Abstract
Introduction
Acute coronary syndrome (ACS) accounts for coronary artery disease (CAD) –related morbidity and mortality. There has been growing concern about the rising incidence of ACS among young individuals globally both in developed and developing countries, including Sub-Saharan Africa. This group’s phenotypic characteristics; risk factors and clinical outcomes are not well described. contextual and regional studies are necessary to understand the magnitude of ACS among young Individuals and help highlight challenges and opportunities for improved ACS outcomes in the region. The study aimed to describe the demographic and clinical characteristics of young individuals hospitalized with ACS and report on in-hospital outcomes.
Methodology
This single-center retrospective study was conducted at the Aga Khan University Hospital, Nairobi. Medical records of all young individuals hospitalized with ACS from 30th June 2020 to 1st May 2023 were reviewed. We defined young individuals as 50 years or below. Categorical variables were reported as frequencies and proportions, and compared with Pearson chi- square or Fisher’s exact tests. Continuous variables were reported as means or medians and compared with independent t-tests or Mann-Whitney U tests. P- value < 0.05 was considered statistically significant.
Results
Among 506 patients hospitalized with ACS, (n = 138,27.2%) were aged 50 years and below. The study population was male (n = 107, 79.9%) and African(n = 82,61.2%) predominant with a median age of 46.5 years (IQR 41.0–50.0). Hypertension (n = 101,75.4%) was noted in most study participants. More than half of the cohort were smokers (n = 69,51.5%) having a family history of premature ASCVD(n = 70,52.2%) and were on lipid-lowering therapy(n = 68,50.7%) prior to presentation. ST-segment–elevation myocardial infarction (STEMI) was the most common clinical manifestation of ACS (n = 77, 57.5%). Of the significant coronary artery disease (n = 75,56.0%), the majority of the individuals had single vessel disease (n = 60, 80%) with a predilection of left anterior deciding artery(n = 47,62.6%). The Main cause of ACS was atherosclerosis (n = 41,54.6%). The mean left ventricular ejection fraction was 46.0 (± 12.4). The in-hospital mortality was (n = 2, 1.5%).
Conclusion
This study highlights that young individuals contribute to a relatively large proportion of patients presenting with ACS at our center. The most common presentation was STEMI. The principal cause was atherosclerosis. The findings of this study highlight the importance of developing systems of care that enable the early detection of CAD. Traditional cardiovascular risk factors were prevalent and modifiable, thus targets of intervention.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) are the leading cause of mortality and loss of Disability Adjusted Life Years (DALYs) worldwide [1]. A substantial burden of it occurs in Low and Middle- income countries (LMICs) [2]. In Africa, CVDs are the most significant contributor to the total Non-Communicable Disease (NCD) burden [3, 4]. Acute coronary syndrome (ACS) accounts for coronary artery disease (CAD) related morbidity and mortality [3]. Growing evidence suggests that the incidence of ACS is increasing in Sub-Saharan Africa due to poorly controlled cardiovascular risk factors and rapid urbanization [5, 6]. While the incidence of ACS among the elderly has steadily decreased globally during the last decade, it has been more frequently diagnosed among young individuals in recent years [7, 8]. Similar trends have been reported in Sub-Saharan Africa (SSA), where it affects a relatively younger population [6]. These alarming trends merit particular attention as they may have a more significant economic, health, societal effect given the higher number of productive years of life at risk [9].
The global incidence of ACS among young individuals is difficult to establish due to its atypical presentation and variability in how it is reported in different healthcare systems [10]. Several large multicenter observational studies conducted outside the African continent have reported an incidence between 4–10% [8, 11,12,13,14,15,16]. Reports from Northern America, Europe, some parts of Asia have reported unique characteristics with distinct risk factors [14, 15, 17,18,19,20], clinical presentation [11], angiographic severity [16, 21,22,23], clinical outcomes [12, 14, 24] when compared to older patients. Nevertheless, the findings are not uniform and vary significantly across different cohorts. Despite the epidemiological transition, healthcare systems in Africa are traditionally geared towards addressing infectious diseases. Data on ACS is limited in the African continent and more so poorly reported in the young [6]. To date, no study has reviewed the spectrum of ACS among young individuals in Sub-Saharan Africa (SSA). Recent national reports indicate high CVD mortality in Kenya with more than 50% occurring prematurely [25].
