Abstract
Background and aims
The present study aimed to investigate the predictive ability of selected adiposity indices, such as body mass index (BMI), waist-to-hip ratio (WHR), waist circumference (WC), and waist-to-height ratio (WHtR), for new-onset hypertension in metabolically healthy Taiwanese adults. The study also sought to establish sex-specific cutoff points for these indices and to analyze the risk of new-onset hypertension, taking into account sex and age.
Methods
This prospective cohort study utilized the Taiwan Biobank database to examine metabolically healthy participants aged between 20 and 65 at baseline. Four adiposity indices, namely BMI, WHR, WC, and WHtR, were calculated and used to predict new-onset hypertension over 4 years. Receiver operating characteristics (ROCs) and areas under the curve (AUCs) were used to evaluate the effectiveness of the parameters in predicting new-onset hypertension over 4 years. Sex-specific cutoff points were identified and used to assess the risk of new-onset hypertension.
Results
This study analyzed 13,375 participants over 4.28 years. The incidence of new-onset hypertension was 17.65%. The new-onset rate of hypertension was 34.39% in men and 65.61% in women. Adiposity indices effectively predict new-onset hypertension, with WHtR having the highest predictive value (i.e., AUC) for both sexes. The classification of participants into low and high categories for each adiposity index was based on sex-specific cutoff points, and the risk of new-onset hypertension was assessed according to sex and age. This study found that high adiposity indices predicted a significantly higher risk of new-onset hypertension in metabolically healthy adults. The risk was equal for both sexes. Young women had a higher risk of new-onset hypertension than middle-aged women when they were further categorized. All risk ratios of the indices in young women were over two-fold and significant.
Conclusion
According to the sex-specific cutoff point, high adiposity indices had a higher predictive value for new-onset hypertension in metabolically healthy Taiwanese young women.
Similar content being viewed by others
Introduction
Hypertension is a significant contributor to cardiovascular mortality and morbidity, responsible for approximately half of such incidence [1]. Early screening and prevention programs can effectively reduce the burden of hypertension, which is a preventable cardiovascular risk factor [2]. The prevalence of hypertension varies by age, sex, and ethnicity, with Asia, particularly Southeast, South, and East Asia, having a high prevalence of the condition [3, 4]. The prevalence of hypertension in Taiwan reached 20.8%, as reported by the National Health and Nutrition Examination Survey (NHANES), conducted from 2013 to 2016 [5].
Excess adiposity is a significant risk factor for hypertension, and weight reduction is often included in blood pressure-lowering treatment [6,7,8]. In assessing excess adiposity, imaging modalities provide detailed information on the composition of excess adiposity. However, anthropometric adiposity indices are still preferred in clinical practice because of their convenience [9]. Clinical practice employs various adiposity indices, including the body mass index (BMI), waist-to-hip ratio (WHR), waist circumference (WC), and waist-to-height ratio (WHtR) [10, 11]. These parameters have been established as predictors of cardiometabolic risk, specifically hypertension [12, 13].
Adiposity can induce a rise in blood pressure without prior metabolic abnormalities through neurohumoral and renal mechanisms [14]. The mechanism of adiposity-induced hypertension also differed among sexes, mainly due to differences in hormonal regulation, sympathetic nervous system, and renin–angiotensin–aldosterone regulation [15, 16]. Sex should be considered when predicting hypertension through excess adiposity.
Additionally, adiposity's crucial role in identifying individuals who transition from metabolically healthy to metabolically unhealthy has also been highlighted [17,18,19,20]. The accumulation of adipose tissue, especially visceral fat, is often the first manifestation of metabolic disorders. In a 5-year follow-up study, researchers found that the younger the age at which adults became overweight, the higher their risk of developing high blood pressure. The group with the highest relative risk was those who became overweight between the ages of 18 and 39, with overweight being the only risk factor for these subjects [21]. This shows the importance of detecting early obesity in metabolically healthy individuals. Consequently, the impact of excess adiposity on predicting hypertension in metabolically healthy individuals requires further investigation, particularly considering age and sex.
