic shock group with DTA time ≤ 1 h, there were only 2 patients with in-hospital mortality. The small sample size may not accurately represent the outcome for sepsis patients in a larger population. Furthermore, this study may have missed sepsis cases that were not diagnosed during the patient’s stay in ED, resulting in delayed diagnoses that occurred later after the patients were admitted to the ward. We also did not look into other confounding factors that could affect the outcome of sepsis patients, such as the patient comorbidities, severity of sepsis, choice of antibiotic, the duration of antibiotics, and presence of positive cultures. Future studies may be done to explore these factors.
Additionally, our study only demonstrated that there was a delay in DTA, without establishing the exact cause. We recommend future studies to investigate factors that affect DTA time such as pharmacy delays, order processing time between nurses and physicians.
Conclusions
ED overcrowding is associated with an increase in in-hospital mortality for sepsis patient. However, ED overcrowding did not directly impact LOS and DTA time. Also, the DTA time itself does not affect the in-hospital mortality. This suggest that other factors in the sepsis management pathway may be more critical in determining mortality outcome for sepsis patients during ED overcrowding. Further research is necessary to identify these factors so as to improve survival rate in sepsis patients.
Data availability
Data that support the findings of this study have been deposited in the Harvard Dataverse and are available at the following URL: https://doi.org/10.7910/DVN/UNMHX5.
Abbreviations
- ED:
-
Emergency Department
- NEDOCS:
-
National Emergency Department Overcrowding Score
- SOFA:
-
Sequential Organ Failure Assessment
- DTA:
-
door-to-antibiotic
- LOS:
-
length of stay
- SCC:
-
Surviving Sepsis Campaign
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus definitions for Sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247.
Gaieski DF, Agarwal AK, Mikkelsen ME, Drumheller B, Sante SC, Shofer FS, et al. The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am J Emerg Med. 2017;35(7):953–60.
Ithan D, Peltan JR, Bledsoe TA, Oniki JS, Al R, Jephson TL, Allen, et al. Emergency Department crowding is Associated with delayed antibiotics for Sepsis. Ann Emerg Med. 2019;73(4):345–55.
Shin TG, Jo IJ, Choi DJ, Kang MJ, Jeon K, Suh GY, et al. The adverse effect of emergency department crowding on compliance with the resuscitation bundle in the management of severe sepsis and septic shock. Crit Care. 2013;17:1–11.
Darraj A, Hudays A, Hazazi A, Hobani A, Alghamdi A, editors. The association between emergency department overcrowding and delay in treatment: a systematic review. Healthcare: MDPI; 2023.
Ergin M, Demircan A, Keles A, Bildik F, Aras E, Maral I, et al. An overcrowding measurement study in the Adult Emergency Department of Gazi University Hospital, using the National Emergency Departments Overcrowding Study(Nedocs) Scale/Gazi Üniversitesi Hastanesi Eriskin Acil Servisinde Ulusal Acil Servisler Kalabalik Çalismasi (Nedocs) Skalasini Kullanarak Kalabalik Ölçüm Çalismasi. Eurasian J Emerg Med. 2011;10(2):60.
Arunah C, Teo A, Faizah A, Mahathar A, Tajuddin A, Khairi K. Emergency and trauma services in Malaysian hospitals. Natl Healthc Establishment Workforce Stat Kuala Lumpur 2010:73–86.
Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):501–9. e1.
Pines JM, Hollander JE, Localio AR, Metlay JP. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13(8):873–8.
Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):510–6.
Laporan Tahunan Hospital Canselor Tuanku Muhriz 2022 [Internet]. Hospital Canselor Tuanku, Muhriz UKM. 2022 [cited 26 January 2024]. Available from: https://hctm.ukm.my/wp-content/uploads/2024/01/bukulaporanPRINTFINAL.pdf.
Fethi Gül MKA. İsmail Cinel, Anand Kumar. Changing definitions of Sepsis. Turk J Aneaesthesiol Reanim. 2017;45:10.
Weiss SJ, Derlet R, Arndahl J, Ernst AA, Richards J, Fernández-Frankelton M, et al. Estimating the degree of emergency department overcrowding in academic medical centers: results of the national ED Overcrowding Study (NEDOCS). Acad Emerg Med. 2004;11(1):38–50.
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P et al. Assessment of global incidence and mortality of hospital-treated sepsis– current estimates and limitations. AJRCCM. 2015.
Ko BS, Choi S-H, Shin TG, Kim K, Jo YH, Ryoo SM, et al. Impact of 1-hour bundle achievement in septic shock. J Clin Med. 2021;10(3):527.
Leisman DE, Angel C, Schneider SM, D’Amore JA, D’Angelo JK, Doerfler ME. Sepsis presenting in hospitals versus emergency departments: demographic, resuscitation, and outcome patterns in a multicenter retrospective cohort. J Hosp Med. 2019;14(6):340–8.
Abe T, Kushimoto S, Tokuda Y, Phillips GS, Rhodes A, Sugiyama T, et al. Implementation of earlier antibiotic administration in patients with severe sepsis and septic shock in Japan: a descriptive analysis of a prospective observational study. Crit Care. 2019;23:1–11.
Kassyap C, Abraham SV, Krishnan SV, Palatty BU, Rajeev P. Factors affecting early treatment goals of sepsis patients presenting to the emergency department. Indian J Crit care Medicine: peer-reviewed Official Publication Indian Soc Crit Care Med. 2018;22(11):797.
Natsch S, Kullberg B, Van der Meer J, Meis J. Delay in administering the first dose of antibiotics in patients admitted to hospital with serious infections. Eur J Clin Microbiol Infect Dis. 1998;17(10):681–4.
