Abstract
Background
The impact of hypertrophic cardiomyopathy (HCM) on cardiovascular and obstetrical outcomes in pregnant women remains unclear, particularly in Asian populations. This study aimed to evaluate the maternal cardiovascular and obstetrical outcomes in Korean women with HCM.
Methods
Using data from the Korean National Health Insurance Service database, we identified women who gave birth via cesarean section or vaginal delivery after being diagnosed with HCM between 2006 and 2019. Maternal cardiovascular and obstetrical outcomes were assessed based on the trimester of pregnancy.
Results
This study included 122 women and 158 pregnancies. No maternal deaths were noted; however, 21 cardiovascular events, such as hospital admission for cardiac problems, including heart failure and atrial fibrillation (AF), new-onset AF or ventricular tachycardia (VT) occurred in 14 pregnancies (8.8%). Cardiac events occurred throughout pregnancy with a higher occurrence in the third trimester. Cesarean sections were performed in 49.3% of the cases, and all cardiovascular outcomes occurring after delivery were observed in patients who had undergone cesarean sections. Seven cases involved preterm delivery, and two of these cases were accompanied by cardiac events, specifically AF. Pre-existing arrhythmia (AF: odds ratio (OR): 7.44, 95% confidence interval (CI): 2.61–21.21, P < 0.001; VT: OR: 31.61, 95% CI: 5.85–172.77, P < 0.001) was identified as a predictor for composite outcomes of cardiovascular events or preterm delivery.
Conclusions
Most pregnant women with HCM were well-tolerated. However, cardiovascular complications could occur in some patients. Therefore, planned delivery may be necessary for selected patients, especially the women with pre-existing arrhythmias.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is one of the most prevalent genetic diseases which can lead to adverse cardiovascular outcomes, including heart failure (HF), atrial fibrillation (AF), thrombosis and sudden cardiac death [1]. With the increased use of echocardiography and genetic screening, the incidence of HCM diagnosis has gradually increased. A recent study from a team of South Korean researchers demonstrated a prevalence of approximately 0.031% in patients with a mean age of > 60 years. Notably, the number of patients with HCM is also increasing among individuals in their 20 and 30 s, as well as among women, albeit at a slower rate [2].
Pregnancy induces various hemodynamic changes, such as decreased peripheral vascular resistance, increased cardiac output and tachycardia. During the gestational period, the left ventricular chamber undergoes dilation attributed to increased blood volume and enhanced contractility, while tachycardia concurrently reduces diastolic filling time [3, 4]. Consequently, HF may be more pronounced in patients with HCM during pregnancy. Additionally, vaginal delivery can cause a significant increase in heart rate and cardiac output, [5] while general or spinal anesthesia for cesarean section can reduce systemic vascular resistance and blood pressure owing to the parasympathetic effect [6]. Theoretically, these hemodynamic changes during delivery could provoke adverse events in patients with HCM. However, the actual impact of pregnancy in patients with HCM remains inadequately understood because of the small sample size [7,8,9,10]. Despite being at a relatively higher risk for cardiovascular issues, most pregnant patients with HCM tolerated their pregnancies well. However, reported complication rates varied widely, ranging from 15 to 45%, depending on the reports [7,8,9,10]. Therefore, this study aimed to evaluate maternal outcomes during pregnancy in patients with HCM using the Korean National Health Insurance Service database.
Methods
Data sources
This study was based on a database provided by the National Health Insurance Services-Health Screening (NHIS-HEALS) cohort in Korea. The NHIS is a mandatory insurance service in Korea covering 97.2% of the Korean enrollees, with individuals aged ≥ 40 being eligible for a general health screening program every 2 years. The remaining enrollees with a low income are covered by the Medical Aid Program, and the information has been incorporated into a single database since 2006. The database includes data regarding demographics, inpatient and outpatient services utilization, diagnoses, prescriptions, deaths and health screening examinations. The cohort details have been described previously. The study was approved by the Institutional Review Board of Chung-Ang University Hospital (#2108-011-19379). The anonymized dataset and unidentified information were provided to the researchers from the NHIS, and the requirement for informed consent was waived.
