Abstract
Background
This study was conducted to assess the net clinical benefit (NCB) for oral anticoagulant (OAC) in atrial fibrillation (AF) patients according to the CHA2DS2-VASc score.
Methods
Patients with AF were prospectively recruited in the COOL AF Thailand registry from 2014 to 2017. The incidence rate of thromboembolic (TE) events and major bleeding (MB) was calculated. Cox proportional hazards model was used to compare the TE and MB rate in patients with and without OACs in CHA2DS2-VASc score of 0–1 and ≥ 2, respectively. The survival analysis was performed based on CHA2DS2-VASc score. The NCB of OACs was defined as the TE rate prevented minus the MB rate increased multiplied by a weighting factor.
Results
A total of 3,402 AF patients were recruited. An average age of patients was 67.38 ± 11.27 years. Compared to non-anticoagulated patients, the Kaplan Meier curve showed anticoagulated patients with CHA2DS2-VASc score of 2 or more had the lower thromboembolic events with statistical significance (p = 0.043) and the higher MB events with statistical significance (p = 0.018). In overall AF patients, there were positive NCB in warfarin patients with CHA2DS2-VASc score of 3 or more while there were positive NCB in DOACs patients regardless of CHA2DS2-VASc score. Females with CHA2DS2-VASc score of 3 or more had a positive NCB regardless of OACs type. Good anticoagulation control (TTR ≥65%) improved an NCB in males with CHA2DS2-VASc score of 3 or more.
Conclusions
AF patients with CHA2DS2-VASc score of 3 or more regardless warfarin or DOACs had a positive NCB. The NCB of OACs was more positive for DOACs compared to warfarin and for females compared to males.
Similar content being viewed by others
Background
Ischemic stroke prevention is of paramount importance in patients with atrial fibrillation (AF). Previous clinical trials have shown that oral anticoagulants (OACs) can be used for prevention of ischemic stroke in patients with AF [1,2,3]. CHA2DS2-VASc score is recommended for selection of those patients who have a benefit of OACs by all international standard guidelines [4,5,6,7].
However, OACs increase the risk of bleeding even in patients with CHA2DS2-VASc score of 0. The benefit of stroke prevention would be offset by the occurrence of bleeding [8]. Warfarin-associated intracranial hemorrhage (ICH), the most catastrophic complication, is responsible for mortality in 90% of patients treated with warfarin [9]. Several studies have shown the lower risk of ICH in patients treated with direct oral anticoagulants (DOACs) compared with warfarin [10,11,12,13].
Several studies have shown that warfarin had a positive net clinical benefit (NCB) in AF patients with high stroke risk [14, 15]. Additionally, DOACs have been studied in elderly with AF and shown a positive NCB as well [16]. The NCB assessment in previous clinical trials comprised ischemic stroke and ICH, however, the extracranial bleeding was not considered. Nevertheless, the AnTicoagulation and Risk Factors In Atrial Fibrillation (ATRIA) study has demonstrated that major extracranial bleeding is still detrimental and causing many hospital admission in anticoagulated AF patients [9].
Until now, there was a lack of data on the NCB between thromboembolic and major bleeding events in patients treated with warfarin or DOACs. This study was conducted to assess the NCB of OACs in AF patients according to their CHA2DS2-VASc score.
Methods
Study population and setting
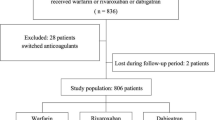
Patients with AF aged 18 years or more in 27 hospitals including university and/or general hospitals in Thailand were prospectively recruited from 2014 to 2017 to the COhort of antithrombotic use and Optimal INR Level in patients with non-valvular atrial fibrillation in Thailand (COOL AF Thailand) study [17]. Patients with prosthetic heart valve, rheumatic mitral valve disease, recent ischemic stroke within 3 months, transient reversible cause of AF, life expectancy below 3 years, pregnancy, thrombocytopenia (< 100,000/mm3), myeloproliferative diseases, refusal to be enrolled, and/or could not visit for follow-up were excluded.
The trial protocol was approved by the Central Research Ethics Committee (CREC). Written informed consent was obtained by all participated patients. The study was conducted in compliance with the Declaration of Helsinki and the International Conference on Harmonization for Good Clinical Practice Guidelines (ICH-GCP).
