Abstract
Background
Acute myocardial infarction (AMI) with consequent heart failure is one of the leading causes of death in humans. The aim of this study was to develop a prediction model to identify heart failure risk in patients with AMI during hospitalization.
Methods
The data on hospitalized patients with AMI were retrospectively collected and divided randomly into modeling and validation groups at a ratio of 7:3. In the modeling group, the independent risk factors for heart failure during hospitalization were obtained to establish a logistic prediction model, and a nomogram was constructed. The receiver operating characteristic (ROC) curve, calibration curve, and decision curve analysis (DCA) were used to evaluate the predictive performance and clinical value. Machine learning models with stacking method were also constructed and compared to logistic model.
Results
A total of 1875 patients with AMI were enrolled in this study, with a heart failure rate of 5.1% during hospitalization. The independent risk factors for heart failure were age, heart rate, systolic blood pressure, troponin T, left ventricular ejection fraction and pro-brain natriuretic peptide levels. The area under the curve (AUC) of the model in modeling group and validation group were 0.829 and 0.846, respectively. The calibration curve showed high prediction accuracy and the DCA curve showed good clinical value. The AUC value of the ensemble model by the stacking method in the validation group were 0.821, comparable to logistic prediction model.
Conclusions
This model, combining laboratory and clinical factors, has good efficacy in predicting heart failure during hospitalization in AMI patients.
Similar content being viewed by others
Introduction
As one of the most common causes of death, acute myocardial infarction (AMI) is a serious disease [1, 2]. AMI leads to 6.4 million deaths per year in the USA and Europe, and it accounts for more than a third of deaths in other developed countries [3, 4]. According to the China Cardiovascular Health and Disease Report 2021, AMI rose from 23.2/100,000 in 2003 to 62.33/100,000 in 2008 for urban residents in China. AMI results bring heavy burdens to family and society due to its high cost in the treatment. Moreover, baseline diseases such as diabetes would increase the mortality of patients with AMI, which could be explained that diabetes might accelerate the process of atherosclerosis [5, 6].
Heart failure is a common complication of AMI. It is characterized by severe systolic and/or diastolic function impairment of the heart [7, 8]. The progression from AMI to heart failure involves myocardial shock, remodeling, and chronic neuroendocrine system activation [9]. AMI impairs the ventricle function through wall thinning of the infarct zone, ventricular dilatation, and ultimately compensatory hypertrophy and fibrosis [10]. The larger the infarct size leads to heavier burden on the remaining viable myocardium, consequently contributing to higher probability of heart failure [11].
Previous studies have reported that being complicated with heart failure increased the mortality rate of 10 times higher for patients with acute coronary syndrome [12]. It is thus particularly important to predict the risk of heart failure in patients with AMI. Recent studies have shown that carbohydrate antigen 125, brain derived neurotrophic factor, serum soluble growth stimulation expressed gene 2, and interleukin-33 are effective predictors of heart failure in patients with AMI [12, 13]. However, these indicators are rarely measured in clinical trials, which largely limits their clinical practice. In another way, the clinical indexes available from routine laboratory tests during admission would be convenient for evaluating the risk of heart failure, but previous models hardly test the linear relationship between involved variables and terminal event or any interaction among the involved variables. Furthermore, the small sample size or the recruitment of certain subpopulation limits the reliability of the established prediction models to general patients with AMI [14]. In this study, the risk factors related to heart failure in patients with AMI after admission were combined to develop a logistic prediction model and a nomogram was established to evaluate how much the involved indexes contribute to heart failure. This model will help clinicians to predict the possibility of heart failure in patients with AMI during hospitalization and make personalized measures in their therapy process.