The aims of this study were twofold: (1) to investigate the predictive power of selected adiposity indices, including BMI, WHR, WC, and WHtR, and to establish sex-specific cutoff points for these indices about new-onset hypertension among metabolically healthy Taiwanese adults; and (2) to evaluate the risk of new-onset hypertension in metabolically healthy Taiwanese adults by utilizing these adiposity indices, taking into account age and sex.
Materials and methods
Study design and population
This prospective cohort study included participants selected from the Taiwan Biobank (TWB) database. The TWB is a significant genomic database for Chinese populations, containing extensive demographic and health-related survey data, physical measurements, biochemical data, and genomic data, all aimed at enhancing the capability of clinicians to prescribe personalized and precise medication in Taiwan [22, 23]. All patients submit written informed consent before being enrolled in the TWB [24]. The Taipei Medical University Institutional Review Board (number N202104112) approved the study after receiving clearance.
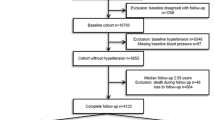
In this study, the population is the individuals with two interviews, those between 20 and 65 years of age, who were metabolically healthy at baseline. Participants with a history of self-reported coronary artery disease, stroke, hyperlipidemia, hypertension, or gout at baseline were excluded. Of the 14,141 participants who fulfilled the inclusion criteria, 62 reported a history of coronary artery disease, 417 had hyperlipidemia, 24 had a history of stroke, 201 had gout, and none had hypertension. Moreover, 96 subjects who had missing data for blood pressure measurements and/or self-reported hypertension status during the first follow-up (loss to follow-up) were excluded from the study. A total of 13,375 participants were included in this study (Fig. 1).
Data collection
Questionnaires, blood samples, and physical examinations were collected. Age, sex, menopausal status, self-reported smoking status, and alcohol consumption were recorded. Smoking status was divided into three categories: never/occasional, quitting, and still smoking. Alcohol consumption was divided into three categories: never/occasional drinking, quitting drinking, and drinking.
Blood pressure measurements were performed on the right upper arm, with the patient sitting, using a sphygmomanometer after a 5-min rest. Average systolic blood pressure (SBP) and diastolic blood pressure (DBP) were used in the analysis. A calibrated body scale measured the weight (kg) and height (cm). Waist circumference (WC; cm) was measured around the abdomen immediately superior to the iliac crest. Hip circumference (HC; cm) was the largest circumference across the buttock.
Fasting blood samples were collected from the antecubital vein. Fasting plasma glucose (FPG; mg/dL), triglyceride (TG; mg/dL), total cholesterol (TC; mg/dL), and high-density lipoprotein cholesterol (HDL-C; mg/dL) levels were measured using an autoanalyzer (COBAS Integra 400, Roche Diagnostics, Mannheim, Germany).
Definitions of metabolic health
In our study, four metabolic indicators were considered: (1) SBP ≥ 130 mmHg or DBP ≥ 80 mmHg; (2) elevated fasting glucose levels (≥ 100 mg/dL); (3) raised triglycerides (≥ 150 mg/dL); and (4) reduced HDL-C (< 40 mg/dL in men and < 50 mg/dL in women) [25, 26]. A metabolically healthy individual has none of these four metabolic indicators [27].
Determining adiposity indices
BMI, WHR, and WHtR were calculated using the following formulas [28, 29]:
Outcome definition
The follow-up duration was calculated from baseline to the first follow-up. The outcome was the presence of new-onset hypertension, which is defined as SBP ≥ 130 mmHg or DBP ≥ 80 mmHg or self-reported hypertension in the first follow-up (the criteria of hypertension of the 2022 Guidelines of the Taiwan Society of Cardiology or the Taiwan Hypertension Society for the Management of Hypertension) [26].
Statistical analysis
All statistical computations were performed using the SAS software (version 9.4; SAS Institute, Cary, NC, USA). Continuous variables are presented as means ± standard deviations and were tested using the t-test. Categorical variables are presented as numbers (percentages) and tested using the chi-square test.
