Abstract
Objective
Maternal cardiac arrest is a rare and complex process requiring pregnancy-specific responses and techniques. The goals of this study were to (1) identify, evaluate, and determine the most current best practices to treat this patient population and (2) establish a standardized set of guidelines to serve as a foundation for a future educational simulation-based curriculum.
Study design
We used a three-step modified Delphi process to achieve consensus. Twenty-two healthcare experts from across North America agreed to participate in the expert panel. In round 1, 12 pregnancy-specific best practice statements were distributed to the expert panel. Panelists anonymously ranked these using a 7-point Likert scale and provided feedback. Round 2 consisted of a face-to-face consensus meeting where statements that had not already achieved consensus were discussed and then subsequently voted upon by the panelists.
Results
Through two rounds, we achieved consensus on nine evidence-based pregnancy-specific techniques to optimize response to maternal cardiac arrest. Round one resulted in one of the 12 best practice statements achieving consensus. Round two resulted in six of the remaining 12 gaining consensus. Best practice techniques involved use of point-of care ultrasound, resuscitative cesarean delivery, cardiopulmonary resuscitation techniques, and the use of extracorporeal cardiopulmonary resuscitation.
Conclusion
The results of this study provide the foundation to develop an optimal, long-term strategy to treat cardiac arrest in pregnancy. We propose these nine priorities for standard practice, curricula, and guidelines to treat maternal cardiac arrest and hope they serve as a foundation for a future educational curriculum.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Maternal cardiac arrest
Maternal cardiac arrest (MCA) is the final common pathway for many critical illnesses and comorbidities, however, anatomic and physiologic changes specific to pregnancy and the presence of a fetus create a very different situation as compared to non-pregnant patients. Therefore, pregnant patients who suffer cardiac arrest require a modified and multidisciplinary approach to maximize their survival and ensure optimal outcomes for the fetus. Rates of maternal mortality in the United States are increasing [1], and too many women are dying from pregnancy-related complications [2]. Research suggests that 60 % of these deaths are preventable [3], affording a meaningful opportunity to address these devastating outcomes.
Collectively, cardiovascular conditions, cardiomyopathy, and stroke accounted for more than 30% of pregnancy-related deaths from 2011 to 2016 [4]. Although cardiac arrest during delivery is rare [5], the incidence of this clinically challenging scenario may be increasing [4, 6, 7].
In 2015 the American Heart Association (AHA) published its first scientific statement on MCA [3]. However, despite the AHA’s rigorous scientific processes and dissemination, practitioners have not widely implemented these care modifications. In fact, several studies have shown that multidisciplinary teams often completely miss or incorrectly perform multiple key steps to successful MCA resuscitation [8, 9]. The 2015 AHA guidelines did not address extracorporeal cardiopulmonary resuscitation (ECPR) or point of care ultrasound (POC-US) within the setting of MCA. It also refers to the potentially life-saving measure of MCA resuscitation as “perimortem cesarean delivery,” which was originally described as a procedure to perform to save the fetus in the dying mother [10].
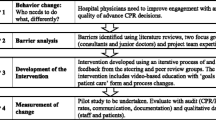
Recognizing this practical deficit, the core investigators (A.S, J.B, B.T, P.N.) identified critical gaps in treatment since the publication of the AHA statement, developed a consensus on treatment priorities, and created a foundation for a future simulation-based curriculum to train providers to treat maternal cardiac arrest successfully. The AHA have subsequently updated their guidelines in 2020, and ILCOR updated their guidelines in 2021. While the AHA guidelines do specifically address MCA resuscitation, ILCOR did not. Table 1 highlights several key similarities and differences between the 2020 AHA and 2022 OBLS guidelines.
Modified Delphi method [11]
The modified Delphi method relies on group consensus to increase content validity in the setting of limited data. An iterative process, it combines an initial literature review with repeated rounds of voting by stakeholders to achieve group consensus. Incorporating a RAND (Research and Development)/UCLA (University of California- Los Angeles) Appropriateness Method (RAM) also includes face-to-face discussion, which is lacking from the traditional Delphi method. First, stakeholders identify the problem and perform a literature search. A questionnaire of best practices is developed and sent to experts in the field, who then anonymously score the best practices based on importance and relevance for inclusion into the desired guidelines. Experts are defined as 20–40 individuals from diverse geographic regions and with subject area knowledge [12]. Stakeholder responses are tallied after each round. The process is then repeated in a moderated, face-to-face meeting during which the panel discusses items that have not yet reached consensus. The RAM method also allows for modification of the technique in question to attempt to gain consensus during this discussion. Upon completion of discussion, panelists again rate the remaining items. Consensus is achieved if mean scores cross a certain threshold, which is determined by the researchers.
