Abstract
Objectives
Our study aimed to assess the safety and efficacy of cardiac contractility modulation (CCM) therapy in patients with heart failure with reduced ejection fraction (HFrEF) depending on HF etiology.
Methods
We enrolled 166 patients with optimal medical therapy-resistant HFrEF (median age 59 years, 83.7% males, median NYHA class − 2, median left ventricular ejection fraction (LVEF) − 29.0%) who underwent CCM therapy device implantation from 2013 to 2019 in four medical centers in Russia. The HF etiology was determined based on invasive coronary angiography or cardiac MRI data. Transthoracic echocardiography (TTE), 6-minute walking test (6MWT), and NTproBNP-tests were performed at a baseline and 12 months after the implantation.
Results
The ischemic etiology of HF was revealed in 100 patients (61.5%) (ICM group); the non-ischemic group (NICM) evolved 66 patients (38.5%). Patients in the ICM group were significantly older (61[57–69] vs. 55 [42.8–61], p < 0.001), more frequently had hypertension (79% vs. 42.4%, p < 0.001) and chronic kidney disease (43% vs. 22.7%, p = 0.012). Patients in the NICM group had significantly more often atrial fibrillation (AF) (58% vs. 74%, p = 0.048), larger end-diastolic volume (EDV) (249 [208–309] vs. 220 [192–271], p = 0.019) and end-systolic volume (ESV) (183 [147–230] vs. 154 [128–199], p = 0.003). There were no significant differences in mortality between ICM and NICM groups (14.4 vs. 10.8%, p = 0.51). In 12 months, there was a significant increase in LVEF in the NICM group (+ 2.0 [2–6] vs. +7.7 [2–12], p < 0.001), while the improvement in the 6MWT (+ 75 [22–108] vs. +80 [10–160], p = 0.851) and NYHA class did not reach the level of significance. The subanalysis between patients with improved NYHA class and those without improvement revealed that patients without improvement more frequently had AF (56% vs. 89%; p < 0.01), chronic obstructive lung disease (18% vs. 35% p = 0.047), higher blood pressure (110 [105–120] vs. 120[110–129]; p = 0.032).
Conclusion
In this multicenter retrospective study, patients with non-ischemic HFrEF showed a significantly higher improvement in LVEF and LV reverse remodeling following CCM therapy device implantation. There was no significant association between HF etiology and survival in drug-resistant HFrEF patients following CCM therapy.
Similar content being viewed by others
Introduction
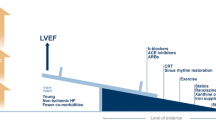
Cardiac contractility modulation (CCM) is a relatively new device-based (the Optimizer™ system by Impulse Dynamics, Orangeburg, NY, USA) therapy for heart failure with reduced ejection fraction (HFrEF). It can be recommended for patients with optimal medical therapy (OMT)-persistent symptoms of HF. CCM involves the administration of a biphasic non-excitatory electrical impulse to the interventricular septum during the ventricular absolute refractory period. CCM affects myocardial cell biology: in vitro studies showed that it enhances myocardial contraction via calcium circulation regulation without increasing myocardial oxygen consumption [1]. The results of clinical studies supported these data: the administration of CCM was associated with clinical improvement and lower hospitalization rates in patients with HFrEF (II-IV NYHA class, left ventricular ejection fraction (LVEF) < 40%) [2,3,4,5,6]. The meta-analysis of randomized controlled trials conducted by Giallauria et al. [7] revealed a moderate effect on peak oxygen consumption (VO2 peak) and exercise tolerance, thus improving the quality of life. Still, it demonstrated no effect on LVEF and mortality.
The impact of HF etiology on CCM therapy efficacy remains controversial. The etiology of heart failure (nonischemic vs. ischemic) was not associated with improvement in the etiology-dependent subgroup analysis of the FIX-HF-5 study [8]. On the contrary, the single-center study conducted by Fastner et al. reported a significant increase in LVEF and LV reverse modeling in NICM patients in the mid-term perspective [9]. A year later, Fastner et al [10] presented their findings in a larger cohort of patients. The authors did not reveal any significant difference in 12-month LVEF between ICM and NICM patients. These changes achieved the level of significance only in patients completing the 5-year follow-up.