In light of this background, we aimed to describe the clinical spectrum of ACS among young individuals in Kenya and elucidate prevalent risk factors. Insights gained from this report will identify prognostic characteristics and generate intervention targets.
Methods
Study design and settings
This was a single-center retrospective cohort study conducted at the Aga Khan University Hospital, Nairobi (AKUH, N). The AKUH, N is one of the largest private hospitals in the country with a current inpatient capacity of 289 beds. The Aga Khan University hospital Nairobi is the first hospital in Kenya to be accredited by the Joint Commission International (JCI) accreditation, USA and the only hospital in the region accredited for the management of heart attacks by JCI. This accreditation testifies commitment to provide quality patient care guided by patient safety standards aimed at good clinical outcomes. The inpatient cardiology section includes a 24-hour operational catherization laboratory and a 6 bed Coronary Care Unit (CCU) able to provide Level III [26] cardiovascular care with a 24-hour coverage by on call cardiology fellow and an interventional cardiologist. A 24 h back up cardiothoracic surgeon is available when the need arises. Patients admitted to the CCU receive a 1:1 nurse to patient care. The Cardiology section of the AKUHN is registered with Cardiovascular Data Registry (NCDR- CathPCI). The CathPCI is the American College of Cardiology (ACC) suite of data registries which help hospital’s improve quality of cardiovascular care they provide committed to ensuring evidence-based practice while improving patient outcomes. This powerful tool captures adherence to ACC/AHA clinical practice guideline recommendations, procedure performance standards and appropriate use criteria (AUC) for coronary revascularization. Data into the NCDR- CathPCI is entered by a designated research nurse and then verified by the interventional cardiologist for accuracy and completeness on a case to case basis. Variables (demographics, laboratory parameters, patient specific treatments, reperfusion strategies and in-hospital outcomes) collected are recommended by the ACC- NCDR- CathPCI [27].
Study population and sample size determination
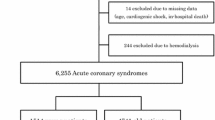
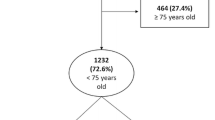
The current study involved extracting data from CathPCI registry of all the young individuals who presented with ACS from 1st June 2020 to 31st May 2023. We defined “young” with the age below 50 years. There has not been a universal consensus definition of young in regard to ACS but often considered reasonable and justified by various other studies for individuals below 50 years of age [9, 28,29,30]. All patients aged 50 years or below presenting with Acute Coronary Syndrome (ACS) were included in the study. Patients with complete missing medical records, transferred to other facilities and those leaving against medical advice were excluded from the study. The diagnosis of ACS was based on patients’ clinical signs and symptoms, electrocardiographic changes and elevation of cardiac - biomarkers [31]. Patients were grouped into two categories: (i) ST-elevation myocardial infarction (STEMI) and (ii)non-ST elevation Acute coronary Syndrome (NSTE- ACS) (Fig. 1). Evidence-based assessment, risk stratification and therapeutic strategy are followed by the institution as indicated in updated guidelines by American college of cardiology/ American Heart Association (ACC/AHA) [32, 33] Electrocardiograph (ECG) changes were documented according to the territory involved [34]. Experienced interventional cardiologists determined the cause of ACS according to previous validated methods [35, 36]. The angiographic characteristics were grouped into atherosclerotic [36], thrombotic [36] and spontaneous coronary artery dissection [35, 37]. Significant CAD was defined by invasive coronary angiography as a narrowing of the internal diameter > 50% stenosis of the left main stem and > 70% stenosis in a major coronary vessel [38]. Percentage diameter less than the mentioned above was characterized as non-obstructive coronary artery disease [39]. 2D echocardiography parameters prior to discharge were documented and confirmed by attending cardiologists. Left Ventricular function was classified as per the recommendations of the American Society of Echocardiography (ASE) [40].Patients were followed up to hospital discharge and grouped as alive or dead. The admission and CathPCI NCDR were used to identify patients who met the inclusion criteria.