Receiver operating characteristics (ROCs) and areas under the curve (AUCs) were used to assess the classification fitness of each index for hypertension. The ROC curves of the four indices were compared using the Wald test. The cutoff points for each index were determined using the maximal Youden index (J), calculated as sensitivity + specificity − 1 [30]. We then divided the participants into lower and upper groups based on the cutoff value.
The risk ratios (RRs) of hypertension for the upper cutoff group were compared with those for the lower cutoff group using binomial logistic regression (PROC GENMOD statement in SAS). The hypertension models were stratified by sex and age. Two age groups were: a young-adult (20–45 years old) group and a middle-aged-adult (46–65 years old) group [31]. Forrest plots were generated using Medcalc Software to visualize the RRs.
Results
Baseline characteristics
Following the exclusion of ineligible participants, 13,375 were included in the analysis, as depicted in Fig. 1. The median follow-up period in participants was 4.28 years. The average age was 46.67 years, with women comprising 76.96% of the total population. There were 2631 cases (17.65%) of new-onset hypertension. The new-onset rate of hypertension was 34.39% in men and 65.61% in women. The mean values of the adiposity indices were 22.39 kg/m2 for BMI, 0.83 for WHR, 78.04 cm for WC, and 0.49 for WHtR. The distribution of these indices is shown in Figure S1 in the Supplementary Materials.
Participants with new-onset hypertension tended to have higher adiposity indices. Metabolic parameters such as FPG, TG, and TC were higher in patients with new-onset hypertension, and HDL-C was lower than in those without hypertension. Other risk factors appeared to differ significantly between the two groups (Table 1). As the population was dominated by women (76.76%), the baseline characteristics of the subjects were also assessed according to sex.
The mean values of adiposity indices were found to be higher in men, except for WHtR, which was similar between men and women (0.48 vs. 0.49, p = 0.08). Men demonstrated higher levels of FPG and TG and lower levels of TC and HDL-C than women. Additionally, men had higher baseline SBP and DBP values than women (SBP 110.6 vs. 105.4 mmHg, p < 0.0001; DBP 69.65 vs. 65.28 mmHg, p < 0.0001). Furthermore, a greater proportion of men reported smoking and alcohol consumption habits, whereas there were no significant differences in exercise habits between the sexes.
Classification of adiposity indices for predicting new-onset hypertension
The receiver operating characteristic curves (ROCs) and area under the curves (AUCs) are shown in Fig. 2 and Table 2. In general, adiposity indices have demonstrated the ability to predict new-onset hypertension (AUC 0.58–0.66). Specifically, WHtR showed a higher AUC than the other indices among men and women tested using the Wald test. These differences remained significant even after adjusting for multiple covariates (Table 2, Model 2).
Receiving Operating Characteristics (ROC) of adiposity indices for new-onset hypertension in metabolically healthy adults. Model 1 was unadjusted; Model 2 was adjusted for age, total cholesterol, smoking status, alcohol consumption and menopausal status (for women). BMI, body mass index; WHR, waist-to-hip ratio; WC, waist circumference; WHtR, waist-to-height ratio
Sensitivity, specificity and cutoff points of adiposity indices in metabolically healthy adults
Table 3 presents the cutoff points of the adiposity indices in both men and women. The WC and WHR’s cutoff points were higher in men than in women (WHR 0.87 vs. 0.82; WC 82 cm vs. 76.8 cm), whereas BMI (23.59 kg/m2 vs. 23.20 kg/m2) and WHtR (0.49 vs. 0.48) were similar in both sexes. The cutoff point of waist circumference (WC) in men demonstrated the highest sensitivity (67%), while the waist-to-hip ratio (WHtR) showed the highest specificity (63%). In addition, the WHtR cutoff point in women was associated with the highest sensitivity (71%), whereas body mass index (BMI) had the highest specificity (73%).
