Abstract
Background
Access to emergency department (ED) services is important for patients with acute asthma; however, ED crowding may impact the quality of care and compromise outcomes. We examine the association between ED crowding metrics and individual patient outcomes for adults presenting with asthma.
Methods
This population-based retrospective cohort study extracted all ED presentations made by patients aged 18 to 55 years to 18 high-volume EDs in Alberta from April 2014 to March 2019. Physician initial assessment (PIA) time and ED length of stay (LOS) for discharged and admitted patients were calculated. Other metrics and patient outcomes were also obtained. Linear and generalized linear models were fit for continuous and categorical outcomes. Cox proportional hazards models were used for time-to-event outcomes.
Results
There were 17,724 ED presentations by 12,569 adults. The median age was 33 years, and females (58.7%) made more presentations. ED crowding affected the PIA time for all triage groups. For the high acuity group (Canadian Triage and Acuity Scale [CTAS] 1/2), 1 h increase in median facility-specific PIA was associated with 26 min (95%CI: 24,28) increase; for the moderate acuity (CTAS 3) and low acuity (CTAS 4/5) groups, the individual-level PIA increased by 54 min (95%CI: 53,55) and 61 min (95%CI: 59,63), respectively adjusted by other predictors. Increases in facility PIA resulted in increase in odds of admissions for the high acuity group and increase odds of left without completion of care for the moderate and low acuity groups.
Conclusion
The care provided for patients from all triage groups was impacted when EDs experienced crowding. Effective interventions are needed to mitigate ED crowding and improve care and outcomes for this important patient group.
Similar content being viewed by others
Background
Emergency department (ED) crowding is a longstanding concern for the healthcare system in major economies [1,2,3]. Crowding is a state where the demand for emergency care services exceeds the capacity for providers to deliver timely and high-quality care [1,2,3]. Studies focussed on ED crowding have documented delays in time-sensitive interventions, poor patient outcomes, increased patient departures without completion of care, patient and provider dissatisfaction, increased health care costs, and even higher mortality [4,5,6]. These results were directly attributed to ED crowding, especially when hospital capacity was reached, and the physician initial assessment (PIA) was delayed [7]. While ED-based, these studies involved general ED presentations, and it is unclear how crowding affects care and outcomes for specific conditions.
Asthma is a common disease in North America. The prevalence of asthma among adults [8] in the U.S. is approximately 15%, and Canada has similar statistics [9]. Exacerbations of asthma can be life-threatening and exert additional pressure on hospital capacity in the absence of timely and evidence-based care [10]. Moreover, nearly 25% of the total asthma costs are attributed to acute asthma treatment in North America [11, 12]. Importantly, there are time-sensitive interventions that impact outcomes and delays in management during periods of ED crowding could have impacts on outcomes for these patients.
The objective of this study is to examine the association between crowding metrics in EDs and outcomes in adult patients presenting with acute asthma in the province of Alberta, Canada.
Patients and methods
Study design
This retrospective cohort study extracted data from population-based databases of patients residing in Alberta, Canada. No funding organization had any role in the conduct and reporting of this study.
Study setting and population
All presentations acute asthma at the 18 highest-volume EDs during April 1, 2014, to March 31, 2019 were extracted for patients aged 18 to 55 years. The highest-volume EDs in Alberta were the focus for this project and were categorized into three groups: regional, urban, and academic/teaching.
Study protocol
There were 6 administrative patient databases used for the study. The National Ambulatory Care Reporting System (NACRS) database collects information on ED presentations. Linkages to other large health administrative databases were made to provide other information for analysis. The Annual Cumulative Registry File (CRF) provided demographic and geographic information; the Discharge Abstract Database (DAD) provided inpatient hospitalization data; the Physician Claim File (PCF) provided physician follow-up visits; and the Alberta Vital Statistics (VS) provided death records. Community size and neighbourhood income level were provided by Statistics Canada based on postal code.