Data collection and outcomes
Baseline demographic and clinical data of patients with AF were collected and recorded. Patients were follow-up every 6 months until 3 years. Each patient data was recorded on electronic case record form via web-based system. The following clinical event data during follow-up visit were recorded: thromboembolic events including ischemic stroke, transient ischemic attack (TIA) and/or systemic embolization and major bleeding including ICH and/or extracranial bleeding.
Ischemic stroke was defined as a sudden onset of neurological deficit that lasted at least 24 h without ICH by computed tomography (CT) or magnetic resonance imaging (MRI). TIA was defined as a sudden neurological deficit that lasted less than 24 h. Systemic embolism was defined as the disruption of blood flow to other arteries such as acute limb arterial occlusion or acute mesenteric arterial occlusion.
Major bleeding was defined as fatal bleeding, critical organ bleeding including ICH, intraspinal, intraocular/retinal, retroperitoneal, intraarticular, pericardial, intramuscular with/without compartment syndrome and/or bleeding causing a fall in hemoglobin level of 2 g/dL or more or leading to 2 or more units of blood transfusion [18].
Each component of the CHA2DS2 -VASc score was evaluated and recorded as C = congestive heart failure (1 point); H = hypertension (1 point); A = age ≥ 75 years (2 points); D = diabetes mellitus (1 point); S = stroke and/or TIA (2 points); V = vascular disease (1 point); A = age 65–74 years (1 point); and Sc = female sex category (1 point) [19].
Statistical analysis
Categorical data are presented as percentage and number. Continuous data are presented as mean ± standard deviation (SD). The annual incidence rate of thromboembolic and major bleeding events in patients within each group of the CHA2DS2-VASc score was shown as rate per 100 person-years. Univariable Cox proportional hazards model was used to compare the annual incidence rate of both events in patients with and without OACs in CHA2DS2-VASc score of 0–1 and ≥ 2, respectively. Hazard ratio (HR) was adjusted by symptoms and pattern of AF, cardiovascular implantable electronic devices (CIEDs), dyslipidemia, chronic kidney disease (CKD), dementia, a history of bleeding, alcohol use, left ventricular ejection fraction (LVEF) < 50%, antiplatelet drugs. The results were illustrated with adjusted HR and 95% confidence interval (CI). The survival analysis from the outcome of interest in each group of the CHA2DS2-VASc score are presented with Kaplan-Meier curve. A p-value < 0.05 was considered as statistical significance.
The NCB of OACs was defined as the annual incidence rate of thromboembolic events (TE rate) prevented minus the annual incidence rate of major bleeding events (MB rate) increased multiplied by a weighting factor (WF) [14]. The following equation was demonstrated below:
NCB = (TE rate no OACs – TE rate on OACs) – [WF x (MB rate on OACs – MB rate no OACs)]
The WF reflected the relative impact of death and/or disability of MB rate in patients with warfarin or DOACs versus suffering from TE rate in those with no OACs. We assigned a WF of 1.0 as a base case and also provided additional sensitivity analyses by using WF of 1.5 and 2.0.
The NCB of warfarin and DOACs was calculated in overall, male and female AF patients according to the NCB of OACs in warfarin and DOACs cohort, respectively.
Results
A total of 3,402 AF patients were recruited in the COOL AF Thailand study. The mean age of patients was 67.38 ± 11.27 years (Table 1). Patients with OACs at baseline were older than those without OACs. Nearly 60% of patients were male sex. Most patients had hypertension and about one-third had a history of heart failure or left ventricular systolic dysfunction. Most patients in this study had high stroke risk (CHA2DS2-VASc score of 2 or more) and low bleeding risk (HAS-BLED less than 3). About one-fifth of patients had concomitant antiplatelet therapy. The proportion of patients treated with antiplatelets in the group without OACs was higher than those with OAC. Warfarin was commonly used in this study. The average time in therapeutic range (TTR) in patients with warfarin was 53.6 ± 26.4%.
Risk of thromboembolic events according to the CHA2DS2-VASc score
Annual thromboembolic (TE) events of AF patients with or without OACs increased according to CHA2DS2-VASc score (Table 2). The cumulative incidences of thromboembolic events increased following CHA2DS2-VASc score as well (Fig. 1).
The overall TE rate in non-anticoagulated AF patients with CHA2DS2-VASc score of 2 or more was 2.34% (95%CI 1.55–3.42%) while it was 0.73% (95%CI 0.09–2.68%) and 1.24% (95%CI 0.41–2.92%) in those with score of 0 or 1, respectively.