The cutoff points for new-onset hypertension according to age in the metabolically healthy population are presented in Table S1 in the supplementary materials. According to age, WHR and WHtR showed similar cutoff points among age categories, whereas BMI had higher cutoff points in middle age and WC had higher cutoff points in young adults.
The risk of new-onset hypertension was found to differ between individuals in the high and low categories based on sex-specific cutoff points. In particular, four adiposity indices revealed higher risks for women than men, although the differences were not statistically significant. However, the risk differences between men and women decreased in the adjusted model (Model 2) (see Fig. 3).
The sex-stratified new-onset hypertension risk in metabolically healthy adults determined using adiposity indices. Model 1 was unadjusted; Model 2 was adjusted for age, total cholesterol, smoking status, alcohol consumption and menopausal status (for women). BMI, body mass index; WHR, waist-to-hip ratio; WC, waist circumference; WHtR, waist-to-height ratio
We extended our analysis to encompass age, examining the new-onset hypertension risk assessed by adiposity indices for both men and women in the young and middle-aged populations. Our research determined that young women had a significantly higher risk of developing new-onset hypertension when compared to middle-aged women when utilizing BMI, WC, and WHtR as adiposity indices (unadjusted: BMI RR = 2.58, 95%CI: 2.15–3.09, p < 0.0001 vs 1.70, 95%CI 1.53–1.88, p < 0.0001; WC RR = 2.40, 95%CI: 1.98–2.90, p < 0.0001 vs 1.61, 95%CI 1.44.-1.80, p < 0.0001; WHtR RR = 2.51, 95%CI: 2.07–3.04, p < 0.0001 vs 1.69, 95%CI 1.51–1.91,p < 0.0001; adjusted: BMI RR = 2.58, 95%CI: 2.13–3.11, p < 0.0001 vs 1.69, 95%CI 1.52–1.88,p < 0.0001; WC RR = 2.40, 95%CI: 1.96–2.92, p < 0.0001 vs 1.58, 95%CI 1.41–1.76, p < 0.0001; WHtR RR = 2.46, 95%CI: 2.01–3.00, p < 0.0001 vs 1.66, 95%CI 1.48–1.88, p < 0.0001). In the unadjusted model utilizing waist circumference (WC), a substantial increase in the risk of hypertension was observed among young men compared with middle-aged men (young men RR = 2.13, 95%CI: 1.72–2.63, p < 0.0001 vs middle-aged men RR = 1.46, 95%CI: 1.25–1.71, p < 0.0001). Additionally, for other adiposity indices, no significant differences in risk were observed between young and middle-aged men. When comparing the various age categories, young and middle-aged women exhibited a similar risk of hypertension compared to their respective male counterparts, as depicted in Fig. 4.
The age- and sex- stratified new-onset hypertension risk in metabolically healthy adult determined using adiposity indices. Model 1 was unadjusted; Model 2 was adjusted for age, total cholesterol, smoking status, alcohol consumption and menopausal status (for women). BMI, body mass index; WHR, waist-to-hip ratio; WC, waist circumference; WHtR, waist-to-height ratio
Discussion
This prospective cohort study highlighted the effectiveness of adiposity indices (BMI, WHR, WC, and WHtR) for independently predicting new-onset hypertension in metabolically healthy adults in both unadjusted and adjusted models. Although there is still controversy surrounding which adiposity indices have the best performance for predicting new-onset hypertension, our findings showed that the WHtR had the highest prediction performance among adiposity indices in both sexes, which is consistent with several previous studies. Lin et al. reported that the WHtR was an ideal indicator for screening cardiovascular disease risk factors, particularly for hypertension; the AUCs of the WHtR were 0.658 for men and 0.752 for women [32].