Material and methods
Patient inclusion and exclusion
Patients with AMI admitted to Dongyang People’s Hospital from January 2010 to September 2022 were included. Patients with AMI were diagnosed upon getting two of three points: clinical manifestations including chest pain and chest distress; abnormal electrocardiogram indicating for ST segment elevation and complete left bundle branch block; troponin or creatine kinase isoenzyme levels higher than 2 times the upper limitation range [15, 16]. Patients who met one of the following exclusion criteria were removed: a previous history of heart failure; existence of heart failure within 24 h after admission, indicated from by clinical manifestation and laboratory examination; presence of cancer, mental illness, or other serious complications; missing data; no myocardial infarction confirmation by emergency percutaneous coronary intervention (PCI). The terminal event was heart failure during hospitalization, and its diagnosis was based on guidelines from the European Society of Cardiology [17]. Heart failure was diagnosed during hospitalization based on the presence of risk factors, corresponding symptoms or signs, abnormal electrocardiogram, BNP ≥ 35 pg/mL and abnormal findings of echocardiography [17]. This study was approved by the Ethics Committee of Dongyang People’s Hospital. Written informed consent for participation was not required for this study due to its retrospective design, and the study was undertaken in accordance with national legislation and institutional requirements.
Observation indicator collection from a clinical record information mining database
Patient information was extracted retrospectively from a clinical record information mining database (supported Le 9 Co., Ltd.) and included sex, age, history of non-ST segment elevation myocardial infarction (NSTEMI). Laboratory examination results within 24 h after admission were collected, including troponin T, creatine kinase isoenzyme (CKMB), D-dimer, B-type pro-brain natriuretic peptide, aspartate aminotransferase, high-sensitivity C-reactive protein (CRP), creatinine, white blood cell (WBC) count, platelets, hematocrit. Physical examination was performed to get systolic blood pressure (SBP), left ventricular ejection fraction (LVEF) and heart rate. The treatment intervenes for AMI such as emergency PCI (PCI treatment performed within 12 hours after the onset of the disease is defined as emergency PCI treatment) was also included in this study. Each index unit was converted to the current international unit.
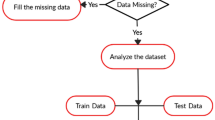
Variable screening for inclusion in the established prediction model
RStudio 4.4.1 software and IBM SPSS 25.0 software were used to process the data. After collecting the patient data, the variables with missing data more than 25% were removed. The remaining missing variables were interpolated by multiple imputation function as previously described [18]. Count data have been expressed as numbers (percentages), and measurement data have been represented as medians (interquartile ranges). Following univariate analysis (“twogrps” function in CBCgrps package), the boxTidwell function was used to analyze whether there was a linear relationship between significant variables in the univariate analysis and logitp. A multicollinearity test was then performed to test for the presence of multicollinearity between the involved variables, and variance inflation factors (VIFs) of less than 10 indicated no collinearity [19]. Finally, logistic and bidirectional stepwise regression analyses were used to obtain the independent risk factors, and a nomogram was constructed. The area under the curve (AUC) of the receiver operating characteristic (ROC) curve was used to evaluate the discrimination ability of the established model. At the optimal cutoff value, the prediction accuracy, positive prediction value (PPV) and negative predictive value (NPV) were calculated. Calibration evaluation was used to determine whether the predicted probability was consistent with the observed probability. In addition, a decision curve analysis (DCA) was conducted to evaluate the clinical benefit of the nomogram. A P value less than 0.05 was considered significant. Also, the model based on stacking method was established in the validation group, which combined the advantages of SVM, C5.0 and Xgboost methods as described previously [20, 21]. The importance of involved variables in the model was evaluated by SHAP summary plots. Finally, the differences among the discrimination powers of established models were tested by using Delong test based on the AUCs.
Results
Baseline characteristics of subjects
A total of 1875 patients were enrolled in this study, including 1313 patients in the modeling group, and 562 patients in the validation group. The global heart failure rate was 5.1% (97/1875). The clinical characteristics were comparable between the modeling and validation groups (Table 1).