Methods
We conducted a three-step modified Delphi process between November 2018–February 2019, consisting of a methodological assessment, a rating evaluation, and a face-to-face consensus meeting. We received approval from the Institutional Review Board for Baylor College of Medicine and Affiliated Hospitals (Protocol Number: H-43780). Given the study was minimal risk, informed consent was not required.
We contacted specialists in) the prehospital arena (paramedics, flight nursing, and EMS medical director), anesthesia, emergency medicine, obstetrics/gynecology, maternal-fetal-medicine, family medicine, neonatology, pulmonary critical care, nursing, certified nurse midwifery and cardiology. We invited subject matter experts in these fields as we felt these fields were most likely to come into contact with a patient in MCA. We invited them to join the panel based on their leadership positions on national committees/panels, or publications in related subject matter. Of the 25 experts invited; 22 individuals agreed to serve as panelists. Of those, almost half are women (42%), nearly half actively treat pregnant patients (46%), nearly a fifth represent those who provide out-of-hospital care (19%), and more than half (54%) represent in-hospital sectors.
We first established a baseline of the current evidence-based techniques used to resuscitate pregnant patients in cardiac arrest. Using a web-based assessment tool, 10 of the 12 invited experts and four of the clinician-investigators assessed the methodological quality of the AHA statement (AGREE II; 2010–2014, Hamilton, ON, Canada). Using a seven-point Likert scale, they assessed six quality domains of the AHA statement: scope and purpose; stakeholder involvement; rigor of development; clarity of presentation; applicability; and editorial independence (scale rankings one = strongly disagree to seven = strongly agree).
After reviewing the literature, internal investigator assessments, and expert assessment of the AHA statement, we developed and assigned a class of recommendation and level of evidence [13] to 12 pregnancy-specific resuscitation techniques for expert consideration. We categorized these into four themes: (1) resuscitative cesarean delivery, (2) point-of-care ultrasound, (3) extracorporeal cardiopulmonary resuscitation, and (4) targeted temperature management. We then performed two modified Delphi rounds to gain consensus on relevant pregnancy-specific technique statements.
Round 1
First, the four investigators and 19 of the invited 22 experts used a seven-point Likert scale to rank the 12 technique statements through a secure, web-based data collection software (REDCap at Baylor College of Medicine) (Tables 2, 3 and 4). Investigators brought those that met the a priori consensus threshold to the face-to-face consensus meeting for facilitated discussion. An a priori determination of consensus to support the recommendation included an average score of 5.0 or greater; if any key question had a score of 1 “dangerous or inappropriate” it was automatically reviewed in round two. We calculated an average ranking score for each statement and incorporated reviewer comments for statement modifications.
Round 2
We held the face-to-face meeting on January 31–February 1, 2019. All 22 of the invited experts attended. We presented the individual statements and a summary of supporting evidence and facilitated a discussion to solicit perspectives. Our flexible agenda allowed for discussion and questions that followed. When differences resulted from the specific wording of the pregnancy-specific technique statements, we discussed, revised, and agreed on the rewording. Participants discussed all statements again, giving experts a chance to reconsider their earlier rating considering their colleagues’ views. We made all revisions and then provided participants with an online anonymous audience response system (Poll Everywhere, San Francisco, CA). Experts ranked the statements using a six-point Likert scale and answered, “Should this statement be incorporated into a future curriculum?” To be considered for affirmation and inclusion into the curriculum, an a priori result of 4.0 or greater, and > 80% consensus was set. A pre and post T-test was performed for each statement to determine the effect of face-to-face consensus discussion on change in ranking.
Affirmation
Techniques that met preset criteria advanced to final affirmation. Via REDCap, participants individually and anonymously voted to include the pregnancy-specific resuscitation technique in the final overall curriculum priorities.