Data management
All available data in paper-based and electronic format were obtained from the institutional medical records department. Data extracted included demographic characteristics, past medical history, underlying comorbid illness, symptoms on presentation, duration of symptoms, ACS diagnosis, angiographic findings and in- hospital outcome. Data were extracted by the primary investigator and randomly verified by a supervising faculty for accuracy and completeness. Data was collected in the MS Excel 2020.
The Study protocol was presented at the section level and department level before obtained ethical clearance from the Aga Khan university - Institution Scientific and Ethic Review Committee (ISERC). The study accepted by the Scientific and Ethic Review Committee (ISERC) of the Aga Khan University, Hospital Nairobi. Reference number Ref: AKU/2023/ISERC-65 (vl).
Data analysis
Data analysis was performed using R version 4.1.3 (2022-03-10). Categorical variables were reported as frequencies and percentages and compared with chi- squared or Fisher’s exact tests. Continuous variables were summarized descriptively as means or medians with the corresponding measures of variability and compared with t-tests or Mann-Whitney U tests. Statistical significance was set at P- Value < 0.05.
Results
A total of 506 patients presented with ACS during the study period, of which 138 patients met the inclusion criteria. 4 patients were excluded from the final analysis as seen in Fig. 1 above. The incidence of ACS among young individuals presenting to our institution was 27.2% (95% CI:22.8-30.5%).
The median age of our cohort was 46.5 years (IQR 41.0–50.0). Our cohort was male (n = 107,79.9%) and African predominant (n = 82, 61.2%) as seen in Table 1 below. The median BMI of our cohort was 29.6 Kg/m2 (IQR 26.0–32.0) of which only a fraction had a normal BMI (n = 15, 14.9%). The youngest patient was 31 years old.
More than one comorbid condition per patient was recorded when present. The most common comorbid condition amongst our cohort was hypertension (n = 101,75.4%). Approximately half of the study population were smokers(n = 69,51.5%), had a family history of premature ASCVD (n = 72,53.7%) and were on cholesterol-lowering medication (n = 68, 50.7%) prior to presentation. Among diabetic individuals (n = 58, 43.2%) the majority had suboptimal control with HbA1c above 7% (n = 33, 64.7%) as seen in Table 2 below.
The most common presentation was chest pain (n = 109,81.3%). The median duration of chest pain for patients with STEMI was (6.1 h, IQR 2–8) lower than those with NSTE- ACS (12 h, IQR 3.8–24). The Majority had no evidence of heart failure (n = 94, 70.1%) on presentation. Anterior- Septal was the most common ECG territory affected (n = 84, 62.6%) as seen in Table 3 below.
Significant coronary stenosis was identified in more than 50% of individuals (n = 75,56%), single vessel disease was the main coronary finding(n = 60,80%) with a predilection of the Left anterior descending artery(n = 42,62.6%). Atherosclerosis(n = 41,54.6%) of the coronary artery was the main cause of ACS in our cohort as seen in Table 4 below.
Patients with STEMI had a lower mean HDL when compared with patients with NSTEMI. Other Laboratory parameters are illustrated in Table 5 below.
Table 6 Below illustrates the reperfusion strategy among patients with STEMI. More than half (n = 52, 67.5%) underwent coronary intervention as illustrated below.
Table 7 below illustrates the type of Intervention and strategy performed among patients with NSTE - ACS. The most common strategy was intervention within the first 24 h (n = 40, 70.2%). More than half of the population did not require any form of revascularization (n = 32, 56.1%).
The Mean Left Ventricular Ejection fraction (LVEF) was 46.0 (± 12.4). Statistical significance was noted (P Value 0.05) when the mean LVEF of patients with STEMI and NSTE - ACS were compared as seen below in Table 8.
The median length of stay was 3 days (IQR 3.0–5.0). Prolonged hospital stay was noted in individuals with STEMI. The in-hospital mortality rate amongst our cohort was 1.5% as seen in Table 9 below.
Figure 2 below illustrates the organ support needed amongst our cohort. Inotropic support was the most frequently used organ support.