Here, we present the 12-month results of our multicenter HF etiology-specified analysis of CCM therapy efficacy and safety in real-world practice.
Methods
This multicenter retrospective analysis included data from 166 patients with OMT-resistant HFrEF and NYHA class II-IV who underwent CCM therapy system implantation using Optimizer™ IV or Optimizer™ Smart (Impulse Dynamics, Orangeburg, NY, USA) from 2013 to 2019 in four medical centers in Russia within the framework of the national CCM therapy device implantation program. The federal program protocol was initially approved by the National Ethics Committee and, after that, by each centers’ Independent Ethics Committee. All patients signed a written informed consent before recruitment.
The inclusion criteria were age ≥ 18 years, OMT-resistant HFrEF, and NYHA class ≥ II. The exclusion criteria were patients on the heart transplant waiting list, a history of myocardial infarction, PCI, cardiac surgeries within three months, acute myocarditis, hypertrophic cardiomyopathy, reversible causes for HF, mechanical tricuspid valve, severe comorbidities (acute decompensation, injury, or failure in other organ systems).
The implantation procedures were performed under local anesthesia with lidocaine hydrochloride (10 mg/ml). An infraclavicular incision was made, and a pocket was created in the right subclavian region. The leads via the subclavian approach were advanced to the heart. Patients implanted with Optimizer™ IV got three screw-in leads - one atrial (Boston Scientific 7741 Ingevity IS-1 52 cm) and two ventricular leads (Boston Scientific 7742 Ingevity IS-1 59 cm, St Jude Tendril STS IS-1 59 cm); patients with Optimizer™ Smart - only two ventricular leads (Boston Scientific 7742 Ingevity IS-1 59 cm, St Jude Tendril STS IS-1 59 cm). The atrial lead was fixed into the right atrial appendage; the two ventricular leads were implanted in the right ventricular aspect of the interventricular septum. The tip-to-tip distance between ventricular leads was ≥ 2 cm.
Follow-up
The clinical follow-up duration was 12 months, with follow-up visits at 2, 6, and 12 months. Devices’ interrogation (Optimizer™ and CRT-D) and data analysis were performed at each follow-up visit. Data regarding clinical events and healthcare utilization were also collected. We thoroughly screened the available medical records of all 166 patients. The following parameters were collected at baseline and 12 months after implantation: demographics, medical history, physical examination data, laboratory examination data, NYHA class, six-minute walking distance (6MWD), transthoracic echocardiography (TTE), NTproBNP levels. Since February 2020, the follow-up protocol has been changed due to the COVID-19 pandemic. In some patients, the 12-month follow-up data was acquired remotely.
Statistical analysis
Continuous variables were presented as median (Me), interquartile range (IQR), mean (M), and standard deviation (SD) depending on the distribution. Categorical variables were presented as frequencies (percentages). Differences in the patients’ continuous data results were checked for significance with the Wilcoxon signed-rank test or the Student’s T-test, respectively. The chi-square test was used to compare categorical variables. The correlation between metrics was evaluated by calculating the Spearman correlation coefficient. For survival analyses, Kaplan-Maier curves were done. A two-tailed p-value ≤ 0.05 was regarded to be significant. Data were analyzed with the R programming language.
