Abstract
Background
Cognitive frailty (CF) is currently a significant issue, and most of the associated factors discovered in current studies are not modifiable. Therefore, it is crucial to identify modifiable risk factors that can be targeted for interventions in patients with chronic heart failure (CHF). This study aimed to investigate the prevalence and modifiable risk factors of CF in CHF patients in China.
Methods
In this cross-sectional study, we sequentially enrolled patients diagnosed with CHF. CF served as the dependent variable, assessed through the Montreal Cognitive Assessment (MoCA) Scale and the FRAIL Scale. The independent variable questionnaire encompassed various components, including general demographic information, the Social Support Rating Scale (SSRS), the Simplified Nutrition Appetite Questionnaire (SNAQ), the Hamilton Depression Scale (HAMD), the Hamilton Anxiety Scale (HAMA), and the Minnesota Living with Heart Failure Questionnaire (MLHFQ). Logistic regression analysis was employed to identify independent factors contributing to CF.
Results
A total of 271 patients with CHF were included in the study. The overall prevalence of CF was found to be 49.4%, with 28.8% of patients exhibiting potentially reversible cognitive frailty and 20.7% showing reversible cognitive frailty. Among middle-young CHF patients, 10.7% had reversible cognitive frailty and 6.4% had potentially reversible cognitive frailty, with a prevalence of CF at 17.1%. Logistic regression analysis revealed that body mass index (OR = 0.826, 95%CI = 0.726–0.938), blood pressure level (OR = 2.323, 95%CI = 1.105–4.882), nutrition status (OR = 0.820, 95%CI = 0.671–0.979), and social support (OR = 0.745, 95%CI = 0.659–0.842) were independent factors associated with CF (p < 0.05).
Conclusions
We observed a relatively high prevalence of CF among Chinese patients diagnosed with CHF. Many factors including BMI, blood pressure level, nutrition status, and social support emerging as modifiable risk factors associated with CF. We propose conducting clinical trials to assess the impact of modifying these risk factors. The outcomes of this study offer valuable insights for healthcare professionals, guiding them in implementing effective measures to improve the CF status in CHF patients during clinical practice.
Similar content being viewed by others
Introduction
Chronic heart failure (CHF) is a persistent state of heart failure and a major cause of death from various cardiovascular diseases. According to the European Heart Association’s Guidelines for Diagnosis and Treatment of Acute and Chronic Heart Failure, the prevalence of heart failure in developed countries ranges from 1.5 to 2.0% [1]. According to the Report on Cardiovascular Health and Diseases in China 2021: an Updated Summary, there were 8.9 million patients with heart failure in China [2]. Heart failure is a chronic and recurring disease, with a high 30-day readmission rate of up to 20–25% and a five-year survival rate of 56.7% [3, 4]. The development of CHF is a lengthy process with a poor overall prognosis.
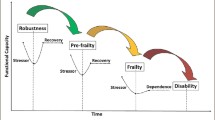
The concept of frailty is increasingly being considered in the study and treatment of CHF patients. Frailty is an age-related clinical syndrome characterized by reduced physiological reserves in stressful situations, constituting a state of vulnerability that involves a higher risk of adverse events [5]. It adversely impacts the mortality of heart failure patients [6], seriously interferes with the recovery process and increases the risk of suicide in CHF patient [7]. Frailty encompasses both physical and mental aspects, and research indicates a close correlation between physical frailty in CHF patients and cognitive impairment [8]. While physical frailty and cognitive impairment were previously studied separately, recent research has highlighted their close relationship [9].
Thus, the concept of cognitive frailty (CF) was proposed to combine physical frailty and cognitive impairment. CF is characterized by the coexistence of physical frailty and cognitive impairment, with a Clinical Dementia Rating (CDR) score of 0.5, but excluding Alzheimer’s disease or other forms of dementia [10]. Previous research has shown that CF is prevalent in patients with cardiovascular disease and can have a negative impact on their clinical outcome, functional status and quality of life [11]. A study of Japanese heart failure patients over the age of 65 found that those with CF had a 1.55 times higher risk of poor prognostic outcomes in the first year compared to those without CF [12]. Previous studies indicated that CF could be reversible [13], thus, identifying and responding to risk factors for CF can help to slow down or even reverse its progression. However, the associated factors discovered in current studies of CF, such as age, education level, etc., are not intervenable [14]. A review shows that social status, nutrition status, physical and cognitive activities and functional status are factors shown to be associated with CF [15]. However, the effect of depression in CF remains controversial and we need to explore future [16, 17]. Social support has been shown to be an influential factor for CF in hypertensive patients [18] and other studies have found the effects of BMI and nutrition status of CF [19]. This study includes some known influencing factors of CF and hypothesizes that these factors are also relevant for patients with CHF. Therefore, this study aims to investigate the prevalence and modifiable risk factors of CF in patients with CHF in China. We hope to draw the attention of medical staff and improve the prognosis of CHF patients by intervening on modifiable risk factors of CF and to improve the recovery process of patients and reduce mortality.