Discussion
To the best of our knowledge, we present one of the first studies to report on ACS among young individuals in the African continent. Findings from this study indicate that approximately 25% of patients hospitalized with ACS at our center were less than or equal to 50 years of age. This confirms a higher proportion compared to age- matched registry studies done in the Western world, which reported an incidence between 4 and 10% [8, 11,12,13,14,15,16]. We hypothesize the higher proportion to the increased prevalence of cardiovascular risk factors in our population, namely; diabetes mellitus, hypertension, obesity, and cigarette smoking. These factors are considered silent preventable killers and the main reasons for premature CAD globally and in SSA. Registry studies have documented the aforementioned to be highly prevalent in the East African region [41,42,43]. These observations support the present-day emphasis on controlling cardiovascular risk factors and quitting cigarette smoking to prevent adult coronary artery disease. Additionally, the presence of ASCVD risk enhancers [44] and presence of at risk population [45] in our cohort could account for a higher proportion of ACS among young individuals.
Despite differences in geographical and population dynamics. The demographic, clinical profile, risk, and sex distribution of our cohort are similar to studies conducted in Northern America, Asia, and Europe [11, 12, 46]. Our study population was male-predominant and followed a pattern observed in previous studies. Nonetheless, 20% of our patients were females; representing a higher percentage than observed by other comparable studies [11, 12]. Young women with ACS comprise an especially interesting group given the protective effect of estrogen. This paradox has been associated with: Psychosocial [17], abnormal menstrual cycle [18] and oral contraceptive use [47]. More importantly, few studies [30] have suggested sex- specific influence on ACS outcomes with young women having a higher 30-day mortality. The scope of our study and the small sample size limited us to explore this association in our cohort.
The study showed that majority of the individuals presented with classical chest pain as their main symptom. Young individuals are less likely to present with typical chest pain, a common symptomology of ACS [11]. Instead, they present with atypical symptoms such as awareness of heartbeat, nausea, fatigue, and dizziness [11]. These atypical presentations might account for the lower threshold of detection. Findings from our study describe a higher rate of STEMI as observed in various other age matched cohorts [12, 20, 48].
Cigarette smoking has been identified as the primary modifiable factor among young individuals in various populations [8, 14, 15] with a higher rate noted in the very young and linked with increased readmission rates, need for revascularization, and poor 5-year survival [15, 16]. Our results are parallel and depict similar trends with more than half of our cohort involved in cigarette smoking. Although dyslipidemia is an important risk factor for young, there seems to be little difference when compared to older patients. Several studies have reported increased triglyceride [19] and low HDL [19, 20] as the main factors associated with ACS in the young. Our study findings are comparable to reports published globally. Of note, approximately half of our cohort was already on cholesterol- lowering medications and yet presented with an acute coronary event suggesting failed appropriate primary or secondary prevention of ASCVD. This raises concern about either compliance among patients or incorrect doses of statins prescribed by healthcare workers, a major observation noted in clinical practice. Due to the study’s retrospective design, both mentioned parameters were not objectively assessed. Poor compliance and under-dosing of statin therapy predispose an individual to heightened cardiovascular risk, progression of coronary artery disease and increased health care costs [49]. These factors have been observed across patient subgroups (younger individuals) and by the intensity of statin therapy (high intensity) [50]. This analysis is therefore timely and creates a considerable opportunity for improvement in the primary prevention of ASCVD [50]. Furthermore, obesity appears to be an independent risk factor for premature coronary atherosclerosis especially, in young males [51], our cohort is a mere reflection of the at-risk population. Recent reports have indicated a better index [52] in predicting premature CAD than BMI and waist circumference and could be area of further research in different ethnic cohorts. Additionally, family history of premature ASCVD was a strong elucidated risk in our study population with reports validating it is a strong surrogate of premature ASCVD [53]. Polymorphism in novel genes among young individuals has been linked with the progression of atherosclerosis and CAD [52] with scientific evidence to support Lipoprotein a (LPa) measurement in identifying young individuals at heightened risk of premature ASCVD [54, 55].
Young Individuals presenting with ACS have a higher incidence of normal coronary arteries [23, 56] with only mild luminal narrowing. Our study findings contrast to what has been published globally and rather depict a higher frequency of angiographically significant coronary artery disease. The scope of the current study was beyond explaining the difference. A Strong family history of premature ASCVD and a higher prevalence of traditional and modifiable atherothrombotic risks may account for the disparity. The findings of predominately single vessel disease [12, 24] and predilection of Left Anterior Descending Artery (LAD) [16, 21] are in accord with previous studies. COVID − 19 myocarditis and vasospastic angina both mimic ACS in clinical presentation and might be accountable for our cohorts non - obstructive coronary artery disease.