In the group with CHA2DS2-VASC score of 0–1, the rate of TE in patients treated with OAC was similar to those without OACs (0.16 vs. 1.03, p value 0.100). In the group with CHA2DS2-VASC score of 2 or more, the rate of TE in patients with OACs was numerically lower than those without OACs (1.52 vs. 2.34, p value 0.740), however, the difference was not statistically significant (adjusted HR 0.74, 95%CI 0.41–1.34, p value 0.74) (Table 3). In warfarin cohort, AF patients without OACs had increased TE rate in those patients with CHA2DS2-VASc score of 2 or more compared with those with score of 0–1 as well as any OACs cohort. However, there was a trend in reduced TE rate in those patients with CHA2DS2-VASc score of 2 or more with non-statistical significance (adjusted HR 0.77; 95%CI 0.43 to 1.40; p = 0.391) (Table 3). In DOACs cohort, AF patients without OACs had incremental TE rate in those patients with CHA2DS2-VASc score of 2 or more compared with those with score of 0–1 as well as aforementioned cohort. As warfarin cohort, DOACs could reduce TE rate in those patients with CHA2DS2-VASc score of 2 or more with no statistical significance (adjusted HR 0.56; 95%CI 0.13 to 2.48; p = 0.444) (Table 3).
The Kaplan Meier curve showed anticoagulated AF patients with CHA2DS2-VASc score of 2 or more had the lower TE rate compared to those non-anticoagulated patients with statistical significance (p = 0.043) (Fig. 2A) while there was comparable TE rate in AF patients taking DOACs and warfarin (p = 0.245) (Fig. 2C). Nevertheless, there were trends in lower TE rate in AF patients taking warfarin (p = 0.067) and DOACs (p = 0.055) compared to no OACs (Fig. 2E and G).
Risk of major bleeding events based on CHA2DS2-VASc score
Annual MB events of overall AF patients with or without OACs increased according to CHA2DS2-VASc score (Table 4). The cumulative incidences of MB events increased following CHA2DS2-VASc score as well (Fig. 1).
In the group with CHA2DS2-VASC score of 2 or more, the incidence of MB events in patients treated with OACs was higher than those without OACs (p = 0.018) (Fig. 2B). while there were comparable MB events in AF patients taking DOACs compared to warfarin (p = 0.169) (Fig. 2D) and those patients taking DOACs compared to no OACs (p = 0.843) (Fig. 2H). Nevertheless, there were higher MB events in AF patients taking warfarin compared to no OACs (p = 0.012) (Fig. 2F).
In the Cox regression model, OACs was associated with higher risk of major bleeding than those without OACs (OACs vs. no OAC; adjusted HR 2.29, 95%CI 1.26–4.14, p = 0.006). The difference was driven by a significant higher bleeding risk in those who were treated with warfarin (warfarin vs. no OACs; adjusted HR 2.38, 95%CI 1.32–4.32, p = 0.004). Compared with no OACs, the risk of major bleeding in those treated with DOACs was numerically higher (DOACs vs. no OACs; adjusted HR 3.62, 95%CI 0.88–14.80), the difference was not statistically significant (p = 0.074) (Table 5).
Net clinical benefit between TE and MB rate based on CHA2DS2-VASc score
The NCB for any OACs was superior to no OACs in the group with CHA2DS2-VASc score of 3 or more (NCB 0.52; 95%CI 0.33 to 0.73). The NCB for any OACs was slightly superior to no OACS in patients with CHA2DS2-VASc score of 0–1 (NCB 0.04; 95%CI 0.04 to 0.05) while inferior in those with CHA2DS2-VASc score of 2 (NCB − 1.78; 95%CI -2.07 to -1.49). However, the NCB was lower when we assigned WF of 1.5 and 2.0, respectively (Table 6; Fig. 3).
In the analysis of warfarin versus no OACs, there were positive NCB for warfarin in patients with CHA2DS2-VASc score of 3 or more (NCB 0.38; 95%CI 0.19 to 0.58) while there were negative NCB in patients with CHA2DS2-VASc score of 0–1 (NCB − 0.17; 95%CI
− 0.28 to − 0.05) and those with CHA2DS2-VASc score of 2 (NCB − 1.97; 95%CI -2.29 to -1.65). However, the NCB was lower when we assigned WF of 1.5 and 2.0, respectively. In the analysis of only well-controlled warfarin (TTR ≥ 65%) compared to no OACs, there was more positive NCB in patients with CHA2DS2-VASc score of 3 or more (NCB 2.63; 95%CI 2.52 to 2.73). In addition, there has been still positive NCB in those patients despite we assigned WF of 1.5 and 2.0, respectively (Table 6; Fig. 3).