Results
Assessment of the AHA statement
Rating the acceptability, usability, and feasibility of the AHA statement, experts scored stakeholder involvement level low (58%) and clarity of presentation high (90%). They ranked the other four domains (scope and purpose, rigor of development, applicability, and editorial independence) greater than 72%. Reviewer comments for suggested modifications were collected and summarized into several common themes listed in Table 5.
Modified RAM Delphi method
After the first round of consensus, only one statement met the predefined rank (> 5). While the remainder of the statements had a “high” (> 4) or “moderate” (> 3) level of consensus, they did not meet the threshold rank (Table 6).
Following the second round, nine of the 11 techniques met the predetermined rank for affirmation (> 4). Following participant discussion, experts scored three of these lower than they had in the first round. Investigators removed these methods from further consideration.
Discussion
We obtained consensus among a diverse stakeholder group of experts regarding the most current evidence-based techniques to treat maternal cardiac arrest successfully. Experts agreed on themes related to resuscitative cesarean delivery, point-of-care ultrasound, extracorporeal cardiopulmonary resuscitation, and targeted temperature management. We hope that clinicians will incorporate these critical techniques to treat maternal cardiac arrest into future simulation-based education. (Table 7).
The study’s strengths include a robust literature search and rigorous process to generate an initial set of relevant, pregnancy-specific resuscitation techniques. Additionally, this systematic and thorough process brought together a multidisciplinary panel of experts representing out-of- and in-hospital settings in all North America regions. We believe this is the most diverse group of experts that has gathered around this specific topic area.
Limitations include our directing experts to select “0” if they did not feel qualified to rank a statement. They may have answered a question instead of selecting “0”, introducing bias.
Our decision to use anonymous voting was to limit bias. However, because we chose not to link answers to specific individuals, we were unable to calculate analytic statistics of individual member responses during the consensus rounds. Although we chose experts to represent diverse expertise and backgrounds, they may not adequately represent the full spectrum of views.
One other possible limitation is the rare nature of the topic of MCA. While best practice statements were based on a robust literature search it was primarily low-level evidence papers, which included multiple case reports and studies.. Future metrics to determine the validity of the best practices will also most likely rely heavily on simulation data due to the overall low volume of MCA. Low volume aside, there is still great benefit to assembling these best practices, as research has also shown significantly improved maternal response to resuscitation in MCA, particularly when they are applied promptly and aggressively.
Conclusions
The results of this study provide the foundation to develop an optimal, long-term strategy to treat cardiac arrest in pregnancy through simulation-based training. We propose these nine priorities for standard practice, curricula, and guidelines to treat maternal cardiac arrest and hope they serve as a foundation for a future educational curriculum.
Supplement
Resuscitative cesarean delivery (formerly Perimortem cesarean delivery)
-
1.
Use the term ‘resuscitative cesarean (or vaginal) delivery’ (RCD) instead of ‘perimortem cesarean delivery’ to more correctly describe the purpose/indication and increase the timeliness and sense of urgency for performing this procedure (Class I; Level of Evidence C).
Perimortem cesarean delivery was originally used to describe the last-ditch effort to save the fetus in a dying pregnant patient. However, we now understand that the technique to rapidly evacuate uterine contents may actually improve maternal resuscitation efforts by increasing cardiac output through the reduction of aortocaval compression and the resultant autotransfusion from the decompressed uterus [14,15,16]. As it incorporates delivery of the fetus and placenta, “resuscitative cesarean delivery” (RCD) is a more accurate description of the procedure, making it instantly recognizable to non-obstetric staff who may be assisting in the resuscitation. It reflects the mutual optimization of resuscitation efforts that would potentially provide earlier and more substantial benefit to both the pregnant woman and fetus.
-
2.
Perform an RCD immediately in a pregnant patient with a fundal height at or above the umbilicus with a non-shockable rhythm (Class IIb; Level of Evidence C).
Delivery of the fetus early in a maternal cardiac arrest following the absence of ROSC results in a high probability of ROSC in the pregnant patient, more than 50% in some studies, by improving maternal cardiac output through the reduction of aortocaval compression, and the resultant autotransfusion from the decompressed uterus [14, 15]. A recent study of 462 women with maternal cardiac arrest found that only 11.2% presented with a shockable rhythm [16, 17]. This highlights the need for simultaneous RCD preparations with ongoing cardiopulmonary resuscitation (CPR) efforts, and immediate performance of an RCD if the maternal cardiac rhythm is non-shockable and the uterus is at or above the umbilicus, regardless of gestational age or the presence of fetal cardiac activity.