Definition of HCM and pregnancy
HCM was defined by (1) claims for diagnostic codes (International Classification of Disease 10th Revision, ICD-10, I42.1 or I42.2) with at least one admission or outpatient visit, and (2) registration in the Korean Rare Intractable Disease (RID) program (code: V127), which includes patients with HCM. A previous study from Korea validated the definition using hospital data and showed high accuracy [11]. Pregnant patients were identified among the patients diagnosed with HCM according to the above definitions. Given the nature of the data, determining the precise onset of each patient’s pregnancy was not possible. Therefore, we utilized codes for vaginal delivery and cesarean section as indicators of pregnancy. The definitions of vaginal delivery and cesarean section were based on ICD-10 (Supplementary Table 1).
Definition of comorbidities and pregnancy trimester
Comorbidities, including hypertension, diabetes, dyslipidemia, stroke, AF, HF and ventricular tachycardia (VT), were defined using the ICD-10 code and the prescription list in the NHIS database. The detailed definition of comorbidities is summarized in Supplementary Table 1. In pregnancy, the first day of the last menstrual period (LMP) was defined as the beginning of the first trimester (“day zero”). However, LMP was unavailable in the NHIS data, and the algorithm assumed “day zero” as the delivery date minus 39 weeks (273 days), if there was no code for preterm birth. If there was a code for preterm delivery (O601, O603), day zero was assumed as the delivery date minus 35 weeks (245) days [12, 13]. Therefore, baseline comorbidities were only included if diagnosed before 39 weeks prior to the delivery date (or 35 weeks for preterm delivery). The detailed definition of trimesters is summarized in Supplementary Table 2. We collected prescriptions for medications related to renin-angiotensin-aldosterone system (RAS) blockers, beta-blockers, calcium channel blockers, and amiodarone that were prescribed in Korea up to the estimated first day of pregnancy (Table 1).
Definition of cardiovascular and obstetrical outcomes
We evaluated cardiovascular and obstetrical outcomes during pregnancy and one month after delivery. Hospitalization due to HF and AF, thromboembolic events, new-onset AF and new-onset VT were evaluated as cardiovascular events. The detailed definitions of outcomes are summarized in Supplementary Table 1. In cases where both new-onset AF and AF-related hospitalization were recorded within the same specification, the latter was included, and the former was excluded from the analysis. Preeclampsia, gestational hypertension, placenta previa, intrauterine growth retardation and preterm delivery were evaluated as obstetrical outcomes.
Statistical analysis
Categorical variables were presented as percentages, and continuous variables as means ± standard deviations. Patient characteristics between groups were compared using Pearson’s chi-squared test for categorical variables and Student’s t-test for continuous variables. Logistic regression analysis was performed to identify independent variables associated with adverse outcomes in pregnancy. To investigate the correlation in detail, factors considered as risk factors in pregnant HCM patients were analyzed. A two-sided significance level of P < 0.05 was considered statistically significant. Statistical analyses were performed using the SAS software (version 9.4; SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
Of the total 30,378 patients with HCM, 122 women experienced delivery after the HCM diagnosis. Patients with more than two pregnancies were classified as individual cases, resulting in 158 pregnancies. (Fig. 1) Baseline characteristics of all pregnancy cases are summarized in Table 1. The mean age of women was 34.1 ± 4.3 years old. Among them, cesarean section was performed in 78 (49.4%) pregnancies, and women who underwent cesarean section were older than those who opted for vaginal delivery. No women received an implantable cardioverter defibrillator (ICD) before delivery; however, septal myectomy had been performed in two women who delivered by cesarean section. There were no significant differences in the prevalence of hypertension, diabetes, stroke, AF, HF, and history of VT. No significant difference was observed in cardiovascular medications before pregnancy except RAS blockers. The period from the diagnosis of HCM to delivery was a median of 933 (interquartile range: 222–2088) days.
