Abstract
Background
Prehospital telephone triage stratifies patients into five categories, “need immediate hospital visit by ambulance,” “need to visit a hospital within 1 hour,” “need to visit a hospital within 6 hours,” “need to visit a hospital within 24 hours,” and “do not need a hospital visit” in Japan. However, studies on whether present and past histories cause undertriage are limited in patients triaged as need an early hospital visit. We investigated factors associated with undertriage by comparing patient assessed to be appropriately triaged with those assessed undertriaged.
Methods
We included all patients classified by telephone triage as need to visit a hospital within 1 h and 6 h who used a single after-hours house call (AHHC) medical service in Tokyo, Japan, between November 1, 2019, and November 31, 2020. After home consultation, AHHC doctors classified patients as grade 1 (treatable with over-the-counter medications), 2 (requires hospital or clinic visit), or 3 (requires ambulance transportation). Patients classified as grade 2 and 3 were defined as appropriately triaged and undertriaged, respectively.
Results
We identified 10,742 eligible patients triaged as need to visit a hospital within 1 h and 6 h, including 10,479 (97.6%) appropriately triaged and 263 (2.4%) undertriaged patients. Multivariable logistic regression analyses revealed patients aged 16–64, 65–74, and ≥ 75 years (adjusted odds ratio [OR], 2.40 [95% confidence interval {CI} 1.71–3.36], 8.57 [95% CI 4.83–15.2], and 14.9 [95% CI 9.65–23.0], respectively; reference patients aged < 15 years); those with diabetes mellitus (2.31 [95% CI 1.25–4.26]); those with dementia (2.32 [95% CI 1.05–5.10]); and those with a history of cerebral infarction (1.98 [95% CI 1.01–3.87]) as more likely to be undertriaged.
Conclusions
We found that older adults and patients with diabetes mellitus, dementia, or a history of cerebral infarction were at risk of undertriage in patients triaged as need to visit a hospital within 1 h and 6 h, but further studies are needed to validate these findings.
Similar content being viewed by others
Introduction
Background
Prehospital telephone triage systems identify the appropriate care required for patients and determine their need for a hospital visit or an immediate hospital visit by ambulance [1]. Telephone triage plays a pivotal role in managing hospital workload and patient flow [2], and many countries have adopted telephone triage protocols [2,3,4]. Similarly in Japan, the Fire and Disaster Management Agency developed telephone triage protocols and established telephone consultation centers in several large cities, including Tokyo, to provide telephone triage to patients [5].
Recently, to reduce overcrowding in emergency departments, many countries have launched after-hours house call (AHHC) medical services or out-of-hours services [6] because delays in care for patients increase the risk of serious complications [7].
Similarly, a private AHHC service was established in Tokyo, Japan. This service provides consultations through telephone triages using developed telephone triage protocols. These protocols classify patients into five categories: “need immediate hospital visit by ambulance (red),” “need to visit a hospital within 1 hour (orange),” “need to visit a hospital within 6 hours (yellow),” “need to visit a hospital within 24 hours (green),” and “do not need a hospital visit (white).” The AHHC or out-of-hours medical services target patients triaged as “need to visit a hospital within 1 hour (orange)” and “need to visit a hospital within 6 hours (yellow).”
Previous telephone triage studies on AHHC medical services have explored the safety, efficiency, or quality of records documented by the nurse or doctor during telephone triage [8,9,10,11]. However, to the best of our knowledge, no study has assessed whether patients’ present and past histories cause undertriage, especially in patients who are classified under the “need to visit a hospital within 1 hour (orange)” and “need to visit a hospital within 6 hours (yellow)” category by telephone triage.
We aimed to investigate risk factors for undertriaging by comparing patients who are classified as need an early hospital visit from the appropriately triaged and undertriaged groups using records from a single AHHC medical service.
Methods
Study design
This study had a retrospective design and used anonymized data from medical records of patients who used the AHHC medical service from November 1, 2019, to November 31, 2020. The study design was reviewed and approved by the Research Ethics Committee of the University of Tsukuba (approval number: 1527).
Telephone triage system in Tokyo, Japan
A well-used telephone triage protocol developed by the Fire and Disaster Management Agency functions as follows: when a patient calls an emergency telephone consultation service, an operator classifies the patient into one of the five categories (red, orange, yellow, green, or white) based on a telephone triage protocol [5, 12, 13]. The protocols are divided into two categories: one for patients aged < 16 years and the other for those aged ≥16 years.