The in-hospital mortality amongst our cohort was 1.5%. Due to the lower mortality rate, we couldn’t elucidate factors associated. Similar mortality rates have been documented in western series ranging between 0 to 4% [15, 16, 24]. The low in- hospital morality can be addressed in two folds. Firstly, Young individuals have favorable outcomes primarily due to the less advanced atherosclerosis and exhibit enhanced response to medical therapy. Additionally, besides, better physiological reserve and better collateral circulation better; the AKUHN has also heavily invested in care for patients with ACS. The AKUHN has been at the forefront of quality cardiac care for the past 10 years within the region.
Findings of the current study, add to the already existing knowledge. Data on the incidence of ACS especially among young adults are lacking and poorly documented in the Sub-Saharan region. This analysis presents a forward step in exploring the rising incidence of ACS among young individuals. To fully comprehend the effect of this syndrome; in detail, multi-center, case- control studies are needed with an exploration of contextual risk factors. The AKUHN follows protocols and guidelines from the European Society of Cardiology (ESC) and the American College of Cardiology (ACC) and there have been no major changes in the core components of the management of ACS from the recently ended ESC congress.
Limitations
The main purpose of this study was to understand the magnitude of ACS among young individuals in Kenya as well as to obtain contextual risks associated. Nonetheless, it has to be interpreted in light of some limitations. First, its retrospective design; which contained discharge level records and as such is inclined to missing data that hindered us exploring various variables such risk factors, biophysical profiles, several comorbidities, vitals on presentation, education level, marital status and ethnicity. However, We tried our best to extract as much as we could from medical records and databases available for consistent statistical analysis. Another limitation is the lack of a control group of older patients, nevertheless, this was never the primary objective of the study. Since global data on ACS among young is abundant we used it for reference and discussion. Despite the study setting severing more than 25% of heart attacks in Kenya, this was a single-center study conducted in a private hospital; thus, results cannot be generalized nationwide. An ACS diagnosis in young individuals could be challenging since myocarditis can mimic similar symptomatology leading to selection bias. Our data did not have data on the use of substances such as sympathomimetic amines [57] and khat consumption [58] which have been found to correlate with ACS, especially at a younger age. Finally, there is no universal definition of young patients, commonly accepted age range is below 50 years. This may be a confounding factor when comparing literature across various cohorts.
Future directions
The epidemiological profile of patients with Acute Myocardial Infarction (AMI) is changing and is now no longer the disease of the elderly requiring health care workers to become effective in diagnosing ACS in all patient population, regardless of age and sex. Moving Forward, sustained advocacy and investment in primordial and primary prevention of ASCVD is paramount and remains the beast weapon in resource limited setting. The African continent has witnessed a rapid surge in cardiovascular risk factors, especially in a much younger population. We feel, the region is unprepared for the growing burden with evident deficiencies in health care infrastructure. Findings from the studies should attract the community’s attention to seek a healthier life style and better control cardiovascular risk factors. The real time epidemiological transition calls out for a nation- wide implementation in formulating suitable strategies in identifying young individuals at heightened risk for death from CAD. These efforts are essential to offset the enormous costs associated with the care of premature ACS.
Conclusion
Young patients in Kenya contribute to a relatively large proportion of patients presenting with ACS. The majority were men, more than half of the cohort were cigarette smokers and overweight with a fraction having underlying diabetes mellitus and hypertension. Modifiable risk factors are targets of intervention for healthcare workers.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACS:
-
Acute Coronary Syndrome
- SSA:
-
Sub- Saharan Africa
- STEMI:
-
ST- Elevation Myocardial Infarction
- NSTEMI:
-
Non- ST Elevation Myocardial infarction
- LMICs:
-
Low Middle Income Countries
- CVD:
-
Cardiovascular Disease
- NCD:
-
• Non-Communicable Diseases
- • CAD:
-
Coronary Artery Disease
- AKUH, N:
-
Aga Khan University Hospital Nairobi
- JCI:
-
Joint Commission International
- NCDR:
-
National Cardiovascular Data Registry
- ACC:
-
American College of Cardiology
- CCU:
-
Coronary Care Unit
- AHA:
-
American Heart Association
- PCI:
-
Percutaneous Intervention
- ASE:
-
American Society of Echocardiography
- LVEF:
-
Left Ventricular Ejection Fraction
- PCI:
-
Percutaneous Coronary Intervention
References
Mengistu MD, Benti H. Assessment of magnitude and spectrum of cardiovascular disease admissions and outcomes in Saint Paul Hospital Millennium Medical College, Addis Ababa: a retrospective study. PLoS ONE. 2022;17(12):e0267527.