The NCB for DOACs was higher than no OACs in patients with CHA2DS2-VASc score of 0–1 (NCB 1.18; 95%CI 0.70 to 1.66) and those with CHA2DS2-VASc score of 3 or more (NCB 2.19; 95%CI 1.82 to 2.57). There were neutral NCB in patients with CHA2DS2-VASc score of 2 (NCB 0.31; 95%CI -1.03 to 1.64). When we assigned WF of 1.5 and 2.0, there has been still positive and neutral NCB, respectively (Table 6; Fig. 3).
The NCB for DOACs was superior to warfarin regardless CHA2DS2-VASc score. When we assigned WF of 1.5 and 2.0, there has been still positive NCB. However, there was less NCB in patients taking DOACs compared to well-controlled warfarin (TTR ≥ 65%) when we assign WF of 1.0, 1.5 and 2.0 (Table 6; Fig. 3).
When AF patients were stratified according to sex, the superior NCB of any OACs versus no OACS was found in females with CHA2DS2-VASc score of 3 or more. Males with CHA2DS2-VASc score of 0–1 had a positive NCB for both warfarin and DOACs. Males with DOACs had a positive NCB in patients with CHA2DS2-VASc score of 0–2 while the NCB was negative in patients with CHA2DS2-VASc score of 3 or more. In the analysis of only well-controlled warfarin (TTR ≥ 65%) compared to no OACs, there was improved NCB in males with CHA2DS2-VASc score of 3 or more (NCB 0.43; 95%CI -0.16 to 1.01). In the analysis of DOACs compared to warfarin, there was positive NCB in females with CHA2DS2-VASc score of 3 or more and males with CHA2DS2-VASc score of 0–2. Compared to well-controlled warfarin (TTR ≥ 65%), there was less NCB in AF patients regardless sex and CHA2DS2-VASc score (Table 7).
Discussion
To the best of our knowledge, there were several clinical trials demonstrating the OACs can reduce thromboembolic events in AF patients [2, 3]. However, there was increased MB rate including ICH from these medications. Previous trial by Singer et al. has shown that there was a positive NCB between TE rate and ICH in AF patients with CHADS2 of 2 or more among patients taking warfarin [14]. Thereafter, Olesen et al. showed that there was a positive NCB between TE rate and bleeding events in those patients with CHA2DS2-VASc score of 2 or more receiving warfarin [15].
This study was conducted in AF patients with OACs including warfarin and DOACs and stratified patients according to CHA2DS2-VASc score. The TE rate and the MB rate increased according to CHA2DS2-VASc score. The survival analysis illustrated that the OACs reduced TE rate while increased MB rate in those anticoagulated patients with CHA2DS2-VASc score of 2 or more with statistical significance.
Although most anticoagulated patients in this cohort study had a low bleeding risk of OACs reflecting from low HAS-BLED score (83.9%), there was significant increased MB rate in those patients with CHA2DS2-VASc score of 2 or more in patients receiving any OACs driven by the use of warfarin. Nevertheless, in the group of CHA2DS2-VASC score of 2 or more, patients treated with DOACs had higher MB rate than patients without OACs, though the difference was not statistically significant. The results of DOACs cohort were consistent with previous DOACs trials showing that these medications did not increase major bleeding events and reduce ICH [10,11,12,13].
When the NCB between TE and MB rate was analyzed, this cohort study showed that the positive NCB of any OACs in AF patients with CHA2DS2-VASc score of 3 or more while there was negative NCB of any OACs in those patients with CHA2DS2-VASc score of 2. Our results were not consistent with previous VKA trial from Olesen et al. However, previous aforementioned trial defined bleeding events including all bleedings in gastrointestinal tract, urinary tract, airways and ICH [15]. No major or minor bleeding events was classified in Olesen’s trial [15]. This led to the benefit of thromboembolic reduction outweighed the risk of bleeding events from inclusion of minor bleeding.