AHHC medical service
We used a private AHHC medical service in Tokyo, established by Fast Doctor Ltd. (Shinjuku, Tokyo, Japan) in 2016, which sends doctors directly to the residence of patients who need a hospital visit. The company operates 7 days a week outside of regular hospital visiting hours (18:00 to 06:00 on weekdays and Saturdays and 24 h on Sundays and holidays).
When a patient calls the AHHC service, operators (trained telephone triage nurses) perform the telephone triage using the telephone triage protocol. The operators determine the following: whether the patient is to remain at home (white), whether an AHHC doctor’s visit to the patient’s residence is needed (orange and yellow), or whether they need an ambulance (red). The operators call an ambulance for patients triaged as red and opt to provide the patient with information about nearby clinics or a primary hospital for patients triaged as green. The trained telephone triage nurses can consult a doctor beside the AHHC medical service call center.
After the AHHC medical service doctors conduct home visits for patients, these doctors classify patients into three categories: grade 1 (can be treated using over-the-counter medications), grade 2 (require a hospital or clinic visit), or grade 3 (require ambulance transportation) [14,15,16].
The doctors affiliated to the AHHC medical service are specialized attending doctors working at a university hospital and aged approximately 35 years. The telephone triage nurses are trained to use the telephone triage protocol in the AHHC medical service.
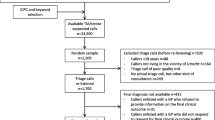
Figure 1 shows a correspondence table describing telephone triage and the grades assessed by AHHC doctors. Patients who were initially classified as orange and yellow and subsequently classified as grade 2 by AHHC doctors formed the appropriately triaged group. Patients initially classified as orange and yellow and subsequently as grade 3 by AHHC doctors formed the undertriaged group.
Study participants
We included all patients who had used the AHHC medical services between November 1, 2019, and November 31, 2020, and excluded those with missing records of age, sex, telephone triage categories, or doctor grade assessments after consultations.
Data source
The study used anonymized data from medical records of patients using the AHHC medical service (Fast Doctor Ltd.).
Data on the following variables of patients were extracted from medical records: sex, age, comorbidities (hypertension, diabetes mellitus, hyperlipidemia, gout, chronic lung disease, heart failure, liver disease, cerebral infarction, cancer, and dementia), telephone triage categories, protocols, doctor assessments after consultations, vital signs, and time from patients’ phone call to doctors’ consultations.
Statistical analyses
First, we compared baseline characteristics between the appropriately triaged and undertriaged groups. Pearson’s chi-square test or Fisher’s exact test was performed to compare categorical variables (age categories [0–15, 16–64, 65–74, and > 75] years, sex, comorbidities, telephone triage categories, protocols, and doctor assessments), and Student’s t-test or the Wilcoxon-Mann-Whitney test was performed to compare continuous variables (age, vital signs, and time from telephone triage to patient consultation), as appropriate. Second, we conducted a multivariable logistic regression analysis to identify factors associated with undertriage. Third, we conducted sensitivity analyses to exclude patients aged 0–15 years because the protocol used for these patients is different from that used for patients aged > 15 years. All statistical analyses were performed using JMP 16.0 statistical software (SAS Institute, Cary, NC, USA). The significance threshold was set at P of < 0.05.
Results
Proportion of undertriage
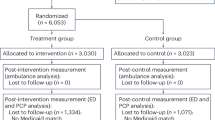
A total of 22,008 patients consulted the AHHC medical service between November 1, 2019, and November 31, 2020. We excluded 2249 patients owing to the lack of data on telephone triage, leaving a total of 19,759 patients classified as yellow or orange. After AHHC doctor consultation, 9017 (45.6%), 10,479 (53.0%), and 263 (1.3%) were classified as grade 1, grade 2 (appropriately triaged), and grade 3 (undertriaged), respectively (Fig. 2 and Supplementary File 1).