The NACRS database provided the dates and times of ED presentations, triage level, physician initial assessment (PIA) diagnostic and intervention data, and disposition status. We defined the start of the ED presentation as the minimum date-time between the patient registration and triage. Fiscal year, month and year, weekday/weekend, and shift time were defined by the ED presentation date-time. The International Classification of Diseases (ICD-10-CA) [13] was used to define the asthma cases and the study population. Since asthma diagnoses for ages greater than 55 may be inaccurate and ED research has found that patients above 55 years of age frequently have COPD [14], this project only includes patients diagnosed with asthma between 18 and 55 years of age. Triage was determined based on the Canadian Triage and Acuity Scale (CTAS) used in most Canadian EDs, which is used to indicate the level of acuity and urgency for each ED presentation [15, 16]. There are five levels of triage with associated PIA targets: CTAS 1 (Resuscitation): immediate (= 0 min); CTAS 2 (Emergent): ≤15 min; CTAS 3 (Urgent): ≤ 30 min; CTAS 4 (Semi-urgent/less urgent): ≤ 60 min; CTAS 4 (Non-urgent): ≤ 120 min. Ten disposition codes represent the patient’s status at the end of each ED presentation, and were grouped into six disposition categories: discharged (i.e., discharged home, discharged from program or clinic), admitted to hospital (i.e., admitted to critical care or operating room, admitted to regular ward), transferred (i.e., to another acute care facility, to another non-acute care facility), death (i.e., on arrival or in the ED), and left without completion of care (left without being seen [LWBS] or left against medical advice [LAMA]).
The CRF database provided demographic and geographic information on individual patients. Age was defined as the age at the date of the ED presentation and calculated based on the patients’ birthdate. Patient sex was coded as male or female. Using the postal code of the patients’ residence at fiscal year-end, patients were geo-coded into one of the province’s five health zones (North, Edmonton, Central, Calgary, South). Community size and neighbourhood income quintile were identified by linking postal codes and the 2006 census data, the Postal Code Conversion File Plus [17].
The PCF database provided data on follow-up visits, including the physician’s specialty, if any. Physician specialists of interest were coded as respiratory medicine specialists or other specialists. DAD database provided the start and end date-time of each patient’s hospitalization. The ICD diagnostic codes were used to determine the Charlson Comorbidity Score [18] and comorbidity indicator variables.
Crowding metrics
Length of stay (LOS) and PIA time were calculated as ED crowding metrics [1] using data extracted from NACRS for patients presenting at any age for any condition (i.e., not restricted to adults or patients with asthma). For each ED presentation not ending in “left without completion of care”, the PIA time was defined as the difference between the presentation start time and the first physician assessment time. The first interaction for patients in Canadian EDs is with a nurse who performs triage. In the event that a patient is severe (CTAS 1 and some CTAS 2 cases), registration occurs after the PIA. Because, the PIA may occur before the reported ED start time in critical situations, negative values of PIA time were set as zero [19]. Each metric was calculated for each of the high volume ED facilities each hour within the same date during the study period. Hourly facility-specific ED crowding metrics (mean or median for skewed data) were calculated using all ED presentations within the same hour (e.g., 08:00–08:59) at the same facility. For each ED presentation, LOS was defined as the time from the start of ED presentation to the time of disposition; LOS for hospitalized patients and discharged patients were also calculated. Because the crowding metrics are continuous measures, they provide a measure of crowding on a continuum rather than classifying EDs into crowded or not crowded categories.
Key outcome measures
Outcome variables were derived or calculated based on the original variables of the data sources and were broadly classified as duration time variables and categorical outcome variables. Duration time variables measure delays that potentially affect patient outcomes and categorical outcome variables measure patient severity and status at the end of ED presentation. Some outcomes were only applicable to subsets of the ED presentation data (e.g., outcomes measure for admitted or discharged patients only). Emergency department LOS was defined as the difference between the presentation start time and end time. For admitted patients, the end time was defined as the time of departure from the ED to an in-patient unit. For discharged patients, the end time was defined as the time of disposition decision [19]. The length of hospital admission was calculated as the time from the start of the hospitalization to the time of discharge.