-
3.
Train providers staffing EDs in RCD (Class IIb; Level of Evidence C)
Inherent in our recommendations is the recognition that medical professionals staffing emergency departments and hospitals who do not provide obstetric care need to have the capability to perform a resuscitative cesarean delivery to improve maternal survival within the 5 min window from arrest (if in-hospital) or at the time of admission to the Emergency Department if the maternal cardiac arrest occurred out-of-hospital. It is imperative that physicians in all fields that staff emergency departments learn the proper techniques of resuscitative cesarean delivery through proctored clinical experience and maintain clinical competency via simulation [18,19,20].
Extracorporeal cardiopulmonary resuscitation
Recommendations
-
1.
Consider ECPR to manage maternal cardiac arrest when there is no ROSC after RCD or for refractory CPR where the uterus has not yet reached the umbilicus and the patient is in an extracorporeal membrane oxygenation center with the capacity to care for critically ill pregnant patients (Class IIa; Level of Evidence C).
Extracorporeal cardiopulmonary resuscitation (ECPR) has emerged as a beneficial intervention when sustained ROSC is not achieved. ECPR maintains organ perfusion while the underlying etiology of the cardiac arrest is determined and treated. As of 2018, we identified 36 cases of ECPR use in maternal cardiac arrest, with many cases resulting in maternal survival [18, 19, 18,19,21,22,23]. ECPR has been used for a variety of etiologies in maternal cardiac arrest including massive pulmonary embolism, severe cardiomyopathy/cardiac disease, amniotic fluid embolism, sepsis, and postpartum hemorrhage in which CPR failed to result in sustained ROSC [19, 24,25,26,27,28]. Although ECPR has been applied at a variety of gestational ages, it is generally applied after RCD in the second half of pregnancy [24]. When ECPR has been applied in the setting of maternal cardiac arrest without ROSC, survival rates to discharge have been reported as high as 77% of women and 67% of fetuses [21]. These rates compare very favorably to a recently published overall maternal survival rate to discharge of 40.7% after cardiac arrest [17].
-
2.
Consider ECPR for organ procurement in pregnant patients, post-arrest with circulatory determination of death (Class IIb; Level of Evidence C).
If a pregnant woman is unsuccessfully resuscitated, ECPR has been shown to be effective for the procurement of organs in the circulatory determination of death [29, 30]. Reproductive-age women who have maternal cardiac arrest with unsuccessful CPR are generally younger and in better health, making them ideal candidates for organ procurement. Moreover, the results of some studies have highlighted the favorable impact of organ donation on the reduction of sorrow from the loss of a loved one, and the concept that “live organs in recipients’ body somehow reflect immortality.” [31, 32].
-
3.
Report all pregnant women who receive ECPR in the setting of maternal cardiac arrest, regardless of outcome, in the Extracorporeal Life Support Organization (ELSO) registry (https://www.elso.org/Registry.aspx) (Class IIb, Level of Evidence C).
Future directions on the application of ECPR for refractory CPR in pregnant patients and the refinements to the use of ECPR in this population will depend on registry reporting and continued re-evaluation of observational trials and case reports or series.
Point of care ultrasound
Recommendations
-
1.
Where available, POC-US should be used in the management of maternal cardiac arrest for identification of an intrauterine pregnancy and quick determination of gestational age to guide decision making on RCD (Class IIa; Level of Evidence C)
Currently, focused assessment of sonography for trauma (FAST) protocols and extended FAST (eFAST) protocols used in the setting of trauma do not incorporate an examination of the abdominopelvic area to detect pregnancy in reproductive-age women. However, at least one case demonstrated a timely diagnosis of intrauterine pregnancy during a FAST exam in a reproductive-age female with gunshot wounds to the chest [33]. Adding POC-US for the rapid identification of pregnancy to FAST and eFAST protocols for this patient population may decrease time to RCD, which may optimize outcomes.