Results
Baseline characteristics
Data from 166 patients with OMT-resistant HFrEF who underwent Optimizer device implantation from 2013 to 2019 in four medical centers in Russia were analyzed in this study. The median age of the total study participants was 59 [54.0;66.0] years; the majority were males (83.7%). The median LVEF was 29% [24.1–33.0], with a median NYHA class of 2 [2;3]. The ischemic etiology of HF was revealed in 100 patients (61.5%) (ICM group); the non-ischemic group (NICM) evolved 66 patients (38.5%). Patients in the ICM group were significantly older (61[57–69] vs. 55 [42.8–61], p < 0.001), more frequently had hypertension (79% vs. 42.4%, p < 0.001), and chronic kidney disease (43% vs. 22.7%, p = 0.012). Patients in the NICM group had significantly more often atrial fibrillation (AF) (58% vs. 74%, p = 0.048), larger enddiastolic volume (EDV) (249 [208;309] vs. 220 [192;271], p = 0.019) and endsystolic volume (ESV) (183 [147;230] vs. 154 [128;199], p = 0.003). They also more frequently received angiotensin receptor/neprilysin inhibitors [28.8% vs. 9%, p = 0.002] and anticoagulants [77.3% vs. 60%, p = 0.032]. Only a third of the patients (29.5%) were previously implanted with ICD/CRT-D due to the limited quantity of state-funded available devices. Baseline characteristics of patients in detail, as well as the number of available records for each parameter, are presented in Table 1.
Successful device implantation was carried out in all patients. During the 12-month follow-up, five patients developed major pectoral muscle pacing, requiring device lead replacement in three patients. In two patients, we set the device parameters so that the CCM pacing was continued with one lead, and the other was used only for sensing.
CCM device pacing rate
The CCM device pacing rate data was available for 134 patients (80.7%). The CCM pacing rate > 75% was achieved in 112 patients (83.6%); 86 of them (76.8%) have also reached the level of > 90% with a median rate of 95.2% [88.2;99.0]. The subanalysis of the CCM pacing rate in patients with AF showed a high Optimizer pacing rate regardless of AF type (Fig. 1).
Survival
21 patients (13%) died during the 12-month follow-up. Cardiovascular death was confirmed in 12 patients. 9 patients died due to acute decompensation of chronic heart failure; 3 patients developed sudden cardiac death (only one had a previously implanted ICD). No mortality differences existed between patients with ICM and NICM (14.4 and 10.8% p = 0.51) (Fig. 2).
Changes in transthoracic echocardiography, six-minute walking distance, and NTproBNP parameters
The thorough analysis of changes in TTE parameters, 6MWD test, and NTproBNP levels is presented in Table 2. We missed 12-month follow-up data in some patients due to remote follow-up during the COVID-19 pandemic.
The overall 12-month LVEF was improved in most of the patients (Fig. 3). Moreover, 12-month LVEF in 16 patients (24%) in the NICM group increased up by ≥ 40%. The analysis of 12-month TTE data revealed a significant increase in LVEF (+ 2.0 [2.0;6.0] vs. +7.7[2.0;12.0], p < 0.001), and a significant decrease in end-systolic volume (-3.0 [-18.0;10.0] vs. -24.0[-74.5;0.0], p < 0.001) and end-diastolic volume (-3.0[-22.75;21.8] vs. -24[-69.5;6.0], p = 0.007) in the NICM group.
We detected an improvement in the 6MWT, but these changes did not reach the level of significance (+ 75 [22;108] vs. +80 [10;160], p = 0.851).
The NTproBNP level decreased in both groups, which was more pronounced in the NICM groups. However, this decrease did not reach statistical significance (-262.55 vs. -591.0, p = 0.091).
We revealed a modest NYHA class improvement in both groups, which was more significant in the NICM group (p = 0.041). Almost half of the patients completing 12 months of follow-up showed ≥ 1 NYHA class improvement (Fig. 4). Patients with improving/stable NYHA class significantly less frequently suffered from COPD (17.5% vs. 37%, p = 0.047), AF (56% vs. 89%, p = 0.010), and lower extremity edema (22.4% vs. 50%, p = 0.008). They also had lower baseline systolic blood pressure (110.0 [105.0;120.0] vs. 120.0[110.0;129.0], p = 0.032), baseline pulmonary artery systolic pressure (34.5[26.2;44.8] vs. 40.0[31.5;55.0], p = 0.030), ESD (57.0[52.0;63.0] vs. 61.0[56.0;68.0], p = 0.036), baseline NTproBNP (1279.0[665.0;2280.0] vs. 2472.0[1208.0; 6492.0, p = 0.001). The detailed comparative analysis of patients with improving/stable and worsening NYHA classes/fatal outcomes is presented in Table 3.