Variable screening by univariate and multivariate analyses
Univariate analysis showed there were 12 indicators significantly related to heart failure in the modeling group (Table 2) (P < 0.05). There were linear relationships between 12 variables and logitp (Supplementary Table 1), but no multiple-collinearity was found between the variables (Supplementary Table 2). Logistic and stepwise regression analyses showed that six variables (troponin T, age, heart rate, SBP, LVEF and pro-brain natriuretic peptide) were independent risk factors of heart failure (Table 3) (P < 0.05). Consequently, a logistic prediction model was constructed.
Establishment of a nomogram from the modeling group
Based on the logistic regression model, a nomogram graph was established by evaluating how much the significant risk factors contributed to the heart failure risk (Fig. 1). Individual points corresponding to the indicated variables were obtained by mapping their detailed results to the upper scoring line; then, the summed score was displayed as the total points. Finally, the risk value of heart failure was obtained by matching the total points to the scoring line at the bottom of the graph.
Prediction ability of the established model in the modeling validation groups
The AUC value of the model was 0.829 in the modeling group (95% CI: 0.779–0.879), with an optimal cut-off point of 0.038, a sensibility of 70.0%, and a specificity of 81.8%, (Fig. 2A). The prediction accuracy was 0.706 (95% CI:69.6–71.2%), with a PPV of 0.126 (95% CI:9.5–15.8%) and a NPV of 0.986 (95% CI:97.9–99.4%). The P value of the calibration curve was 0.940, R2: 0.246, slope: 1.000, Brier: 0.041 (Fig. 2B). DCA curves showed that the model could predict the risk of heart failure with good net clinical benefit (Fig. 2C).
The AUC value for patients in the validation group was 0.846 (95% CI: 0.774–0.918), with an optimal cut-off point of 0.050, a sensibility of 70.8%, and a specificity of 87.1% (Fig. 3A). The prediction accuracy was 0.717 (95% CI:71.6–71.8%), with a PPV of 0.148 (95% CI:9.7–20.0%) and a NPV of 0.989 (95% CI:97.9–99.9%). The P value of the calibration chart was 0.947, R2: 0.257, slope: 1.000, Brier: 0.045 (Fig. 3B). Additionally, the DCA curve was far away from the two extreme curves (Fig. 3C).
Another model was constructed by the stacking method using SVM, C5.0 and XGboost. The AUC value was 0.821 (Fig. 4A), which was comparable to the logistic model by Delong test (P = 0.662). Among the enrolled variables, the top three important variables were the level of pro-BNP higher than 15,000 pg/ml, heart rate and LVEF (Supplementary Fig. 1). However, the calibration of the final integrated model is poor (Fig. 4B).
Discussion
AMI and its subsequent heart failure are the leading causes of death worldwide [22]. Therefore, early identification of AMI patients with high risks of heart failure during hospitalization could cause doctors’ more attention in the patients’ management. The independent risk factors related to heart failure could be corrected by active inventions, eventually leading to improvement in their survival rate [23, 24]. In this study, the risk factors associated with heart failure in AMI patients during hospitalization were age, heart rate, SBP, LVEF and troponin T and pro-brain natriuretic peptide levels. A logistic model and could efficiently predict the risk of heart failure and the nomogram could visually display how the model predicted the risk.
Previous studies have shown that age is closely related to the incidence of heart failure [12]. Due to slow blood circulation and altered myocardial metabolism in the elderly, the gradual myocardial cell atrophy and insufficient myocardial reserve capacity lead to heart failure after AMI [25]. A number of studies have shown that long-term hypertension eventually leads to heart failure [26, 27]. In fact, hypertension can cause excessive myocardial cell hypertrophy, myocardial cell degeneration and necrosis, eventually leading to heart failure. In addition, patients with heart failure who have lower systolic blood pressure have a worse prognosis than those with higher systolic blood pressure [28]. This phenomenon could be explained by impairment in pump function and cardiac output [28]. In this study, lower blood pressure also contributed significantly to the heart failure in AMI patients. Therefore, for AMI patients with low blood pressure, the blood pressure should be corrected as soon as possible to improve the coronary perfusion pressure and reduce the occurrence of heart failure.