Bowry AD, Lewey J, Dugani SB, Choudhry NK. The Burden of Cardiovascular Disease in Low- and Middle-Income countries: Epidemiology and Management. Can J Cardiol. 2015;31(9):1151–9.
Bergmark BA, Mathenge N, Merlini PA, Lawrence-Wright MB, Giugliano RP. Acute coronary syndromes. Lancet. 2022;399(10332):1347–58.
Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115.
Onen CL. Epidemiology of ischaemic heart disease in sub-saharan Africa. Cardiovasc J Afr. 2013;24(2):34–42.
Yao H, Ekou A, Niamkey T, Hounhoui Gan S, Kouame I, Afassinou Y, et al. Acute Coronary syndromes in Sub-saharan Africa: a 10-Year systematic review. J Am Heart Assoc. 2022;11(1):e021107.
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–65.
Cole JH, Miller JI 3rd, Sperling LS, Weintraub WS. Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol. 2003;41(4):521–8.
Wu WY, Berman AN, Biery DW, Blankstein R. Recent trends in acute myocardial infarction among the young. Curr Opin Cardiol. 2020;35(5):524–30.
Vedanthan R, Seligman B, Fuster V. Global perspective on acute coronary syndrome: a burden on the young and poor. Circ Res. 2014;114(12):1959–75.
Doughty M, Mehta R, Bruckman D, Das S, Karavite D, Tsai T, et al. Acute myocardial infarction in the young–the University of Michigan experience. Am Heart J. 2002;143(1):56–62.
Fournier JA, Sanchez A, Quero J, Fernandez-Cortacero JA, Gonzalez-Barrero A. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. 1996;19(8):631–6.
Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction. An update on the Framingham study. N Engl J Med. 1984;311(18):1144–7.
Hoit BD, Gilpin EA, Henning H, Maisel AA, Dittrich H, Carlisle J, et al. Myocardial infarction in young patients: an analysis by age subsets. Circulation. 1986;74(4):712–21.
Zimmerman FH, Cameron A, Fisher LD, Ng G. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (coronary artery surgery Study Registry). J Am Coll Cardiol. 1995;26(3):654–61.
Wolfe MW, Vacek JL. Myocardial infarction in the young. Angiographic features and risk factor analysis of patients with myocardial infarction at or before the age of 35 years. Chest. 1988;94(5):926–30.
Chang PP, Ford DE, Meoni LA, Wang NY, Klag MJ. Anger in young men and subsequent premature cardiovascular disease: the precursors study. Arch Intern Med. 2002;162(8):901–6.
Hamelin BA, Methot J, Arsenault M, Pilote S, Poirier P, Plante S, et al. Influence of the menstrual cycle on the timing of acute coronary events in premenopausal women. Am J Med. 2003;114(7):599–602.
Malmberg K, Bavenholm P, Hamsten A. Clinical and biochemical factors associated with prognosis after myocardial infarction at a young age. J Am Coll Cardiol. 1994;24(3):592–9.
Chen L, Chester M, Kaski JC. Clinical factors and angiographic features associated with premature coronary artery disease. Chest. 1995;108(2):364–9.
Davia JE, Hallal FJ, Cheitlin MD, Gregoratos G, McCarty R, Foote W. Coronary artery disease in young patients: arteriographic and clinical review of 40 cases aged 35 and under. Am Heart J. 1974;87(6):689–96.
McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki Disease: A Scientific Statement for Health professionals from the American Heart Association. Circulation. 2017;135(17):e927–99.
Gurevitz O, Jonas M, Boyko V, Rabinowitz B, Reicher-Reiss H. Clinical profile and long-term prognosis of women < or = 50 years of age referred for coronary angiography for evaluation of chest pain. Am J Cardiol. 2000;85(7):806–9.
