Abstract
Background
The shock index (SI) and its derivatives have been shown to predict mortality in severely injured patients, both in pre-hospital and in-hospital settings. However, the impact of the time of measurement on the discriminative ability of the pre-hospital SI is unknown. The aim of this study was to evaluate whether the time of measurement influences the discriminative ability of the SI multiplied by age (SIA) and divided by the Glasgow Coma Score (SIA/G).
Methods
Registry data were obtained from the national helicopter emergency medical services (HEMS) on trauma patients aged ≥ 18 years. The SI values were calculated based on the first measured vitals of the trauma patients by the HEMS unit. The discriminative ability of the SIA/G, with 30-day mortality as the endpoint, was evaluated according to different delay times (0 − 19, 20 − 39 and ≥ 40 min) from the initial incident. Sub-group analyses were performed for trauma patients without a traumatic brain injury (TBI), patients with an isolated TBI and patients with polytrauma, including a TBI.
Results
In total, 3,497 patients were included in the study. The SIA/G was higher in non-survivors (median 7.8 [interquartile range 4.7–12.3] vs. 2.4 [1.7–3.6], P < 0.001). The overall area under the receiver operator characteristic curve (AUROC) for the SIA/G was 0.87 (95% CI: 0.85–0.89). The AUROC for the SIA/G was similar in the short (0.88, 95% CI: 0.85–0.91), intermediate (0.86, 95% CI: 0.84–0.89) and long (0.86, 95% CI: 0.82–0.89) measurement delay groups. The findings were similar in the three trauma sub-groups.
Conclusions
The discriminative ability of the SIA/G in predicting 30-day mortality was not significantly affected by the measurement time of the index in the pre-hospital setting. The SIA/G is a simple and reliable tool for assessing the risk of mortality among severely injured patients in the pre-hospital setting.
Similar content being viewed by others
Background
Trauma is one of the leading causes of death and disability worldwide, with a considerable portion of the injured being young adults [1]. Therefore, it is vital to be able to identify critically ill, deteriorating patients to provide optimal early treatment. A simple instrument to evaluate mortality and facilitate resource allocation throughout the chain-of-treatment would be highly useful, particularly in the pre-hospital setting.
The shock index (SI), originally proposed by Allgöwer et al. in 1967, was developed as a simple tool for detection of circulatory collapse in haemodynamically unstable patients and has been shown to have predictive value in trauma patient mortality [2, 3]. The SI, which is determined by the heart rate divided by the systolic blood pressure (mmHg), has since been used in a variety of settings. A normal SI is categorized as 0.5–0.7, with an SI above 1 indicating uncompensated haemodynamic shock, which is accompanied by increased morbidity and mortality [3,4,5,6].
Several modifications of the SI have been proposed to increase its prognostic value. Earlier studies increased the predictive value of the SI by incorporating variables, such as age and the Glasgow Coma Score (GCS), into models [4] Further, the functionality of the SI has been assessed using a reverse SI (rSI), on the premise that clinicians typically view uncompensated circulatory shock as systolic blood pressure lower than the heart rate, not the other way around [7, 8]. A model incorporating both age and GCS into the SI, defined as the SI multiplied by age and divided by the GCS (SIA/G), has been shown to be more accurate than the SI, GCS or age alone, especially in elderly patients [3, 4].
Other potential variables affect the predictive value of the SI and its variations. In real life settings, for example, the delay in reaching a trauma patient varies greatly due to limitations in geography, infrastructure, and availability of resources. At present, the SI is considered a dynamic variable, with conflicting results, and the accuracy of the SI in identifying high-risk patients according to the time from an accident to the measurement of the SI remains unclear [5, 9, 10]. For appropriate use of the SI in decision making, including in trauma centres, this should be clarified.
The aim of this study was to evaluate whether the time of measurement of the SIA/G influences its discriminative ability in terms of 30-day mortality.