BNP belongs to a family of natriuretic peptides that are mainly secreted by atrial myocytes in the normal heart [29], and its secretion is directly proportional to the severity of left ventricular dysfunction [30]. Brain natriuretic peptide and troponin T have long been used as indicators to predict heart failure [31,32,33,34,35,36]. Therefore, for patients with high BNP, limiting the blood volume could partly reduce the pressure on the heart by diuresis and other means, finally reducing the incidence of heart failure. This study also showed that heart rate was positively linked to heart failure risk in patients with AMI. This possibly occurs because tachycardia causes cardiac cycle shortening, mainly diastole, and reduces blood return to the heart, resulting in significant reductions in cardiac output per minute and more serious coronary ischemia [37]. Therefore, in the case with left ventricular dysfunction caused by acute myocardial infarction, β-blockers and calcium-channel blockers could be applied to reduce the heart rate, improving the clinical outcome [38]. LVEF is one of the important variables to evaluate the type of heart failure, and was negatively associated with the risk of new-onset heart failure among patients with acute myocardial infarction [17]. This is consistent with the findings of others [39].
In addition, machine learning models by Stacking methods showed no advantage in performance compared with the logistic model. Moreover, the decision support provided by machine learning models is often difficult to interpret [40]. In this study, the prediction model is presented as a nomogram, and has advantages in clinical interpretation and application.
In this study, the established model helped with the early identification of patients at high risk of heart failure. Considering that previous studies mainly focus on the effect of a single factor on the outcomes, this study synthesizes all of the independent factors by establishing a prediction model. This approach makes them intuitive and clearly present, which is helpful for clinician analysis and diagnosis. Compared with the prediction model of Tan et al., our prediction model owned a higher AUC value with less involved factors, indicating a higher discrimination ability [41]. Compared with the prediction model of Yan et al., our model is applicable to a larger population of patients than the elderly women alone [14]. Although studies have shown that women with coronary artery disease have a higher risk of heart failure than men, it is generally accepted that men are more susceptible to cardiovascular disease [39, 42]. Therefore, models that target larger patient populations are highly desirable. The different variables in our prediction model from previous study is due to the variable screening method and patient population heterogenicity. In detail, this study clearly confirmed the relationship between continuous variables and logitp, as well as the absence of collinearity relationship between variables, making it more scientific and accurate compared with previous work. Furthermore, the variables included in our study are more clinically available, which will enable clinicians to quickly identify patients at risk for heart failure [40].
Of course, this study has its limitations. First, case data from only one hospital was selected for this single-center retrospective analysis, and the external validation was not performed due to no data from another center. This limitation might decrease the credibility of the study. Second, data for other important factors, such as socio-economic status and detailed periods before the occurrence of heart failure, were not included due to missing information in the database.
Conclusion
Age, heart rate, systolic blood pressure, and troponin T, left ventricular ejection fraction and pro-brain natriuretic peptide levels were the independent risk factors for heart failure in patients with AMI. The logistic prediction model can effectively identify patients with high risks of heart failure with good discriminatory power and accuracy. Ultimately, this intuitive and convenient model will be useful for clinicians in AMI patients’ management.
Availability of data and materials
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s (Email: 13575915795@163.com).
References
Zhang C, Wang H, Chan GCF, et al. Extracellular vesicles derived from human umbilical cord mesenchymal stromal cells protect cardiac cells against hypoxia/Reoxygenation injury by inhibiting endoplasmic reticulum stress via activation of the PI3K/Akt pathway. Cell Transplant. 2020;29:963689720945677.
Zhang Y, Wang B, Fu X, et al. Exogenous NAD(+) administration significantly protects against myocardial ischemia/reperfusion injury in rat model. Am J Transl Res. 2016;8(8):3342–50.