For discharged patients, the time to next follow-up visit with a physician was defined as the number of days between the ED presentation and the next physician visit. The time-to-event variable was censored if: (1) the patient died within 183 days (i.e., 6 months) after the ED presentation and there was no follow-up physician visit after the visit (data censored on the date of death); (2) follow-up physician visit did not occur within 183 days. The time to next follow-up visit with a respiratory medicine specialist, and time to next follow-up visit with other specialists, were defined similarly for discharged patients. The time to next ED presentation was censored at March 31, 2019 or death date during the study period. Corresponding censoring indicators were developed for all time-to-event outcomes.
Data analysis
Numerical summaries (e.g., means and standard deviations [SDs]; medians and interquartile ranges [IQR]) and frequency distributions (percentages) described ED presentations. For medians, IQRs represent the 25th percentile and 75th percentile. Three CTAS groups were collapsed from the triage levels: high acuity for CTAS 1/ 2, moderate acuity for CTAS 3, and low acuity for CTAS 4/5. Linear and Cox proportional hazards (PH) models were applied for duration time variables, including time-to-event variables with censoring indicators, and generalized linear models used for categorical outcome variables. Models were applied to assess the association between the ED crowding metric and the outcome variables by CTAS groups. Random effects accommodated the multiple correlated data from the same patient and variation in each ED facility.
Each crowding metric variable was included in both the model for unadjusted estimates and the full models for adjusted estimates to assess its effects on outcomes. Other predictors included in the full models were: age, sex, zone, weekday/weekend, month of year, shift, fiscal year, ED category, income level (lowest and second lowest neighbourhood income quintile vs. others), community size (population ≥ 100,000 vs. others), and selected comorbidities (i.e., mild/moderate/severe liver disease, diabetes mellitus, cancer or metastatic solid tumor, myocardial infarction, congestive heart failure, renal disease, peripheral vascular disease, stroke).
In addition, estimates, odds ratios (ORs), hazard ratios (HRs), and associated 95% confidence intervals (CIs) were provided. A p-value (p) less than 0.05 was considered to be statistically significant. Statistical analyses were conducted in R [20] and SAS [21].
Results
Demographics
There were 4,264,025 ED presentations made by adults for all conditions during the study period (Fig. 1); 17,724 (0.4%) presentations from 12,569 unique adult patients were made during the study period for acute asthma. There were 7 presentations deleted due to missing triage levels. The final dataset had 17,724 ED presentations (12,569 unique patients) for statistical analysis.
The median age was 33 years (IQR: 24.8, 42.5; Table 1), with more presentations made by females (58.7%). Approximately 60.6% of the presentations were from communities greater than 100,000 population, and 51.8% of presentations were made in the two main urban regions.
Main results
Patients presenting to the Edmonton zone had higher acuity than the other zones (Table 1). Overall, 52.9% (9,379) of the ED presentations had an urgent (CTAS 3) triage level. The resuscitation (CTAS 1) and emergency (CTAS 2) triage levels accounted for 1.6% (278) and 23.6% (4,190) presentations, respectively (Fig. 1). There were 3,480 (19.6%) semi-urgent presentations (CTAS 4) and 397 (2.2%) ED non-urgent (CTAS 5).
Percent of adult presentations with asthma and any condition by Canadian Triage and Acuity Scale (CTAS) groups. Dark gray indicates adult presentations with any condition and light gray indicates asthma presentations and. The numbers on top of the bars represent the count of presentations with asthma and all conditions by CTAS groups
Among all presentations, the vast majority (15,755, 88.9%) were discharged as expected. There were only three deaths that occurred for the high acuity group during the study period. Unsurprisingly, presentations that had less acute triage levels were less likely to be admitted. In the moderate and low acuity groups, 4.5% and 1.0% of the presentations were admitted, respectively, whereas 20.4% of presentations in the high acuity group were admitted.