There are also certain circumstances where the estimation of gestational age using fundal height alone is inadequate, such as extreme obesity. In this setting it may be necessary to use POC-US to determine gestational age quickly. Emerging data shows that providers with limited ultrasound training can effectively perform swift and targeted POC-US to determine gestational age [34, 35]. A single feasibility study evaluated the ability to teach emergency medicine providers (residents, fellows, sonographers) limited goal-directed obstetrical ultrasound to estimate gestational age. The learners quickly and accurately estimated gestational age in second and third trimester pregnancies using ultrasound measurement of biparietal diameter (BPD) [35]. Recently, MacCarthur et al. recommended incorporating a fetal FAST exam in trauma protocols in pregnant women and using femur length to determine gestational age quickly [36, 37]. Using POC-US to estimate gestational age, when indicated, appears promising.
-
2.
Consider POC-US during maternal cardiac arrest in emergency protocols for identification of potentially reversible causes of cardiac arrest, identification of cardiac contractility activity without palpable pulse for clinical reclassification of pulseless electrical activity, and identification of the absence of cardiac contractility where further attempts at resuscitation may be unsuccessful (Class IIa; Level of Evidence C).
Point-of-care ultrasound (POC-US) is currently used across emergency protocols to identify potentially reversible causes of cardiac arrest, cardiac contractility activity without a palpable pulse for clinical reclassification of pulseless electrical activity, and the absence of cardiac contractility where further tries at resuscitation may be unsuccessful. Despite the differences in maternal physiology from non-pregnant adults, many case reports highlight the successful application of POC-US to manage maternal cardiac arrest [34, 38,39,40]. POC-US has been used for earlier diagnosis and treatment of pulmonary embolism, pneumothorax, and pericardial effusion in out-of-hospital and in-hospital maternal cardiac arrest.
Where properly trained and resources are available, out-of-hospital practitioners may use POC-US for diagnosis and management of maternal cardiac arrest (Class IIa; Level of Evidence C).
POC-US has also been used for the rapid identification of an intrauterine pregnancy to help guide resuscitation management [34]. The knowledge compels EMS providers to transport the patient to the most appropriate care location and mobilize advanced resources to perform an RCD. This more rapid care flow and timing may improve maternal outcomes.
Targeted temperature management
Recommendations
-
1.
Current AHA recommendation: TTM should be considered in pregnancy on an individual basis (Class IIb; Level of Evidence C).
The routine use of targeted temperature management (TTM) in cardiac arrest is supported by the AHA based on the positive results of two large randomized trials in non-pregnant adults [41,42,43]. As there were only two case reports of TTM use in maternal cardiac arrest at the time of publication [44, 45] and lingering concerns for bleeding because of impaired systemic coagulation, the 2015 AHA statement recommended using post-arrest cooling on an individualized basis, and, if used, follow the same current protocol as for non-pregnant) [3]. Recently, several case reports noted using post-arrest TTM in the setting of maternal cardiac arrest with favorable maternal outcomes [5, 46,47,48,49,50,51]. This mounting evidence bolsters the current AHA position supporting the use of post-arrest TTM on an individual basis in pregnancy, with particular focus on the potential for bleeding complications during TTM.
-
2.
We recommend against the routine use of out-of-hospital induction of cooling after ROSC in pregnancy (Class III: No Benefit, Level of Evidence A)
The 2015 AHA Executive Summary for Cardiopulmonary Resuscitation recommends against the use of out-of-hospital cooling in cardiac arrest in non-pregnant adults [41]. A recent large meta-analysis of seven randomized controlled trials demonstrated potential harm from out-of-hospital induction of cooling. Out-of-hospital induction of cooling may increase the risk of cardiac re-arrest. We support this AHA recommendation in the setting of pregnancy as well.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- MCA:
-
Maternal cardiac arrest
- AHA:
-
American Heart Association
- RAM:
-
RAND/UCLA Appropriateness Method
- ACLS:
-
Advanced cardiac life support
- PMCD:
-
Perimortem cesarean delivery
- ROSC:
-
Return of spontaneous circulation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- POC-US:
-
Point-of-care ultrasound
- RCD:
-
Resuscitative cesarean delivery
- ECMO:
-
Extracorporeal membrane oxygenation
- BMV:
-
Bag-mask-valve
References
MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128:447.
Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011-2015, and strategies for prevention, 13 states, 2013-2017. MMWR Morb Mortal Wkly Rep. 2019;68:423–9.
Jeejeebhoy FM, Zelop CM, Lipman S, et al. Cardiac arrest in pregnancy: a scientific statement from the American Heart Association. Circulation. 2015;132:1747–73.
Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System. Website. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed 17 Sept 2019.
Mhyre JM, Tsen LC, Einav S, et al. Cardiac arrest during hospitalization for delivery in the United States, 1998-2011. Anesthesiology. 2014;120(4):810–8.
Zelop CM, Einav S, Mhyre JM, Martin S. Cardiac arrest during pregnancy: ongoing clinical conundrum. Obstet Gynecol. 2018;219(1):52.
Creanga A, Syverson C, Seed K, Callaghan W. Pregnancy-related mortality in the United States. 2011-2013. Obstet Gynecol. 2017;130:366.
Adams J, Cepeda Brito JR, Baker L, Hughes PG, et al. Management of Maternal Cardiac Arrest in the third trimester of pregnancy: a simulation-based pilot study. Crit Care Res Prac. 2016;2016, Article ID 5283765:8. https://doi.org/10.1155/2016/5283765.
Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol. 2010;203(179):e1–5.
Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol. 1986;68(4):571–6 PMID: 3528956.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15. https://doi.org/10.1046/j.1365-2648.2000.t01-1-01567.x.
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53:205–12.
Jacobs AK, Kushner FG, Ettinger SM, Guyton RA, et al. ACCF/AHA clinical practice guideline methodology summit report. A report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;61(2):213–65.
Dijkman A, Huisman C, Smit M, Schutte J, Zwart J, van Roosmalen J, et al. Cardiac arrest in pregnancy: increasing use of perimortem caesarean section due to emergency skills training? BJOG. 2010;117:282–7. https://doi.org/10.1111/j.1471-0528.2009.02461.
Einav S, Kaufmana N, Sela HY. Maternal cardiac arrest and perimortem caesarean delivery: evidence or expert-based? Resuscitation. 2012;83:1191–200. https://doi.org/10.1016/j.resuscitation.2012.05.005.
Rose C, Faksh A, Traynor K, Cabrera D, Arendt K, Brost B. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213(5):653–656,653.e1. https://doi.org/10.1016/j.ajog.2015.07.019.
Zelop CM, Einav S, Mhyre JM, Lipman SS, Arafeh J, Shaw RE, et al. Characteristics and outcomes of maternal cardiac arrest: a descriptive analysis of get with the guidelines data. Resuscitation. 2018;132:17–20. https://doi.org/10.1016/j.resuscitation.2018.08.029.
Kim HY, Jeon HJ, Yun JH, Lee JH, Lee GG, Woo SC. Anesthetic experience using extracorporeal membrane oxygenation for cesarean section in the patient with peripartum cardiomyopathy-a case report. Korean J Anesthesiol. 2014;66(5):392–7. https://doi.org/10.4097/kjae.2014.66.5.392.
Seong GM, Kim SW, Kang HS, Kang HW. Successful extracorporeal cardiopulmonary resuscitation in a postpartum patient with amniotic fluid embolism. J Thorac Dis. 2018;10(3):E189–93. https://doi.org/10.21037/jtd.2018.03.06.
Accreditation Council for Graduate Medical Education (ACGME). ACGME Program Requirements for Graduate Medical Education in Emergency Medicine 2017. https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirement
Moore SA, Dietl CA, Coleman DM. Extracorporeal life support during pregnancy. J Thorac Cardiovasc Surg. 2016;151(4):1154–60. https://doi.org/10.1016/j.jtcvs.2015.12.027.
McDonald C, Laurie J, Janssens S, Zazulak C, Kotze P, Shekar K. Successful provision of inter-hospital extracorporeal cardiopulmonary resuscitation for acute post-partum pulmonary embolism. Int J Obstet Anesth. 2017;30:65–8. https://doi.org/10.1016/j.ijoa.2017.01.003.
Takacs M, Damisch K. Extracorporeal life support as salvage therapy for massive pulmonary embolus and cardiac arrest in pregnancy. J Emerg Med. 2018;55(1):121–4. https://doi.org/10.1016/j.jemermed.2018.04.009.
Bataillard A, Hebrard A, Gaide-Chevronnay L, Casez M, Dessertaine G, Durand M, et al. Extracorporeal life support for massive pulmonary embolism during pregnancy. Perfusion. 2016;31(2):169–71. https://doi.org/10.1177/0267659115586578.