Cardiovascular outcomes
Cardiovascular outcomes are summarized in Table 2 according to the trimester of the pregnancy. There was no maternal mortality in this data. During pregnancy and the first month postpartum, 21 cardiovascular events occurred. These events included two hospitalizations for HF, six hospitalizations for AF and 13 cases of new-onset arrhythmias. Among patients with new onset arrhythmia, eight new-onset AF and five new-onset VT were detected during pregnancy, but there was no thromboembolic event during pregnancy in patients with HCM. When evaluated based on the number of patients, a total of 14 (8.8%) individuals experienced cardiovascular events, with some patients experiencing two or more events in the whole period. Cardiac events occurred throughout pregnancy during the first, second, and a high frequency of events was noted during the third trimester (Fig. 2). There were two hospitalizations for cardiovascular outcomes after delivery, and both patients had undergone a cesarean section.
Obstetrical outcomes
Table 3 shows the obstetric outcomes for the total pregnancies. Regarding obstetrical complications, 23 (14.6%) patients with HCM experienced at least one complication, accounting for a total of 27 obstetric complications. Notably, most obstetrical complications developed after the second trimester and showed the highest rates in the third trimester. Preterm delivery occurred in seven of the 158 pregnancies (4.4%), and all preterm deliveries were performed in the third trimester. A cardiac event accompanied two cases of preterm delivery, and the period from cardiac event to delivery was 87 days and 164 days, respectively. In both cases, preterm delivery followed the diagnosis of new-onset atrial fibrillation.
Factors associated with cardiovascular outcomes or preterm delivery
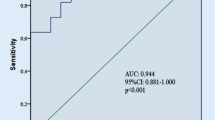
As shown in the logistic regression analysis (Table 4), arrhythmias, including AF (odds ratio (OR): 7.44, 95% confidence interval (CI): 2.61–21.21, P < 0.001) and VT (OR: 31.61, 95% CI: 5.85–172.77, P < 0.001) diagnosed before pregnancy were significantly associated with cardiovascular outcomes or preterm delivery. Similar results were seen when only cardiovascular outcomes were analyzed separately (AF, OR: 10.67, 95% CI: 3.28–34.69, P < 0.001; VT, OR: 53.25, 95% CI: 9.24–306.93, P < 0.001, Supplementary Table 3). Older age, nulliparity, hypertension, diabetes, smoking, HF and surgical myectomy were not associated with adverse cardiovascular events and preterm delivery.
Discussion
The present study investigated cardiovascular and obstetrical complications during pregnancy in patients with HCM. Patients diagnosed with HCM tolerated pregnancy well and did not have a high rate of cardiovascular or obstetrical complications. However, 8.8% of women experienced cardiovascular complications during pregnancy, resulting in hospitalization or treatment. These complications were more commonly observed in the second half of pregnancy. Among the underlying conditions, arrhythmias, such as AF and VT were related to adverse cardiovascular outcomes related to the pregnancy. Although most women with HCM can safely undergo pregnancy and childbirth, careful planning is necessary when arrhythmias are present.
Prevalence of cardiovascular outcomes in pregnant women with HCM
HCM is one of the most prevalent hereditary heart diseases [14]; however, it is mainly diagnosed in individuals beyond middle age [2], resulting in a relatively low proportion of reproductive women with HCM. The physiological changes during pregnancy and childbirth impose additional hemodynamic challenges for individuals with HCM. Nevertheless, research in this area has been limited due to the small number of patients available for study. Moreover, most existing studies primarily focus on Western populations, with only a small-scale study involving approximately 30 Japanese participants [9]. Consequently, there is a significant dearth of studies examining the pregnancy-related impact of HCM on Asian populations. In this regard, our study is significant and relevant, because it represents the first comprehensive Asian study encompassing a substantial number of pregnant cases.
Previous research has consistently indicated a remarkably low occurrence of pregnancy-related mortality among patients with HCM [7,8,9,10]. This observation is supported by two relatively recent studies [9, 10], which reported no maternal death. Similarly, our study, which comprised 158 pregnancies, also showed no cases of maternal death. According to previous studies, the prevalence of cardiovascular complications in patients with HCM during pregnancy, such as HF and arrhythmia, has been reported to range from 15 to 45% [7, 9, 10, 15]. In our study, we observed cardiovascular issues in 8.8% of cases, which was slightly less frequent compared to previous findings. The feature of the Korean RID program, which comprehensively covers costs, may have influenced some of these differences. Some patients previously diagnosed with HCM may be admitted to the hospital based solely on the diagnosis of HCM when presenting with cardiovascular symptoms related to HCM. We identified eight cases in which patients were hospitalized with a diagnosis of HCM alongside concurrent cardiovascular symptoms such as dyspnea and chest pain without a diagnosis of HF or arrhythmias. Therefore, our findings may have underestimated the number of events compared to those of other studies.