Methods
Design and participates
This cross-sectional was conducted in the Cardiology Department of Jiangsu Province Hospital from August 2022 to February 2023. Patients with CHF were enrolled sequentially using a convenience sampling method. The inclusion criteria were as follows: (a) meeting the diagnostic criteria of CHF in Chinese guidelines for the diagnosis and treatment of heart failure 2018 [20]; (b) being ≥ 18 years old; (c) having a New York Heart Association functional classification of I ~ IV; (d) being able to communicate normally; (e) volunteering and signing an informed consent form. The exclusion criteria were as follows: (a) having dementia or other mental illnesses; (b) having a medical history of severe liver, kidney, brain etc. or other physical diseases; (c) being unable to cooperate with this study. The research protocol was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2022-SR-502).
The questionnaire was collected without hindering the treatment and rest of patients. During data collection, the investigators performed face-to-face conversation to give corresponding explanations in time to ensure the integrity of data. To facilitate communication and future follow-up studies, each patient was individually marked during the survey. Subsequent to data collection, the collectors promptly organized and verified the data. All information underwent a thorough recheck and was independently entered into the computer by two investigators.
General demographic data
We utilized a self-made questionnaire to obtain the sociodemographic data from patients, including age, gender, education level, marital status, work status, smoking and drinking habits, body mass index (BMI, kg/m2), and more. Clinical information was obtained from electronic medical records, including the New York Heart Association (NYHA) functional classification, CHF course, physician-diagnosed comorbidities (such as hypertension, diabetes, coronary artery disease, etc.), and left ventricular ejection fraction (LVEF) (%), etc. For some continuous variables, we applied a transformation. We found that the course of disease was measured by a classification [18], which has not been applied in the study of CHF, although it has been done clinically. In line with the education system in China, we categorized education levels into five groups. According to guidelines [20], we used a cut-off point of 125 pg/ml to group NT-proBNP. LVEF was divided into three categories: heart failure with reduced ejection fraction (HFrEF, LVEF < 40%), heart failure with mid-range ejection fraction (HFmrEF, LVEF between 40% and 49%) and heart failure with preserved ejection fraction (HFpEF, LVEF ≥ 50%).
Cognitive frailty
CF refers to the combination of physical frailty (PF) and cognitive impairment, excluding dementia. To assess cognitive function, we utilized the Montreal Cognitive Assessment (MoCA) (Beijing version) [21], which consists of 30 points and a score of less than 26 indicates cognitive impairment. The MoCA evaluates cognitive abilities in various areas, including spatial/executive thinking, naming, memory, attention, language, abstraction, delayed recall and orientation. The Cronbach’s α coefficient for this scale is 0.818. Measurement of the frailty using the FRAIL Scale [22] proposed by the experts of the International Nutrition, Health and Work Group in 2008. It is based on the frailty phenotype and Frailty Index, and consists of 36 items selected from the Short Form of medical outcome study, as well as some items on disease and weight loss. The resulting 5-item scale assigns 1 point to each item, with a total score ranging from 0 to 5. A score of 3 or higher indicates frailty, 1–2 indicates pre-frailty, and 0 indicates no frailty. The Cronbach’s α coefficient for this scale is 0.826. According to Ruan’s definition of CF, this study distinguishes between reversible cognitive frailty and potentially reversible cognitive frailty [23]. Patients who were in physical frailty or pre-frailty and had a MoCA score of less than 26 were classified as potentially reversible cognitive frailty. For those with frailty or pre-frailty who had a normal MoCA score, subjective cognitive frailty was considered reversible if they answered “Yes” to the question “Do you think you have memory decline compared to a year ago?”. Patients who responded with a “No” to the question or those who exhibited no signs of frailty or cognitive impairment were categorized as none cognitive frailty. All of our investigators have received training in this area.
Social support
The Social Support Rating Scale (SSRS), developed by Xiao in 1986, was utilized to evaluate social support [24]. The scale comprises 10 items and three dimensions: objective support (three items), subjective support (four items) and support utilization (three items). The objective support score ranges from 4 to 16, the subjective support score ranges from 5 to 38, and the support utilization score ranges from 3 to 12. A higher total score indicates a higher level of support. The SSRS scale demonstrates good reliability and validity, with a Cronbach’s α coefficient of 0.941. This scale was employed to gain a better understanding of patients’ social support and its correlation with mental health, mental illness, and various physical conditions.