Definitions of appropriate triage and undertriage. When a patient calls the AHHC medical service, an operator classifies the patient into one of the five categories (red, orange, yellow, green, or white; at the left of the table). Doctors from the AHHC medical service visited patients who were classified as red, orange, and yellow and assessed them as grades 1, 2, or 3 after home visit and consultation (at the top of the table). Patients who were initially classified as orange and yellow and subsequently classified as grade 2 by AHHC doctors formed the appropriately triaged group. Patients who were initially classified as orange and yellow and subsequently as grade 3 by AHHC doctors formed the undertriaged group. AHHC, after-hours house call
Comparing patient characteristics between the appropriately triaged and undertriaged groups
Among the 19,759 patients, we compared patients who were classified in the appropriately triaged (10,479 patients) and undertriaged (263 patients) groups. The patient characteristics are shown in Table 1.
The proportions of patients aged 65–74 and ≥ 75 years were higher in the undertriaged group than in the appropriately triaged group. The proportion of patients with hypertension, diabetes mellitus, hyperlipidemia, gout, heart failure, cerebral infarction, cancer, and dementia was higher in the undertriaged group than in the appropriately triaged group.
Associated factors for undertriage
The results of the multivariable logistic regression analyses are shown in Table 2. Patients aged 16–64, 65–74, and ≥ 75 years (adjusted odds ratio {OR}: 2.40 [95% confidence interval {CI} 1.71–3.36], 8.57 [95% CI 4.83–15.2], and 14.9 [95% CI 9.65–23.01], respectively; reference patients aged < 15 years) and those with diabetes mellitus (adjusted OR, 2.31 [95% CI 1.25–4.26]), dementia (adjusted OR 2.32, [95% CI 1.05–5.10]), and a history of cerebral infarction (adjusted OR 1.98, [95% CI 1.01–3.87]) were more likely to be undertriaged. The results of the sensitivity analyses performed to exclude patients aged 0–15 years showed similar results.
Discussion
In this study, we found that 1) undertriage occurred in 1.3% of patients who were classified by the telephone triage as “hospital visit required” and 2) patients with old age, diabetes mellitus, dementia, and a history of cerebral infarction were at risk of undertriage.
Securing a safe and efficient telephone triage is challenging as a balance between an acceptable low level of overtriage and a minimal level of undertriage needs to be maintained for high patient safety [8]. Thus, investigating risk factors for undertriage in telephone triage is essential for patient safety.
Proportion of Undertriage
We found that the proportion of undertriage was < 2%. A previous systematic review showed that telephone undertriage occurred in 10% of AHHC medical service cases [9]. Meanwhile, recently, an AHHC service in Copenhagen reported that the incidence of undertriage was 0.04% [11]. It is difficult to compare undertriage rates across studies owing to differences in the definition of undertriage and institutional triage protocols [3]; this may be because there are dozens of telephone triage protocols, and the telephone triage protocol utilized varies across countries or communities [3]. In addition, modified telephone triage protocols have been developed [17, 18], leading to a decrease in undertriage. Thus, telephone triage protocols adapted in each country, area, or modified telephone triage should be evaluated with regard to the level of triage and according to each telephone triage protocol.
Risk factors associated with Undertriage
We found that old age, diabetes mellitus, dementia, and a history of cerebral infarction were associated with undertriage. A previous study conducted at a trauma center showed that age ≥ 65 years [19], female sex, dementia [20], history of cerebral infarction, and heart failure [21] were risk factors for undertriage of trauma patients. Among these risk factors for undertriage of trauma patients, old age, dementia, and history of stroke were also identified as risk factors in our study.
The telephone triage protocols are used to carefully record and document the patient’s medical history, including hypertension, diabetes mellitus, myocardial infarction, heart failure, liver disease, chronic lung disease, and collagen disease, as well as age ≥ 65 years and the AHHC medical service used in the telephone protocols. However, age ≥ 75 years and history of cerebral infarction are not factors incorporated in the telephone triage protocol. In Japan, the population is rapidly aging, leading to an increased incidence of dementia and cerebral infarction [22]; thus, the patient may not be able to report their symptoms well or a caregiver may not be able to make the call or report their patients’ symptoms well. Therefore, adding dementia or history of cerebral infarction to the telephone protocol may improve the accuracy of telephone triage.