Methods
This was a retrospective cohort study combining data from national registries. The discriminative ability of the SIA/G was evaluated in trauma patients treated by the helicopter emergency medical services (HEMS) with different delay times from the incident. The study did not affect patient treatment and therefore patient consent was not required nor acquired. The Ethical Committee of Helsinki University Hospital approved the waiver for the need for informed consent due to only registry data was used. STROBE (The Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were followed in reporting of the study [11].
The study protocol was approved by the ethics committee of Helsinki University Hospital (HUS/3115/2019 §194). The hospital districts responsible for the HEMS (Oulu University Hospital: 200/2019 2.7.2019; Helsinki University Hospital: HUS/280/2019 9.7.2019; Turku University Hospital: J30/19 4.8.2019; the Hospital District of Lapland: 32/2019 22.8.2019; Kuopio University Hospital: RPL 102/2019 22.8.2019; and Tampere University Hospital: RTL-R19580 2.9.2019), Population Register Centre (VRK/5613/2019–3 1.11.2019) and Finnish institute for health and welfare (VRK/5613/2019–3 1.11.2019) responsible for the hospital discharge registry also approved the protocol. All methods used are in accordance with the Declaration of Helsinki.
Setting
The patients were treated by the national HEMS personnel. The HEMS consist of five units staffed by a physician and one unit staffed by a paramedic with specific training in pre-hospital critical care. The HEMS is part of public health care in Finland and free of charge for patients.
HEMS units are dispatched by emergency response centres in response to emergency calls. They are dispatched simultaneously with the emergency medical service (EMS) units based on pre-determined criteria to provide pre-hospital critical care and transport/escort patients directly to a tertiary hospital, if appropriate. HEMS units can also be dispatched on request from the EMS unit at a scene. Each HEMS mission is recorded in a national database by the physician or paramedic on call. The national HEMS and database have been described recently in detail [12].
Participants
We included all trauma patients over 18 years who were treated by the national HEMS from January 1, 2012 to December 31, 2018. Patients with a corrupt or missing personal identification code, as given by the Finnish Population Information System, were excluded, as this was used to identify and combine data from the registries.
Variables
The exposure studied was the SIA/G, and the primary outcome measurement was 30-day survival. The SI was calculated from the vital signs measured upon patient contact by the HEMS unit. SIA/G was calculated in our study as follows: ((HR/SBP) x Age) / GCS. The initial GCS as evaluated by the HEMS unit was incorporated into the SIA/G. The method of measuring vital signs was not controlled and included different defibrillator and monitoring devices used by EMS units. The SI was calculated from the vital signs measured upon patient contact by the HEMS unit. No serial or further SI measurements were done or analyzed during transport to or at the receiving hospital.
For evaluation of the effect of the delay time from the incident to the recording of the SIA/G on the discriminant ability of the index, the patients were divided into three groups according to the elapsed time between the emergency call and HEMS unit arrival on scene, I.E. first measurement of SI by a HEMS unit. The delay time was then divided into three groups: 0 − 19, 20 − 39 and ≥ 40 min.
The need for airway management during the pre-hospital phase was included in the analyses, as this has been shown to be strongly associated with subsequent mortality in this population [13]. In this study, tracheal intubation or the placement of a supraglottic airway device was considered advanced airway management.
ICD-10 based Injury Severity Scores (ICISS) were created using hospital discharge diagnoses [14].
Data sources
Data were combined from three registries: the national HEMS database, the national hospital discharge registry and the Population Information System. The national HEMS database has been used since the launch of the national HEMS system in 2012. The database includes the variables according to the international consensus-based recommendations on data collection in physician-staffed pre-hospital care and pre-hospital advanced airway management [15]. Data entry in the hospital discharge registry is mandatory for all hospitals in the country at the time of hospital admission. Hospital-related data included in the registry include data on the length of stay, diagnoses, and procedures.
The Population Information System includes data on Finnish citizens and foreign citizens who are residents in Finland. These data include the date of birth, place of residence and the time of death. In Finland, a personal identity code is automatically issued to each resident by the Finnish Population Information System. This code was used to identify and combine data from the different registries.
Sample size
No power calculation was performed, as all data available at the time of formation of the study dataset were included.