Porter A, Wurzel M, Ben-Gal T, Sulkes J, Sagie A. Long-term prognosis of 210 patients who underwent coronary angiography before 40 years of age. Am J Cardiol. 1998;81(9):1168–70.
Mbau L, Fourie JM, Scholtz W, Scarlatescu O, Nel G, Gathecha G. PASCAR and WHF Cardiovascular diseases Scorecard project. Cardiovasc J Afr. 2021;32(3):161–7.
Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and critical Care Medicine. J Crit Care. 2017;37:270–6.
Nelson AJ, Inohara T, Rao SV, Kaltenbach LA, Wojdyla D, Wang TY. Comparing the classification of Percutaneous Coronary interventions using the 2012 and 2017 appropriate Use Criteria: insights from 245,196 patients in the NCDR CathPCI Registry. Am Heart J. 2023;255:117–24.
Gulati R, Behfar A, Narula J, Kanwar A, Lerman A, Cooper L, et al. Acute myocardial infarction in Young individuals. Mayo Clin Proc. 2020;95(1):136–56.
Egred M, Viswanathan G, Davis GK. Myocardial infarction in young adults. Postgrad Med J. 2005;81(962):741–5.
Ricci B, Cenko E, Vasiljevic Z, Stankovic G, Kedev S, Kalpak O et al. Acute Coronary Syndrome: the risk to Young Women. J Am Heart Assoc. 2017;6(12).
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of Acute Coronary syndromes: a review. JAMA. 2022;327(7):662–75.
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, AHA/ACC/ASE/CHEST et al. /SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454.
Devon HA, Rosenfeld A, Steffen AD, Daya M. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J Am Heart Assoc. 2014;3(2):e000586.
Sattar Y, Chhabra L, Electrocardiogram. StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Lovely Chhabra declares no relevant financial relationships with ineligible companies.2023.
Hayes SN, Kim ESH, Saw J, Adlam D, Arslanian-Engoren C, Economy KE, et al. Spontaneous coronary artery dissection: current state of the Science: A Scientific Statement from the American Heart Association. Circulation. 2018;137(19):e523–57.
Shibata T, Kawakami S, Noguchi T, Tanaka T, Asaumi Y, Kanaya T, et al. Prevalence, clinical features, and prognosis of Acute myocardial infarction attributable to coronary artery embolism. Circulation. 2015;132(4):241–50.
Tweet MS, Olin JW, Bonikowske AR, Adlam D, Hayes SN. Physical activity and exercise in patients with spontaneous coronary artery dissection and fibromuscular dysplasia. Eur Heart J. 2021;42(37):3825–8.
Neglia D, Rovai D, Caselli C, Pietila M, Teresinska A, Aguade-Bruix S et al. Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging. 2015;8(3).
Dees D, Rahimi F, Amann M, Nuhrenberg TG, Loffelhardt N, Schmitz R et al. Prevalence and causes of myocardial infarction with non-obstructive coronary arteries in a contemporary cohort of patients with suspected myocardial infarction. J Clin Med. 2021;10(21).
Kosaraju A, Goyal A, Grigorova Y, Makaryus AN. Left ventricular ejection Fraction. StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Amandeep Goyal declares no relevant financial relationships with ineligible companies. Disclosure: Yulia Grigorova declares no relevant financial relationships with ineligible companies. Disclosure: Amgad Makaryus declares no relevant financial relationships with ineligible companies.2023.
Okello S, Muhihi A, Mohamed SF, Ameh S, Ochimana C, Oluwasanu AO, et al. Hypertension prevalence, awareness, treatment, and control and predicted 10-year CVD risk: a cross-sectional study of seven communities in East and West Africa (SevenCEWA). BMC Public Health. 2020;20(1):1706.
Azevedo M, Alla S. Diabetes in sub-saharan Africa: Kenya, Mali, Mozambique, Nigeria, South Africa and Zambia. Int J Diabetes Dev Ctries. 2008;28(4):101–8.
Ekpor E, Akyirem S, Adade Duodu P. Prevalence and associated factors of overweight and obesity among persons with type 2 diabetes in Africa: a systematic review and meta-analysis. Ann Med. 2023;55(1):696–713.