Nichols M, Townsend N, Scarborough P, et al. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35(42):2929.
Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–65.
Dutta P, Courties G, Wei Y, et al. Myocardial infarction accelerates atherosclerosis. Nature. 2012;487(7407):325–9.
Jacoby RM. Nesto RW acute myocardial infarction in the diabetic patient: pathophysiology, clinical course and prognosis. J Am Coll Cardiol. 1992;20(3):736–44.
O'Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. Jama. 2009;301(14):1439–50.
Ranganath SH, Levy O, Inamdar MS, et al. Harnessing the mesenchymal stem cell secretome for the treatment of cardiovascular disease. Cell Stem Cell. 2012;10(3):244–58.
Dargie H. Heart failure post-myocardial infarction: a review of the issues. Heart. 2005;91(Suppl 2(Suppl 2)):ii3–6. discussion ii31, ii43-38
Lacey L. Tabberer M economic burden of post-acute myocardial infarction heart failure in the United Kingdom. Eur J Heart Fail. 2005;7(4):677–83.
Uriel N, Sayer G, Annamalai S, et al. Mechanical unloading in heart failure. J Am Coll Cardiol. 2018;72(5):569–80.
Wu HB, Shao K, Wang YC, et al. Research progress of CA125 and BDNF in serum of patients with acute myocardial infarction for predicting acute heart failure. Clin Hemorheol Microcirc. 2020;75(1):99–106.
Xing J, Liu J. Geng T predictive values of sST2 and IL-33 for heart failure in patients with acute myocardial infarction. Exp Biol Med (Maywood). 2021;246(23):2480–6.
Yan Q, Ye L, Zhang Q, et al. Nomogram to predict the incidence of new-onset heart failure after acute coronary syndrome among women. Front Cardiovasc Med. 2023;10:1131813.
Chinese Society of Cardiology of Chinese Medical Association; Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST-segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(10):766–83.
Gao RL. Guidelines for diagnosis and treatment of acute myocardial infarction [in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi. 2001;29(12):710–25.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30.
Hsieh FY. Lavori PW sample-size calculations for the cox proportional hazards regression model with nonbinary covariates. Control Clin Trials. 2000;21(6):552–60.
Tiwari A, Chugh A. Sharma a ensemble framework for cardiovascular disease prediction. Comput Biol Med. 2022;146:105624.
Yoon T. Kang D multi-modal stacking Ensemble for the Diagnosis of cardiovascular diseases. J Pers Med. 2023;13(2):373.
Ong SB, Hernández-Reséndiz S, Crespo-Avilan GE, et al. Inflammation following acute myocardial infarction: multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol Ther. 2018;186:73–87.
Arrigo M, Jessup M, Mullens W, et al. Acute heart failure. Nat Rev Dis Primers. 2020;6(1):16.
Heidenreich P. Inflammation and heart failure: therapeutic or diagnostic opportunity? J Am Coll Cardiol. 2017;69(10):1286–7.
Wang M, Pan W, Xu Y, et al. Microglia-mediated Neuroinflammation: a potential target for the treatment of cardiovascular diseases. J Inflamm Res. 2022;15:3083–94.
Iptakalim CAD. A new or just another KCO? Cardiovasc Res. 2009;83(3):417–8.
Ignatowicz A, Odland ML, Bockarie T, et al. Knowledge and understanding of cardiovascular disease risk factors in Sierra Leone: a qualitative study of patients' and community leaders' perceptions. BMJ Open. 2020;10(12):e038523.
Messerli FH, Rimoldi SF. Bangalore S the transition from hypertension to heart failure: contemporary update. JACC Heart Fail. 2017;5(8):543–51.
Christoffersen C, Goetze JP, Bartels ED, et al. Chamber-dependent expression of brain natriuretic peptide and its mRNA in normal and diabetic pig heart. Hypertension. 2002;40(1):54–60.