Statistical analysis
The distribution of the variables was tested using the D’agostino − Pearson omnibus normality test. As all the variables were non-normally distributed, non-parametric tests were used in comparisons, and the data were reported as medians (interquartile range). The discriminant ability of the SIA/G was evaluated by visualization of receiver operator characteristic curves (ROCs) and calculating the area under the ROC (AUROC), with 95% confidence intervals (95% CIs). Sub-groups of traumatic brain injury (TBI) patients were evaluated. The ROCs were compared using the following equation: \(Z=\frac{\left|{Area}_{1}-{Area}_{2}\right|}{\sqrt{{SE}_{Area1}^{2}+{SE}_{Area2}^{2}}}\). The two-tailed P values were consequently calculated from Z scores using Microsoft Excel. The TBI classification was based on the hospital discharge diagnosis. A TBI was classified according to an ICD-10 diagnosis of an intracranial injury. The patients were divided into three TBI subgroups: trauma without a TBI, an isolated TBI or polytrauma, including a TBI. A detailed list of the diagnoses is presented in Additional file 1: Appendix 1. The statistical analyses were performed using SPSS 27 (IBM Corporation, Armonk, NY, USA).
Results
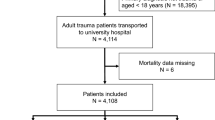
In total, 3,497 patients were included in the analyses (Fig. 1). Of these, 1,866 (51%) patients had a trauma without a TBI, 1,426 (43%) patients had an isolated TBI, and 205 (6%) patients had polytrauma, including a TBI. In terms of HEMS delay times, these were 0 − 19, 20 − 39 and ≥ 40 min in 1,402, 1,478 and 617 of cases, respectively. The characteristics of the patients are presented in Table 1. Mortality was higher and airway management more frequently performed in the patients with longer HEMS delay times (Table 2). In the study population, the crude 30-day mortality was 14.0% (488/3,497).
The SIA/G was 2.2 (1.5 − 3.1) in patients without a TBI, 3.9 (2.3 − 7.4) in patients with an isolated TBI and 3.6 (2.3 − 6.7) in polytrauma patients with a TBI. The SIA/G was significantly higher in patients that died within 30 days (7.8 [4.7 − 12.3] vs. 2.4 [1.7 − 3.6], P < 0.001).
The overall AUROC of the SIA/G for predicting 30-day mortality was 0.87 (95% CI: 0.85- 0.89). The AUROC in the patients without a TBI was 0.83 (95% CI: 0.78–0.88). It was 0.82 (95% CI: 0.80–0.85) in those with an isolated TBI and 0.84 (95% CI: 0.76–0.92) in multi-trauma patients with a TBI.
There was no discernible difference for the ROCs of the SIA/G for prediction of 30-day mortality between the groups with different time delays (Fig. 2). The AUROC CIs are presented in Fig. 3, showing no statistically significant difference between the delay groups. Additional file 2: Appendix 2 displays Z scores and P values for different patient groups.
A − D Area under the receiver operator characteristic curves (ROCs), with 95% confidence intervals (CIs) for the shock index multiplied by age and divided by the Glasgow Coma Score (SIA/G) in the prediction of 30-day mortality in trauma patients treated by the helicopter emergency medical services (HEMS) unit according to delays in SIA/G measurement times. The AUROC CIs presented in Fig. 3 show no statistically significant difference between the delay groups. Please refer to Additional file 3: Appendix 3 for numerical results
Discussion
This study demonstrated that the discriminative ability of the pre-hospital SIA/G was not affected by the time at which the index was first measured. To our knowledge, this is the first study to report the impact of the time of measurement on the utility of a pre-hospital age-adjusted SI incorporating the GCS. Furthermore, we found that the SIA/G was a good differentiator of severely injured patients with a high risk of death.
Critically injured trauma patients require a streamlined treatment protocol and advance preparation in the pre-hospital setting for the emergency department to ensure optimal treatment and resource allocation. The SI and its derivatives have been shown to be simple tools for predicting the need for the highest level of trauma-team activation, blood transfusions and mechanical ventilation and mortality in severely injured patients, with a single measurement in the in-hospital setting being predictive of mortality [3,4,5,6, 16,17,18,19]. The present findings on the SIA/G could be used to develop HEMS cancellation and secondary dispatch criteria.