Nutrition
The Simplified Nutrition Appetite Questionnaire (SNAQ) was developed from the Appetite Scale (CNAQ) by the Community Committee for Long-term Nutrition Care Strategy [25]. It consists of only four items, each with five response options represented by letters A to E. The scoring method used is a Likert five-level scale, with scores ranging from 4 to 20 points. A lower score indicates a poorer appetite and an increased risk of weight loss. A score of ≤ 14 suggests a higher risk of malnutrition, with more than a 5% weight loss in the last six months. The Cronbach’s α coefficient for this scale is 0.72.
Anxiety and depression
The Hamilton Depression Scale (HAMD) [26] and the Hamilton Anxiety Scale (HAMA) [27] were utilized to evaluate depression and anxiety. The HAMD scale comprises seven factor structures, including anxiety/somatization, body mass, cognitive impairment, day-night change, delay, sleep disturbance and sense of hopelessness. Scores between 8 and 20 indicate mild depression, 21 to 35 indicate moderate depression, and scores greater than 35 indicate severe depression. A score of 8 or below on the HAMD is considered clinical remission, with a Cronbach’s α coefficient of 0.92. The HAMA scale consists of two component structures: psychological anxiety and physical anxiety. Trained researchers score each item on a 5-point scale. A score of 14 to 21 indicates mild anxiety, 22 to 29 indicates moderate anxiety, and scores greater than 29 indicate severe anxiety.
Health-related quality of life
The term “health-related quality of life” refers to a patient’s personal experience and feelings regarding heart failure and its treatment’s impact on their daily life. The Minnesota Living with Heart Failure Questionnaire (MLHFQ) was utilized to assess it [28]. This 21-item questionnaire is specifically designed to evaluate the physical, socioeconomic, and psychological impairment perceived by patients with HF. Each item has six response options, ranging from 0 to 5, with higher scores indicating poorer HRQOL. The scale is the most commonly used tool for measuring HRQOL in heart failure studies, and it has demonstrated acceptable reliability and validity, with a Cronbach’s α coefficient of 0.91.
Data analysis
General demographic data, cognitive frailty, nutrition, anxiety, depression and health-related quality of life of patients were analyzed descriptively. Normally distributed data were expressed as mean ± standard deviation, while non-normally distributed data were expressed as percentage or median (25th and 75th percentiles). Categorical variables were presented as frequency and percentage. Pearson correlation analysis was employed for continuous variables with a normal distribution, while Spearman correlation analysis was used for continuous variables with a non-normal distribution. Following the correlation analysis, independent variables with a p-value < 0.05 were included in logistic regression analysis to identify the independent factors associated with cognitive frailty. Data analysis was conducted using SPSS 25.0.
Results
Descriptive statistics
A total of 271 patients were included in this study, of which 78 patients exhibited potentially reversible cognitive frailty, resulting in a prevalence of 28.8%. Among these patients, 56 were diagnosed with reversible cognitive frailty, resulting in a prevalence of 20.7%. The overall prevalence of CF in CHF patients was found to be 49.4%. In middle-young CHF patients, 10.7% exhibited reversible cognitive frailty, while 6.4% displayed potentially reversible cognitive frailty. The total prevalence of cognitive frailty in this group was 17.1%.
Differences in physiological functioning and psychological characteristics of CHF patients with different degrees of CF
Table 1 presents additional general data and disease-related information. Univariate analysis revealed that age, caregiver status, education level, marital status, combined with hypertension and cerebral disease, course of CHF, newly diagnosed CHF, blood type, LVEF, NYHA functional classification, Barthel self-care ability, BMI, nutrition status, and degree of anxiety and depression degree were all significantly associated with CF (p < 0.05).
Correlations of physiological function and psychological characteristics with CF in CHF patients
The study found that the average SSRS score of CHF patients was 34.92 ± 3.72, while the average MLHFQ score was 50.99 ± 12.83. Correlation analyses revealed that CF was positively associated with age (r = 0.551, p < 0.001), anxiety (r = 0.337, p < 0.001), depression (r = 0.364, p < 0.001), and health-related quality of life (r = 0.272, p < 0.001). Conversely, CF demonstrated negative associations with BMI (r = -0.220, p < 0.001), nutrition state (r = -0.252, p < 0.001), and social support (r = -0.503, p < 0.001). The results are presented in Table 2.
Independent influencing factors of CF
The findings from the logistic regression analysis indicate that BMI, blood pressure level, nutrition status, and social support were all independent factors of CF (p < 0.05). Body mass index (OR = 0.826, 95%CI = 0.726–0.938), blood pressure level (OR = 2.323, 95%CI = 1.105–4.882), nutrition status (OR = 0.820, 95%CI = 0.671–0.979), and social support (OR = 0.745, 95%CI = 0.659–0.842) are independent influencing factors on CF. Table 3 displays the specific outcomes.