However, Singer et al. showed that there was the positive NCB between TE rate and ICH in those patients with CHADS2 score of 2 or more receiving warfarin [14]. Previous trials have demonstrated that the stroke risk in AF patients with CHADS2 score of 2 was 4.0% which was consistent with CHA2DS2-VASc score of 4 [20, 21]. For this evidence, those trial should reflect the positive NCB of warfarin in patients with CHA2DS2-VASc score of 4 as well. Nevertheless, those trial used only ICH for calculating NCB that was different from our trials.
When this trial classified patients according to the types of OACs, the NCB in patients with warfarin was similar to the results of any OACs cohort while there was positive NCB in patients with DOACs and CHA2DS2-VASc score of 0–1 and 3 more. This showed that the patients taking DOACs had lower MB rate compared with patients taking warfarin leading to more NCB as aforementioned results. This was confirmed by the NCB for DOACs was superior to warfarin regardless CHA2DS2-VASc score.
Previous trials demonstrated that Asian patients had more bleeding events compared with western patients [22,23,24,25,26,27]. This led to the negative NCB in those patients with warfarin in our cohort study. Because DOACs did not increase MB rate and decreased ICH, patients with DOACs and CHA2DS2-VASc score of 0–1 and 3 more had the positive NCB.
In addition, prior cohort study has shown the influence of sex was appeared to be associated with stroke and MB risk. Females have been associated with increased stroke risk while males have been associated with increased MB risk. The benefit of OACs favored in females [28]. This supported our study demonstrating that the NCB of OACs was more positive and negative according to increased CHA2DS2-VASc score in females and males, respectively.
However, our cohort study had several limitations. First, most patients in this trial were prescribed warfarin (91.1%) while patients without OACs may be prescribed other antithrombotic therapy such as antiplatelets. An ischemic stroke had many mechanisms and some patients might have large-artery atherosclerosis mechanism [29]. This mechanism of ischemic stroke was prevented by antiplatelets leading to decreased benefit of thromboembolic prevention in NCB formula. However, this study recruited only AF patients, so most TE rate in these patients was expected to be from thromboembolism and previous trial has shown that antiplatelet alone increased the risk of ischemic stroke/TIA with statistically significance [30]. Second, only 8.9% of OACs was DOACs leading to limit the power for interpretation of TE and MB rate. The lower prevalence of DOACs uses might cause the lower expected event rate and led to difficult for interpretation of NCB. However, this trial was the first study demonstrating the positive NCB in patients with DOACs. Finally, this study enrolled only Thai AF patients leading to limit the generalizability in other races.
Conclusions
AF patients with CHA2DS2-VASc score of 3 or more regardless warfarin or DOACs had a positive NCB. The NCB of OACs was more positive for DOACs compared to warfarin and for females compared to males.
Data Availability
The dataset that was used to support the conclusion of this study is included within the manuscript. Any other additional data will be made available upon request to the corresponding author.
Abbreviations
- AF:
-
Atrial fibrillation
- ATRIA:
-
AnTicoagulation and Risk Factors In Atrial Fibrillation
- CI:
-
Confidence interval
- CIEDs:
-
Cardiovascular implantable electronic devices
- CKD:
-
Chronic kidney disease
- CREC:
-
Central Research Ethics Committee
- CT:
-
Computed tomography
- DOACs:
-
Direct oral anticoagulants
- HR:
-
Hazard ratio
- ICH:
-
Intracranial hemorrhage
- ICH:
-
GCP-International Conference on Harmonization for Good Clinical Practice Guidelines
- LVEF:
-
Left ventricular ejection fraction
- MB:
-
Major bleeding
- MRI:
-
Magnetic resonance imaging
- NCB:
-
Net clinical benefit
- OACs:
-
Oral anticoagulants
- SD:
-
Standard deviation
- TE:
-
Thromboembolic
- TIA:
-
Transient ischemic attack
- TTR:
-
Time in therapeutic range
- WF:
-
Weighting factor
References
Risk factors for stroke. And efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154(13):1449–57.
Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent Stroke in patients with atrial fibrillation: a meta-analysis. Ann Intern Med. 1999;131(7):492–501.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent Stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857–67.
Chiang CE, Okumura K, Zhang S, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on Stroke prevention in atrial fibrillation. J Arrhythm. 2017;33(4):345–67.
Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018;154(5):1121–201.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS Guideline for the management of patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74(1):104–32.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2020;42(5):373–498.