Limitations
This study has several limitations. First, the study included a relatively small number of undertriaged patients; thus, we could not stratify and analyze each telephone triage level and protocol (Supplementary File 2), including decision-making factors. Second, this study was performed in a single AHHC medical service in Japan; thus, it may be difficult to adapt our results to other triage levels and other countries. However, our approach would be useful to other telephone triage systems to evaluate factors associated with undertriage in other countries. Third, this was a retrospective cohort study; therefore, missing or residual confounding factors could have caused undertriage. However, we believe that important confounding factors (e.g., age ≥ 65 years, heart failure, history of stroke, and dementia), which have been previously reported to cause undertriage, were covered in the present study. Fourth, we did not evaluate inter-rater reliability among AHHC medical service doctors. Fifth, the AHHC medical service could not conduct a follow-up of patients assessed in the undertriaged group sent to the hospital. If very few patients sent to the hospital are admitted and most are sent home, then the telephone triage protocols may well be working and some physicians may in fact be overtriaging. Lastly, the level of triage may have changed by the time the AHHC doctor arrived; the reason for this change should be investigated in the future.
Conclusion
Telephone triage in an AHHC should be carefully performed for patients with advanced age, dementia, and a history of cerebral infarction. Further studies are warranted to evaluate other telephone triage protocols.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHHC:
-
After-hours house call
- CI:
-
confidence interval
- IQR:
-
interquartile range
- OR:
-
odds ratio
References
Derkx HP, Rethans JJ, Muijtjens AM, et al. Quality of clinical aspects of call handling at Dutch out of hours centres: cross sectional national study. BMJ. 2008;337(sep12 1):a1264. https://doi.org/10.1136/bmj.a1264.
Anderson A, Roland M. Potential for advice from doctors to reduce the number of patients referred to emergency departments by NHS 111 call handlers: observational study. BMJ Open. 2015;5(11):e009444. https://doi.org/10.1136/bmjopen-2015-009444.
Montandon DS, de Souza-Junior VD, Dos Santos Almeida RG, Marchi-Alves LM, Costa Mendes IA, de Godoy S. How to perform prehospital emergency telephone triage: a systematic review. J Trauma Nurs. 2019;26(2):104–10. https://doi.org/10.1097/JTN.0000000000000380.
Smits M, Rutten M, Keizer E, Wensing M, Westert G, Giesen P. The development and performance of after-hours primary care in the Netherlands: a narrative review. Ann Intern Med. 2017;166(10):737–42. https://doi.org/10.7326/M16-2776.
Sakurai A, Morimura N, Takeda M, Miura K, Kiyotake N, Ishihara T, et al. A retrospective quality assessment of the 7119 call triage system in Tokyo - telephone triage for non-ambulance cases. J Telemed Telecare. 2014;20(5):233–8. https://doi.org/10.1177/1357633X14536347.
Australian Government Department of Health. Review of after hours primary health care. 2015. https://www1.health.gov.au/internet/main/publishing.nsf/Content/primary-ahphc-review. Accessed 1 Nov 2021.
Pines JM, Pollack CV, Diercks DB, Chang AM, Shofer FS, Hollander JE. The association between emergency department crowding and adverse cardiovascular outcomes in patients with chest pain. Acad Emerg Med. 2009;16(7):617–25. https://doi.org/10.1111/j.1553-2712.2009.00456.x.
Graversen DS, Christensen MB, Pedersen AF, et al. Safety, efficiency and health-related quality of telephone triage conducted by general practitioners, nurses, or physicians in out-of-hours primary care: a quasi-experimental study using the assessment of quality in telephone triage (AQTT) to assess audio-recorded telephone calls. BMC Fam Pract. 2020;21:84.
Huibers L, Smits M, Renaud V, Giesen P, Wensing M. Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care. 2011;29(4):198–209. https://doi.org/10.3109/02813432.2011.629150.
Hansen EH, Hunskaar S. Telephone triage by nurses in primary care out-of-hours services in Norway: an evaluation study based on written case scenarios. BMJ Qual Saf. 2011;20(5):390–6. https://doi.org/10.1136/bmjqs.2010.040824.
Gamst-Jensen H, Lippert FK, Egerod I. Under-triage in telephone consultation is related to non-normative symptom description and interpersonal communication: a mixed methods study. Scand J Trauma Resusc Emerg Med. 2017;25(1):52. https://doi.org/10.1186/s13049-017-0390-0.