Discussion
This study aimed to examine the prevalence of cognitive frailty (CF) in patients with chronic heart failure (CHF) and identify any modifiable risk factors. Our findings revealed a high prevalence of CF in this population, with BMI, blood pressure level, nutrition status and social support being identified as significant modifiable risk factors for CF.
In this study, it was found that the total prevalence of CF in patients with CHF was 49.4% [95%CI = 43.5–55.4%], with reversible cognitive frailty at 20.7% and potentially reversible cognitive frailty at 28.8%. Researchers from South Korea [29] and Japan [12] evaluated heart failure patients over the age of 65 and discovered that 34.5% and 23% of patients had CF, respectively. They did not investigate the two types of CF separately. However, Yao et al. investigated the prevalence of frailty and cognitive impairment in hospitalized patients with cardiovascular diseases and discovered that only 8% of patients had both conditions [30]. This difference may be due to the fact that Yao’s study included hospitalized patients with various cardiovascular disease, whereas our study only included CHF patients. Meanwhile, we used different assessment tools. Currently, cognitive and frailty assessment tools are commonly used to assess CF, but uniform assessment standards have yet to be developed. As the terminal stage of various cardiovascular diseases, CHF has a long course that involves many different systems and mechanisms. These include brain changes, vascular mechanisms, inflammation, hormones, sarcopenia, oxidative stress process, mitochondrial dysfunction and intestinal microbiome changes, all of which have a significant impact on physical frailty and cognitive function [11]. Simultaneously, it was found that the prevalence of CF in the elderly and middle-young patients undergoing maintenance hemodialysis was 35.8% and 8.8%, respectively, indicating that middle-young patients are equally susceptible to CF [19]. Our study found that the prevalence of CF was 17.1% among middle-young CHF patients, suggesting that the prevalence of CF in CHF patients of different age ranges should not be ignored. Previous studies on CF have focused on the elderly population, with little attention paid on middle-young demographic. Despite the limited number of middle-young patients included in this study, we found a significant prevalence of CF in this population. While CF has been extensively studied in the field of geriatrics, more research is needed to understand the current status of CF in middle-aged individuals. For middle-young CHF patients with CF, appropriate interventions should be implemented promptly to reverse CF, prevent its worsening with age, and reduce the risk of poor cardiovascular outcomes.
In this study, it was found that BMI was a modifiable risk factor of CF in patients with CHF (OR = 0.826, 95%CI = 0.726–0.938). Rietman et al. conducted a cohort research which discovered a slight linear correlation between BMI and CF, with higher BMI being associated with more severe CF [31]. However, other studies have found opposite results, with a higher BMI being linked to a lower risk of CF [32]. Therefore, the relationship between BMI and CF remains contentious. By reviewing data from the CLHLS project, Ju et al. discovered a U-shaped correlation between BMI, waist circumference (WC), and frailty in elderly Chinese women [33]. However, the biological mechanism underlying this relationship remains unknown. Further research is needed to identify additional indicators with predictive value. The study found that only being overweight was a risk factor for CF, while being underweight may also affect CF in patients with CHF. However, the specific effect and degree of influence of BMI require further investigation.
Nutrition status is another modifiable risk factor of CF (OR = 0.810, 95%CI = 0.671–0.979). Numerous studies have shown that malnutrition is a significant risk factor for CF [34], and it is negatively correlated with nutrition status. Malnutrition can lead to weight loss, muscle tissue loss, body wasting, and other physical frailties, ultimately contributing to the development of CF. Furthermore, the lack of essential nutrients such as serum proteins, vitamins, and trace elements can affect cognitive function, which is also a crucial factor in the development and progression of physical frailty and cognitive impairment [35]. Zupo et al. found that malnourished elderly people with CF had a higher mortality rate [36], highlighting the urgent need to improve the nutrition status of patients with CF. Consequently, we aim to substantiate the impact of nutrition status on CF in patients with CHF through forthcoming clinical trials.
Patients with hypertension had a 2.323 times higher likelihood of developing CF compared to those without hypertension (95%CI = 1.105–4.882). Wang et al. found that 9.8% of elderly hypertensive patients had CF [18], While up to 28% of hypertension and diabetes patients who underwent physical examination in community health service centers had CF [34]. These findings suggest that the prevalence of CF in elderly hypertensive patients in China should not be ignored. Scholars have identified that frequent morbidity, such as hypertension and heart disease, as influential factor for CF [37]. This may indicate that hypertension, heart disease and CF are interrelated and interconnected. As a major cause of cardiovascular disease, hypertension can damage brain capillaries, leading to cognitive impairment and accelerating the development of dementia. These risk factors for cognitive impairment are associated with the onset and deterioration of PF. Consequently, there is a necessity to initiate clinical trials to investigate the impact of hypertension on CF in patients with CHF.