To our knowledge, no previous studies have researched the impact of the pre-hospital time of measurement of the SIA/G on its discriminative ability regarding mortality. Overall, in our study, the discriminative ability of SIA/G regarding mortality remained unchanged, regardless of the time of the measurement. Previous studies where the SI was utilized as a dynamic variable reported somewhat contradictory results. According to these studies, an unchanged or increasing SI at the time of pre-hospital care in patients with a high baseline SI was associated with increased mortality [5, 9, 10]. The utilization of the SI as a dynamic variable makes sense, as it is straightforward, easy to comprehend and logical. A natural assumption might be that a longer delay to SI measurement would equate to an elevated SI, as more time has elapsed since the initial injury. However, this assumption did not hold true in our study. Thus, the dynamic nature of the SI seems to be limited. This finding is clearly in contrast to that of Nordin et al., who evaluated the paediatric age-adjusted SI as a dynamic variable from the pre-hospital setting to the emergency department and found significant association between the change of SI and outcome. However, in our study the time of measurement of the SIA/G was upon arrival of the HEMS unit. As such, the SI may be artificially enhanced by potential first-line, life-saving treatments provided by EMS units prior to HEMS arrival.
We found the discriminative ability of SIA/G regarding 30-day mortality in critically injured patients to be relatively high. Kimura et al. previously compared the discriminative ability of different variations of the SI and concluded that the SIA/G or rSIG/A is superior to the SI alone in trauma patients aged 55 years or older [4]. Earlier studies that integrated both age and the GCS into the SI reported that age is a major factor affecting mortality of severely injured trauma patients, with older age corresponding to higher mortality [5, 6]. Other studies demonstrated that the GCS, which has been widely adopted and readily describes the level of consciousness of a patient, is independently and strongly correlated with mortality among patients with a TBI [20, 21].
In the current study, the patients with the longest delay in measurement of the SI (≥ 40 min) had a lower GCS, more frequent advanced airway management and higher mortality. We found no difference in the incidence of TBI among the different time measurement delay groups, which would have conveniently explained the higher need for airway management and increased mortality in the group with the longest delay to SI measurement. A delayed time of arrival of a HEMS unit might indicate a longer distance, which, in turn, might lower the threshold for airway management. However, the differences in treatment and outcome of the patients between the delay groups are most likely explained by selection, as a HEMS mission can be cancelled by a HEMS physician if EMS personnel attending the scene report no need for interventions. In contrast, there might not be sufficient time to cancel a HEMS rescue mission if a HEMS unit arrives promptly at the scene.
The calculation of the original SI does not require complicated multiple variable inputs or difficult equations, making it a simple and useful tool in both pre-hospital and hospital settings. Although the addition of the GCS and age to the basic SI equation slightly increases the complexity of the calculation, its enhanced accuracy in predicting mortality is considerable when compared to the SI alone [4]. Furthermore, in an age of increasing automation and data-driven analytics, the incorporation of a mechanically calculated SI into EMS systems could provide a valuable tool in the pre-hospital setting. The potential benefits of an automatically calculated SI include the possibility of resource assessment based on the probability of mortality. In this way, EMS units might bypass a lower-level trauma centre and instead head directly to a level 1 trauma centre, thus reducing delays and unnecessary stopovers.
Strengths and limitations
The national HEMS registry constituted a considerable strength of the study, as it covers all HEMS missions in the country. However, the patient population consisted of critically injured patients treated by a single HEMS unit. Thus, the generalizability of the findings to the general pre-hospital patient population is somewhat limited. Further confounding factors that may have affected the accuracy of the study are related to the recording of the data in the registries. The actual times from injury occurrence to injury logging and emergency service dispatch may not be entirely accurate, as delays may have arisen in contacting emergency commination centre. In addition, chronic illnesses or potentially decreased functional ability that the patients may have had prior to their injuries were not considered. The determination of the three groups regarding time-of-delay was made based upon geographically realities, relatively short delay times and the presumption that adequate differences with regard to mortality would be found between the groups.