Discussion
The impact of HF etiology on CCM therapy is poorly studied and remains controversial. Such an important HF marker as LVEF was not assessed in RCTs as the primary endpoint of CCM therapy; most of the RCTs assessed exercise tolerance [2,3,4,5]. So, the interpretation of LVEF changes following Optimizer system implantation is understudied. Our analysis revealed that CCM therapy in NICM patients led to significant LVEF improvement with no statistically significant effect on 12-month survival. We also detected a significant improvement in the NICM group in other TTE data, such as EDV and ESV, reflecting the LV reverse remodeling. Our findings correlated well with the study results conducted by Fastner et al. [9], showing not only a remarkable LVEF improvement in NICM patients but also an LV reverse remodeling process reflected in LVEDD reduction.
On the one hand, these results could have been predictable. Although the SCD rates were similar for ICM and NICM patients [11], an older age, significantly more frequent comorbidities, worse response to HF drug therapy, a higher risk of cardiovascular death (especially due to myocardial infarction), and worse survival in patients with ischemic cardiomyopathy [12,13,14,15] suggest a poorer outcome of CCM therapy in those patients. However, Abraham et al. [8] did not reveal any association between HF etiology and patients’ improvement. LVEF improvement was not dependent on HF etiology in the study conducted by Müller et al., too [16]. On the other hand, the last study evolved patients with > 35% LVEF, which can be a possible explanation for such discrepancy in study results.
Our study also confirmed the tendency for the NTproBNP level to decrease, which was more pronounced in NICM patients. It is interesting to notice that NTproBNP level reduction tendency reached the level of statistical significance in the study conducted by Kuschyk et al. [17] evaluating the long-term efficacy (34.2 ± 28 months) of CCM therapy. This may reflect the long-term beneficial effects of CCM therapy on cardiac myocytes. However, Kuschyk et al. did not specify the HF etiology.
In our study, the 12-month 6MWD improvement did not reach the significance level. We also did not reveal any differences in 6MWD changes depending on HF etiology. Most of the studies, including RCTs, showed a significant increase in exercise tolerance, particularly in 6MWD [7, 18,19,20,21,22]. The involvement of more patients with advanced heart failure in our study can be the possible explanation for not reaching the significance level for 6MWD improvement during 12 months of follow-up. However, the 12 months of follow-up confirmed the more significant improvement of the NYHA in NICM patients.
Our subanalysis of patients’ characteristics with and without clinical impairment revealed, that patients without clinical improvement more frequently suffered from COPD, AF, and edema, and had higher baseline systolic blood pressure, baseline pulmonary artery systolic pressure, ESD, and baseline NTproBNP. Our results indicate the crucial role of patients’ thorough selection for effective CMM therapy, as patients with progressive congestive heart failure, edema, and frequent hospitalizations may not benefit from CCM therapy. Thus, we could recommend, that these patients should immediately be placed on the waiting list for heart transplantation skipping the CCM therapy device implantation. However, further larger, multicenter studies with a control group and optimal medical therapy are necessary to clarify these findings.
Limitations
There are some possible limitations of this study: First, this is a retrospective analysis of the prospective collected data. These data were collected within the framework of a state-funded CCM therapy implementation program in Russia. The state-funded character of the program predefined the number of participants and the duration of the clinical follow-up visits. Second, optimal medical therapy has changed over the years; most patients were implanted with Optimizer devices before ARNI and SGLT2 inhibitors became available in Russia. Third, the Optimizer device provides information about the device pacing rate, which is not always the same as the CCM therapy rate. Fourth, due to the COVID-19 pandemic, some follow-up visits were done remotely, and we don’t have complete follow-up data for some patients.
Conclusion
Patients with non-ischemic HFrEF showed a significantly higher improvement in LVEF and LV reverse remodeling following CCM therapy device implantation. There was no significant association between HF etiology and survival in drug-resistant HFrEF patients following CCM therapy.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Imai M, Rastogi S, Gupta RC, Mishra S, Sharov VG, Stanley WC, et al. Therapy with Cardiac Contractility Modulation Electrical signals improves left ventricular function and remodeling in Dogs with Chronic Heart failure. J Am Coll Cardiol. 2007;49(21):2120–8.