Madamanchi C, Alhosaini H, Sumida A, et al. Obesity and natriuretic peptides, BNP and NT-proBNP: mechanisms and diagnostic implications for heart failure. Int J Cardiol. 2014;176(3):611–7.
Braga JR, Tu JV, Austin PC, et al. Outcomes and care of patients with acute heart failure syndromes and cardiac troponin elevation. Circ Heart Fail. 2013;6(2):193–202.
Felker GM, Mentz RJ, Teerlink JR, et al. Serial high sensitivity cardiac troponin T measurement in acute heart failure: insights from the RELAX-AHF study. Eur J Heart Fail. 2015;17(12):1262–70.
Lee DS, Lee JS, Schull MJ, et al. Prospective validation of the emergency heart failure mortality risk grade for acute heart failure. Circulation. 2019;139(9):1146–56.
Pang PS, Teerlink JR, Voors AA, et al. Use of high-sensitivity troponin T to identify patients with acute heart failure at lower risk for adverse outcomes: an exploratory analysis from the RELAX-AHF trial. JACC Heart Fail. 2016;4(7):591–9.
Vander Werf BD, Watt J, Joseph B, et al. Can plasma B-type natriuretic peptide levels predict need for mechanical ventilation after injury? Am J Surg. 2010;200(6):845–50. discussion 850
Zakynthinos E, Kiropoulos T, Gourgoulianis K, et al. Diagnostic and prognostic impact of brain natriuretic peptide in cardiac and noncardiac diseases. Heart Lung. 2008;37(4):275–85.
Böhm M. Reil JC perspectives of I(f) inhibition by ivabradine in cardiology. Drugs. 2007;67(Suppl 2):43–9.
Ferrari R. Fox K heart rate reduction in coronary artery disease and heart failure. Nat Rev Cardiol. 2016;13(8):493–501.
Núñez J, Lorenzo M, Miñana G, Palau P, Monmeneu JV, López-Lereu MP, et al. Sex differences on new-onset heart failure in patients with known or suspected coronary artery disease. Eur J Prev Cardiol. 2021;28(15):1711–9.
Kelly CJ, Karthikesalingam A, Suleyman M, et al. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019;17(1):195.
Tan J, He Y, Li Z, et al. Establishment and validation of a non-invasive diagnostic nomogram to identify heart failure in patients with coronary heart disease. Front Cardiovasc Med. 2022;9:875702.
Colafella KMM, Denton KM. Sex-specific differences in hypertension and associated cardiovascular disease. Nat Rev Nephrol. 2018;14(3):185–201.
Acknowledgements
Thank you for the technical support provided by Le9 Health platform and the efforts and contributions of each author in this study.
Funding
This research was supported by The Science and Technology Bureau of JinHua (2022–4-260). The funding institution was not involved in the collection of data and writing this article.
Author information
Authors and Affiliations
Contributions
BW and JM were responsible for the conception and design of the work. SC and XP were responsible for data collection and article drafting. SC, XP, JM and BW were responsible for data analysis and substantial revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the 1964 Declaration of Helsinki. This study was approved by the Ethics Committee of the Dongyang People’s Hospital, and the ethics serial number is 2022-YX-269. Waiver of informed consent was approved by the Ethics Committee of Dongyang People’s Hospital. The study was undertaken in accordance with national legislation and institutional requirements.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Fig. 1. The SHAP summary plot of enrolled variables in the machine learning models by the ensemble method
Additional file 2: Table 1.
The linear relationship analysis between continuous variables and logit (p). Table 2. Multicollinear relationship of continuous variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, S., Pan, X., Mo, J. et al. Establishment and validation of a prediction nomogram for heart failure risk in patients with acute myocardial infarction during hospitalization. BMC Cardiovasc Disord 23, 619 (2023). https://doi.org/10.1186/s12872-023-03665-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03665-2