In our study, the majority of cardiovascular events occurred during the third trimester of pregnancy. This pattern aligns with observations from two previous representative studies [9, 10]. The critical periods during pregnancy when patients are the most vulnerable to cardiac complications are typically the end of the first trimester, the second trimester at around 20 weeks’ gestation, at 32 to 34 weeks’ gestation, when blood volume is at its maximum, and during the peripartum period [16]. Given the consistent finding of a high frequency of events in the third trimester, both in similar studies and in our investigation, it can be concluded that pregnant women with HCM have an elevated risk of cardiovascular outcomes during this period. Hence, close observation is imperative during the third trimester to manage and mitigate potential complications.
Arrhythmia in pregnant women with HCM
Our study highlighted arrhythmia as a prominent complication, consistent with the findings of a prior Japanese study [9] Notably, even within the general population, pregnancy is associated with a greater risk of arrhythmias, and patients with a history of arrhythmias are at significant risk of arrhythmia recurrence during pregnancy [17]. This heightened risk can be attributed to the physiologic changes of pregnancy, which include a decrease in parasympathetic nerves and an upsurge in sympathetic nerve activity. The increased sympathetic nerve response is intricately linked to automaticity, reentry, and triggered activity [17]. Hence, in individuals with HCM, who already exhibit a greater predisposition to arrhythmia compared to the general population, the likelihood of exacerbated arrhythmia during pregnancy is increased. Indeed, our study demonstrated that patients with underlying arrhythmias, such as AF or VT, were more prone to experience adverse cardiovascular outcomes. This emphasizes the importance of closely monitoring and providing appropriate care to patients with arrhythmias following pregnancy.
Obstetric outcomes in pregnant women with HCM
In line with a prior retrospective cohort study that utilized large-scale NHIS data, which reported on obstetric complication rates in the general population, our study similarly identified obstetric complications such as preeclampsia, gestational hypertension, placenta previa, and abruptio placentae, occurring in approximately 1% of normal subjects. However, due to the limited sample size of patients in our study, making direct comparisons proves challenging. Nonetheless, we observed generally similar trends [18]. However, we did observe a higher incidence of gestational diabetes mellitus in the third trimester of pregnancy among patients with HCM. Currently, no existing research has explored the association between gestational diabetes mellitus and HCM. Further investigations in the future are required to confirm this relationship. Preterm delivery is a significant concern in pregnant women with HCM, which can lead to various complications. Our study identified seven preterm delivery cases and cardiovascular problems accompanied two cases. These findings align with the results of a Japanese study, wherein it was noted that approximately 30% of premature births were associated with underlying maternal heart issues [9]. This similarity further emphasizes the importance of monitoring and addressing the risk of preterm delivery in HCM pregnant women with cardiovascular complications.
Delivery methods in pregnant women with HCM
In our study, approximately half of the pregnancy cases with HCM underwent a cesarean section for delivery, and no significant differences were observed in other baseline collected data. Notably, the cesarean section rate in the general population of Korea has shown an upward trend, increasing from 36.3 to 45% from 2006 to 2015 [19]. Considering our study’s inclusion of patients from 2006, it is reasonable to assume a higher prevalence of cesarean sections compared to the general population during that timeframe. While the literatures recommend vaginal delivery in cases of structural heart disease owing to the higher risks associated with cesarean section, such as bleeding, thromboembolic events, and infection, [20, 21] studies showed that cesarean sections have been more frequently performed in such cases [22]. Nevertheless, our findings indicate that there is no apparent need to prioritize cesarean section as the preferred method of delivery for patients with HCM.