A systematic review and meta-analysis of the potential screening ability of the WHtR reported that the WHtR had a higher discriminative power for cardiometabolic risk (4%–5%) than BMI and WC did.[33] Choi JR. et al. reported that WHtR improved hypertension prediction of age, sex, and SBP (AUC age + sex + SBP 0.675; AUC age + sex SBP + WHtRR 0.722, p = 0.001) [34]. Since WHtR was one of the parameter reflecting central adiposity, this result also emphasized stronger effect of central adiposity toward hypertension [35, 36]. The potential explanation on how including an individual’s stature when analyzing central adiposity can improve its discriminative power for hypertension was because of the effects of stature on vascular function and fat distribution [37, 38]. Moreover, short stature is associated with higher central adiposity and lower vasculature diameter resulting in high blood pressure level [33, 37, 38].
The optimal sex cutoff points for predicting new-onset hypertension in our study were calculated using the maximal Youden Index method. The cutoff points for BMI were 23.59 kg/m2 for men and 23.20 kg/m2 for women. In the previous study, the BMI cutoff points for hypertension were 23.9 kg/m2 for men and 22.5 kg/m2 for women [32]. WHO (World Health Organization) also set a 23 kg/m2 threshold to predict hypertension in the Asia Pacific population [39]. The cutoff points for WHR in this study were 0.87 for men and 0.82 for women, comparable with a similar study conducted using the Taiwanese population, 0.86 for men and 0.77 for women [32]. The WC cutoff point for men was 82 cm, and for women, it was 76 cm. The threshold was similar for men compared to the previous study using the Taiwanese population, which was 81.5 cm, and higher in women compared to the same study, which was 72.5 cm [32]. The WHtR cutoff points were similar between men (0.49) and women (0.48). This finding was similar to a prior study, which had cutoff points of 0.48 for men and 0.46 for women, and also other kinds of literature that set up a threshold for WHtR in 0.5 for both sexes to predict cardiometabolic disease, including hypertension [32, 34, 40, 41].
Our study observed that the cutoff points for BMI, WC, and WHR among men were comparable to those of the general Taiwanese population. However, the cutoff points for women were higher for all three adiposity indices. These results add to the evidence suggesting a greater impact of metabolic status on women than men. Additionally, our study verified the consistency of the WHtR cutoff point (0.5) for hypertension prediction in metabolically healthy Taiwanese adults since the cutoff points remain stable among sexes and age categories.
In this study, men had a higher incidence of new-onset hypertension than women did. However, prediction using sex-specific cutoff points of adiposity indices carried a similar risk of new-onset hypertension in both sexes, even after multivariable adjustment. This finding underlined that the burden of excess adiposity in women was equal to that in men, and sex-specific factors played an important role in the mechanism of adiposity-related hypertension. Gender, sociocultural, environmental, and psychological factors have complex interactions underlying the differential impact of excess adiposity between the sexes [42]. Besides sex hormones, women's sedentary lifestyle, unhealthy diet, and stress increase the impact of excess adiposity, especially on cardiometabolic diseases [43].
When stratified by sex and age, young women with excess adiposity had a significantly higher risk of hypertension than middle-aged women. Previous research has confirmed that young adults have the highest risk of weight gain and metabolic consequences [44,45,46]. Among cardiometabolic risk factors, high WC and high BMI had a stronger link to increased high sensitivity C-reactive protein (hs-CRP) in young adults [46]. According to the results of our study, young women, who are believed to be protected by estrogen, are at a higher risk of developing new-onset hypertension than middle-aged women, and their risk is comparable to that of young men.
Previous reports have suggested that in younger adults, men have higher blood pressure than women and that women’s blood pressure tends to increase more rapidly during midlife, eventually surpassing that of men [47,48,49]. These phenomena observed indicate that the protective effects of estrogen decrease during midlife [50]. However, this new information contradicts those reports and states the opposite. Therefore, it is essential to carefully consider the new-onset hypertension risk faced by young women. One possible explanation for the higher risk of new-onset hypertension in young women is alteration of sex-hormone regulation and protective effect by excessive and malfunctioning adipose tissue, as predicated by adiposity indices [51, 52]. It has been suggested that early menarche in women may be linked to excess body fat in young women [53, 54]. Nonetheless, the exact mechanism by which excess adiposity leads to new-onset hypertension is complex and involves multiple factors. Further research is needed to identify the specific pathological pathways involved in adiposity-related hypertension in women.