Methavigul K, Winijkul A, Apiyasawat S, Methavigul R, Patmuk T, Srirattana P. Rate and reasons for the use of oral anticoagulants in patients with non-valvular atrial fibrillation and a CHA2DS2-VASc score of 0 in Thailand: the COOL-AF Registry. J Med Assoc Thai. 2020;103(10):987–95.
Fang MC, Go AS, Chang Y, et al. Death and disability from warfarin-associated intracranial and extracranial hemorrhages. Am J Med. 2007;120(8):700–5.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Singer DE, Chang Y, Fang MC, et al. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151(5):297–305.
Olesen JB, Lip GY, Lindhardsen J, et al. Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation: a net clinical benefit analysis using a ‘real world’ nationwide cohort study. Thromb Haemost. 2011;106(4):739–49.
Alnsasra H, Haim M, Senderey AB, et al. Net clinical benefit of anticoagulant treatments in elderly patients with nonvalvular atrial fibrillation: experience from the real world. Heart Rhythm. 2019;16(1):31–7.
Krittayaphong R, Winijkul A, Methavigul K, et al. Risk profiles and pattern of antithrombotic use in patients with non-valvular atrial fibrillation in Thailand: a multicenter study. BMC Cardiovasc Disord. 2018;18(1):174.
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the S, Standardization Committee of the International Society on T, Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–4.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting Stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting Stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–70.
Lip GY, Frison L, Halperin JL, Lane DA. Identifying patients at high risk for Stroke despite anticoagulation: a comparison of contemporary Stroke risk stratification schemes in an anticoagulated atrial fibrillation cohort. Stroke. 2010;41(12):2731–8.
Methavigul K, Boonyapisit W. Optimal INR level in Thai atrial fibrillation patients who were receiving warfarin for Stroke prevention in Thailand. J Med Assoc Thai. 2014;97(12):1274–80.
Cheung CM, Tsoi TH, Huang CY. The lowest effective intensity of prophylactic anticoagulation for patients with atrial fibrillation. Cerebrovasc Dis. 2005;20(2):114–9.
You JH, Chan FW, Wong RS, Cheng G. Is INR between 2.0 and 3.0 the optimal level for Chinese patients on warfarin therapy for moderate-intensity anticoagulation? Br J Clin Pharmacol. 2005;59(5):582–7.
Yamaguchi T. Optimal intensity of warfarin therapy for secondary prevention of Stroke in patients with nonvalvular atrial fibrillation: a multicenter, prospective, randomized trial. Japanese Nonvalvular Atrial Fibrillation-Embolism Secondary Prevention Cooperative Study Group. Stroke. 2000;31(4):817–21.
Optimal oral anticoagulant. Therapy in patients with nonrheumatic atrial fibrillation and recent cerebral ischemia. N Engl J Med. 1995;333(1):5–10.
Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial Hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007;50(4):309–15.
Krittayaphong R, Phrommintikul A, Winijkul A, et al. Influence of gender on the clinical outcomes of Asian non-valvular atrial fibrillation patients: insights from the prospective Multicentre COOL-AF registry. BMJ Open. 2021;11(5):e043862.
Adams HP Jr., Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic Stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Krittayaphong R, Winijkul A, Methavigul K, et al. The rate of clinical outcomes in Atrial Fibrillation according to Antithrombotic Strategy: the COOL-AF Registry. Cardiovasc Ther. 2022;2022:5797257.
Acknowledgements
The authors gratefully acknowledge all of the investigators and nurse coordinators of the COOL-AF Thailand registry.
Funding
This study was funded by grants from the Health Systems Research Institute (HSRI) (grant no. 59 − 053), and from the Heart Association of Thailand under the Royal Patronage of H.M. the King.
Author information
Authors and Affiliations
Contributions
KM, RK - conception and design of the study, or acquisition of data, AY - analysis and interpretation of data, KM, RK, PC - drafting the article or revising it critically for important intellectual content, all authors read and approved the final manuscript to be submitted.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The trial protocol was approved by the Central Research Ethics Committee (CREC; certificate number is COA-CREC 003/2014). Written informed consent was obtained by all participated patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Methavigul, K., Chichareon, P., Yindeengam, A. et al. Net clinical benefit of oral anticoagulants in Asian patients with atrial fibrillation based on a CHA2DS2-VASc score. BMC Cardiovasc Disord 23, 623 (2023). https://doi.org/10.1186/s12872-023-03643-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03643-8