Fernandes P, Allen P, Valdis M, Guo L. Successful use of extracorporeal membrane oxygenation for pulmonary embolism, prolonged cardiac arrest, post-partum: a cannulation dilemma. Perfusion. 2015;30(2):106–10. https://doi.org/10.1177/0267659114555818.
Huang KY, Li YP, Lin SY, Shih JC, Chen YS, Lee CN. Extracorporeal membrane oxygenation application in post-partum hemorrhage patients: is post-partum hemorrhage contraindicated? J Obstet Gynaecol Res. 2017;43(10):1649–54. https://doi.org/10.1111/jog.13426.
Imaeda T, Nakada T, Abe R, Tateishi Y, Oda S. Veno-arterial extracorporeal membrane oxygenation for streptococcus pyogenes toxic shock syndrome in pregnancy. J Artif Organs. 2016;19:200. https://doi.org/10.1007/s10047-015-0884-3.
van Zwet CJ, Rist A, Haeussler A, Graves K, Zollinger A, Blumenthal S. Extracorporeal membrane oxygenation for treatment of acute inverted Takotsubo-like cardiomyopathy from hemorrhagic pheochromocytoma in late pregnancy. A A Case Rep. 2016;7(9):196–9. https://doi.org/10.1213/XAA.0000000000000383.
Helviz Y, Einav S. Maternal cardiac arrest. Curr Opin Anaesthesiol. 2019;32(3):298–306. https://doi.org/10.1097/ACO.0000000000000719.
Rojas-Peña A, Sall L, Gravel M, Cooley E, Pelletier S, Bartlett R, et al. Donation after circulatory determination of death: the University of Michigan experience with extracorporeal support. Transplantation. 2014;98(3):328–34. https://doi.org/10.1097/TP.0000000000000070.
Tavakoli AH, Rasoulian M, Ghadrigolestani M. The comparison of depression and consent in families of brain dead patients in donor and non-donor groups. Iran J Psychol Clin. 2006;11:4138.
Yousefi H, Roshani A, Nazari F. Experiences of the families concerning organ donation of a family member with brain death. Iran J Nurs Midwifery Res. 2014;19(3):323–30.
De Assis V, Shumbusho D, York B, Shields A. Resuscitation of maternal cardiac arrest after trauma. Crit Care Med. 2020;48(1):864. https://doi.org/10.1097/01.ccm.0000649416.95970.29.
Brun PM, Chenaitia H, Dejesus I, Bessereau J, Bonello L, Pierre B. Ultrasound to perimortem caesarean delivery in prehospital settings. Injury. 2013;44(1):151–2. https://doi.org/10.1016/j.injury.2012.08.029.
Shah S, Teismann N, Zaia B, Vahidnia F, River G, Price D, et al. Accuracy of emergency physicians using ultrasound to determine gestational age in pregnant women. Am J Emerg Med. 2010;28(7):834–8. https://doi.org/10.1016/j.ajem.2009.07.024.
MacArthur B, Foley M, Gray K, Sisley A. Trauma in pregnancy: a comprehensive approach to the mother and fetus. Am J Obstet Gynecol. 2019;220(5):465–468.e1. https://doi.org/10.1016/j.ajog.2019.01.209.
Snijders R, Nicolaides K. Fetal biometry at 14–40 weeks’ gestation. Ultrasound Obstet Gynecol. 1994;4(1):34–48. https://doi.org/10.1046/j.1469-0705.1994.04010034.x.
Wei J, Yang HS, Tsai SK, Hsiung MC, Chang CY, Ou CH, et al. Emergent bedside real-time three-dimensional transesophageal echocardiography in a patient with cardiac arrest following a caesarean section. Eur J Echocardiogr. 2011;12(3):E16. https://doi.org/10.1093/ejechocard/jeq161.
Venkataramani R, Im M, Rao S. Breathless to pulseless: a classic use of bedside ultrasonography to the rescue. Crit Care Med. 2016;44(12):491. https://doi.org/10.1097/01.ccm.0000510336.34856.a0.
Byhahn C, Tobias M, Bingolda TM, Zwissler B, Maier M, Walcher F. Prehospital ultrasound detects pericardial tamponade in a pregnant victim of stabbing assault. Resuscitation. 2008;76(1):146–8. https://doi.org/10.1016/j.resuscitation.2007.07.020.
Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. 2015 American health association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S315–67. https://doi.org/10.1161/CIR.0000000000000252.
Hypothermia After Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest [published correction appears in N Engl J Med. 2012;346:1756.]. N Engl J Med. 2002;346:549–56. https://doi.org/10.1056/NEJMoa012689.
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63. https://doi.org/10.1056/NEJMoa003289.
Rittenberger JC, Kelly E, Jang D, Greer K, Heffner A. Successful outcome utilizing hypothermia after cardiac arrest in pregnancy: a case report. Crit Care Med. 2008;36:1354–6. https://doi.org/10.1097/CCM.0b013e318169ee99.
Chauhan A, Musunuru H, Donnino M, McCurdy MT, Chauhan V, Walsh M. The use of therapeutic hypothermia after cardiac arrest in a pregnant patient. Ann Emerg Med. 2012;60:786–9. https://doi.org/10.1016/j.annemergmed.2012.06.004.
Oguayo KN, Oyetayo OO, Stewart D, Costa SM, Jones RO. Successful use of therapeutic hypothermia in a pregnant patient. Tex Heart Inst J. 2015;42(4):367–71. https://doi.org/10.14503/THIJ-14-4331.
Oami T, Oshima T, Oku R, Nakanishi K. Successful treatment of pulmonary embolism-induced cardiac arrest by thrombolysis and targeted temperature management during pregnancy. Acute Med Surg. 2018;5(3):292–5. https://doi.org/10.1002/ams2.345.
Hayroğlu M, Gümüşdağ A, Keskin M, Öz A, Çinier G, Ekmekçi A. Rhabdomyolysis secondary to therapeutic hypothermia after cardiopulmonary resuscitation: a rare complication. Am J Ther. 2016;23(5):e1255–6. https://doi.org/10.1097/MJT.0000000000000299.
Ocegueda-Pacheco C, García JC, Varon J, Polderman KH. Therapeutic hypothermia for cardiovascular collapse and severe respiratory distress after amniotic fluid embolism. Ther Hypothermia Temp Manag. 2014;4(2):96–8. https://doi.org/10.1089/ther.2013.0025.
De Santis V, Negri M, Nencini C, Fusari M. Successful use of targeted temperature management in pregnancy after out-of-hospital cardiac arrest. Am J Emerg Med. 2016;34(1):122.e3–4. https://doi.org/10.1016/j.ajem.2015.05.049.
Song KH, Lee BK, Jeung KW, Lee SM. Safely completed therapeutic hypothermia in postpartum cardiac arrest survivors. Am J Emerg Med. 2015;33(6):861.e5–6. https://doi.org/10.1016/j.ajem.2014.12.042.
Acknowledgments
The investigators thank the Center for Advanced Pediatric and Perinatal Education team at Stanford University for allowing us to use the name OBLS and Aaron Rome for his help submitting our grant to AHRQ.
Funding
Research reported in this publication was supported by the AHRQ of the National Institutes of Health under award number R18HS026169–02. The total program costs financed with Federal money is $341,460. There are no costs financed by nongovernmental sources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sources of funding
AHRQ Grant# 5 R18 HS026169-02.
Author information
Authors and Affiliations
Contributions
AS: Analyzed and interpreted data, and major contributor to writing the manuscript. JB: Analyzed data, major contributor to writing and editing manuscript. LK: Contributor to writing, editing manuscript. BT: Analyzed data, editing manuscript. PN: Analyzed data, editing manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. All methods were performed in accordance with the relevant guidelines and regulations. The Baylor IRB deemed the study minimal risk and informed consent was not required.
Consent for publication
Not applicable.
Competing interests
AS, Varda5.
JB, Varda5.
LK, None.
BT, Varda5, ACOG (modest), Research Grant Jim Hill AMAG study on Preeclampsia ($0).
PN, Varda5.
Drs. Andrea Shields, Jacqueline Battistelli, Peter Nielsen, and Brook Thomson are all members of Varda5, LLC, which is a consulting company for patient safety and quality initiatives.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shields, A.D., Battistelli, J.D., Kavanagh, L.B. et al. A modified Delphi approach to determine current treatment advances for the development of a resuscitation program for maternal cardiac arrest. BMC Emerg Med 22, 149 (2022). https://doi.org/10.1186/s12873-022-00704-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-022-00704-7