The facility-specific hourly ED crowding metrics were calculated for all presentations of any condition. The median facility-specific PIA for all ED presentations was 1 h (hour) and 22 min (IQR: 48 min, 2h8min, Table S1).For adults presenting with acute asthma, the median facility-specific PIA was 1 h 6 min (IQR: 32, 124, Table 2). The high acuity group had shorter PIA (median = 36 min, IQR 18 min, 78 min) than other triage groups.
Among all 15,755 presentations ending in discharge, 7.6% (1,198) returned to the ED within 30 days; 34% (5,363) had a physician follow-up visit within seven days; 7.7% (1,207) had a respiratory medicine specialist follow-up visit within 30 days, and 5.6% (885) had a follow-up visit with other specialists within 30 days (Table 3).
For presentations ending in hospital admission (n = 1,376, Table 4) the median length of hospital stay was 3.0 days (IQR 1.8, 5.1). The median time from disposition decision to admission was 4 h 11 min (IQR 1 h 35 min, 13 h 33 min) and was, expectedly, longer for the high acuity group.
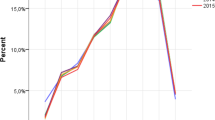
Individual-level PIA times for adults with asthma in all acuity groups increased as the median facility-specific PIA increased (Fig. 2, Table S2). For the high acuity group, a 1 h increase in median facility-specific PIA was associated with 26 min (95% CI: 24, 27) increase in individual-level PIA, adjusted by other predictors. For the moderate and low acuity groups, the individual-level PIA increased by 54 min (95% CI: 53, 55) and 61 min (95% CI: 59, 63), respectively, for every 1 h increase in median facility-specific PIA. Similarly, every 1 h increase in median facility-specific PIA was associated with 30 min (95% CI: 14, 47), 57 min (95% CI: 50, 63), and 52 min (95% CI 46, 58) increase in individual-level length of stay, for high, moderate and low acuity groups, respectively. For discharged patients, a 1 h increase in median facility-specific PIA, the individual LOS increased by 25, 53, and 54 min for the high, moderate, and low acuity groups, respectively. For the high acuity group, hospitalization was more likely with longer median facility-specific PIA (adjusted OR [aOR] = 1.13; 95% CI: 1.03, 1.23), adjusted by other predictors (Table S2). For the moderate acuity group, longer median facility-specific PIA was associated with a greater likelihood of leaving without completion of care (aOR = 1.48; 95% CI: 1.13, 1.95) and a lower likelihood of a return ED presentation within 30 days (aOR = 0.80, 95% CI: 0.67, 0.95).
Adjusted coefficient estimates (with 95% confidence intervals) for ED crowding metric time to physician initial assessment (PIA) for each continuous outcome and each Canadian Triage and Acuity Scale (CTAS) group. Numerical values are provided in Table S2. CTAS Canadian Triage and Acuity Scale, d days, ED emergency department, PIA physician initial assessment
When median hourly facility-specific LOS was used as a predictor, longer LOS was associated with a higher likelihood of admission in the high (aOR = 1.29; 95% CI: 1.23, 1.34) and moderate (aOR = 1.47; 95% CI: 1.31, 1.64) acuity groups (Table S3).
Discussion
This large, population-based administrative data study extracted all 17,724 ED presentations for acute asthma made by patients aged between 18 and 55 years to 18 high-volume EDs during a five-year period. We described the characteristics of patients and ED presentations and examined the association between the PIA time, ED crowding time metric and patient outcomes. We found that ED crowding affects care differently based on patient acuity. For example, ED crowding appeared to generate less impact on high acuity patients with acute asthma. The PIA and overall length of stay increased the least for these patients; however, delays were associated with a higher likelihood of admission.
Conversely, patients with moderate acuity presentations were affected most by ED crowding as the increase in facility specific PIAs resulted in increased individual PIAs, LOS for all ED presentations, LOS for discharged patients, and a higher proportion of patients requiring admission. These results suggest that delays in timely, evidence-based care have a negative impact on outcomes for patients with acute asthma of moderate severity. Early management of patients with acute asthma using systemic corticosteroids [22], inhaled short-acting anti-cholinergic agents [23], intravenous magnesium [24], and inhaled corticosteroids [25] in the ED have been shown to reduce hospitalization in systematic reviews. Moderate acuity group patients also tended to have less relapse back to the ED. This finding is not surprising since moderate and low acuity patients have less severe disease and lower risk of relapse.