Morimura N, Aruga T, Sakamoto T, Aoki N, Ohta S, Ishihara T, et al. The impact of an emergency telephone consultation service on the use of ambulances in Tokyo. Emerg Med J. 2011;28(1):64–70. https://doi.org/10.1136/emj.2009.073494.
Q suke. https://www.fdma.go.jp/relocation/neuter/topics/filedList9_6/kyukyu_app/kyukyu_app_web/index.html Accessed 11 Nov 2021.
Inokuchi R, Morita K, Iwagami M, Watanabe T, Ishikawa M, Tamiya N. Changes in the proportion and severity of patients with fever or common cold symptoms utilizing an after-hours house call medical service during the COVID-19 pandemic in Tokyo, Japan: a retrospective cohort study. BMC Emerg Med. 2021;21(1):64. https://doi.org/10.1186/s12873-021-00458-8.
Morita K, Inokuchi R, Jin X, Ishikawa M, Tamiya N. Patients' impressions of after-hours house-call services during the COVID-19 pandemic in Japan: a questionnaire-based observational study. BMC Fam Pract. 2021;22(1):184. https://doi.org/10.1186/s12875-021-01534-5.
Inokuchi R, Morita K, Jin X, Ishikawa M, Tamiya N. Pre- and post-home visit behaviors after using after-hours house call (AHHC) medical services: a questionnaire-based survey in Tokyo. BMC Emerg Med: Japan; 2021. [In press]
Sakurai A, Oda J, Muguruma T, Kim S, Ohta S, Abe T, et al. Revision of the protocol of the telephone triage system in Tokyo, Japan. Emerg Med Int. 2021;2021:8832192–6. https://doi.org/10.1155/2021/8832192.
Smits M, Keizer E, Ram P, Giesen P. Development and testing of the KERNset: an instrument to assess the quality of telephone triage in out-of-hours primary care services. BMC Health Serv Res. 2017;17(1):798. https://doi.org/10.1186/s12913-017-2686-1.
Knotts CM, Modarresi M, Samanta D, Richmond BK. The impact of under-triage on trauma outcomes in older populations ≥65 years. Am Surg. 2021;3134820951456(9):1412–9. https://doi.org/10.1177/0003134820951456.
Barsi C, Harris P, Menaik R, Reis NC, Munnangi S, Elfond M. Risk factors and mortality associated with undertriage at a level I safety-net trauma center: a retrospective study. Open Access Emerg Med. 2016;8:103–10. https://doi.org/10.2147/OAEM.S117397.
Benjamin ER, Khor D, Cho J, Biswas S, Inaba K, Demetriades D. The age of undertriage: current trauma triage criteria underestimate the role of age and comorbidities in early mortality. J Emerg Med. 2018;55(2):278–87. https://doi.org/10.1016/j.jemermed.2018.02.001.
Nojiri S, Itoh H, Kasai T, Fujibayashi K, Saito T, Hiratsuka Y, et al. Comorbidity status in hospitalized elderly in Japan: analysis from National Database of health insurance claims and specific health checkups. Sci Rep. 2019;9(1):20237. https://doi.org/10.1038/s41598-019-56534-4.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from Fast Doctor Ltd.
Author information
Authors and Affiliations
Contributions
RI conceived the study. RI performed the statistical analyses and wrote the first draft of the manuscript. XJ, MI, TA, MI, and NT critically reviewed the manuscript. All authors contributed to the study design, interpretation of results, and critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Committee of University of Tsukuba approved this study (approval number: 1527) and waived the need for informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable (individual-level data not included).
Competing interests
1) RI’s joint appointment as an associate professor and 2) XJ as an assistant professor at the University of Tsukuba were sponsored by Fast Doctor Ltd. from October 2019 to date. Fast Doctor Ltd. had no role in this study. Iwagami M, TA, Ishikawa M, and NT declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: File 1.
All patients classified as grades 1, 2, and 3
Additional file 2: File 2.
Protocol causing undertriage
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Inokuchi, R., Jin, X., Iwagami, M. et al. Factors associated with undertriage in patients classified by the need to visit a hospital by telephone triage: a retrospective cohort study. BMC Emerg Med 21, 155 (2021). https://doi.org/10.1186/s12873-021-00552-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-021-00552-x