We have found that social support is a modifiable risk factor for CF (OR = 0.745, 95%CI = 0.659–0.842). Studies have shown that low social support is an independent risk factor of CF in the elderly [38]. Apart from CHF, Wang et al. found that social support was also an independent factor impacting CF in hypertensive patients [18]. We speculate that social support may be a factor influencing CF in other diseases. Lack of social support may lead to various psychological problems. However, this study did not find evidence that depression, anxiety, or other mental states are independent factors influencing CF in CHF patients. Hou et al. found that depressive symptoms do not directly affect CF in older adults, but rather, feelings of loneliness are the link between the two [39]. Loneliness can reflect social support to some extent. However, Wang et al. found that psychological distress could regulate the relationship between social support and the prevalence of CF [17]. Therefore, the relationship between mental state and CF remains vague and requires further study.
The study did not find old age and low education level to be significant risk factors for CF, despite their correlation in the univariate analysis. This discrepancy may be attributed to the specific population and region included in the study. Although we transformed some continuous variables, we re-analyzed the data using the original continuous variables. Variables associated with CHF were treated as additional independent variables associated with CF risk. The prevalence of HFrEF was higher in the non-CF group (41%) compared to the CF groups (27% and 25%), while the prevalence of HFpEF was higher in the CF groups. This would suggest that CF is more prevalent in diastolic dysfunction rather than systolic dysfunction, but further studies are needed. Importantly, more than half of the Non-CF patients had CHF for ≤ 1 year, while the CF groups had a longer duration. This is significant in the regression analysis, where we seek to identify modifiable risk factors for CF. Additionally, the Non-CF group had a higher prevalence in the lower NYHA classes. In this study, we also found a strong correlation between CHF and CF, particularly through the indicators associated with CHF. As a result, it is crucial to monitor the condition of CHF patients and provide them with relief from CF while maintaining disease stability.
In this study, we broadened the scope of our research by including patients above the age of 18. This is because middle-aged and young people are also at risk of cognitive frailty, which has been previously overlooked in studies that mainly focused on the elderly. We also categorized patients into two groups: reversible cognitive frailty and potentially reversible cognitive frailty to better understand the status quo of CF in CHF patients. We identified modifiable risk factors that influence CF in patients with CHF. Nonetheless, clinical trials are imperative to ascertain whether these modifiable risk factors have the potential to reverse CF in CHF patients. This study adds to the current situation in domestic research on cognitive frailty in CHF patients above the age of 18.
Although this study has yielded valuable insights, there are still some limitations that need to be addressed. Firstly, it is a single-center study, and the majority of patients are from nearby towns and cities, which limits the generalizability of the findings. Future multi-center studies with large sample sizes are needed to overcome this limitation. Secondly, this study is constrained by its cross-sectional design, which impedes our ability to establish the predictive value of the aforementioned factors for CF. We urge and encourage researchers to delve further into the relationship among these factors. Future investigations could benefit from non-clinical population controls and longitudinal follow-up studies to provide a more comprehensive understanding of these associations. Thirdly, prevalence estimates obtained from convenience sampling are strongly subjected to sampling bias. In future studies, we intend to employ a more judicious and rational sampling method to enhance the robustness and generalizability of our findings. Finally, no unique influencing factors connected to CHF are discovered in this investigation, which may be related to the disease severity of the included patients. Additionally, the baseline data included in this study are incomplete, and there may be undiscovered influencing factors that require further investigation.
Conclusion
There is a high prevalence of CF among patients with CHF in China. Therefore, healthcare providers need to conduct a comprehensive assessment of individual CHF patients to identify and prevent risks at an early stage. We suggest conducting clinical trials to test the effects of these modifiable risk factors. Our study adds to the research on CF in patients with CHF. These findings augment the existing knowledge on CF in CHF patients and offer valuable reference for medical staff to implement effective measures for improving the CF status in clinical practice.
Data availability
The datasets analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CF:
-
cognitive frailty
- CHF:
-
chronic heart failure
- MoCA:
-
Montreal Cognitive Assessment
- BMI:
-
body mass index
- AD:
-
Alzheimer’s disease
- NYHA:
-
New York Heart Association
- LVEF:
-
left ventricular ejection fraction
- PF:
-
physical frailty
- SSRS:
-
Social Support Rating Scale
- SNAQ:
-
Simplified Nutrition Appetite Questionnaire
- HAMD:
-
the Hamilton Depression Scale
- HAMA:
-
the Hamilton Anxiety Scale
- MLHFQ:
-
Minnesota Living with Heart Failure Questionnaire
- WC:
-
waist circumference
References
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, ESC Scientific Document Group. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726. https://doi.org/10.1093/eurheartj/ehab368.