We also found that the patients’ odds of left without completion of care also increased proportionally to delay in facility-specific PIA for the moderate acuity group. Leaving without completion of care is considered an indicator of ED crowding and poor quality of care [26]. While some research has found that adult patients who leave the ED without completion of care tend to be at a lower risk of admission within seven days than patients assessed by a physician and later discharged [4], such data include all ED presentations, not a time-sensitive condition such as asthma. The time to PIA is also strongly correlated with the number of patients who leave the ED without being assessed by a physician [27]. Clearly, LWBS and LAMA outcomes are potentially dangerous, and reducing these events is important for conditions like asthma, where with the risk of poor outcomes is higher.
Finally, patients with low acuity presentations reacted differently to increasing evidence of ED crowding. In these cases, patients already had a low risk of being admitted; however, with increasing crowding, these patients reacted by more often leaving prior to the completion of care. Since the effectiveness of within-ED care is transient, out-patient treatment following discharge with systemic and inhaled corticosteroids is critically important to reduce relapse and improve outcomes. Patients who elect to LAMA may be at risk of not receiving the evidence-based care required for safe transition back into the community.
Asthma is a chronic respiratory condition and exacerbations of acute asthma are common, especially in patients with poorly controlled disease. Exacerbations can be triggered by non-adherence to evidence-based care, as well as exposure to airways irritants (e.g., perfumes, cigarette smoke, chemicals), the environment (e.g., air pollution, smoke from wildfires, etc.), and upper respiratory tract infections. These irritants result in airway inflammation and bronchospasm that results in symptoms of cough, wheezing and shortness of breath, which when severe or when alternative care is unavailable (e.g., holidays, weekends, and off hours) may necessitate ED presentation. Fortunately, treatments are effective especially in the ED setting. For example, systemic corticosteroids as well as short-acting beta-agonists and anticholinergic agents are effective treatments to relieve symptoms and prevent admission. These evidence-based and guideline–directed treatments, however, must be delivered in a timely manner to prevent adverse outcomes. As this study has demonstrated, when ED crowding delays physician assessment, the administration of these treatments is also delayed. When crowding is present and cannot be avoided, innovative strategies (e.g., nurse- or respiratory therapist-initiated protocols, early administration of systemic corticosteroids, asthma teams, etc.) to expedite care may be warranted.
Notwithstanding the large sample, population-based data and robust data linkages, this study has several limitations. First, these administrative datasets do not include data about the treatments, prescriptions, and recommendations that each patient received in the ED. The number of patients referred to a specialist is also not available. Second, the databases do not contain other information about smoking status, body mass index, diet, exercise, sleep and other factors known to impact asthma control. Further, although asthma is more common in Indigenous Peoples (First Nations, Métis and Inuit) [28] and may be an indicator of outcomes in some conditions, for a variety of reasons membership in any of the Indigenous communities in Canada was not requested. Further research in this area is warranted. Third, the results may not be generalizable to other areas with different healthcare systems because the study only focused on EDs in Alberta, a Canadian province where no barriers to access health care exist. Fourth, this study did not include patients who seek care from other health services. The study population may not represent all adults with asthma. Finally, there was no confirmation of the diagnosis of asthma; however, by mixing asthma with other diagnosis (e.g., COPD, bronchitis) this would reduce the chance of identifying differences. Overall, we do not believe any of these limitations invalidate the results presented here.
Conclusions
Adult patients with acute asthma represent a small, albeit important, group of ED patients. While most patients experience excellent outcomes, some present with severe disease, and hospitalization occurs following 10% of presentations. Timely interventions exist to reduce hospitalization and improve outcomes; however, over the study period, these high volume EDs experienced periods of worsening crowding. When conditions deteriorate and delays increase, patients with acute asthma suffer unintended consequences. These EDs generally demonstrate flexibility to accommodate the most severe patients; however, during periods of crowding admissions increased, and low acuity patients often left prior to completion of care. Overall, general interventions designed to reduce ED crowding and efforts to deliver care in a timely manner to patients with acute asthma both appear warranted.