Our study has several strengths, including the use of a large prospective cohort and adequate follow-up. This is the first study to investigate the predictive performance of adiposity indices for new-onset hypertension in metabolically healthy Taiwanese adults. Despite these strengths, our study had some limitations. First, we did not collect data regarding therapy for cardiometabolic diseases, which may have affected our results. Second, our study lacked exact data on antihypertensive therapy and drug use and may have been influenced by recall bias due to our inclusion of patients with self-reported hypertension. Finally, our study used office blood pressure measurements, meaning masked hypertension may not have been detected.
In summary, a high level of adiposity index, as determined by sex-specific cutoff points, indicates a higher risk of new-onset hypertension in metabolically healthy Taiwanese adults. It is worth noting that young women should be a particular concern as they have a significantly greater risk of new-onset hypertension compared to middle-aged adults, and their risk is comparable to that of young men.
Availability of data and materials
The dataset used in the current study is available at the request of the corresponding author (baich@tmu.edu.tw).
Abbreviations
- BMI:
-
Body mass index
- WHR:
-
Waist-to-hip ratio
- WC:
-
Waist circumference
- WHtR:
-
Waist-to-height ratio
- FPG:
-
Fasting plasma glucose
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TWB:
-
Taiwan Biobank
References
Zhou D, Xi B, Zhao M, Wang L, Veeranki SP. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: the NHANES III Linked Mortality Study. Sci Rep. 2018;8(1):9418.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 InternationalSociety of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334–57.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18(11):785–802.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–37.
Pan HY, Lin HJ, Chen WJ, Wang TD. Prevalence, Treatment, Control and Monitoring of Hypertension: A Nationwide Community-Based Survey in Taiwan, 2017. Acta Cardiol Sin. 2020;36(4):375–81.
Stenehjem JS, Hjerkind KV, Nilsen TIL. Adiposity, physical activity, and risk of hypertension: prospective data from the population-based HUNT Study Norway. J Hum Hypertens. 2018;32(4):278–86.
Ahmadi MN, Lee IM, Hamer M, Del Pozo CB, Chen LJ, Eroglu E, et al. Changes in physical activity and adiposity with all-cause, cardiovascular disease, and cancer mortality. Int J Obes (Lond). 2022;46(10):1849–58.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42(5):878–84.
Cornier MA, Despres JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019.
Powell-Wiley TM, Poirier P, Burke LE, Despres JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2021;143(21):e984–1010.
Sommer I, Teufer B, Szelag M, Nussbaumer-Streit B, Titscher V, Klerings I, et al. The performance of anthropometric tools to determine obesity: a systematic review and meta- analysis. Sci Rep. 2020;10(1):12699.
Tian T, Zhang J, Zhu Q, Xie W, Wang Y, Dai Y. Predicting value of five anthropometric measures in metabolic syndrome among Jiangsu Province, China. BMC Public Health. 2020;20(1):1317.
Sheppard JP, Fletcher B, Gill P, Martin U, Roberts N, McManus RJ. Predictors of the Home- Clinic Blood Pressure Difference: A Systematic Review and Meta-Analysis. Am J Hypertens. 2016;29(5):614–25.
Hall JE. Carmo JMd, Silva AAd, Wang Z, Hall ME. Obesity-Induced Hypertension. Circ Res. 2015;116(6):991–1006.
Shi Z, Wong J, Brooks VL. Obesity: sex and sympathetics. Biol Sex Differ. 2020;11(1):10.
Faulkner JL, Belin de Chantemele EJ. Sex Differences in Mechanisms of Hypertension Associated With Obesity. Hypertension. 2018;71(1):15–21.
Lei L, Changfa W, Ting Y, Xiaoling Z, Yaqin W. Metabolically healthy transition and association with body size change patterns among different adult age groups. Diabetes Res Clin Pract. 2022;192:110108.