Study limitations
This study had several limitations. First, it is important to acknowledge that our study may have been susceptible to coding errors in diagnosing underlying diseases such as hypertension, diabetes, or HF. Since these diagnoses were based on diagnostic codes from the administrative database, there is a possibility of inaccuracies or misclassification in the coding process. This limitation should be considered when interpreting and generalizing the study results. Second, in patients with HCM, the echocardiography results are crucial in assessing the condition. However, we were unable to confirm these echocardiographic findings owing to the nature of the data source and study design. A previous study found that specific echocardiographic variables, such as left ventricular outflow tract obstruction and left ventricular ejection fraction, were not predictive indicators of major adverse cardiovascular events during pregnancy [9, 10]. Third, given the nature of the database, cardiac magnetic resonance or genetic test results could not be obtained. Fourth, considering the reimbursement characteristics of the Korea RID program, cardiovascular outcomes could be underestimated. Finally, our results were obtained only from Korean women; hence, its application to other ethnic groups may be limited.
Conclusion
Based on the cohort of women diagnosed with HCM who underwent delivery in the current study, cardiovascular complication rate was low (8.8%) and obstetrical complications comparable to those observed in the general population except gestational diabetes mellitus. Consequently, it was noted that pregnancy and childbirth were generally well-tolerated by most women. However, for selected patients, particularly those with a history of arrhythmias, a planned delivery approach may be needed to mitigate the risks associated with cardiovascular outcomes.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- HCM:
-
Hypertrophic cardiomyopathy
- HF:
-
Heart failure
- ICD:
-
Implantable cardioverter defibrillator
- LMP:
-
Last menstrual period
- NIHS-HEALS:
-
National Health Insurance Services-Health Screening
- RAS:
-
Renin-angiotensin-aldosterone system
- RID:
-
Rare intractable disease
- VT:
-
Ventricular tachycardia
References
Maron BJ, Desai MY, Nishimura RA, Spirito P, Rakowski H, Towbin JA, Rowin EJ, Maron MS, Sherrid MV. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(4):372–89.
Moon I, Lee SY, Kim HK, Han KD, Kwak S, Kim M, Lee HJ, Hwang IC, Lee H, Park JB, et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: a nationwide population-based cohort study. PLoS ONE. 2020;15(1):e0227012.
Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, Gatzoulis MA, Gohlke-Baerwolf C, Kaemmerer H, Kilner P, et al. ESC guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31(23):2915–57.
Elkayam U, Goland S, Pieper PG, Silverside CK. High-risk Cardiac Disease in pregnancy: part I. J Am Coll Cardiol. 2016;68(4):396–410.
Kuhn JC, Falk RS, Langesaeter E. Haemodynamic changes during labour: continuous minimally invasive monitoring in 20 healthy parturients. Int J Obstet Anesth. 2017;31:74–83.
Dyer RA, Piercy JL, Reed AR, Lombard CJ, Schoeman LK, James MF. Hemodynamic changes associated with spinal anesthesia for cesarean delivery in severe preeclampsia. Anesthesiology. 2008;108(5):802–11.
Autore C, Conte MR, Piccininno M, Bernabo P, Bonfiglio G, Bruzzi P, Spirito P. Risk associated with pregnancy in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;40(10):1864–9.
Thaman R, Varnava A, Fau - Hamid MS, Hamid Ms Fau -, Firoozi S, Firoozi S, Fau - Sachdev B, Sachdev B, Fau - Condon M, Condon M. Fau - Gimeno JR, Gimeno Jr Fau - Murphy R, Murphy R Fau - Elliott PM, Elliott Pm Fau - McKenna WJ, McKenna WJ: pregnancy related complications in women with hypertrophic cardiomyopathy. (1468-201X (Electronic)).
Tanaka H, Kamiya C, Katsuragi S, Tanaka K, Miyoshi T, Tsuritani M, Yoshida M, Iwanaga N, Neki R, Yoshimatsu J, et al. Cardiovascular events in pregnancy with hypertrophic cardiomyopathy. Circ J. 2014;78(10):2501–6.
Goland S, van Hagen IM, Elbaz-Greener G, Elkayam U, Shotan A, Merz WM, Enar SC, Gaisin IR, Pieper PG, Johnson MR, et al. Pregnancy in women with hypertrophic cardiomyopathy: data from the European Society of Cardiology initiated Registry of pregnancy and cardiac disease (ROPAC). Eur Heart J. 2017;38(35):2683–90.