Conclusion
The discriminative ability of the SIA/G regarding 30-day mortality is not significantly affected by the time at which it is first measured during pre-hospital setting. The SIA/G is a simple and reliable tool for assessing the risk of 30-day mortality among severely injured patients in the pre-hospital setting.
Availability of data and materials
The dataset used and analysed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUROC:
-
Area under the receiver operator characteristic curve
- CIs:
-
Confidence intervals
- EMS:
-
Emergency medical services
- GCS:
-
Glasgow Coma Score
- HEMS:
-
Helicopter emergency medical services
- ROC:
-
Receiver operator characteristic curve
- rSI:
-
Reverse shock index
- SI:
-
Shock index
- SIA/G:
-
Shock index multiplied by age and divided by the GCS
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- TBI:
-
Traumatic brain injury
References
WHO Global Health Estimates. https://www.who.int/healthinfo/global_burden_disease/en/ . Accessed 22 Nov 2021.
Allgöwer M, Burri C. Shock index. Wochenschrift. 1967;27(92):1947–50.
Wan-Ting C, Chin-Hsien L, Cheng-Yu L, Cheng-Yu C, Chi-Chun L, Keng-Wei C, et al. Reverse shock index multiplied by Glasgow Coma Scale (rSIG) predicts mortality in severe trauma patients with head injury. Sci Rep. 2020;10(1):1–7.
Kimura A, Tanaka N. Reverse shock index multiplied by Glasgow Coma Scale score (rSIG) is a simple measure with high discriminant ability for mortality risk in trauma patients: An analysis of the Japan Trauma Data Bank. Crit Care. 2018;22(1):1–7.
McNab A, Burns B, Bhullar I, Chesire D, Kerwin A. An analysis of shock index as a correlate for outcomes in trauma by age group. Surg (United States). 2013;154(2):384–7.
Bruijns SR, Guly HR, Bouamra O, Lecky F, Lee WA. The value of traditional vital signs, shock index, and age-based markers in predicting trauma mortality. J Trauma Acute Care Surg. 2013;74(6):1432–7.
Kuo SCH, Kuo PJ, Hsu SY, Rau CS, Chen YC, Hsieh HY, et al. The use of the reverse shock index to identify high-risk trauma patients in addition to the criteria for trauma team activation: A cross-sectional study based on a trauma registry system. BMJ Open. 2016;6(6):e011072.
Chuang JF, Rau CS, Wu SC, Liu HT, Hsu SY, Hsieh HY, et al. Use of the reverse shock index for identifying high-risk patients in a five-level triage system. Scand J Trauma Resusc Emerg Med. 2016;24(1):1–10.
Nordin A, Shi J, Wheeler K, Xiang H, Kenney B. Age-adjusted shock index: From injury to arrival. J Pediatr Surg. 2019;54(5):984–8. https://doi.org/10.1016/j.jpedsurg.2019.01.049 Available from.
Marenco CW, Lammers DT, Do WS, Morte KR, Horton JD, Eckert MJ. Dynamic trend or static variable: Shock Index Pediatric-Adjusted (SIPA) in warzone trauma. J Pediatr Surg. 2021;56(2):405–11.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Saviluoto A, Björkman J, Olkinuora A, Virkkunen I, Kirves H, Setälä P, et al. The first seven years of nationally organized helicopter emergency medical services in Finland - the data from quality registry. Scand J Trauma Resusc Emerg Med. 2020;28(1):46.
Björkman J, Laukkanen-Nevala P, Olkinuora A, Pulkkinen I, Nurmi J. Short-term and long-term survival in critical patients treated by helicopter emergency medical services in Finland: a registry study of 36 715 patients. BMJ Open. 2021;11(2):e045642.