Wijayatunga NN, Dhurandhar EJ. Normal weight obesity and unaddressed cardiometabolic health risk-a narrative review. Int J Obes (Lond). 2021;45(10):2141–55.
Schulze MB. Metabolic health in normal-weight and obese individuals. Diabetologia. 2019;62(4):558–66.
Stefan N, Schick F, Häring H-U. Causes, Characteristics, and Consequences of Metabolically Unhealthy Normal Weight in Humans. Cell Metab. 2017;26(2):292–300.
Li W, Fang W, Huang Z, Wang X, Cai Z, Chen G, et al. Association between age at onset of overweight and risk of hypertension across adulthood. Heart. 2022;108(9):683–8.
Chen CH, Yang JH, Chiang CWK, Hsiung CN, Wu PE, Chang LC, et al. Population structure of Han Chinese in the modern Taiwanese population based on 10,000 participants in the Taiwan Biobank project. Hum Mol Genet. 2016;25(24):5321–31.
Lu MY, Cheng HY, Lai JC, Chen SJ. The Relationship between Habitual Coffee Drinking and the Prevalence of Metabolic Syndrome in Taiwanese Adults: Evidence from the Taiwan Biobank Database. Nutrients. 2022;14(9).
Fan C-T, Hung T-H, Yeh C-K. Taiwan Regulation of Biobanks. J Law Med Ethics. 2015;43(4):816–26.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5.
Wang TD, Chiang CE, Chao TH, Cheng HM, Wu YW, Wu YJ, et al. 2022 Guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the Management of Hypertension. Acta Cardiol Sin. 2022;38(3):225–325.
Candi E, Campanelli M, Sica G, Schinzari F, Rovella V, Di Daniele N, et al. Differences in the vascular and metabolic profiles between metabolically healthy and unhealthy obesity. Endocrine and Metabolic Science. 2021;2.
Lechner K, Lechner B, Crispin A, Schwarz PEH, von Bibra H. Waist-to-height ratio and metabolic phenotype compared to the Matsuda index for the prediction of insulin resistance. Sci Rep. 2021;11(1):8224.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, et al. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;9(1):9693.
Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644–7.
Geifman N, Cohen R, Rubin E. Redefining meaningful age groups in the context of disease. Age (Dordr). 2013;35(6):2357–66.
Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, et al. Optimal cutoff values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002;26(9):1232–8.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–86.
Choi JR, Koh SB, Choi E. Waist-to-height ratio index for predicting incidences of hypertension: the ARIRANG study. BMC Public Health. 2018;18(1):767.
Kolb H. Obese visceral fat tissue inflammation: from protective to detrimental? BMC Med. 2022;20(1):494.
Bogaert YE, Linas S. The role of obesity in the pathogenesis of hypertension. Nat Clin Pract Nephrol. 2009;5(2):101–11.
Yano S. Does body height affect vascular function? Hypertens Res. 2022;45(2):369–71.
Stefan N, Häring HU, Hu FB, Schulze MB. Divergent associations of height with cardiometabolic disease and cancer: epidemiology, pathophysiology, and global implications. Lancet. 2016;4(2213–8595 (Electronic)).
World Health Organization. Regional Office for the Western P. The Asia-Pacific perspective : redefining obesity and its treatment: Sydney : Health Communications Australia; 2000 2000.
Ashwell M, Gibson S. Waist to height ratio is a simple and effective obesity screening tool for cardiovascular risk factors: Analysis of data from the British National Diet And Nutrition Survey of adults aged 19–64 years. Obes Facts. 2009;2(2):97–103.
Lu Y, Liu S, Qiao Y, Li G, Wu Y, Ke C. Waist-to-height ratio, waist circumference, body mass index, waist divided by height(0.5) and the risk of cardiometabolic multimorbidity: A national longitudinal cohort study. Nutr Metab Cardiovasc Dis. 2021;31(9):2644–51.
Cooper AJ, Gupta SR, Moustafa AF, Chao AM. Sex/Gender Differences in Obesity Prevalence, Comorbidities, and Treatment. Curr Obes Rep. 2021;10(4):458–66.