Availability of data and materials
Data is the property of Alberta Health and the authors are not allowed to provide the data. Requests can be made for the same data from Alberta Health for researchers who meet the criteria for access to confidential data. Researchers are welcome to inquire for further information at Health.RESDATA@gov.ab.ca.
Abbreviations
- aOR:
-
adjusted odds ratio
- CI:
-
confidence interval
- COPD:
-
chronic obstructive lung disease
- CRF:
-
Annual Cumulative Registry File
- CTAS:
-
Canadian Triage and Acuity Scale
- d:
-
day
- DAD:
-
Discharge Abstract Database
- ED:
-
emergency department
- h:
-
hour
- HR:
-
hazard ratio
- ICD:
-
The International Classification of Diseases
- IQR:
-
interquartile range
- LAMA:
-
left against medical advice
- LOS:
-
length of stay
- LWBS:
-
left without being seen
- min:
-
minute
- n:
-
count
- NACRS:
-
National Ambulatory Care Reporting System
- OR:
-
odds ratio
- PCF:
-
Physician Claim File
- PIA:
-
physician initial assessment
- VS:
-
Alberta Vital Statistics
References
Affleck A, Parks P, Drummond A, Rowe B, Ovens H. Emergency department overcrowding and access block. CJEM. 2013;15(6):59–37.
Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–80.
Pines J, Hollander J, Localio AR, Metlay J. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13(8):873–8.
Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983.
Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–6.
Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. Association between hospital overcrowding and mortality among patients admitted via western Australian emergency departments. Med J Aust. 2006;184:208–12.
Chalfin DB, Trzeciak S, Likourezos A. Impact of delayed transfer of critically ill patients form the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–83.
Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012;94:1–8.
Manfreda J, Becklake MR, Sears MR, Chan-Yeung M, Dimich-Ward H, Siersted HC, et al. Prevalence of asthma symptoms among adults aged 20–44 years in Canada. CMAJ. 2001;164:995–1001.
Camargo CA Jr, Rachelefsky G, Schatz M. Managing asthma exacerbations in the emergency department. Proceedings of the American Thoracic Society. 2009;6(4):357–66.
Krahn MD, Berka C, Langlois P, Detsky AS. Direct and indirect costs of asthma in Canada. CMAJ. 1996;154:821–31.
Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. NEJM. 1992;326:862–6.
Canadian Institute of Health Information. The Canadian enhancement of ICD-10 (International Statistical classification of Diseases and related health problems, Tenth Revision). Ottawa: Canadian Institute of Health Information; 2001.
Radeos MS, Cydulka RK, Rowe BH, Barr RG, Clark S, Camargo CA. Jr. Validation of self-reported chronic obstructive pulmonary disease among patients in the ED. Am J Emerg Med. 2009;27:191–6.
Bullard MJ, Unger B, Spence J, Grafstein E, CTAS National Working Group. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) adult guidelines. CJEM. 2008;10(2):136–51.
Gravel J, Manzano S, Arsenault M. Validity of the Canadian paediatric triage and acuity scale in a tertiary care hospital. CJEM. 2009;11(1):23–8.
Wilkins R, Peters PA. PCCF + version 5K* user’s guide. In: Automated Geographic Coding based on the Statistics Canada Postal Code Conversion Files, including Postal Codes through May 2011. Catalogue no. 82F0086-XDB ed. Ottawa: Health Statistics Division, Statistics Canada; 2012.
Olsson T, Terent A, Lind L. Charlson Comorbidity Index can add prognostic information to Rapid Emergency Medicine score as a predictor of long-term mortality. Eur J Emerg Med. 2005;12(5):220–4.
Canadian Institute for Health Information. eNACRS Reports: Emergency Department Wait Time Indicators. Ottawa, Ontario: Canadian Institute for Health Information; 2012.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018. http://www.r-project.org/.