Gedeborg R, Warner M, Chen LH, Gulliver P, Cryer C, Robitaille Y, et al. Internationally comparable diagnosis-specific survival probabilities for calculation of the ICD-10-based injury severity score. J Trauma Acute Care Surg. 2014;76(2):358–65.
K Tønsager M Rehn KG Ringdal HM Lossius I Virkkunen Ø Østerås et al 2019 Collecting core data in physician-staffed pre-hospital helicopter emergency medical services using a consensus-based template: international multicentre feasibility study in Finland and Norway BMC Health Serv Res. 19 1 151 http://www.ncbi.nlm.nih.gov/pubmed/30849977. [Cited 14 Mar 2019]. Available from
Jehan F, Con J, McIntyre M, Khan M, Azim A, Prabhakaran K, et al. Pre-hospital shock index correlates with transfusion, resource utilization and mortality; the role of patient first vitals. Am J Surg. 2019;218(6):1169–74.
Lee YT, Bae BK, Cho YM, Park SC, Jeon CH, Huh U, et al. Reverse shock index multiplied by Glasgow coma scale as a predictor of massive transfusion in trauma. Am J Emerg Med. 2020;46:404–9.
Wang IJ, Bae BK, Park SW, Cho YM, Lee DS, Min MK, et al. Pre-hospital modified shock index for prediction of massive transfusion and mortality in trauma patients. Am J Emerg Med. 2019;38(2):187–90.
Lammers DT, Marenco CW, Do WS, Conner JR, Horton JD, Martin MJ, et al. Pediatric adjusted reverse shock index multiplied by Glasgow Coma Scale as a prospective predictor for mortality in pediatric trauma. J Trauma Acute Care Surg. 2021;90(1):21–6.
Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: Standing the test of time. Lancet Neurol. 2014;8:844–54.
Majdan M, Steyerberg EW, Nieboer D, Mauritz W, Rusnak M, Lingsma HF. Glasgow coma scale motor score and pupillary reaction to predict six-month mortality in patients with traumatic brain injury: Comparison of field and admission assessment. J Neurotrauma. 2015;32(2):101–8.
Acknowledgements
Not applicable.
Funding
This study was supported by Helsinki University Hospital (state funding, VTR TYH2019243) and FinnHEMS Research and Development Unit.
Author information
Authors and Affiliations
Contributions
ML formulated the study concept, analyzed and interpreted the data collected, contributed to the study design and was a contributor to both the writing process and manuscript preparation. JB devised the study, contributed to the study design, performed the statistical analysis, analysed the data and contributed to the writing process. TI developed the research plan, analyzed the data and contributed to the study design and writing of the manuscript. LR contributed to the study design, data processing and editing of the manuscript. JN devised the study, coordinated the workflow, and contributed to the study design and writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study did not affect patient treatment and therefore patient consent was not required nor acquired. The Ethical Committee of Helsinki University Hospital approved the waiver for the need for informed consent due to only registry data was used. The study protocol was approved by the ethics committee of Helsinki University Hospital (HUS/3115/2019 §194). The hospital districts with responsibility for the HEMS (Oulu University Hospital: 200/2019 2.7.2019; Helsinki University Hospital: HUS/280/2019 9.7.2019; Turku University Hospital: J30/19 4.8.2019; the Hospital District of Lapland: 32/2019 22.8.2019; Kuopio University Hospital: RPL 102/2019 22.8.2019; and Tampere University Hospital: RTL-R19580 2.9.2019), Population Register Centre (VRK/5613/2019–3 1.11.2019) and Finnish Institute for Health and Welfare (VRK/5613/2019–3 1.11.2019) responsible for the hospital discharge registry also approved the protocol. All methods used in the study have been performed in accordance with good ethical principles (Declaration of Helsinki). The study did not affect patient treatment and therefore patient consent was not required nor acquired.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Laaksonen, M., Björkman, J., Iirola, T. et al. The effect of time of measurement on the discriminant ability for mortality in trauma of a pre-hospital shock index multiplied by age and divided by the Glasgow Coma Score: a registry study. BMC Emerg Med 22, 189 (2022). https://doi.org/10.1186/s12873-022-00749-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-022-00749-8