Choi YJ, Choi EK, Han KD, Jung JH, Park J, Lee E, Choe W, Lee SR, Cha MJ, Lim WH, et al. Temporal trends of the prevalence and incidence of atrial fibrillation and stroke among Asian patients with hypertrophic cardiomyopathy: a nationwide population-based study. Int J Cardiol. 2018;273:130–5.
Margulis AV, Setoguchi S, Mittleman MA, Glynn RJ, Dormuth CR, Hernandez-Diaz S. Algorithms to estimate the beginning of pregnancy in administrative databases. Pharmacoepidemiol Drug Saf. 2013;22(1):16–24.
Toh S, Li Q, Cheetham TC, Cooper WO, Davis RL, Dublin S, Hammad TA, Li DK, Pawloski PA, Pinheiro SP, et al. Prevalence and trends in the use of antipsychotic medications during pregnancy in the U.S., 2001–2007: a population-based study of 585,615 deliveries. Arch Womens Ment Health. 2013;16(2):149–57.
Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary artery Risk Development in (Young) adults. Circulation. 1995;92(4):785–9.
Schinkel AF. Pregnancy in women with hypertrophic cardiomyopathy. Cardiol Rev. 2014;22(5):217–22.
Adam K. Pregnancy in women with Cardiovascular diseases. Methodist Debakey Cardiovasc J. 2017;13(4):209–15.
Tamirisa Kamala P, Elkayam U, Briller Joan E, Mason Pamela K, Pillarisetti J, Merchant Faisal M, Patel H, Lakkireddy Dhanunjaya R, Russo Andrea M, Volgman Annabelle S, et al. Arrhythmias in pregnancy. JACC: Clin Electrophysiol. 2022;8(1):120–35.
Lim NG, Lee JY, Park JO, Lee JA, Oh J. Pregnancy, prenatal care, and delivery of mothers with disabilities in Korea. J Korean Med Sci. 2015;30(2):127–32.
Kim HY, Lee D, Kim J, Noh E, Ahn KH, Hong SC, Kim HJ, Oh MJ, Cho GJ. Secular trends in cesarean sections and risk factors in South Korea (2006–2015). Obstet Gynecol Sci. 2020;63(4):440–7.
Pieper PG. The pregnant woman with heart disease: management of pregnancy and delivery. Neth Heart J. 2012;20(1):33–7.
Sawada M, Yoshimatsuj J, Nakai M, Tsukinaga R, Yokouchi-Konishi T, Shionoiri T, Nakanishi A, Horiuchi C, Tsuritani M, Kamiya CA et al. Appropriate delivery method for cardiac disease pregnancy based on noninvasive cardiac monitoring. J Perinat Med 2020.
Ruys TP, Roos-Hesselink JW, Pijuan-Domenech A, Vasario E, Gaisin IR, Iung B, Freeman LJ, Gordon EP, Pieper PG, Hall R et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart 2015, 101(7):530–536.
Acknowledgements
None.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
W.C.: Investigation, Formal analysis, Writing-original draft, K-T.P.: Investigation, Formal analysis, Writing-original draft, H.K.: Conceptualization, Investigation, Formal analysis, Writing-original draft, Writing – review & editing, J.C.: Methodology, Writing – review & editing, G.N.: Methodology, Writing – review & editing, J.H.: Methodology, Writing – review & editing, D.K.: Methodology, Writing – review & editing, J.L.: Methodology, Writing – review & editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board (IRB) of Chung-Ang University Hospital approved this study protocol (#2108-011-19379). IRB of Chung-Ang University Hospital waived the requirement for informed consent because of the retrospective nature of this national cohort and there was no risk of the exposure of personal information of the participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Choi, W.Y., Park, KT., Kim, H.M. et al. Pregnancy related complications in women with hypertrophic cardiomyopathy: a nationwide population-based cohort study. BMC Cardiovasc Disord 24, 268 (2024). https://doi.org/10.1186/s12872-024-03812-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03812-3