SAS Institute Inc. SAS 9.4. Cary. NC: SAS Institute Inc.; 2014.
Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001(1):CD002178.
Kirkland SW, Vandenberghe C, Voaklander B, Nikel T, Campbell S, Rowe BH. Combined inhaled beta-agonist and anticholinergic agents for emergency management in adults with asthma. Cochrane Database Syst Rev. 2017;1(1):Cd001284.
Kew KM, Kirtchuk L, Michell CI. Intravenous magnesium sulfate for treating adults with acute asthma in the emergency department. Cochrane Database Syst Rev. 2014(5):CD010909.
Edmonds ML, Milan SJ, Camargo CA Jr, Pollack CV, Rowe BH. Early use of inhaled corticosteroids in the emergency department treatment of acute asthma. Cochrane Database Syst Rev. 2012;12(12):Cd002308.
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS ONE. 2018;13(8):e0203316-e.
Kyriacou DN, Ricketts V, Dyne PL, McCollough MD, Talan DA. A 5-Year time study analysis of emergency department patient care efficiency. Ann Emerg Med. 1999;34(3):326–35.
Ospina MB, Voaklander DC, Stickland MK, King M, Senthilselvan A, Rowe BH. Prevalence of asthma and chronic obstructive pulmonary disease in Aboriginal and non-aboriginal populations: a systematic review and meta-analysis of epidemiological studies. Can Respir J. 2012;19(6):355–60.
Acknowledgements
The authors thank Meng Lin of the Alberta SPOR data platform and AHS Research Data Services for providing health datasets. The authors also thank Larry Laliberte at the University of Alberta for providing the Statistics Canada data.
Funding
Dr. Rowe’s research is supported by a Scientific Director’s Grant (SOP 168483) from the Canadian Institutes of Health Research (CIHR). The funder was not involved in any aspect of the conduct, analysis, and manuscript preparation of this study and they take no responsibility for the conduct or results of this research. The funders had no role in the study design, data collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
YH cleaned data, performed modeling analysis, interpreted results, provided an initial draft of the manuscript, and critically reviewed and revised the manuscript for important intellectual content. SSO cleaned data, performed some statistical analyses, interpreted results, and critically reviewed and revised the manuscript for important intellectual content. BHR conceptualized and designed the study, searched the literature, provided clinical expertise in the modeling, interpreted, and critically reviewed and revised the manuscript for important intellectual content. R.J.R. conceptualized and designed the study, coordinated and supervised data extraction, directed statistical analyses, interpreted results, and critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Health Research Ethics Board of the University of Alberta (Pro00056282) approved this study. The need for Informed Consent was waived by the Health Research Ethics Board of the University of Alberta (Pro00056282) due to the retrospective nature of the study. Alberta Health Services, the data custodian, provided operational and administrative approval. A data sharing agreement governed data use and only de-identified data were shared. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Summaries of facility-specific hourlymetric median time to physician initial assessment and length of stay forpresentations for any condition and any age. Table S2. Regression estimates for linear models(beta coefs), odds ratios for logistic models (ORs), and hazard ratios for Coxproportional hazard models (HRs) with associated 95% confidence intervals (CIs)for Emergency Department (ED) crowding metric time to physician initialassessment (PIA) for each outcome and each Canadian Triage and Acuity Score(CTAS) group. Table S3. Regression estimates for linear models(beta coefs), odds ratios for logistic models (ORs), and hazard ratios for Coxproportional hazard models (HRs) with associated 95% confidence intervals (CIs)for Emergency Department (ED) crowding metric ED length of stay (LOS) for eachoutcome and each Canadian Triage and Acuity Score (CTAS) group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, Y., Ortiz, S.S., Rowe, B.H. et al. Emergency department crowding negatively influences outcomes for adults presenting with asthma: a population-based retrospective cohort study. BMC Emerg Med 22, 209 (2022). https://doi.org/10.1186/s12873-022-00766-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-022-00766-7