Georgiopoulos G, Delialis D, Aivalioti E, Georgakis V, Mavraganis G, Angelidakis L, et al. Implementation of risk enhancers in ASCVD risk estimation and hypolipidemic treatment eligibility: a sex-specific analysis. Hellenic J Cardiol. 2023;73:16–23.
Mangalmurti SS, Paley A, Gany F, Fisher EA, Hochman JS. South asians and risk of cardiovascular disease: current insights and trends. Ethn Dis. 2010;20(4):474–8.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24(1):239.
Petitti DB, Sidney S, Quesenberry CP. Oral contraceptive use and myocardial infarction. Contraception. 1998;57(3):143–55.
Klein LW, Agarwal JB, Herlich MB, Leary TM, Helfant RH. Prognosis of symptomatic coronary artery disease in young adults aged 40 years or less. Am J Cardiol. 1987;60(16):1269–72.
Razavi AC, Mehta A, Sperling LS. Statin therapy for the primary prevention of cardiovascular disease: pros. Atherosclerosis. 2022;356:41–5.
Rodriguez F, Maron DJ, Knowles JW, Virani SS, Lin S, Heidenreich PA. Association of Statin Adherence with mortality in patients with atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2019;4(3):206–13.
McGill HC Jr., McMahan CA, Herderick EE, Zieske AW, Malcom GT, Tracy RE, et al. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation. 2002;105(23):2712–8.
Aggarwal A, Srivastava S, Velmurugan M. Newer perspectives of coronary artery disease in young. World J Cardiol. 2016;8(12):728–34.
Bao W, Srinivasan SR, Wattigney WA, Berenson GS. The relation of parental cardiovascular disease to risk factors in children and young adults. Bogalusa Heart Study Circulation. 1995;91(2):365–71.
Enas EA, Varkey B, Dharmarajan TS, Pare G, Bahl VK. Lipoprotein(a): an underrecognized genetic risk factor for malignant coronary artery disease in young indians. Indian Heart J. 2019;71(3):184–98.
Raitakari O, Kartiosuo N, Pahkala K, Hutri-Kahonen N, Bazzano LA, Chen W, et al. Lipoprotein(a) in Youth and Prediction of Major Cardiovascular outcomes in Adulthood. Circulation. 2023;147(1):23–31.
Sullivan AK, Holdright DR, Wright CA, Sparrow JL, Cunningham D, Fox KM. Chest pain in women: clinical, investigative, and prognostic features. BMJ. 1994;308(6933):883–6.
Qureshi AI, Suri MF, Guterman LR, Hopkins LN. Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: data from the Third National Health and Nutrition Examination Survey. Circulation. 2001;103(4):502–6.
Al-Motarreb A, Al-Suwaidi J. Khat Chewing and Cardiovascular Disease. Heart Views. 2022;23(2):103–7.
Acknowledgements
We want to thank the medical records of the Aga Khan University hospital Nairobi for their support in the successful completion of the research. We also like to thank Mr. James Orwa for his time and knowledge to towards the successful end of this project.
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
NK and MV drafted the original research protocol.MN,JM reviewed the study design. MM assisted in the collection of data. All authors made an important and substantial contribution to the conception, study design, execution, acquisition of data, analysis, interpretation and implementation. All authors equally contributed in writing, revising, and critically revising the article. All authors approved the final document to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was presented to the section of cardiology and accepted by the Scientific and Ethic Review Committee (ISERC) of the Aga Khan University, Hospital Nairobi. Reference number Ref: AKU/2023/ISERC-65 (vl). The Institution Scientific and Ethic Review Committee (ISERC) of the Aga Khan University Hospital, Nairobi exempted individual Informed consent from study participants as the study design was purely based on extracting data from a registry and did not affect the rights and welfare of the patients. The study was conducted in line with principals of the Aga Khan university Hospital Nairobi.
Consent for publication
Not applicable.
Conflict of interest
The authors report no conflict on interest in this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kassam, N., Ngunga, M., Varwani, M. et al. Acute coronary syndrome patterns in the Young: risk factor profile and in-hospital outcomes in a tertiary referral hospital in Kenya. BMC Cardiovasc Disord 24, 192 (2024). https://doi.org/10.1186/s12872-024-03832-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03832-z