The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Report on Cardiovascular Health and diseases in China 2021: an updated Summary. Chin J Circulation. 2022;37(06):553–78. https://doi.org/10.3969/j.issn.1007-5410.2022.04.001.
Roger VL. Epidemiology of Heart failure: a contemporary perspective. Circul Res. 2021;128(10):1421–34. https://doi.org/10.1161/CIRCRESAHA.121.318172.
Jones NR, Roalfe AK, Adoki I, Hobbs FDR, Taylor CJ. Survival of patients with chronic heart failure in the community: a systematic review and meta-analysis. Eur J Heart Fail. 2019;21(11):1306–25. https://doi.org/10.1002/ejhf.1594.
Díez-Villanueva P, Arizá-Solé A, Vidán MT, Bonanad C, Formiga F, Sanchis J, Martín-Sánchez FJ, Ros R, Sanmartín Fernández V, Bueno MH, Martínez-Sellés M. Recommendations of the Geriatric Cardiology Section of the Spanish Society of Cardiology for the Assessment of Frailty in Elderly Patients With Heart Disease. Revista espanola de cardiologia (English ed.). 2019;72(1):63–71. https://doi.org/10.1016/j.rec.2018.06.035.
Jiménez-Méndez, C, Díez-Villanueva P, Bonanad C, Ortiz-Cortés C, Barge-Caballero E, Goirigolzarri J, Esteban-Fernández A, Pérez-Rivera Á, Cobo M, López J, Sanz-García A, Guerrero C, Pardo HG, Robles C, Iglesias D, Pinilla JMG, Rodríguez LL, Formiga F, Martín-Sánchez FJ, Vidán MT, … en representación de los investigadores del registro FRAGIC. Frailty and prognosis of older patients with chronic heart failure. Revista espanola de cardiologia (English ed.). 2022;75(12):1011–1019. https://doi.org/10.1016/j.rec.2022.04.016.
Jankowska-Polańska B, Polański J, Dudek K, Sławuta A, Mazur G, Gajek J. The role of Sleep Disturbance, Depression and anxiety in Frail patients with AF-Gender differences. J Clin Med. 2020;10(1):11. https://doi.org/10.3390/jcm10010011.
Yuan Y, Lapane KL, Tjia J, Baek J, Liu SH, Ulbricht CM. Physical Frailty and Cognitive Impairment in older adults in United States Nursing Homes. Dement Geriatr Cogn Disord. 2021;50(1):60–7. https://doi.org/10.1159/000515140.
Jongsiriyanyong S, Limpawattana P. Mild cognitive impairment in clinical practice: a review article. Am J Alzheimer’s Dis Other Dement. 2018;33(8):500–7. https://doi.org/10.1177/1533317518791401.
Kelaiditi E, Cesari M, Canevelli M, van Kan GA, Ousset PJ, Gillette-Guyonnet S, Ritz P, Duveau F, Soto ME, Provencher V, Nourhashemi F, Salvà A, Robert P, Andrieu S, Rolland Y, Touchon J, Fitten JL, Vellas B, IANA/IAGG. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging. 2013;17(9):726–34. https://doi.org/10.1007/s12603-013-0367-2.
Yao SM, Zheng PP, Wang H, Yang JF. Research progress on cognitive frailty in cardiovascular disease. Chin J Geriatr. 2022;41(1):95–9. https://doi.org/10.3760/cma.j.issn.0254-9026.2022.01.020.
Yamamoto S, Yamasaki S, Higuchi S, Kamiya K, Saito H, Saito K, Ogasahara Y, Maekawa E, Konishi M, Kitai T, Iwata K, Jujo K, Wada H, Kasai T, Nagamatsu H, Ozawa T, Izawa K, Aizawa N, Makino A, Oka K, Matsue Y. Prevalence and prognostic impact of cognitive frailty in elderly patients with heart failure: sub-analysis of FRAGILE-HF. ESC Heart Fail. 2022;9(3):1574–83. https://doi.org/10.1002/ehf2.13844.
Warraich HJ, Kitzman DW, Whellan DJ, Duncan PW, Mentz RJ, Pastva AM, Nelson MB, Upadhya B, Reeves GR. Physical function, Frailty, Cognition, Depression, and quality of life in hospitalized adults ≥ 60 years with Acute Decompensated Heart failure with preserved Versus reduced ejection fraction. Circulation. Heart Fail. 2018;11(11):e005254. https://doi.org/10.1161/CIRCHEARTFAILURE.118.005254.