Neelagaru SB, Sanchez JE, Lau SK, Greenberg SM, Raval NY, Worley S et al. Nonexcitatory, cardiac contractility modulation electrical impulses: feasibility study for advanced heart failure in patients with normal QRS duration. Heart Rhythm. 2006 Oct [cited 2023 Sep 8];3(10):1140–7. https://pubmed.ncbi.nlm.nih.gov/17018340/.
Borggrefe MM, Lawo T, Butter C, Schmidinger H, Lunati M, Pieske B, et al. Randomized, double blind study of non-excitatory, cardiac contractility modulation electrical impulses for symptomatic heart failure. Eur Heart J. 2008;29:8.
Kadish A, Nademanee K, Volosin K, Krueger S, Neelagaru S, Raval N, et al. A randomized controlled trial evaluating the safety and efficacy of cardiac contractility modulation in advanced heart failure. Am Heart J. 2011;161(2):329–e3372.
Abraham WT, Kuck KH, Goldsmith RL, Lindenfeld JA, Reddy VY, Carson PE, et al. A randomized controlled trial to evaluate the safety and efficacy of Cardiac Contractility Modulation. JACC Heart Fail. 2018;6(10):874–83.
Röger S, Schneider R, Rudic B, Liebe V, Stach K, Schimpf R et al. Cardiac contractility modulation: first experience in heart failure patients with reduced ejection fraction and permanent atrial fibrillation. EP Europace. 2014 Aug 1 [cited 2022 Aug 6];16(8):1205–9. https://academic.oup.com/europace/article/16/8/1205/549781.
Giallauria F, Cuomo G, Parlato A, Raval NY, Kuschyk J, Stewart Coats AJS. A comprehensive individual patient data meta-analysis of the effects of cardiac contractility modulation on functional capacity and heart failure-related quality of life. ESC Heart Fail. 2020;7(5).
Abraham WT, Nademanee K, Volosin K, Krueger S, Neelagaru S, Raval N et al. Subgroup analysis of a randomized controlled trial evaluating the safety and efficacy of cardiac contractility modulation in advanced heart failure. J Card Fail. 2011;17(9).
Fastner C, Akin I, Yuecel G, Rudic B, El-Battrawy I, Kruska M et al. Cardiac contractility modulation efficacy: is there a difference between ischemic vs. non-ischemic patients? Eur Heart J. 2020;41(Supplement_2).
Fastner C, Yuecel G, Rudic B, Schmiel G, Toepel M, Burkhoff D et al. Cardiac Contractility Modulation in Patients with Ischemic versus Non-ischemic Cardiomyopathy: Results from the MAINTAINED Observational Study. Int J Cardiol. 2021 Nov 1 [cited 2024 Apr 29];342:49–55. http://www.internationaljournalofcardiology.com/article/S0167527321011931/fulltext.
Sapp JL, Parkash R, Wells GA, Yetisir E, Gardner MJ, Healey JS et al. Cardiac Resynchronization Therapy Reduces Ventricular Arrhythmias in Primary but Not Secondary Prophylactic Implantable Cardioverter Defibrillator Patients: Insight From the Resynchronization in Ambulatory Heart Failure Trial. Circ Arrhythm Electrophysiol. 2017 Mar 1 [cited 2023 Aug 14];10(3). https://pubmed.ncbi.nlm.nih.gov/28292754/.
Tymińska A, Ozierański K, Balsam P, Maciejewski C, Wancerz A, Brociek E et al. Ischemic cardiomyopathy versus non-ischemic dilated cardiomyopathy in patients with reduced ejection fraction— clinical characteristics and prognosis depending on heart failure etiology (data from European Society of Cardiology Heart Failure Registries). Biology (Basel). 2022;11(2).
Pouleur AC, Barkoudah E, Uno H, Skali H, Finn PV, Zelenkofske SL et al. Pathogenesis of sudden unexpected death in a clinical trial of patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. Circulation. 2010;122(6).