Kanter R, Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3(4):491–8.
Katsoulis M, Lai AG, Diaz-Ordaz K, Gomes M, Pasea L, Banerjee A, et al. Identifying adults at high-risk for change in weight and BMI in England: a longitudinal, large-scale, population-based cohort study using electronic health records. Lancet Diabetes Endocrinol. 2021;9(10):681–94.
Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol. 2018;15(4):230–40.
Ramos-Arellano LE, Matia-Garcia I, Marino-Ortega LA, Castro-Alarcon N, Munoz-Valle JF, Salgado-Goytia L, et al. Obesity, dyslipidemia, and high blood pressure are associated with cardiovascular risk, determined using high-sensitivity C-reactive protein concentration, in young adults. J Int Med Res. 2020;48(12):300060520980596.
Zhernakova DV, Sinha T, Andreu-Sánchez S, Prins JR, Kurilshikov A, Balder J-W, et al. Age- dependent sex differences in cardiometabolic risk factors. Nature Cardiovascular Research. 2022;1(9):844–54.
Ji H, Kim A, Ebinger JE, Niiranen TJ, Claggett BL, Bairey Merz CN, et al. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020;5(3):19–26.
Meredith-Jones K, Taylor R, Brown R, Cooke R, Vlietstra L, Manning P, et al. Age- and sex-specific visceral fat reference cutoffs and their association with cardio-metabolic risk. Int J Obes (Lond). 2021;45(4):808–17.
Wang X, Carcel C, Woodward M, Schutte AE. Blood Pressure and Stroke: A Review of Sex- and Ethnic/Racial-Specific Attributes to the Epidemiology, Pathophysiology, and Management of Raised Blood Pressure. Stroke. 2022;53(4):1114–33.
Faulkner JL, Belin de Chantemele EJ. Sex hormones, aging, and cardiometabolic syndrome. Biol Sex Differ. 2019;10(1):30.
Baraskar K, Thakur P, Shrivastava R, Shrivastava VK. Female obesity: Association with endocrine disruption and reproductive dysfunction. Obesity Medicine. 2021;28.
Werneck AO, Oyeyemi AL, Cyrino ES, Ronque ERV, Szwarcwald CL, Coelho ESMJ, et al. Association between age at menarche and blood pressure in adulthood: is obesity an important mediator? Hypertens Res. 2018;41(10):856–64.
Zhang L, Li Y, Zhou W, Wang C, Dong X, Mao Z, et al. Mediation effect of BMI on the relationship between age at menarche and hypertension: The Henan Rural Cohort Study. J Hum Hypertens. 2020;34(6):448–56.
Acknowledgements
The authors thank Wanda Estinfort, Dedik Sulistiawan, and Pham Thi Minh Thu from the College of Public Health, Taipei Medical University, for their insightful feedback. This study was funded by the Ministry of Science and Technology (contract number MOST 107-2314-B-038-072-MY3 and MOST 110-2314-B038-056-MY3) to Professor Chyi-Huey Bai from Taipei Medical University, as the principal investigator.
Funding
The Ministry of Science and Technology funded this study under the grants MOST 107–2314-B-038–072-MY3 and MOST 110–2314-B038-056-MY3.
Author information
Authors and Affiliations
Contributions
R.A.G contributed to analyzing data and interpreting the result, wrote and approved the manuscript. YCF and SHW contributed to data cleaning and wrangling of Taiwan Biobank database, revised and approved the manuscript. C.H.B constructed the study design and analytical concept, obtained funding, analyzed, critically revised and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the institutional review board of Taipei Medical University (number N202104112). All participants of TWB had given informed consent prior to signing up.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gumilang, R.A., Fan, YC., Wu, SH. et al. Adiposity indices and their higher predictive value for new-onset hypertension in metabolically healthy young women: findings from a population-based prospective cohort study. BMC Cardiovasc Disord 24, 150 (2024). https://doi.org/10.1186/s12872-024-03817-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03817-y