Zhang Y, Zhou JJ, Zhang XM, Liu JT, Li MR, Liang JY, Gao YL. Management of cognitive frailty: a network meta-analysis of randomized controlled trials. Int J Geriatr Psychiatry. 2023;38(9):e5994. https://doi.org/10.1002/gps.5994.
Sugimoto T, Arai H, Sakurai T. An update on cognitive frailty: its definition, impact, associated factors and underlying mechanisms, and interventions. Geriatr Gerontol Int. 2022;22(2):99–109. https://doi.org/10.1111/ggi.14322.
Zhang T, Ren Y, Shen P, Jiang S, Yang Y, Wang Y, Li Z, Yang Y. Prevalence and Associated Risk factors of cognitive Frailty: a systematic review and Meta-analysis. Front Aging Neurosci. 2022;13:755926. https://doi.org/10.3389/fnagi.2021.755926.
Wang Y, Li J, Fu P, Jing Z, Zhao D, Zhou C. Social support and subsequent cognitive frailty during a 1-year follow-up of older people: the mediating role of psychological distress. BMC Geriatr. 2022;22(1):162. https://doi.org/10.1186/s12877-022-02839-5.
Wang C, Zhang J, Hu C, Wang Y. Prevalence and risk factors for cognitive Frailty in Aging Hypertensive patients in China. Brain Sci. 2021;11(8):1018. https://doi.org/10.3390/brainsci11081018.
Chen G, Zhang H, Du X, Yin L, Zhang H, Zhou Q. Comparison of the prevalence and associated factors of cognitive frailty between elderly and middle-young patients receiving maintenance hemodialysis. Int Urol Nephrol. 2022;54(10):2703–11. https://doi.org/10.1007/s11255-022-03188-3.
Heart Failure Group of Chinese Society of Cardiology of Chinese Medical Association, Chinese Heart Failure Association of Chinese Medical Doctor Association, Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for the diagnosis and treatment of heart failure 2018. Chin J Cardiol. 2018;46(10):760–89. https://doi.org/10.3760/cma.j.issn.0253-3758.2018.10.004.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
Lopez D, Flicker L, Dobson A. Validation of the frail scale in a cohort of older Australian women. J Am Geriatr Soc. 2012;60(1):171–3. https://doi.org/10.1111/j.1532-5415.2011.03746.x.
Ruan Q, Yu Z, Chen M, Bao Z, Li J, He W. Cognitive frailty, a novel target for the prevention of elderly dependency. Ageing Res Rev. 2015;20:1–10. https://doi.org/10.1016/j.arr.2014.12.004.
Xiao SY. The theoretical basis and research application of Social Support Rating Scale. Journal of Clinical Psychiatry. 1994;1994(02):98–100. https://kns.cnki.net/kcms2/article/abstract?v=Lty0U-YuiCcP-a00UCLufvKjVuYwiomcKDiwx5rOyNOTO-arsiXhAe4qOdHxO5HnOujgU3uiGqddEobjqEpCBbPp3sVUqYBe3LRwsF2Bh4bseWggY3nAv7YX_b5BgEwu&uniplatform=NZKPT&language=CHS.
Rolland Y, Perrin A, Gardette V, Filhol N, Vellas B. Screening older people at risk of malnutrition or malnourished using the Simplified Nutritional Appetite Questionnaire (SNAQ): a comparison with the Mini-nutritional Assessment (MNA) tool. J Am Med Dir Assoc. 2012;13(1):31–4. https://doi.org/10.1016/j.jamda.2011.05.003.
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–96. https://doi.org/10.1111/j.2044-8260.1967.tb00530.x.
HAMILTON M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–5. https://doi.org/10.1111/j.2044-8341.1959.tb00467.x.
Dunderdale K, Thompson DR, Beer SF, Furze G, Miles JN. Development and validation of a patient-centered health-related quality-of-life measure: the chronic heart failure assessment tool. J Cardiovasc Nurs. 2008;23(4):364–70. https://doi.org/10.1097/01.JCN.0000317439.82704.e8.
Seo EJ, Son YJ. The Prevalence of Cognitive Frailty and Its Association with Sleep duration and Depression Among Older Adults with Heart Failure. Clinical gerontologist. 2022;1–10. Advance online publication. https://doi.org/10.1080/07317115.2022.2125858.
Yao SM, Zheng PP, Liang YD, Wan YH, Sun N, Luo Y, Yang JF, Wang H. Predicting non-elective hospital readmission or death using a composite assessment of cognitive and physical frailty in elderly inpatients with cardiovascular disease. BMC Geriatr. 2020;20(1):218. https://doi.org/10.1186/s12877-020-01606-8.