Cleland JGF, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L et al. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure [the CArdiac REsynchronization-Heart failure (CARE-HF) trial extension phase]. Eur Heart J. 2006;27(16).
Balmforth C, Simpson J, Shen L, Jhund PS, Lefkowitz M, Rizkala AR et al. Outcomes and effect of treatment according to etiology in HFrEF: an analysis of PARADIGM-HF. JACC Heart Fail. 2019;7(6).
Müller D, Remppis A, Schauerte P, Schmidt-Schweda S, Burkhoff D, Rousso B et al. Clinical effects of long-term cardiac contractility modulation (CCM) in subjects with heart failure caused by left ventricular systolic dysfunction. Clin Res Cardiol. 2017;106(11).
Kuschyk J, Roeger S, Schneider R, Streitner F, Stach K, Rudic B et al. Efficacy and survival in patients with cardiac contractility modulation: long-term single center experience in 81 patients. Int J Cardiol. 2015;183.
Stix G, Borggrefe M, Wolpert C, Hindricks G, Kottkamp H, Böcker D et al. FT Chronic electrical stimulation during the absolute refractory period of the myocardium improves severe heart failure. Eur Heart J. 2004 Apr [cited 2021 Jun 3];25(8):650–5. https://pubmed.ncbi.nlm.nih.gov/15084369/.
Nägele H, Behrens S, Eisermann C. Cardiac contractility modulation in non-responders to cardiac resynchronization therapy. Europace. 2008 Dec [cited 2021 Jun 13];10(12):1375–80. https://pubmed.ncbi.nlm.nih.gov/18776196/.
Liu M, Fang F, Luo XX, Shlomo BH, Burkhoff D, Chan JYS et al. Improvement of long-term survival by cardiac contractility modulation in heart failure patients: A case-control study. Int J Cardiol. 2016;206:122–6. https://doi.org/10.1016/j.ijcard.2016.01.071.
Kuschyk J, Roeger S, Schneider R, Streitner F, Stach K, Rudic B et al. Efficacy and survival in patients with cardiac contractility modulation: Long-term single center experience in 81 patients. Int J Cardiol. 2015 Mar 15 [cited 2021 Jun 3];183:76–81. https://pubmed.ncbi.nlm.nih.gov/25662055/.
Müller D, Remppis A, Schauerte P, Schmidt-Schweda S, Burkhoff D, Rousso B et al. Clinical effects of long-term cardiac contractility modulation (CCM) in subjects with heart failure caused by left ventricular systolic dysfunction. Clinical Research in Cardiology. 2017 Nov 1 [cited 2021 Jun 3];106(11):893–904. Available from: /pmc/articles/PMC5655601/.
Acknowledgements
Not applicable.
Funding
The registry data were obtained within the framework of the national CCM therapy device implantation program funded by the Ministry of Health.
Author information
Authors and Affiliations
Contributions
KD, EM, and DL conceived and developed the idea. KD, ICh, and SG developed the study protocol. MKh, SG, OS, MV, MS, EL, ICh, NM, ER, and GS contributed to the data. YuM analyzed the data. ICh and AT wrote the paper with support from KD. KD, EM, and NM helped to supervise the program. All authors discussed the results, contributed to the manuscript’s clinical revision, and approved the final manuscript. All authors agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study program protocol was developed following the Declaration of Helsinki. Primarily, the protocol was approved by the National Ethics Committee Ethics Committee of the Ministry of Health of the Russian Federation. Then the approval was obtained at each participating site by the centers’ Independent Ethics Committee. All patients signed a separate informed consent form before enrolment. Demographics, medical history, laboratory, and physical examination data were collected from clinical records of routine care visits. Data were available from routine follow-ups conducted every 12 months after implantation. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Consent for publication
Not applicable.
Conflicts of interest
The authors have no conflict of interest to declare.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Davtyan, K., Chugunov, I., Topchyan, A. et al. HF Etiology and cardiac contractility modulation therapy. BMC Cardiovasc Disord 24, 279 (2024). https://doi.org/10.1186/s12872-024-03950-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03950-8