Andre CKB, Amaral FRA, Pinto R, Rubenfeld GD, Ellis P, Bookatz B, et al. Patient and organizational factors Associated with delays in Antimicrobial Therapy for septic shock. Crit Care Med. 2016;44(12):2145–53.
Sungkar Y, Considine J, Hutchinson A. Implementation of guidelines for sepsis management in emergency departments: a systematic review. Australasian Emerg care. 2018;21(4):111–20.
Bader MZ, Obaid AT, Al-Khateb HM, Eldos YT, Elaya MM. Developing adult sepsis protocol to reduce the time to initial antibiotic dose and improve outcomes among patients with cancer in emergency department. Asia-Pacific J Oncol Nurs. 2020;7(4):355–60.
Walsh D, Gekle R, Bramante R, Decena E, Raio C, Levy D. Emergency department sepsis huddles: achieving excellence for sepsis benchmarks in New York State. Am J Emerg Med. 2020;38(2):222–4.
Shah T, Sterk E, Rech MA. Emergency department sepsis screening tool decreases time to antibiotics in patients with sepsis. Am J Emerg Med. 2018;36(10):1745–8.
Hayden GE, Tuuri RE, Scott R, Losek JD, Blackshaw AM, Schoenling AJ, et al. Triage sepsis alert and sepsis protocol lower times to fluids and antibiotics in the ED. Am J Emerg Med. 2016;34(1):1–9.
Jo S, Kim K, Lee JH, Rhee JE, Kim YJ, Suh GJ, et al. Emergency department crowding is associated with 28-day mortality in community-acquired pneumonia patients. J Infect. 2012;64(3):268–75.
Dadeh A-a, Pethyabarn W. Effects of Emergency Department Crowding and Time to Antibiotics in Pneumonia. J Med Assoc Thai. 2021;104(4).
Namgung M, Ahn C, Park Y, Kwak I-Y, Lee J, Won M. Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis. Clin Experimental Emerg Med. 2023;10(2):157.
Weng L, Xu Y, Yin P, Wang Y, Chen Y, Liu W, et al. National incidence and mortality of hospitalized sepsis in China. Crit Care. 2023;27(1):84.
Dupuis C, Bouadma L, Ruckly S, Perozziello A, Van-Gysel D, Mageau A, et al. Sepsis and septic shock in France: incidences, outcomes and costs of care. Ann Intensiv Care. 2020;10(1):1–9.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019—results from a systematic review and meta-analysis. Crit Care. 2020;24(1):1–9.
Rothrock SG, Cassidy DD, Barneck M, Schinkel M, Guetschow B, Myburgh C, et al. Outcome of immediate versus early antibiotics in severe sepsis and septic shock: a systematic review and meta-analysis. Ann Emerg Med. 2020;76(4):427–41.
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med. 2015;43(9):1907.
de Groot B, Ansems A, Gerling DH, Rijpsma D, van Amstel P, Linzel D, et al. The association between time to antibiotics and relevant clinical outcomes in emergency department patients with various stages of sepsis: a prospective multi-center study. Crit Care. 2015;19:1–12.
Seok H, Song J, Jeon J, Choi H, Choi W, Moon S, et al. Timing of antibiotics in septic patients: a prospective cohort study. Clin Microbiol Infect. 2020;26(11):1495–500.
Ryoo SM, Kim WY, Sohn CH, Seo DW, Oh BJ, Lim KS, et al. Prognostic value of timing of antibiotic administration in patients with septic shock treated with early quantitative resuscitation. Am J Med Sci. 2015;349(4):328–33.
Seok H, Jeon JH, Park DW. Antimicrobial therapy and antimicrobial stewardship in sepsis. Infect Chemother. 2020;52(1):19.
Levy MM, Evans LE, Rhodes A. The surviving Sepsis Campaign Bundle: 2018 update. Crit Care Med. 2018;46:4.
Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Horton JM, Studnek JR, et al. Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit Care Med. 2011;39(9):2066–71.
Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: Guideline-based management. Cleve Clin J Med. 2020;87(1):53–64.
Mahmoodi S, Faraji M, Shahjooie F, Azadpour A, Ghane MR, Javadzadeh HR, et al. Effect of Emergency Department crowding on patient mortality: a systematic review. Trauma Monthly. 2023;28(3):831–40.
af Ugglas B, Djärv T, Ljungman PL, Holzmann MJ. Emergency department crowding associated with increased 30-day mortality: a cohort study in Stockholm Region, Sweden, 2012 to 2016. J Am Coll Emerg Physicians Open. 2020;1(6):1312–9.
Acknowledgements
The abstract of this article had been presented in the 25th UKM Medical & Health research week in August 2023, and won the third prize in the oral poster presentation competition. The abstract is published in the year-end issue of Medicine and Health, a journal published by the Faculty of Medicine, Universiti Kebangsaan Malaysia. Some additional data has been added in this article. Otherwise, this original article is currently not under review nor has been previously published by other journals.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
EC, AA, IZ, DM: Conceived and designed the study, critical revision of the manuscript for important intellectual content. EC, AZ, SN: data collection and acquisition of data. EC, DM: drafted manuscript, performed statistical analysis and worked out technical details; all authors contributed substantially to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by our Institutional review board, Medical Research Ethics Committee (MREC) Universiti Kebangsaan Malaysia (JEP-2020-634). In view of the nature of the study, informed consent was waived by MREC.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chau, E.Y.W., Bakar, A.A., Zamhot, A.B. et al. An observational study on the impact of overcrowding towards door-to-antibiotic time among sepsis patients presented to emergency department of a tertiary academic hospital. BMC Emerg Med 24, 58 (2024). https://doi.org/10.1186/s12873-024-00973-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-00973-4