Rietman ML, van der A DL, van Oostrom SH, Picavet HSJ, Dollé MET, van Steeg H, Verschuren WMM, Spijkerman AMW. The Association between BMI and different Frailty domains: a U-Shaped curve? J Nutr Health Aging. 2018;22(1):8–15. https://doi.org/10.1007/s12603-016-0854-3.
Anaika G, Regalla SS, Reddy BM, Ganguly E, Sharma PK. Association of Obesity with cognitive impairment and depression among Oldest Old Population having Frailty syndrome. J Frailty Sarcopenia Falls. 2022;7(4):207–21. https://doi.org/10.22540/JFSF-07-207.
Ju AP, Zhou JH, Gu H, Ye LL, Chen C, Guo YB, Wang J, Zhang ZW, Qu YL, Liu Y, Liu L, Xue K, Zhao F, Lyu YB, Ye L, Shi X. Chin J Prev Med. 2022;56(11):1584–90. https://doi.org/10.3760/cma.j.cn112150-20211228-01196.
Lu S, Xu Q, Yu J, Yang Y, Wang Z, Zhang B, Wang S, Chen X, Zhang Y, Zhu X, Hong K. Prevalence and possible factors of cognitive frailty in the elderly with hypertension and diabetes. Front Cardiovasc Med. 2022;9:1054208. https://doi.org/10.3389/fcvm.2022.1054208.
Flores AC, Jensen GL, Mitchell DC, Na M, Wood GC, Still CD, Gao X. Prospective study of Diet Quality and the risk of Dementia in the Oldest Old. Nutrients. 2023;15(5):1282. https://doi.org/10.3390/nu15051282.
Zupo R, Castellana F, Guerra V, Donghia R, Bortone I, Griseta C, Lampignano L, Dibello V, Lozupone M, Coelho-Júnior HJ, Solfrizzi V, Giannelli G, De Pergola G, Boeing H, Sardone R, Panza F. Associations between nutritional frailty and 8-year all-cause mortality in older adults: the Salus in Apulia Study. J Intern Med. 2021;290(5):1071–82. https://doi.org/10.1111/joim.13384.
Lee WJ, Peng LN, Liang CK, Loh CH, Chen LK. Cognitive frailty predicting all-cause mortality among community-living older adults in Taiwan: a 4-year nationwide population-based cohort study. PLoS ONE. 2018;13(7):e0200447. https://doi.org/10.1371/journal.pone.0200447.
Xie B, Ma C, Chen Y, Wang J. Prevalence and risk factors of the co-occurrence of physical frailty and cognitive impairment in Chinese community-dwelling older adults. Health Soc Care Commun. 2021;29(1):294–303. https://doi.org/10.1111/hsc.13092.
Hou P, Xue H, Zhang Y, Ping Y, Zheng Y, Wang Y, Yao Z, Xie X, Dai H, Liu Y. Mediating effect of loneliness in the relationship between depressive symptoms and cognitive Frailty in Community-Dwelling older adults. Brain Sci. 2022;12(10):1341. https://doi.org/10.3390/brainsci12101341.
Acknowledgements
Thanks to Mr. Jiang for his help in data statistics. We thank the study participants who made this study possible.
Funding
This work was supported by the Jiangsu Provincial Medical Innovation Team (CXTDA2017019) and Postgraduate Research & Practice Innovation Program of Jiangsu Province (SJCX23_0822).
Author information
Authors and Affiliations
Contributions
J.X. collected and analyzed data, drafted the initial manuscript and reviewed and revised the manuscript; L.X., H.Z. and X.S. collected and analyzed data, reviewed and revised the manuscript; D.X. and D.W. reviewed and revised the manuscript; C.C. collected data; Z.G. and Y.Z. designed the study, made supportive contributions and contributed to the critical revision of the manuscript. All authors have read and agreed to the published version of the manuscript. # J.X., L.X., H.Z. and X.S. contributed equally to this work and should be considered co-first authors.* Z.G. and Y.Z. contributed equally to this work and should be considered corresponding authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The research protocol was approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University (2022-SR-502). Written informed consent was obtained from all study subjects before study commencement.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yixiong Zhang and Zejuan Gu contributed equally to this work and should be considered corresponding authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, J., Xiang, L., Zhang, H. et al. Prevalence and modifiable risk factors of cognitive frailty in patients with chronic heart failure in China: a cross-sectional study. BMC Cardiovasc Disord 24, 93 (2024). https://doi.org/10.1186/s12872-024-03753-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-03753-x